Abstract
Background
This study aimed to explore the association between drinking water source and risk of upper gastrointestinal (UGI) cancer, including esophageal cancer (EC) and gastric cancer (GC), in the Linxian General Population Nutrition Intervention Trial (NIT) cohort.
Methods
In this study, we used data from the Linxian NIT cohort, which included 29,584 healthy adults aged 40 to 69 years. Subjects were enrolled in April 1986 and followed up until March 2016. Tap water drinking status and demographic characteristics were collected at baseline. Subjects who drank tap water were treated as the exposed group. Hazard ratios (HRs) and 95% confidence intervals (95% CIs) were estimated using the Cox proportional hazard model.
Results
A total of 5,463 cases of UGI cancer were identified during the 30-year follow-up period. After adjusting for multiple factors, the incidence rate of UGI cancer in participants who drank tap water was significantly lower compared with individuals in the control (HR = 0.91, 95% CI: 0.86–0.97). A similar association was observed between tap water drinking and EC incidence (HR = 0.89, 95% CI: 0.82–0.97). The association between drinking tap water and risk of UGI cancer and EC incidence did not vary across the subgroup by age and gender (All Pinteraction > 0.05). For EC incidence, an interaction effect was observed for riboflavin/niacin supplements and drinking water source (Pinteraction = 0.03). No association was observed between drinking water source and GC incidence.
Conclusions
In this prospective cohort study in Linxian, participants who drank tap water had a lower risk of EC incidence. As a source of drinking water, use of tap water may reduce the risk of EC by avoiding exposure to nitrate/nitrite. Measures should be taken to improve the quality of drinking water in high-incidence areas of EC.
Trial registration
The trial is registered with ClinicalTrials.gov (NCT00342654, 21/06/2006), and the trial name is Nutrition Intervention Trials in Linxian Follow-up Study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Both lifestyle and environmental factors are important risk factors for the development of cancer [1, 2], and lifestyle determinants have been found to be significant predictors of environmental carcinogens in humans [3,4,5]. In recent years, the causal relationship between water environments and cancer epidemiology has been extensively studied on multiple scales. Studies have shown that populations in areas with high exposure to organic or inorganic pollutants in water environments may experience high cancer or non-cancer mortality [6,7,8]. Since 2004, certain villages in the Chinese Huai River Basin with high mortality from cancers, referred to as "cancer villages," have been widely reported by the domestic media [9]. In 2013, the Chinese Center for Disease Control and Prevention directly confirmed the association between water pollution and cancer incidence in their research on the Correlation between Cancer and the Huai River Water Environment [10]. This study demonstrated that cancer incidence increased in the 10–15 years after water pollution in the Huai River basin, and pollution levels had a dose–response relationship with cancer incidence/mortality. Additionally, pollutants in the water environment enter the human body, and their metabolites are found in human blood and tissues [10]. Drinking water is known to be an effective exposure route for carcinogenic contaminants, as any chemicals generated by human activity can and will find their way into water supplies [11]. Drinking water habits, as a lifestyle factor, may to some extent reflect pollution in the environment surrounding the drinking water source. Both biological and chemical contaminants (such as nitrate, phosphates, heavy metals, and endocrine-disrupting chemicals) in drinking water can have short- and long-term health effects [12]. Moreover, toxic chemicals ingested from the environment can be present in a variety of human biological samples, including cord blood, placental tissues, and amniotic fluid, which can be transmitted to the fetus through the placenta, leading to adverse pregnancy outcomes [13, 14].
China is a country with high incidence of esophageal (EC) and gastric cancer (GC), both of which are among the top ten most common cancers and top five leading causes of cancer deaths in the Chinese population [15]. In recent years, studies have examined the relationship between drinking water quality and the occurrence of these cancers. A previous study in Iran, a high-incidence country for EC, showed that drinking un-piped water, in addition to common risk factors such as smoking, nutrient-deficient diets, and drinking hot tea, significantly increased the risk of EC incidence [16]. High concentrations of nitrate and nitrite in water are a common characteristic among most countries with a high GC incidence, such as Chile, Costa Rica, and Japan [17]. Linxian, a rural county of Anyang, Henan Province, is one of the high-incidence regions of upper gastrointestinal (UGI) cancer in China [18]. The region's arid climate and low annual rainfall make surface water, such as mountain spring water and shallow well water, the primary water resource [19]. Carcinogens in drinking water were hypothesized to be associated with high cancer incidence, leading to a series of drinking water tests and animal cancer-inducing tests in Linxian. Investigations conducted in the 1980s showed that natural drinking water sources in Linxian contained higher levels of nitrate and nitrite [20]. Etiological studies of digestive cancer have shown that concentrated drinking water can induce esophageal neoplasms and gastric papillomas in mice [21]. The government started to improve water quality in Linxian by installing tap water from the 1970s to 1980s, but few prospective studies evaluated the protective effects of drinking tap water on decreased UGI cancer risk.
In the 1980s, a Nutrition Intervention Trial (NIT) was initiated in Linxian's general population to explore whether vitamin and mineral supplements could reduce cancer incidence and common chronic disease mortality. At baseline, all participants' use of tap water was collected, and the follow-up lasted until the present day. We assumed that UGI cancer incidence varied by the type of drinking water, and in this study, we examined the association between drinking water and the risk of UGI cancer incidence based on the 30-year follow-up data in the Linxian NIT cohort.
Material and methods
Study population
This prospective observational cohort study was conducted between 1986 and 2016 on healthy adults residing in Linxian. The detailed design of the NIT cohort has been previously described [22, 23]. Potential participants were eligible if they were between the ages of 40 and 69, lived in one of the communes in northern Linxian (Yaocun, Rencun, Donggang, and Hengshui), volunteered to participate in the study, and provided consent. Subjects with malignancy, regular intake of vitamin and mineral supplements, or regular use of specific medications such as the traditional drug Anti-Tumor B3 or synthetic retinoids were excluded from this study. Finally, a total of 29,584 subjects were included in the NIT study in 1986. All participants received daily supplementation based on a factorial design consisting of four factors: factor A (retinol/zinc), factor B (riboflavin/niacin), factor C (vitamin C/molybdenum), and factor D (selenium/vitamin E/beta-carotene) [21]. After a baseline survey, subjects were randomly assigned to one of eight intervention groups based on a 24 fractional factorial design, which received factors ABCD, AB, AC, AD, BC, BD, CD, or placebo, respectively. With this design, half of the subjects received each of the four factors and half did not [23]. The doses of these daily supplements are shown in Supplementary Table S1. Before enrollment, each participant was asked to provided informed consent. The intervention lasted from March 1986 to May 1991. This study was approved by the institutional review boards of the Cancer Hospital Chinese Academy of Medical Sciences (CHCAMS) and the US National Cancer Institute (NCI).
Baseline survey
All participants underwent a physical examination at local village hospitals and completed a standardized questionnaire administered by trained study personnel and research technicians. The protocol included quality control measures to ensure consistency across all data collected. The standard questionnaire was used to collect demographic and lifestyle characteristics at baseline, including age, sex, smoking, alcohol consumption, educational level, family history of UGI cancer, and dietary habits. Smoking was defined as the regular use of cigarettes or pipes for at least six months, and alcohol use was categorized as daily, weekly, monthly, yearly, or never according to the frequency of use in the past 12 months. Participants were asked whether they had tap water installed as a source of drinking water in their home, and responses were categorized as 'yes' or 'no'. To assess fresh fruit and vegetable intake, participants were asked how often they consumed fresh fruit and vegetable in the 12 months prior to the interview. To avoid seasonal effects, the frequency of fruit and vegetable consumption in winter/spring and summer/autumn was calculated separately. Responses could be 'never', 'times/day', 'times/week', 'times/month', or 'times/year' and were all converted to one unit (times/year). We also collected data on the frequency of preserved vegetable, moldy vegetable juices, and moldy staple foods consumption (times/year), given the potential presence of dietary carcinogens. Family history of UGI cancer was considered positive if the subject had one or more first-degree relatives diagnosed with esophageal cancer or gastric cancer. Trained staff measured participants' height and weight while subjects were not wearing shoes according to a standard protocol. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared (kg/m2). Additionally, we collected information on the history of consumptive disease. Participants were asked whether they had ever been diagnosed with a severe disease that prevented them from doing household chores or performing labor (such as cardiovascular disease, stroke, cirrhosis, or diabetes mellitus), and the answer was recorded as 'yes' or 'no'.
Follow-up
During the 5.25-year trial period (March 1986—May 1991), village medical staff visited all participants monthly to deliver pills, assess compliance, ascertain endpoint events, and collect diagnostic materials. In this period, cancer cases were confirmed by an International Endpoints Review Committee consisting of American and Chinese senior experts. After the trial period, local medical workers continued to visit surviving participants every three months. New cancer cases and all-cause deaths were verified by a panel of American and Chinese experts from 1991 to 1996, and by senior Chinese doctors from 1996 to 2017, using diagnostic materials such as case records, biochemical results, ultrasound, X-rays, endoscopy, surgery reports, and pathology or cytology slides.
Statistical analysis
Participants were censored at the last known follow-up date, date of death, or the date of the study closure (March 2016), whichever came first. The primary outcomes of our study were primary EC (ICD10: C15) and GC (ICD10: C16) incidence. Participants were divided into two categories according to their tap water drinking status (do not drink tap water and drinking tap water), with no tap water-drinking as the reference. Differences in baseline demographic characteristics between different tap water drinking statuses were compared using the Chi-square test for categorical variables and t-test or nonparametric tests for continuous variables. Univariate and multivariable Cox proportional hazards regression models were used to calculate hazard ratios (HRs) and 95% confidence intervals (95% CIs) for the association between tap water drinking and the risk of UGI cancer incidence. Potential covariates in the models included age at baseline, gender, BMI, smoking, alcohol drinking, family history of UGI cancer, education level, nutrition intervention arms, communes, history of consumptive disease, and frequency of intakes of fresh fruit, fresh vegetables, preserved vegetables, moldy vegetable juice, and moldy staple foods. Subgroup analyses were conducted to evaluate whether the association varied by age at baseline, gender, and nutritional intervention arms. Cumulative incidence rates were estimated using the Kaplan–Meier method, and differences between the cumulative incidence curves were assessed using log-rank tests. Sensitivity analysis was conducted by excluding participants followed up for less than three years to assess reverse causality. Statistical analyses were performed using SPSS 23.0. All tests were two-tailed, and a P value of < 0.05 was considered statistically significant.
Results
Overall, a total of 29,449 individuals were included in the final analysis. The CONSORT flow diagram for the Linxian Nutrition Intervention Trial is shown in Supplementary material Figure S1. During the 30-year follow-up, we identified 5,463 UGI cancer cases, including 3,103 EC cases and 2,360 GC cases. Table 1 shows the baseline characteristics of participants with different drinking tap water statuses. There were significant differences in age at baseline, BMI, smoking status, education level, communes, history of consumptive disease, and frequency of intakes of fresh fruit, fresh vegetable, and moldy staple foods (All P values < 0.05).
Table 2 presents the associations between drinking tap water and the risk of UGI cancer incidence. After adjusting for age at baseline and gender, the risk of UGI cancer and EC incidence in participants who drank tap water was significantly decreased by 14, 16, and 12%, respectively (HRUGI cancer = 0.86, 95%CI:0.81–0.92; HREC = 0.84, 95%CI: 0.77–0.92; HRGC = 0.88, 95%CI:0.80–0.98). The difference was still significant after controlling for potential confounders, including age at baseline, gender, BMI, smoking, alcohol drinking, family history of UGI cancer, education level, nutrition intervention arms, communes, history of consumptive disease, and frequency of intakes of fresh fruit, fresh vegetable, preserved vegetable, moldy vegetable juice, and moldy staple foods (HRUGI cancer = 0.91, 95%CI:0.86–0.97; HREC = 0.89, 95%CI: 0.82–0.97). No association between drinking tap water and the risk of GC incidence was observed in the multivariable model (HRGC = 0.94, 95%CI: 0.85–1.03). Cumulative incidence curves of total UGI cancer, EC, and GC by types of drinking water are presented in Fig. 1.
After stratification by age at baseline and gender, the associations between drinking tap water and the risk of UGI cancer incidence were significant among younger (< 55 years) participants (HR = 0.90, 95%CI:0.83–0.98) and males (HR = 0.89, 95%CI: 0.81–0.98), while for both males and females, subjects who drank tap water had 12% (HR = 0.88, 95%CI: 0.77–0.99) and 13% (HR = 0.87, 95%CI: 0.78–0.98) lower risk of EC incidence, respectively. The association between drinking tap water and the risk of UGI cancer and EC incidence did not vary by age and gender (All P interaction > 0.05) (Table 3).
Table 4 presents the risk of UGI cancer incidence after stratification by nutrition intervention. Among subjects who did not receive Factor B, the incidence of EC was significantly lower in the tap water group (HREC = 0.82, 95%CI: 0.73–0.93). The association between drinking tap water and the risk of EC incidence was different for riboflavin and niacin (Factor B) supplementation (P interaction = 0.03). No interaction effects between drinking tap water and other nutrient supplements were observed for the risk of UGI cancer or GC incidence.
Sensitivity analysis was performed to assess reverse causality. After excluding participants with less than three years of follow-up, our results did not materially change, indicating the robustness of the study's analysis (Table 5).
Discussion
In this prospective cohort study, we observed that drinking tap water was associated with a reduced risk of upper gastrointestinal (UGI) cancer incidence, particularly esophageal cancer (EC). For EC incidence, we noted an interaction effect between riboflavin/niacin supplements and the type of drinking water. However, we did not find any associations with gastric cancer (GC) in all subjects or any subgroup.
The quality of drinking water is essential for human health. Despite improvements in socio-economic levels in recent decades, access to an improved water source remains a significant issue [24]. Assessing potential links between drinking water and cancer could help identify harmful chemicals that appear in water supplies at concentrations sufficient to pose a substantial attributable cancer risk. Many studies have shown the relationship between drinking water quality and the risk of breast, kidney, bladder, and colorectal cancers [21, 25,26,27]. However, few studies have explored the association between drinking water and UGI cancer risk. In this study, we found that participants who drank tap water had a significantly lower risk of EC incidence than those who did not drink tap water. This finding is consistent with a previous study conducted in Iran, which is also a high-incidence country for EC [12]. The association between drinking water and cancer is reportedly due to the contamination of water with chemical pollutants such as nitrite and nitrosamines [28]. Nitrosamines are a group of environmental pollutants that are mutagenic, teratogenic, and carcinogenic [29]. Darvishmotevalli M et al. investigated the carcinogenic risks related to nitrate exposure in drinking water in Iran based on a cross-sectional study [30]. The findings demonstrated that most provinces in Iran had impermissible levels of nitrate in drinking water supplies, and the carcinogen risk values of nitrate exposure through drinking water were 0.001% (Risk level for assessing the carcinogen risk was 10 − 5 [1 per 100,000 persons]). This study also indicated an association between gastrointestinal cancer and nitrate exposure through drinking water [30, 31]. In addition to direct exposure, precursors like nitrates, nitrites, and secondary and tertiary amines are potential sources of nitrosamines in vivo [32].
Before our study, researchers found that the levels of ammonia nitrogen, nitrate, and nitrite in drinking water in Linxian were significantly higher than those in other low-incidence areas [33]. Additionally, the urine nitrate and nitrite content of residents in Linxian were significantly higher than those of the control population from low-incidence areas [33]. To explore the association between drinking water in Linxian and UGI cancer, researchers concentrated well water ten times as drinking water for rats and induced EC and gastric cardia cancer [33]. Since the early 1980s, the villages in Linxian have started to improve water quality. The government mainly replaced mountain spring water, shallow well water, and canal water with deep well water, as well as replacing river water and stream water with mountain spring water [21]. However, some villages with mountain spring water did not change the water source as they did not need to invest. Residents who did not install tap water in their homes usually continued to use shallow well water due to their previous drinking habits [34]. In Linxian, most organic fertilizer comes from farmyard manure, which is the source of contamination of amines and amides. In the 1980s, the management of farmyard manure did not gain enough prominence, and compost heaps, toilets, and pig pens persisted within 30 m of the water source [34]. This could increase intakes of nitrite and amines from drinking water sources. Based on previous research on the etiology of esophageal cancer (EC), improving the quality of drinking water is considered the most effective way to reduce the incidence of EC. Our study found that after controlling for other risk factors that affect the incidence of EC, drinking tap water was associated with an 11% decreased risk of EC incidence, which supports the hypothesis that water sources can reduce the risk of EC.
The influence of drinking water quality on the incidence of upper gastrointestinal (UGI) cancer may vary depending on nutrient intake. Deficiency concentrations of trace elements also play an important role in the medical geology of esophageal cancer (EC). Some metals, when consumed through food and water, are involved in various physiological processes [35]. Keshavarzi et al. compared the concentrations of trace elements in high- and low-incidence areas of EC and found that the average concentrations of Sb, Se, Sr, and Zn in the high-incidence areas of EC were 12.2, 8.9, 3,437.3, and 30.3 µg/L, respectively, while in the low-incidence areas, they were only 4.1, 2.3, 1,102.3, and 83.3 µg/L, respectively [12]. Analysis of EC rates in high- and low-incidence areas of China has shown an inverse association between EC mortality rate and the contents of selenium in the soil [36], which may be related to the inhibitory effect of this element on indigenous nitrosamine compound production. Deficiency of trace elements in the soil has led to reductions in their concentrations in crops [37]. Under conditions of limited trace element intake from diet, the carcinogenesis of esophageal epithelium may be affected. In addition, the antioxidant effect helps counteract carcinogens, including nitrosamine and aflatoxin [38]. Fresh fruits and vegetables are good sources of dietary antioxidants [39]. The existing dietary review survey results revealed that the diet composition in Linxian was monotonous, had obvious seasonal characteristics, and the average levels of various micronutrients and fats in the diet did not meet the nutritional requirements [40]. Therefore, high levels of carcinogens and low trace minerals in natural water sources, combined with a lack of antioxidant intake, may increase the risk of EC. The combined effects of antioxidant deficiency and nitroso compound intake have been supported by animal experiments. Pan et al. evaluated the effects of N-nitroso methylbenzylamine (NMBA) and riboflavin (RBF) deficiency individually or in combination on esophageal tumorigenesis in rats, and the results suggest that RBF deficiency causes chronic inflammation-associated genomic instability that contributes to NMBA-induced esophageal tumorigenesis [41]. Odeleye et al. investigated the contribution of retroviral immunosuppression to esophageal cancer induced by the carcinogen N-nitroso methylbenzylamine (NMBzA) and the effect of increased levels of dietary vitamin E on induced carcinogenesis. They found that vitamin E could play an antioxidant role that reduced the incidence of ECs in both immunocompromised and non-immunocompromised animals [42]. In our study, the difference in UGI cancer and EC incidence between subjects who received Factor A or Factor B was not significant. This could be explained by the anti-cancer properties of nutrients. Among individuals who received nutrition supplements but did not drink tap water, the adverse effects of carcinogens in drinking water are partially offset by nutrients, resulting in a lower incidence of esophageal cancer. This finding could also support the combined effects of antioxidant deficiency and nitroso compounds intake on the risk of EC. Tap water is potable water supplied to a tap inside the household or workplace that has been treated to remove or reduce contaminants to levels where they are not expected to cause any health effects. Therefore, in areas with severe water pollution, choosing tap water as the drinking water source could effectively prevent adverse effects on human health caused by water pollution.
In our study, we did not find an association between drinking tap water and the risk of GC incidence. Limited studies are available on the relationship between drinking water with nitrate/nitrite content and the risk of GC. However, a meta-analysis conducted by Song P et al. reported significant associations of dietary intakes of nitrates and nitrites with GC observed in case–control studies, while cohort studies still showed a slight trend [43]. In some previous studies, high or moderate consumption of nitrates was even found to have a protective effect on GC [44]. Most of these studies speculated that the possible explanation could be the contribution of fruits and vegetables containing nutrients that inhibit N-nitrosation [43, 44]. During digestion in the stomach, nutrients from food are released, which can inhibit endogenous nitrosation and hinder the formation of nitrosation compounds. The function of the esophagus is to transport food and fluids from the mouth to the stomach rather than digest or absorb nutrients. Concentrations of nutrients in different subsites of the upper digestive tract may partly explain the different effect of drinking water on health status.
Our study has several strengths, including a large study population, a prospective design, a long follow-up duration, and a low rate of loss to follow-up (less than 10%). However, several limitations need to be considered. Firstly, we only conducted a one-time baseline investigation, and changes in drinking water source were not repeatedly measured. Secondly, some unmeasured factors, such as passive smoking, physical activity, smoking and alcohol drinking frequency, and socioeconomic status, could inevitably lead to residual confounding. Thirdly, since this is an observational study rather than an interventional study, contamination between the tap water group and non-tap water group could not be strictly controlled. Finally, we did not measure the levels of nitrite and trace elements in drinking water, and thus the cause of the association between drinking water source and UGI cancer risk could not be inferred.
Conclusions
In summary, our study found that individuals who drank tap water in Linxian had a lower risk of EC incidence compared to those who did not drink tap water. This finding is consistent with previous studies on the etiology of EC, which suggest that the use of tap water as a source of drinking water can reduce the risk of esophageal cancer by avoiding nitrate/nitrite exposure. Therefore, appropriate measures should be taken to improve the quality of drinking water in high-incidence areas of EC. Furthermore, the consumption of dietary antioxidants is recommended as a protective measure.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Lewandowska AM, Rudzki M, Rudzki S, et al. Environmental risk factors for cancer - review paper. Ann Agric Environ Med. 2019;26(1):1–7.
Katzke VA, Kaaks R, Kühn T. Lifestyle and cancer risk. Cancer J. 2015;21(2):104–10.
Moradnia M, Attar HM, Heidari Z, et al. Prenatal exposure to chromium (Cr) and nickel (Ni) in a sample of Iranian pregnant women: urinary levels and associated socio-demographic and lifestyle factors. Environ Sci Pollut Res Int. 2021;28(44):63412–21.
Moradnia M, Movahedian Attar H, Heidari Z, et al. Monitoring of urinary arsenic (As) and lead (Pb) among a sample of pregnant Iranian women. J Environ Health Sci Eng. 2021;19(2):1901–9.
Darvishmotevalli M, Bina B, Feizi A, et al. Monitoring of urinary phthalate metabolites among pregnant women in Isfahan, Iran: the PERSIAN birth cohort. J Environ Health Sci Eng. 2019;17(2):969–78.
Aragonés N, Goicoa T, Pollán M, et al. Spatio-temporal trends in gastric cancer mortality in Spain: 1975–2008. Cancer Epidemiol. 2013;37(4):360–9.
Gao Y, Hu N, Han XY, et al. Risk factors for esophageal and gastric cancers in Shanxi Province, China: a case-control study. Cancer Epidemiol. 2011;35(6):e91–9.
Fantini F, Porta D, Fano V, et al. Epidemiologic studies on the health status of the population living in the Sacco River Valley. Epidemiol Prev. 2012;36(5 Suppl 4):44–52.
Ren H, Wan X, Yang F, et al. Association between changing mortality of digestive tract cancers and water pollution: a case study in the Huai River Basin, China. Int J Environ Res Public Health. 2014;12(1):214–26.
Yang G, Zhuang D. Research on the correlation between cancer and the huai river water environment. In: Yang G, Zhuang D, editors. Atlas of the huai river basin water environment: digestive cancer mortality. dordrecht: Springer; 2014. https://doi.org/10.1007/978-94-017-8619-5_1.
Jedrychowski W, Maugeri U, Bianchi I. Environmental pollution in central and eastern European countries: a basis for cancer epidemiology. Rev Environ Health. 1997;12(1):1–23.
Keshavarzi B, Moore F, Najmeddin A, et al. Quality of drinking water and high incidence rate of esophageal cancer in Golestan province of Iran: a probable link. Environ Geochem Health. 2012;34(1):15–26.
Darvishmotevalli M, Moradnia M, Hosseini R, et al. Association between prenatal phthalate exposure and anthropometric measures of newborns in a sample of Iranian population. Environ Sci Pollut Res Int. 2021;28(36):50696–706.
Hajizadeh Y, Moradnia M, Kiani Feizabadi G, et al. The sex-specific association between maternal urinary paraben levels and offspring size at birth. Environ Sci Pollut Res Int. 2021;28(27):36029–38.
Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–32.
Sheikh M, Poustchi H, Pourshams A, et al. Individual and combined effects of environmental risk factors for esophageal cancer based on results from the Golestan Cohort Study. Gastroenterology. 2019;156(5):1416–27.
Ghaffari HR, Yunesian M, Nabizadeh R, et al. Environmental etiology of gastric cancer in Iran: a systematic review focusing on drinking water, soil, food, radiation, and geographical conditions. Environ Sci Pollut Res Int. 2019;26(11):10487–95.
Yang H, Zhang S, Wang J, et al. Oral leukoplakia and the long-term risk of upper gastrointestinal cancer deaths in the Linxian dysplasia population. Thoracic cancer. 2020;11(10):2804–11.
Cao W, Han J, Yuan Y, et al. Drinking water: a risk factor for high incidence of esophageal cancer in Anyang China. J Environ Geochem Health. 2016;38(3):773–82.
Li MX, Lu SJ, Ji C, et al. Nitrates and nitrites in foods and portable water from Linxian. Aizheng. 1986;5(4):320–3.
Han J, Wang M, Ma Y, et al. Relationship between mutagenic effects of the drinking water and incidence of esophageal cancer in Linxian county: a prevalent area. Henan Yufangyixue Zazhi. 2000;11(2):65–9.
Taylor PR, Li B, Dawsey SM, et al. Prevention of esophageal cancer: the nutrition intervention trials in Linxian, China. Linxian Nutrition Intervention Trials Study Group. Cancer Res. 1994;54(7 Suppl):2029s–31s.
Wang SM, Taylor PR, Fan JH, et al. Effects of nutrition intervention on total and cancer mortality: 2.5-year post-trial follow-up of the 525-Year Linxian Nutrition Intervention Trial. J Natl Cancer Inst. 2018;110(11):1229–38.
Levallois P, Villanueva CM. Drinking water quality and human health: an editorial. Int J Environ Res Public Health. 2019;16(4):631.
Cotruvo JA, Amato H. National trends of bladder cancer and trihalomethanes in drinking water: a review and multicountry ecological study. Dose Response. 2019;17(1):1559325818807781.
Keren Y, Magnezi R, Carmon M, et al. Investigation of the association between drinking water habits and the occurrence of women breast cancer. Int J Environ Res Public Health. 2020;17(20):7692.
Jaafarzadeh N, Poormohammadi A, Almasi H, et al. Arsenic in drinking water and kidney cancer: a systematic review. Rev Environ Health. 2022. https://doi.org/10.1515/reveh-2021-0168. Epub ahead of print.
Keszei AP, Goldbohm RA, Schouten LJ, et al. Dietary N-nitroso compounds, endogenous nitrosation, and the risk of esophageal and gastric cancer subtypes in the Netherlands Cohort Study. Am J Clin Nutr. 2013;97(1):135–46.
Gushgari AJ, Halden RU. Critical review of major sources of human exposure to N-nitrosamines. Chemosphere. 2018;210:1124–36.
Darvishmotevalli M, Moradnia M, Noorisepehr M, et al. Evaluation of carcinogenic risks related to nitrate exposure in drinking water in Iran. MethodsX. 2019;6:1716–27.
Moradnia M, Poursadeghiyan M, Mahvi AH, et al. The relation of cancer risk with nitrate exposure in drinking water in Iran. Iran J Public Health. 2019;48(2):362–4.
Zhao C, Lu Q, Gu Y, et al. Distribution of N-nitrosamines in drinking water and human urinary excretions in high incidence area of esophageal cancer in Huai’an China. Chemosphere. 2019;235:288–96.
Liu G, Yang S. The exploring course of carcinogenesis for esophageal cancer in Linzhou Henan Province. Zhongguo Zhongliu. 2008;17(6):454–6.
Cheng L, Lian S, Liu Z, et al. Influence of water quality improvement on incidence and mortality with esophageal cancer in Linzhou Henan. Zhongguo Zhongliu. 2007;16(12):998–9.
Martínez FG, Moreno-Martin G, Pescuma M, et al. Biotransformation of selenium by lactic acid bacteria: formation of seleno-nanoparticles and seleno-amino acids. Front Bioeng Biotechnol. 2020;12(8):506. https://doi.org/10.3389/fbioe.2020.00506.
Keshavarzi B, Moore F, Najmeddin A, et al. The role of selenium and selected trace elements in the etiology of esophageal cancer in high risk Golestan province of Iran. Sci Total Environ. 2012;433:89–97.
Darch T, Dunn RM, Guy A, et al. Fertilizer produced from abattoir waste can contribute to phosphorus sustainability, and biofortify crops with minerals. PLoS One. 2019;14(9):e0221647.
Wang Y, Yang L, Xia L, et al. High C-reactive protein/albumin ratio predicts unfavorable distant metastasis-free survival in nasopharyngeal carcinoma: a propensity score-matched analysis. Cancer Manag Res. 2018;10:371–81.
Dyshlyuk L, Babich O, Prosekov A, et al. The effect of postharvest ultraviolet irradiation on the content of antioxidant compounds and the activity of antioxidant enzymes in tomato. Heliyon. 2020;6(1):e03288.
Yang H, Zhang S, Yan H, et al. Fresh fruit consumption may decrease the long-term risk of esophageal cancer mortality: a 30-year follow-up study in the Linxian Dysplasia Nutrition Intervention trial (NIT). Thoracic cancer. 2020;11(7):1918–26.
Pan F, Chen Y, He JZ, et al. Dietary riboflavin deficiency promotes N-nitrosomethylbenzylamine-induced esophageal tumorigenesis in rats by inducing chronic inflammation. Am J Cancer Res. 2019;9(11):2469–81.
Odeleye OE, Eskelson CD, Mufti SI, et al. Vitamin E protection against nitrosamine-induced esophageal tumor incidence in mice immunocompromised by retroviral infection. Carcinogenesis. 1992;13(10):1811–6.
Song P, Wu L, Guan W. Dietary nitrates, nitrites, and nitrosamines intake and the risk of gastric cancer: a meta-analysis. Nutrients. 2015;7(12):9872–95.
Zhang FX, Miao Y, Ruan JG, et al. Association between nitrite and nitrate intake and risk of gastric cancer: a systematic review and meta-analysis. Med Sci Monit. 2019;25:1788–99.
Acknowledgements
The authors want to thank the citizens of Linxian who have faithfully participated in these studies over the past 35 years.
Funding
This study was supported by National Cancer Institute contract (contract number: HHSN261201700047C).
Author information
Authors and Affiliations
Contributions
JHF had access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. JHF and YLQ participated in the study concept and design. HY, JBW, and XKW acquired and analyzed data. JHF and YLQ were responsible for interpreting the data. HY and JBW took the lead in drafting the report. Every author participated in editing and finalization. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review boards of the Cancer Hospital Chinese Academy of Medical Sciences (CHCAMS) and the US National Cancer Institute (NCI). Written informed consent was obtained from all participants. All methods were carried out in accordance with relevant guidelines and regulations. This study was carried out in compliance with the declaration of Helsinki.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Doses for daily multivitamins and minerals supplementation. Figure S1. Consort flow diagram of the linxian general population trial.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, H., Wang, Jb., Wang, Xk. et al. Association between type of drinking water and upper gastrointestinal cancer incidence in the Linxian General Population. BMC Cancer 23, 397 (2023). https://doi.org/10.1186/s12885-023-10887-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-10887-2



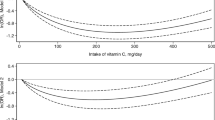


 : non tap water group;
: non tap water group;
 : tap water group
: tap water group