Abstract
Background
Anterior cruciate ligament (ACL) tear is considered as one of the most common sport-related musculoskeletal injuries. Double bundle (DB) and single bundle (SB) surgical techniques has been widely adopted for ACL reconstruction. This systematic review aimed to provide updated evidence by comparing the short-term, mid-term, and long-term knee stability and functional outcomes of DB and SB reconstruction techniques.
Methods
We searched Medline, Web of Science, and CENTRAL. We have selected randomized controlled trials (RCTs) that compared DB and SB ACL reconstruction techniques for primary isolated ACL tear. We have assessed the following outcomes: pivot shift test, Lachman test, KT-1000/2000 knee ligament arthrometer, Lysholm knee function score, Tegner activity score, and graft failure. We have used the standardized mean difference (SMD) was to summarize the continuous outcomes while risk ratio (RR) was used to summarize the dichotomous outcomes.
Results
A total of 34 RCTs that enrolled 2,992 participants deemed eligible. Overall, DB showed significantly better outcomes in terms of pivot shift test (RR = 0.61, 95% confidence interval (CI) 0.49–0.75), Lachman test (RR = 0.77, 95% CI 0.62 to 0.95), and KT 1000/2000 arthrometer (SMD = − 0.21, 95% CI − 0.34 to − 0.08). No discernible difference was found between DB and SB techniques in the overall Lysholm score (SMD = 0.12, 95% CI − 0.03 to 0.27), Tegner score (SMD = 0.03, 95% CI − 0.17 to 0.24), or graft failure rate (RR = 0.78, 95% CI 0.33 to 1.85).
Conclusions
Our review suggests that DB ACL reconstruction technique shows significantly better knee stability and functional outcomes than SB at short-term follow-up. However, both techniques exhibit similar outcomes at mid-term and long-term follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) tear is considered one of the most common sport-related musculoskeletal injuries, representing 50% of all the acute traumatic knee injuries [1]. ACL reconstruction is the standard management approach to restore the biomechanical function of the knee following ACL tears in young active patients [2, 3]. Double bundle (DB) and single bundle (SB) are widely adopted surgical techniques for the anatomical reconstruction of ACL. DB technique involves the anatomical restoration of the anteromedial and posterolateral bundles of the native ACL whereas SB technique in involves the anatomical restoration of the either anteromedial or posterolateral bundle of the native ACL. Recently, there has been a debate about the superiority of DB or SB technique in restoring the knee stability and function following ACL reconstruction [4–6].
A recent systematic review by Kong et al. revealed significantly better knee stability and functional outcomes in favor of DB compared to SB. However, most of the included studies in this review provided short-term follow-up data [7]. More recently, a systematic review by Chen et al. showed that both DB and SB reconstruction techniques confer similar outcomes at mid-term and long-term follow-up. Nonetheless, a small number of studies and relatively small sample size were inherent limitations of this review [8]. In addition, many randomized controlled trials (RCTs) providing mid-term and long-term follow-up data were further introduced to the literature since Chen et al. review [9–12].
The aim was to perform an updated systematic review and meta-analysis by comparing the short-term, mid-term, and long-term knee stability and functional outcomes of DB and SB reconstruction techniques.
Methods
This review was performed according to a pre-established protocol reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [13].
Eligibility Criteria
Patients: adult patients with primary isolated ACL tear; intervention: ACL reconstruction through anatomical DB technique; comparison: ACL reconstruction through anatomical SB technique; outcomes: rotational stability (i.e., pivot shift test), anterior stability (i.e., subjective tests; Lachman test, objective tests; KT-1000/2000 knee ligament arthrometer), functional outcomes including Lysholm knee function score, Tegner activity scale, International Knee Documentation Committee (IKDC) subjective score, and IKDC objective score, return to pre-injury sports activity, and graft failure; study design: RCT. Trials that enrolled participants with concomitant ipsilateral or contralateral posterior cruciate ligament, medial collateral ligament, lateral collateral ligament injury, or previous ligament surgery in the index knee were excluded. DB technique was defined as the individual anatomical restoration of anteromedial and posterolateral bundles of native ACL regardless of the source of the graft or the reconstruction technique. SB technique was defined as the anatomical restoration of the either anteromedial or posterolateral bundle of the native ACL regardless of the source of the graft or the reconstruction technique.
Search Strategy
We searched Medline, Web of Science, Evidence-Based Medicine Review databases via Ovid, and Cochrane Central Register of Controlled Trials (CENTRAL). No restrictions on date or language was applied. We used MeSH terms and keywords for each electronic database when available. Search terms used can be found in the supplementary material. We have also explored the following trial registries for potentially relevant ongoing or recently finished RCTs: ISRCTN registry, Australian New Zealand Clinical Trials Registry, UMIN Clinical Trials Registry, ClinicalTrials.gov, and MetaRegister of Controlled Trials. The last search was performed on August 6, 2020. The bibliographic references of the included RCTs were manually explored for potentially relevant RCTs missed through the electronic search.
Study Selection and Data Extraction
Independently and in duplicate, two reviewers did the eligibility screening for titles and abstracts; full text assessment; and data extraction from the eligible studies. Disagreements were resolved by discussion or the decision of a third reviewer.
Subgroup Analysis
It was pre-specified to perform a subgroup analysis based on different follow-up periods. The different follow-up periods were divided into short-term (≤ 2 years), mid-term (3–5 years), and long-term (> 5 years) follow-up.
Meta-analysis
We used Comprehensive Meta-Analysis version 3 (Biostat, Inc. Eaglewood, New Jersey, USA) for the meta-analysis. The random-effects model was used for all statistical analyses. I2 and the P of the χ2 test were used to assess the statistical heterogeneity. We adopted 95% confidence level as a confidence level and P < 0.05 as a threshold. We have used the standardized mean difference (SMD) was to summarize the continuous outcomes while risk ratio (RR) was used to summarize the dichotomous outcomes. Trials with multiple publications (i.e., follow-up publications for the original trials) were only counted once, but data were derived from all available publications to obtain the longest available follow-up.
Risk of Bias Assessment
Two reviewers, independently and in duplicate, assessed the risk of bias of the eligible RCTs using the Revised Cochrane Risk of Bias Assessment Tool [14]. Any disagreement was resolved by consensus or the decision of a third reviewer. We assessed the publication bias for the primary outcome (pivot shift test) by visual inspection of the funnel plot with RR and standard error. The significance of the funnel plot asymmetry was examined using Egger’s test. Publication bias was further assessed for two of the secondary outcomes Lachman test and Lysholm score.
Results
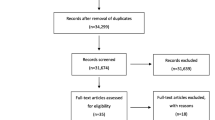
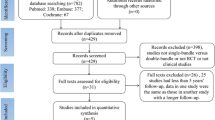
The literature search yielded 10,710 articles, of which 5188 duplicates were excluded. A total of 66 were deemed eligible for full-text assessment, of 27 articles were further excluded, leaving 39 eligible articles which represent 34 RCTs (Fig. 1) [9–12, 15–49].
Trial Characteristics
The 34 eligible RCTs enrolled 2992 participants with ACL tear who received ACL reconstruction through DB (n = 1524) or SB (n = 1468). Of the 2992 participants, 68% were male (n = 2,034) and 32% were female (n = 958). The characteristics of the included RCTs are summarized in Table 1.
Risk of Bias Assessment
Out of 34 RCTs, 7 had an overall low risk of bias, 17 had some concerns, and the remaining 10 had an overall high risk of bias. The risk of bias assessment of the included RCTs is summarized in Table 2.
The funnel plot for pivot shift test was asymmetrical on visual inspection and Egger’s test showed significant plot asymmetry (p < 0.001) (Supplementary Fig. A). The funnel plot for Lachman test was also asymmetrical. However, Egger’s test showed that plot asymmetry was not of statistical significance (P = 0.08) (Supplementary Fig. B). Lysholm score had symmetrical funnel plot on visual inspection, and Egger’s test showed no statistical significance (P = 0.26) (Supplementary Fig. C).
Pivot Shift Test
A total of 26 studies reported data on pivot shift test [9–12, 17, 20–23, 25, 27–36, 38–41, 43–49]. Overall, DB showed significantly better results than SB (RR = 0.61, 95% CI 0.49–0.75, P < 0.001; I2 = 62%). However, subgroup analysis showed that the improvements in pivot shift test in favor of DB became insignificant at mid-term and long-term follow-up (Fig. 2).
Lachman Test
Sixteen studies reported on Lachman test [9, 12, 17, 22, 23, 25, 29, 32, 34–36, 36–41, 43–45]. DB showed a significant reduction in overall the risk of developing positive Lachman test compared to SB (RR = 0.77, 95% CI 0.62 to 0.95, P = 0.01; I2 = 34%). However, subgroup analysis showed that both groups had similar risk of developing positive Lachman test in the mid-term and long-term follow-up (Fig. 3).
KT1000/2000 Arthrometer
Twenty-three studies reported on KT1000-2000 [12, 15–17, 19, 21–24, 27, 28, 30, 32–34, 36, 38–40, 42–49]. Overall, DB showed significantly better results than SB in terms of KT1000/2000 arthrometer (SMD = − 0.21, 95% CI − 0.34 to − 0.08, P < 0.01; I2 = 61%). However, Subgroup analysis showed comparable results in the mid-term and long-term follow-up (Fig. 4).
Lysholm Score
Twelve studies reported on Lysholm score [10, 12, 17–20, 27, 29, 30, 34, 38, 39, 42]. There was no significant difference between DB and SB in terms of overall Lysholm score (SMD = 0.12, 95% CI − 0.03 to 0.27, P = 0.12; I2 = 74%). Similarly, subgroup analysis did not show any statistical significance in the short-term, mid-term and long-term follow-up (Fig. 5).
Tegner Score
Twelve studies reported on Tegner score [10, 12, 17–20, 27, 29, 30, 34, 38, 39, 42]. Overall, no significant difference was found between DB and SB in terms of Tegner score (SMD = 0.03, 95% CI − 0.17 to 0.24, P = 0.74; I2 = 70%). Similarly, subgroup analysis showed similar results between the two groups in the short-term, mid-term, and long-term follow-up (Supplementary Fig. D).
IKDC Subjective Score
Twenty-two studies reported on IKDC subjective score [9–12, 17–22, 24–26, 28, 30–35, 37, 42, 43]. Both DB and SB had similar overall IKDC subjective score (SMD = 0.09, 95% CI − 0.04 to 0.22, P = 0.18; I2 = 78%). Subgroup analysis also showed similar results (Supplementary Fig. E).
IKDC Objective Scale
Eleven studies reported on IKDC objective scale [9, 11, 20, 25, 28, 31, 34, 37, 41, 46–49]. No significant different was found between BD and SB in terms of overall IKDC objective scale. (RR = 0.82, 95% CI 0.64 to 1.04, P = 0.19; I2 = 5%). Likewise, subgroup analysis did not show any statistical significance (Supplementary Fig. F).
Graft Failure
Eight studies reported on graft failure [11, 12, 17, 23, 29, 43, 46–49]. The analysis revealed no significant difference between DB and SB in terms of graft failure rate (RR = 0.78, 95% CI 0.33 to 1.85, P = 0.57; I2 = 54%) (Supplementary Fig. G).
Return to Pre-injury Sport Activity
Five studies reported on Return to pre-injury sports activity [11, 12, 17, 40, 43]. Both groups showed similar rate in terms of return to pre-injury sports activity (RR = 1.09, 95% CI 0.93 to 1.26, P = 0.26; I2 = 1%) (Supplementary Fig. H).
Discussion
This comprehensive systematic review and meta-analysis based on the highest level of evidence obtained from RCTs compared the short-term, mid-term, and long-term outcomes of anatomical SB and anatomical DB ACL reconstruction techniques. The analysis suggests no significant difference between DB and SB techniques in mid-term and long-term follow-up with regard to knee stability and functional outcomes. The analysis also suggests that graft failure and return to pre-injury sports activity rates to be similar in both groups.
Mascarenhas et al. in a systematic review showed that DB was better in terms of knee stability outcomes and functional outcomes compared to SB technique [50]. Similarly, few more recent reviews found better knee stability and functional outcomes associated with DB in the mid-term follow-up. However, participants who received DB or SB reported similar outcomes in the long-term follow-up [7, 8, 51].
Pivot shift test, Lachman test, and KT-1000/2000 knee arthrometer assess the efficacy of ACL reconstruction in restoring the biomechanical function of the knee. Our review showed a substantial improvement in rotational stability measured by pivot shift test, anterior stability measured by Lachman test and KT-1000/2000 knee arthrometer in favor of DB at short term, yet no difference was noted at mid-term and long-term follow-up. Similarly, a recent biomechanical systematic review found that DB was associated with better restoration of anterior knee stability compared to SB ACL reconstruction technique. However, the review found no difference between the two groups in terms of rotational stability [52].
Many reviews reported about graft failure rate which was consistently similar between DB and SB at short-term, mid-term, and long-term follow-up [7, 8, 51]. However, a recent RCT with 10 years follow-up revealed that DB has significantly less graft failure rate compared to SB [53]. Only one systematic review reported about return to pre-injury sports activity which was significantly better in favor of DB technique [54].
Knee Osteoarthritis (OA) progression is one of the most unfavorable complications following ACL injury and perhaps ACL reconstruction. DB was associated with a significant delay with respect to OA progression compared to SB at the mid-term follow-up [51]. However, both surgical techniques found to carry similar risk of developing knee OA at the long-term follow-up [8, 53]. This suggests that SB ACL reconstruction is associated with earlier clinical or radiological manifestations of OA compared to the DB technique, yet the rate of OA progression becomes similar at the long-term follow-up.
Our review provided a relatively large sample size obtained from well-conducted RCTs comparing the clinical outcomes of anatomical DB and SB ACL reconstruction. Furthermore, our review provided short-term, mid-term, and long-term follow-up data for the most commonly assessed knee stability and functional outcomes.
We acknowledge that our review has some limitations. First, we did not assess the risk of developing OA following ACL reconstruction through DB or SB due to the paucity of RCTs reporting this outcome. Second, few of the included RCTs were able to provide long-term follow-up data. So, caution should be taken when interpreting these results. Third, diversity in the graft type, fixation device, and method of femoral drilling across the enrolled papers was an inherent limitation of this systematic review.
Conclusion
Anatomical DB ACL reconstruction technique was superior and showed significantly better results than anatomical SB in terms of overall pivot shift test, Lachman test, and KT 1000/2000 arthrometer. No difference was found between the two surgical techniques in overall Lysholm score, Tegner score, IKDC subjective score, IKDC objective scale, graft failure rate, and return to pre-injury sports activity. DB and SB reconstruction techniques showed similar outcomes in the mid-term and long-term follow-up. Further RCTs are warranted comparing the risk of OA progression between the two surgical techniques in the long-term follow-up.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- DB:
-
Double bundle technique
- SB:
-
Single bundle technique
- RCT:
-
Randomized controlled trial
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- IKDC:
-
International Knee Documentation Committee score
- CENTRAL:
-
Cochrane Central Register of Controlled Trials
- SMD:
-
Standardized mean difference
- RR:
-
Risk ratio
- OA:
-
Osteoarthritis
References
Joseph, A. M., Collins, C. L., Henke, N. M., Yard, E. E., Fields, S. K., & Comstock, R. D. (2013). A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. Journal of Athletic Training, 48(6), 810–817.
Beynnon, B. D., Johnson, R. J., Abate, J. A., Fleming, B. C., & Nichols, C. E. (2005). Treatment of anterior cruciate ligament injuries, part I. The American Journal of Sports Medicine, 33(10), 1579–1602.
Beynnon, B. D., Johnson, R. J., Abate, J. A., Fleming, B. C., & Nichols, C. E. (2005). Treatment of anterior cruciate ligament injuries, part 2. The American Journal of Sports Medicine, 33(11), 1751–1767.
Xu, M., Gao, S., Zeng, C., Han, R., Sun, J., Li, H., Xiong, Y., & Lei, G. (2013). Outcomes of anterior cruciate ligament reconstruction using single-bundle versus double-bundle technique: meta-analysis of 19 randomized controlled trRials. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 29(2), 357–365.
Li, Y. L., Ning, G. Z., Wu, Q., Wu, Q. L., Li, Y., Hao, Y., & Feng, S. Q. (2014). Single-bundle or double-bundle for anterior cruciate ligament reconstruction: A meta-analysis. The Knee, 21(1), 28–37.
Li, X., Xu, C. P., Song, J. Q., Jiang, N., & Yu, B. (2013). Single-bundle versus double-bundle anterior cruciate ligament reconstruction: An up-to-date meta-analysis. International Orthopaedics, 37(2), 213–226.
Kong, L., Liu, Z., Meng, F., & Shen, Y. (2017). Single-bundle versus double-bundle anterior cruciate ligament reconstruction: A systematic review and meta-analysis. International Journal of Clinical and Experimental Medicine, 10(1), 1–5.
Chen, H., Chen, B., Tie, K., Fu, Z., & Chen, L. (2018). Single-bundle versus double-bundle autologous anterior cruciate ligament reconstruction: A meta-analysis of randomized controlled trials at 5-year minimum follow-up. Journal of Orthopaedic Surgery and Research, 13(1), 50.
Mayr, H. O., Bruder, S., Hube, R., Bernstein, A., Suedkamp, N. P., & Stoehr, A. (2018). Single-bundle versus double-bundle anterior cruciate ligament reconstruction—5-year results. Arthroscopy: The Journal of Arthroscopic and Related Surgery, 34(9), 2647–2653.
Sagar, J. V. (2019). A 5 year prospective double blind comparative study of ACL reconstruction using hamstring single bundle vs double bundle graft. International Journal of Orthopaedics, 5(4), 683–688.
Mohtadi, N. G., & Chan, D. S. (2019). A randomized clinical trial comparing Patellar tendon, hamstring tendon, and Double-Bundle ACL reconstructions: Patient-reported and clinical outcomes at 5-year follow-up. JBJS, 101(11), 949–960.
Liu, Y., Cui, G., Yan, H., Yang, Y., & Ao, Y. (2016). Comparison between single-and double-bundle anterior cruciate ligament reconstruction with 6-to 8-stranded hamstring autograft: A prospective, randomized clinical trial. The American Journal of Sports Medicine, 44(9), 2314–2322.
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Annals of Internal Medicine, 151, W-65-W-94.
Sterne, J. A. C., Savovic, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., et al. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ, 366, l4898.
Adachi, N., Ochi, M., Uchio, Y., Iwasa, J., Kuriwaka, M., & Ito, Y. (2004). Reconstruction of the anterior cruciate ligament: single-versus double-bundle multistranded hamstring tendons. The Journal of Bone and Joint Surgery. British Volume, 86(4), 515–520.
Adravanti, P., Dini, F., de Girolamo, L., Cattani, M., & Rosa, M. A. (2017). Single-bundle versus double-bundle anterior cruciate ligament reconstruction: A prospective randomized controlled trial with 6-year follow-up. The Journal of Knee Surgery, 30(09), 898–904.
Aga, C., Risberg, M. A., Fagerland, M. W., Johansen, S., Trøan, I., Heir, S., & Engebretsen, L. (2018). No difference in the KOOS quality of life subscore between anatomic double-bundle and anatomic single-bundle anterior cruciate ligament reconstruction of the knee: A prospective randomized controlled trial with 2 years’ follow-up. The American Journal of Sports Medicine, 46(10), 2341–2354.
Beyaz, S., Güler, Ü. Ö., Demir, Ş, Yüksel, S., Çınar, B. M., Özkoç, G., & Akpınar, S. (2017). Tunnel widening after single-versus double-bundle anterior cruciate ligament reconstruction: A randomized 8-year follow-up study. Archives of Orthopaedic and Trauma Surgery, 137(11), 1547–1555.
Claes, S., Neven, E., Callewaert, B., Desloovere, K., & Bellemans, J. (2011). Tibial rotation in single-and double-bundle ACL reconstruction: A kinematic 3-D in vivo analysis. Knee Surgery, Sports Traumatology, Arthroscopy, 19(1), 115–121.
Gobbi, A., Mahajan, V., Karnatzikos, G., & Nakamura, N. (2012). Single-versus double-bundle ACL reconstruction: is there any difference in stability and function at 3-year followup? Clinical Orthopaedics and Related Research®, 470(3), 824–834.
Hussein, M., van Eck, C. F., Cretnik, A., Dinevski, D., & Fu, F. H. (2012). Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3-to 5-year follow-up. The American Journal of Sports Medicine, 40(3), 512–520.
Kang, H. J., Wang, X. J., Wu, C. J., Cao, J. H., & Zheng, Z. M. (2015). Single-bundle modified patellar tendon versus double-bundle tibialis anterior allograft ACL reconstruction: A prospective randomized study. Knee Surgery, Sports Traumatology, Arthroscopy, 23(8), 2244–2249.
Koga, H., Muneta, T., Yagishita, K., Watanabe, T., Mochizuki, T., Horie, M., Nakamura, T., Otabe, K., & Sekiya, I. (2015). Mid-to long-term results of single-bundle versus double-bundle anterior cruciate ligament reconstruction: randomized controlled trial. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 31(1), 69–76.
Komzák, M., Hart, R., Feranec, M., Šmíd, P., & Kocová, R. (2018). In vivo knee rotational stability 2 years after double-bundle and anatomic single-bundle ACL reconstruction. European Journal of Trauma and Emergency Surgery, 44(1), 105–111.
Mayr, H. O., Benecke, P., Hoell, A., Schmitt-Sody, M., Bernstein, A., Suedkamp, N. P., & Stoehr, A. (2016). Single-bundle versus double-bundle anterior cruciate ligament reconstruction: a comparative 2-year follow-up. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 32(1), 34–42.
Núñez, M., Sastre, S., Núñez, E., Lozano, L., Nicodemo, C., & Segur, J. M. (2012). Health-related quality of life and direct costs in patients with anterior cruciate ligament injury: single-bundle versus double-bundle reconstruction in a low-demand cohort—a randomized trial with 2 years of follow-up. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 28(7), 929–935.
Sasaki, S., Tsuda, E., Hiraga, Y., Yamamoto, Y., Maeda, S., Sasaki, E., & Ishibashi, Y. (2016). Prospective randomized study of objective and subjective clinical results between double-bundle and single-bundle anterior cruciate ligament reconstruction. The American Journal of Sports Medicine, 44(4), 855–864.
Siebold, R., Dehler, C., & Ellert, T. (2008). Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 24(2), 137–145.
Song, E. K., Seon, J. K., Yim, J. H., Woo, S. H., Seo, H. Y., & Lee, K. B. (2013). Progression of osteoarthritis after double-and single-bundle anterior cruciate ligament reconstruction. The American journal of sports medicine, 41(10), 2340–2346.
Streich, N. A., Friedrich, K., Gotterbarm, T., & Schmitt, H. (2008). Reconstruction of the ACL with a semitendinosus tendon graft: A prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes. Knee Surgery, Sports Traumatology, Arthroscopy, 16(3), 232–238.
Sun, R., Chen, B. C., Wang, F., Wang, X. F., & Chen, J. Q. (2015). Prospective randomized comparison of knee stability and joint degeneration for double-and single-bundle ACL reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy, 23(4), 1171–1178.
Ventura, A., Iori, S., Legnani, C., Terzaghi, C., Borgo, E., & Albisetti, W. (2013). Single-bundle versus double-bundle anterior cruciate ligament reconstruction: assessment with vertical jump test. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 29(7), 1201–1210.
Xu, Y., Ao, Y. F., Wang, J. Q., & Cui, G. Q. (2014). Prospective randomized comparison of anatomic single-and double-bundle anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy, 22(2), 308–316.
Zhang, Q., Yang, Y., Li, J., Zhang, H., Fu, Y., & Wang, Y. (2019). Functional double-bundle anterior cruciate ligament reconstruction using hamstring tendon autografts with preserved insertions is an effective treatment for tibiofemoral instability. Knee Surgery, Sports Traumatology, Arthroscopy, 27(11), 3471–3480.
Morey, V. M., Nag, H. L., Chowdhury, B., Sankineani, S. R., & Naranje, S. M. (2015). A prospective comparative study of clinical and functional outcomes between anatomic double bundle and single bundle hamstring grafts for arthroscopic anterior cruciate ligament reconstruction. International Journal of Surgery, 1(21), 162–167.
Araki, D., Kuroda, R., Kubo, S., Fujita, N., Tei, K., Nishimoto, K., Hoshino, Y., Matsushita, T., Matsumoto, T., Nagamune, K., & Kurosaka, M. (2011). A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: Quantitative evaluation using an electromagnetic measurement system. International Orthopaedics, 35(3), 439–446.
Devgan, A., Rohilla, R., Singh, A., Tanwar, M., Devgan, R., & Siwach, K. (2016). A prospective study to evaluate the clinico-radiological outcomes of arthroscopic single bundle versus double bundle anterior cruciate ligament reconstruction. Journal of clinical Orthopaedics and Trauma, 1(7), 236–242.
Ahldén, M., Sernert, N., Karlsson, J., & Kartus, J. (2013). A prospective randomized study comparing double-and single-bundle techniques for anterior cruciate ligament reconstruction. The American Journal of Sports Medicine, 41(11), 2484–2491.
Karikis, I., Desai, N., Sernert, N., Rostgard-Christensen, L., & Kartus, J. (2016). Comparison of anatomic double-and single-bundle techniques for anterior cruciate ligament reconstruction using hamstring tendon autografts: A prospective randomized study with 5-year clinical and radiographic follow-up. The American Journal of Sports Medicine, 44(5), 1225–1236.
Muneta, T., Koga, H., Mochizuki, T., Ju, Y. J., Hara, K., Nimura, A., Yagishita, K., & Sekiya, I. (2007). A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 23(6), 618–628.
Ibrahim, S. A., Hamido, F., Al Misfer, A. K., Mahgoob, A., Ghafar, S. A., & Alhran, H. (2009). Anterior cruciate ligament reconstruction using autologous hamstring double bundle graft compared with single bundle procedures. The Journal of Bone and Joint Surgery. British Volume, 91(10), 1310–1315.
Wang, J. Q., Ao, Y. F., Yu, C. L., Ping, L. I., Yan, X. U., & Chen, L. X. (2009). Clinical evaluation of double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: A prospective, randomized and controlled study. Chinese Medical Journal, 122(6), 706–711.
Aglietti, P., Giron, F., Losco, M., Cuomo, P., Ciardullo, A., & Mondanelli, N. (2010). Comparison between single-and double-bundle anterior cruciate ligament reconstruction: A prospective, randomized, single-blinded clinical trial. The American Journal of Sports Medicine, 38(1), 25–34.
Yagi, M., Kuroda, R., Nagamune, K., Yoshiya, S., & Kurosaka, M. (2007). Double-bundle ACL reconstruction can improve rotational stability. Clinical Orthopaedics and Related Research®, 454, 100–107.
Fujita, N., Kuroda, R., Matsumoto, T., Yamaguchi, M., Yagi, M., Matsumoto, A., Kubo, S., Matsushita, T., Hoshino, Y., Nishimoto, K., & Araki, D. (2011). Comparison of the clinical outcome of double-bundle, anteromedial single-bundle, and posterolateral single-bundle anterior cruciate ligament reconstruction using hamstring tendon graft with minimum 2-year follow-up. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 27(7), 906–913.
Järvelä, T. (2007). Double-bundle versus single-bundle anterior cruciate ligament reconstruction: A prospective, randomize clinical study. Knee Surgery, Sports Traumatology, Arthroscopy, 15(5), 500–507.
Suomalainen, P., Moisala, A. S., Paakkala, A., Kannus, P., & Järvelä, T. (2011). Double-bundle versus single-bundle anterior cruciate ligament reconstruction: Randomized clinical and magnetic resonance imaging study with 2-year follow-up. The American Journal of Sports Medicine, 39(8), 1615–1623.
Järvelä, T., Moisala, A. S., Sihvonen, R., Järvelä, S., Kannus, P., & Järvinen, M. (2008). Double-bundle anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference screw fixation: Prospective, randomized, clinical study with 2-year results. The American Journal of Sports Medicine, 36(2), 290–297.
Suomalainen, P., Järvelä, T., Paakkala, A., Kannus, P., & Järvinen, M. (2012). Double-bundle versus single-bundle anterior cruciate ligament reconstruction: A prospective randomized study with 5-year results. The American Journal of Sports Medicine, 40(7), 1511–1518.
Mascarenhas, R., Cvetanovich, G. L., Sayegh, E. T., Verma, N. N., Cole, B. J., Bush-Joseph, C., & Bach, B. R., Jr. (2015). Does double-bundle anterior cruciate ligament reconstruction improve postoperative knee stability compared with single-bundle techniques? A systematic review of overlapping meta-analyses. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 31(6), 1185–1196.
Chen, G., & Wang, S. (2015). Comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction after a minimum of 3-year follow-up: A meta-analysis of randomized controlled trials. International Journal of Clinical and Experimental Medicine, 8(9), 14604.
Oh, J. Y., Kim, K. T., Park, Y. J., Won, H. C., Yoo, J. I., Moon, D. K., Cho, S. H., & Hwang, S. C. (2020). Biomechanical comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction: A meta-analysis. Knee Surgery & Related Research, 32(1), 1–1.
Järvelä, S., Kiekara, T., Suomalainen, P., & Järvelä, T. (2017). Double-bundle versus single-bundle anterior cruciate ligament reconstruction: A prospective randomized study with 10-year results. The American Journal of Sports Medicine, 45(11), 2578–2585.
Tiamklang, T., Sumanont, S., Foocharoen, T., & Laopaiboon, M. (2012). Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database of Systematic Reviews, 11(11), CD008413. https://doi.org/10.1002/14651858.CD008413.pub2.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alomari, M.S., Ghaddaf, A.A., Abdulhamid, A.S. et al. Single Bundle Versus Double Bundle Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. JOIO 56, 1669–1684 (2022). https://doi.org/10.1007/s43465-022-00718-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-022-00718-0