Abstract
Objective
The purpose of this study was to compare the single-bundle (SB) and double-bundle (DB) surgical techniques for anterior cruciate ligament (ACL) reconstruction with regard to tunnel widening, isokinetic muscle strength, and clinical outcomes over an 8-year follow-up period.
Methods
This study included 31 patients with ACL injury who underwent ACL reconstruction via the SB (n = 16) or the DB (n = 15) technique. Isokinetic and concentric strength measurements of the quadriceps and hamstring muscles were conducted at postoperative 6 months and postoperative 8 years, and 3D-CT scans of the knee joints were performed on the 2nd, 3rd and 6th month, and the 8th year postoperatively. Clinical evaluations were performed at 8 years postoperatively with the International Knee Documentation Committee (IKDC), Tegner, and Lysholm knee scoring systems.
Results
There was marked widening of the parts of the femoral tunnel close to the knee joint in both the SD and the DB groups. There was no difference between the two groups in terms of clinical results and isometric muscle strength at postoperative 8 years; however, there was a significant difference between the preoperative and 6 months postoperative clinical and strength results in both group (P < 0.05). There was no difference between the groups in IKDC score, Lysholm score, Tegner activity scale, and anterior drawer test at postoperative 8 years. On evaluation of the anteromedial bundles alone, the DB group had greater widening than the SB group.
Conclusion
In this study, we have found that the tunnels continue to enlarge after 6 months. However, that has no impact in patients comfort and that did not made any change in our daily routine. On the other hand, we found that the reconstruction of the double-band ligament technique is useless for non-professional athletes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tunnel widening in anterior cruciate ligament (ACL) reconstruction surgery was introduced more than 25 years ago [18]. Previous studies indicate that tunnel widening could lead to inability of the graft to incorporate, long-term joint laxity, and failure in terms of revision surgery requirement and high costs [7, 8, 12]. There has been an increase in ACL surgery of more than 30% in the last two decades, which has led to an increase in ACL surgery-related complications [3].
The clinical effectiveness of double-bundle (DB) ACL reconstruction surgery in which there are two tunnels is controversial [4, 5, 20]. The increase in the number of tunnels reportedly enables a more stable and more anatomic reconstruction rotationally [19, 20]. However, this also results in surgery that is more complicated, longer, more difficult, and causes a greater reduction in bone stock. Difficult revision cases may be encountered due to the greater degree of bone loss when obtaining a more stable ligament [10, 30]. Although previous studies indicate that tunnel widening develops in the early postoperative period or even intraoperatively, no study has yet compared the SB and the DB techniques in the long term [7, 10, 30].
The aim of our study was to make a randomized, prospective comparison of the DB and the SB techniques with regard to tunnel widening, isokinetic muscle strength, and clinical outcomes. These parameters have previously been compared in the short-term [3]; however, our study has the longest follow-up period.
Methods
This study was approved by Başkent University Institutional Review Board and Ethics Committee (Project No: KA15/44) and was supported by the Başkent University Research Fund (Project No: 54462418).
This study included patients who underwent ACL reconstruction surgery via the DB (n = 16) or the SB (n = 18) technique between November 2007 and March 2008, who had participated as described previously [3]. Patients who did not have lower limb bone fractures who had not undergone previous lower extremity surgery and whose other knee examination was normal were included the study. Our previous study included 40 patients with unilateral ACL injury with no systemic disease who agreed to participate. We excluded one patient who had a history of previous knee surgery, two patients who were treated for lower extremity fracture, one patient who had postoperative infection, and five patients who were lost to follow-up. The reconstruction method was decided preoperatively in our first study. We generated an unpredictable random sequence where the first patient was assigned to a treatment group based on a coin toss, and the next patient was then assigned to the other treatment group to achieve a balanced number of patients in both groups. We implemented the sequence in a way that concealed the treatments until the patients were formally assigned to their groups.
Two patients who underwent SB surgery were excluded as they did not agree to participation, and one patient from the SB group was excluded as he underwent ACL reconstruction for another knee in another center. A total of 31 male patients were included, of whom 16 underwent DB surgery (mean age 38.2 years; range 28–48 years) and 15 underwent SB surgery (mean age 35.1 years; range 27–43 years). All the patients were male. This is not by purpose. It is because the demographics of our ACL torn patients. Twenty-seven patients had experienced trauma on a synthetic pitch, three patients had experienced sprain when running, and one experienced trauma during a professional sports activity. Demographics data and characteristics of patients are given in Table 1.
Ethics committee approval was obtained twice (once in 2007 and once in 2015) from Başkent University Medical School. The patients were informed in detail in the presence of witnesses about the aim of the study, expected benefits, amount and effects of radiation they would receive during computed tomography (CT) examination, and the measures taken to protect patients. Informed consent was obtained from patients in 2007 and 2015. Transfer and accommodation costs of four patients who travelled to participate in the study were paid for by a university fund. The patients were not paid.
Surgery
The patients were not informed about which surgical procedure they would undergo. Mean duration between trauma and surgery was 2 months and 19 days (range 3 weeks–18 months) in the SB group, and 2 months and 14 days (range 4 weeks–14 months) in the DB group. Twenty-eight patients were given combination anaesthesia (spinal epidural) and three patients were given general anaesthesia.
In the single-bundle method, the ACL was aligned in the middle of the tibial tunnel exit. The femoral tunnel was opened at 1:30 to 2:00 on the left knee lateral femoral condyle. The semitendinosus and gracilis tendons were doubled and their thickness was measured. Femoral fixation was performed using the EndoButton (Smith & Nephew, Inc., Andover, MA, USA) technique. Tibial fixation was performed using a biodegradable poly(l-lactide)-hydroxyapatite screw (BioRCI; Smith & Nephew, Inc., Andover, MA, USA) and staple.
In the dual-bundle method, a 5 cm oblique incision was made 2 cm below and medial to the tibial tuberosity to harvest gracilis and semitendinosus tendons. The thickness of each doubled tendon was separately measured. For the anteromedial band (AMB), the tibial tunnel was placed at 45° in the sagittal plane and tibia tuberosity to keep as close as possible. For the posterolateral band (PLB), placement was at 45° in the sagittal plane. To keep the tunnels from each other, they were replaced closely to the medial collateral bond. Average distance between the tunnels was between 1.5 and 2 cm. The tibial guide wire placed for the AMB was taken out from the tibial attachment of ACL, approximately 13 mm in front of the anterior corner of the posterior cruciate ligament. The PLB guide wire was taken out approximately 7 mm posterior and lateral to the AMB guide wire. The tunnel was opened with a cannulated drill to the same diameter as the graft. After identification of the femoral insertion site of the ligaments, the knees were placed at 120° and in contrast to the transtibial technique, both guide wires were inserted through the anteromedial portal. Other than the classical clock orientation method, insertions were made at the anatomical attachment site of the tendons accord- ing to soft tissue remnants and bony landmarks as described by Ferretti et al. [9]. By sizing the length of the EndoButton CL, which uses in the total length of the tunnel, the tunnel’s length was found where the graft sat on the femur. Grafts were advanced separately through the EndoButton CL ring (Smith & Nephew, Inc., Andover, MA, USA) and doubled. AMB was opened at the lateral femoral condyle at 1:00 to 2:00 on the left and at 3:00 for PLB. First the PLB, then the AMB EndoButtons were stabilized through the tunnel. Poly(l-lactide)-hydroxyapatite biodegradable screw BioRCI and staple were used for tibial fixation.
A compressive bandage was applied following surgery. Patients who underwent meniscal repair were allowed to mobilize with an extension brace and weight-bearing. Passive ranges of motion (ROM) exercises were started on the first postoperative day. On the second postoperative day, passive ROM was increased and a rehabilitation programme of quadriceps strengthening exercises was added. Rehabilitation programs were not different for patients who underwent single- and dual-bundle reconstruction. Patients were allowed to run in the third postoperative month when 60% muscle strength was obtained. In the 6th month, patients were allowed to participate in competitive sport when quadriceps power reached 80%.
Radiologic examination
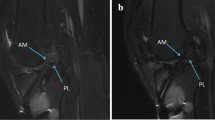
Knee CT was conducted at postoperative 2, 3, and 6 months, and at postoperative 8 years, and three-dimensional reconstruction was done (GE Optima 580, General Electric, USA). The examination technique allowed analysis 12 cm proximal and 10 cm distal to the knee joint line, reconstruction with 2-mm intervals, and produced relatively low levels of radiation. The patients were covered with a lead apron with only the knees exposed. Radiation dose for each examination was confirmed to be less than 1 mSv, which is much lower than the dose given in a normal lung CT (7 mSv) and the yearly effective dose (approximately 3 mSv) [27]. Measurements were done in the sagittal, coronal, and axial planes by the same radiologist using code numbers instead of patient names. CT slices were divided into six equal parts marking the distance between the femoral and tibial tunnels, with the most distal part of the knee joint designated as L1, and the entry-point on the knee joint as L6 (Fig. 1). The tunnel length was measured in mm perpendicular to the tibial axis in the sagittal and coronal planes (HP xw8400; Hewlett-Packard Company, Palo Alto, CA, USA). The tunnel cross-sectional area was measured with the same device on axial reconstructions.
Isokinetic muscle strength measurement
Isokinetic and concentric muscle strength measurements of the quadriceps and hamstrings were done for both knees at 60°, 120°, and 180°/s angular speeds using a Biodex 3 device (Biodex Biomedical Systems Inc., Shirley, NY, USA) preoperatively, at 6 months postoperatively, and at 8 years postoperative for each patient. Peak torque (PT) and peak torque/bodyweight ratios (PT/BW) were recorded.
Clinical evaluation at postoperative 8 years
Lysholm scoring, Tegner activity scale, subjective International Knee Documentation Committee (IKDC) scoring, lachman and anterior drawer tests were done. Anterior laxity of both knees was examined by applying the anterior drawer test when the femur was at 45° and the knee was at 90° flexion, with the patient lying in a flat position. Same physician made all of the tests.
Statistical analysis
In accordance with the shape of the dataset of variables, the multiple imputation method was used to impute missing values in this longitudinal dataset. Library “mice” in R software was used for multiple imputation. The multiple imputation method was to replace each missing item with two or more acceptable values, representing a distribution of possibilities. The shapes of the datasets taken from the results of the Biodex, posterolateral (PL) bundles and anteromedial (AM) bundles, were quadratic through the timepoints of baseline, postoperative 6 months, and postoperative 8 years, and at 60°, 120°, and 180°/s. After imputation, three-way mixed ANOVA was used to evaluate the variation of measures within timepoints, degrees, and bands in Biodex result sets; ANOVA was used to evaluate the variation of measures within timepoints in PL bundle sets; and two-way mixed ANOVA was used to evaluate the variation of measures within timepoints and bands in AM bundle sets. For Biodex results, time and degree effects were taken as within-subject effects, and band effect was taken as a between-subject effect; for AM bundles, time effect was taken as a within-subject effect, and band effect was taken as a between-subject effect. To compare the SB and DB groups according to patient characteristics, the t test or Mann–Whitney U test was used to test the distribution of continuous variables. Distribution of variables was tested for normality by the Shapiro–Wilk test. Type-I error rate was taken as α = 0.05 for statistical significance. R software was used for statistical analyses.
Results
Tunnel widening
All results are given in Table 2. Although significant widening was not detected at postoperative months 2, 3, and 6 in patients who underwent SB surgery, significant widening was detected in the femoral and tibial sides when these data were compared with the results at postoperative 8 years. Widening occurred after the 6th postoperative month in DB surgery, similarly to SB surgery. Widening was significantly greater at the beginning and termination points (L1 and L6) (P < 0.05). For the femoral side, significant differences were found in the following regions: sagittal 1, 2, and 6, coronal 1, 5, and 6, and all six axial views in the SB group; sagittal 1 and 2, coronal 1, 2, and 6, and axial 1, 2, 5, and 6 in the AM bundle in the DB group; sagittal 3, coronal 1, and axial 1 and 4 in the PL bundle in the DB group. For the tibial side, significant differences were found in the following regions: sagittal 1, and axial 1, 2, 5, and 6 in the SB group; sagittal 1, 5, and 6, coronal 1 and 5, and axial 2, 3, 4, 5, and 6 in the AM bundle in the DB group; sagittal 3, and axial 4, 5, and 6 in the PL bundle in the DB group.
Isokinetic muscle strength
While there was no significant difference detected between the isokinetic muscle strength of the hamstrings and the quadriceps measured at 60°, 120°, and 180°/s angular velocities in patients who underwent SB and DB reconstruction (P < 0.05), all of the studied muscles strength were significantly better at postoperative 8 years than preoperatively (P < 0.05). The same comparison was made at postoperative 8 years between the SB and DB, and there was no significant difference between the two groups (P = 0.561 for PT quadriceps; P = 0.725 for PT hamstrings; P = 0.354 for PT/BW quadriceps, and P = 0.613 for PT/BW hamstrings; Table 3).
Clinical outcomes
There was no significant difference between groups at postoperative 8 years with regard to Lysholm score (P = 0.841), Tegner activity scale (P = 0.925), and IKDC score (P = 0.864; Table 4). There was no significant difference in the pre- and post-operative Tegner scores in either group (P > 0.05). Pain that increased with activity, but did not affect daily life was detected in the medial joint space in five patients in the SB group and seven patients in the DB group; all of these patients had osteophytes detected in the medial tibial plateau.
Discussion
The primary purpose of our study was to compare tunnel widening in the long term between SB and DB ACL reconstruction techniques, and to investigate the influence of widening on isokinetic muscle strength and clinical outcomes. In our study, a significant difference was not detected in isokinetic muscle strength at all angles evaluated preoperatively compared with 6 months postoperatively. However, the patients had much better muscle strength when these preoperative measurements were compared with the measurements at postoperative 8 years. There was no significant difference between the two groups with regard to IKDC score, Tegner activity scale, and Lysholm score obtained at postoperative 8 years, which indicates that there was no difference between the two techniques with regard to clinical findings and isokinetic muscle strength.
It was suggested that tunnel widening in ACL reconstruction arose from chemical and biomechanical factors. Biological factors include cytokines and chemical mediators in joint fluid, graft selection, bone quality, and cellular necrosis during tunnel opening [1, 6, 8, 32, 34]. The main mechanical factors include micromovement of the graft in the coronal and sagittal planes [36]. Synovial fluid entering the dead space between the graft and bone is suggested to contribute to abrasion through the wiper interface effect [10]. Other mechanical environmental factors include graft position, graft tension, fixation method, and aggressive rehabilitation [2, 13, 17, 33]. The PL bundle, which is not involved in SB surgery, is suggested to cause insufficiency in control of the combined rotator load and valgus torque that simulates the pivot-shift test [21, 37]. Human cadaver studies showed that PL bundle is required more in anterior tibial and rotator loadings when the knee is in full extension [11, 24]. Although some studies report more anatomic and more successful outcomes with DB ACL reconstruction [23, 28], other studies report no significant difference between SB and DB techniques with regard to biomechanical [15] and clinical outcome [3, 26]. Hence, the clinical success of DB surgery that is theoretically more anatomic is still controversial [25].
Kiekara et al. [22] reported that the tunnels joined 10% in the femur and 27% in the tibia; however, this conjugation did not have an effect on laxity in 2 years of follow-up in 59 patients who underwent DB surgery. Weber et al. [35] used MRI to follow-up patients who underwent SB surgery for 2 years, and found that widening was most common on the tibial side; potential risks for tunnel widening were young age, male sex, and prolonged duration between trauma and surgery. Widening at the L6 point in the present study is in conjunction with these previous results [35]. Our study also showed a widening at the suspensory fixation device location and at the entry-point of the tibial tunnel. When AM bundles were compared in both groups without considering the PL bundle, greater widening was detected at more points and in more sections in the DB group. The reason for this may be thinner graft diameter or greater oscillation.
Measurement results and CT imaging showed that the tunnels did not have a completely cylindric structure. The tunnel became balloon-shaped along with the biodegradable screw, particularly at the tibial side, and narrowed again at the L4 and L5 sections where the screw ended. The similar shape of the tunnel in all patients and detection of these images also on CT at postoperative 2 months suggests that this effect developed intraoperatively. These findings support the hypothesis of Siebold et al. [31] that widening occurs during the operation. We consider that widening occurred at the beginning and termination points of the tunnels in the axial plane and not at the tibial side in the sagittal and coronal planes in patients who underwent SB surgery because the sections are perpendicular to the movement axis. The widening at the joint entry-point may be related to the oscillation movement of the graft, and the widening at the tunnel entry-point may be related to the chemical mediators that are formed during dissolution of the biodegradable screw.
Hamstring grafts are placed to the each tunnel by folding two in DB surgery. A thicker, more durable, more stable ACL reconstruction is obtained in SB surgery as both tendons are passed through a single tunnel. In contrast, tendons are passed through separate tunnels in DB surgery, and a weaker AM bundle is obtained. Considering that the main load is carried by the AM bundle, although the ACL has two bundles, greater widening in the AM bundle in our study may have occurred because it is a more stable and more mobile bundle [29].
Widening points in the PL bundle are lesser compared with those in the AM bundle. Cadaver studies indicate that the PL bundle plays a role in the activities performed by professional sportsmen including downhill running and sudden change of direction [29]. None of our patients were professional sportsmen. The patients whose activity level decreased after trauma did not increase their activity level at postoperative 6 months, or postoperative 8 years. One patient in each group performed sports for 2–3 h/week as hobby. This could have decreased the need for the PL bundle, and led to less oscillation and less widening.
Joining was detected in L6 tunnels on the tibial side in 10 patients who underwent DB reconstruction. Although two of these cases occurred during the first 6 months, eight newly detected cases of joining occurred between 6 months and 8 years postoperatively. In the literature, widening after DB surgery reportedly causes problems in revision surgery [14, 16]. However, none of the patients in the present study required revision surgery. The reason for this may be that our patients did not participate in physically demanding sports or that the duration between trauma and surgery may have been longer compared with the group that did not show joining.
A limitation of our study was the small number of patients. Further studies that include larger numbers of patients and professional sportsmen are warranted. It would also be beneficial to perform CT on postoperative day 1 and to objectively evaluate anterior displacement using a KT-1000 device.
Conclusion
In this study, we have found that the tunnels continue to enlarge after 6 months. However, that has no impact in patients comfort and that did not made any change in our daily routine. On the other hand, we found that the reconstruction of the double-band ligament technique is useless for non-professional athletes.
References
Amiel D, Kleiner JB, Akeson WH (1986) The natural history of the anterior cruciate ligament autograft of patellar tendon origin. Am J Sports Med 14(6):449–462
Baumfeld JA, Diduch DR, Rubino LJ et al (2008) Tunnel widening following anterior cruciate ligament reconstruction using hamstring autograft: a comparison between double cross-pin and suspensory graft fixation. Knee Surg Sports Traumatol Arthrosc 16(12):1108–1113
Beyaz S, Ozkoc G, Akpinar S, Demir S, Adam M, Tuncay IC (2012) Comparison of tunnel expansion and isometric muscle strength after ACL reconstruction with single- or dual-bundle hamstring allograft: a prospective, randomized study. Acta Orthop Traumatol Turc 46(5):353–360
Bjornsson H, Desai N, Musahl V et al (2015) Is double-bundle anterior cruciate ligament reconstruction superior to single-bundle? A comprehensive systematic review. Knee Surg Sports Traumatol Arthrosc 23(3):696–739
Chen G, Wang S (2015) Comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction after a minimum of 3-year follow-up: a meta-analysis of randomized controlled trials. Int J Clin Exp Med 8(9):14604–14614
Clancy WG Jr, Narechania RG, Rosenberg TD, Gmeiner JG, Wisnefske DD, Lange TA (1981) Anterior and posterior cruciate ligament reconstruction in rhesus monkeys. J Bone Jt Surg 63(8):1270–1284
Clatworthy MG, Annear P, Bulow JU, Bartlett RJ (1999) Tunnel widening in anterior cruciate ligament reconstruction: a prospective evaluation of hamstring and patella tendon grafts. Knee Surg Sports Traumatol Arthrosc 7(3):138–145
Fahey M, Indelicato PA (1994) Bone tunnel enlargement after anterior cruciate ligament replacement. Am J Sports Med 22(3):410–414
Ferretti M, Ekdahl M, Shen W, Fu FH (2007) Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthrosc J Arthrosc Relat Surg 23(11):1218–1225
Fink C, Zapp M, Benedetto KP, Hackl W, Hoser C, Rieger M (2001) Tibial tunnel enlargement following anterior cruciate ligament reconstruction with patellar tendon autograft. Arthrosc J Arthrosc Relat Surg 17(2):138–143
Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE (2004) Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res 22(1):85–89
Getelman MH, Friedman MJ (1999) Revision anterior cruciate ligament reconstruction surgery. J Am Acad Orthop Surg 7(3):189–198
Hantes ME, Mastrokalos DS, Yu J, Paessler HH (2004) The effect of early motion on tibial tunnel widening after anterior cruciate ligament replacement using hamstring tendon grafts. Arthrosc J Arthrosc Relat Surg 20(6):572–580
Harner CD, Poehling GG (2004) Double bundle or double trouble? Arthrosc J Arthrosc Relat Surg 20(10):1013–1014
Herbort M, Domnick C, Raschke MJ et al (2015) Comparison of knee kinematics after single-bundle anterior cruciate ligament reconstruction via the medial portal technique with a central femoral tunnel and an eccentric femoral tunnel and after anatomic double-bundle reconstruction: a human cadaveric study. Am J Sports Med 44(1):126–132
Hofbauer M, Muller B, Murawski CD, Baraga M, van Eck CF, Fu FH (2013) Strategies for revision surgery after primary double-bundle anterior cruciate ligament (ACL) reconstruction. Knee Surg Sports Traumatol Arthrosc 21(9):2072–2080
Hoher J, Livesay GA, Ma CB, Withrow JD, Fu FH, Woo SL (1999) Hamstring graft motion in the femoral bone tunnel when using titanium button/polyester tape fixation. Knee Surg Sports Traumatol Arthrosc 7(4):215–219
Hoher J, Moller HD, Fu FH (1998) Bone tunnel enlargement after anterior cruciate ligament reconstruction: fact or fiction? Knee Surg Sports Traumatol Arthrosc 6(4):231–240
Jain V, Goyal A, Mohindra M, Kumar R, Joshi D, Chaudhary D (2016) A comparative analysis of arthroscopic double-bundle versus single-bundle posterior cruciate ligament reconstruction using hamstring tendon autograft. Arch Orthop Trauma Surg 136(11):1555–1561
Jarvela T, Moisala AS, Paakkala T, Paakkala A (2008) Tunnel enlargement after double-bundle anterior cruciate ligament reconstruction: a prospective, randomized study. Arthrosc J Arthrosc Relat Surg 24(12):1349–1357
Kanamori A, Zeminski J, Rudy TW, Li G, Fu FH, Woo SL (2002) The effect of axial tibial torque on the function of the anterior cruciate ligament: a biomechanical study of a simulated pivot shift test. Arthrosc J Arthrosc Relat Surg 18(4):394–398
Kiekara T, Jarvela T, Huhtala H, Moisala AS, Suomalainen P, Paakkala A (2014) Tunnel communication and increased graft signal intensity on magnetic resonance imaging of double-bundle anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg 30(12):1595–1601
Koga H, Muneta T, Yagishita K et al (2015) Mid- to long-term results of single-bundle versus double-bundle anterior cruciate ligament reconstruction: randomized controlled trial. Arthrosc J Arthrosc Relat Surg 31(1):69–76
Mae T, Shino K, Miyama T et al (2001) Single- versus two-femoral socket anterior cruciate ligament reconstruction technique: biomechanical analysis using a robotic simulator. Arthrosc J Arthrosc Relat Surg 17(7):708–716
Mascarenhas R, Cvetanovich GL, Sayegh ET et al (2015) Does double-bundle anterior cruciate ligament reconstruction improve postoperative knee stability compared with single-bundle techniques? A systematic review of overlapping meta-analyses. Arthrosc J Arthrosc Relat Surg 31(6):1185–1196
Mayr HO, Benecke P, Hoell A et al (2015) Single-bundle versus double-bundle anterior cruciate ligament reconstruction: a comparative 2-year follow-up. Arthrosc J Arthrosc Relat Surg 32(1):34–42
Mettler FA Jr, Huda W, Yoshizumi TT, Mahesh M (2008) Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology 248(1):254–263
Morey VM, Nag HL, Chowdhury B, Sankineani SR, Naranje SM (2015) A prospective comparative study of clinical and functional outcomes between anatomic double bundle and single bundle hamstring grafts for arthroscopic anterior cruciate ligament reconstruction. Int J Surg 21:162–167
Petersen W, Zantop T (2007) Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res 454:35–47
Siebold R (2007) Observations on bone tunnel enlargement after double-bundle anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg 23(3):291–298
Siebold R, Cafaltzis K (2010) Differentiation between intraoperative and postoperative bone tunnel widening and communication in double-bundle anterior cruciate ligament reconstruction: a prospective study. Arthrosc J Arthrosc Relat Surg 26(8):1066–1073
Silva A, Sampaio R, Pinto E (2010) Femoral tunnel enlargement after anatomic ACL reconstruction: a biological problem? Knee Surg Sports Traumatol Arthrosc 18(9):1189–1194
Tomihara T, Hashimoto Y, Taniuchi M, Shimada N (2015) Relationship between femoral tunnel location and graft bending angle in outside-in and transportal technique for ACL double bundle reconstruction in 3D-CT study. Arch Orthop Trauma Surg 135(6):839–846
Vergis A, Gillquist J (1995) Graft failure in intra-articular anterior cruciate ligament reconstructions: a review of the literature. Arthrosc J Arthrosc Relat Surg 11(3):312–321
Weber AE, Delos D, Oltean HN et al (2015) Tibial and femoral tunnel changes after ACL reconstruction: a prospective 2-year longitudinal MRI Study. Am J Sports Med 43(5):1147–1156
Wilson TC, Kantaras A, Atay A, Johnson DL (2004) Tunnel enlargement after anterior cruciate ligament surgery. Am J Sports Med 32(2):543–549
Woo SL, Kanamori A, Zeminski J, Yagi M, Papageorgiou C, Fu FH (2002) The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon. A cadaveric study comparing anterior tibial and rotational loads. J Bone Jt Surg 84-A(6):907–914
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the Başkent University Research Fund.
Conflict of interest
All authors declare they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Beyaz, S., Güler, Ü.Ö., Demir, Ş. et al. Tunnel widening after single- versus double-bundle anterior cruciate ligament reconstruction: a randomized 8-year follow-up study. Arch Orthop Trauma Surg 137, 1547–1555 (2017). https://doi.org/10.1007/s00402-017-2774-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2774-z