Abstract
Purpose
The objective of this study was to evaluate knee rotational stability at least 2 years after anatomic single-bundle anterior cruciate ligament (ACL) reconstruction (SB) and double-bundle ACL reconstruction (DB) in comparison with the contralateral healthy knee joint. The Cincinnati, Lysholm and IKDC scores were analysed too.
Methods
There were 40 patients in both groups, the mean follow-up was 27 months. For all measurements, the navigation system OrthoPilot was used. Measurement started with the patient in the standing position in neutral rotation. Then, the patient achieved in 30° knee flexion under weight-bearing maximal external trunk rotation and returned to the neutral position. The same measurement was done for the internal trunk rotation. For the anterior–posterior stability, KT-1000 arthrometer was used. All measurements were repeated three times for each knee joint.
Results
After the DB reconstruction, the mean external rotation of the tibia (ER) was 8.2° and the internal rotation (IR) was 10.2°. In the contralateral healthy knee joint, ER was 8.5° (p = 0.597) and IR was 12.1° (p = 0.064). After the SB reconstruction, ER was 9.4° and IR was 13.1°. In the contralateral healthy knee joint, ER was 7.7° (p = 0.066) and IR was 9.8° (p = 0.005). Anterior–posterior translation was to the same extent for both groups.
Conclusions
The DB reconstruction of the ACL restores the rotational stability of the knee joint without any significant difference in comparison to the contralateral healthy knee (p > 0.05). The main finding of this study is that the internal rotational stability of the knee joint after the anatomic SB technique is not sufficient.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
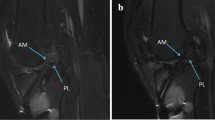
While there is a common understanding of the histological and anatomical structure of the anterior cruciate ligament (ACL), the question of the biomechanical function of its parts (anteromedial—AM and posterolateral—PL bundle) still represents a significant challenge for orthopaedic surgeons and medical researches [1–7]. The main goal of the reconstruction of the ACL is the restoration of the anterior–posterior and rotational stability of the tibia in relation to the femur. The position of the femoral attachment of the ACL is more important for the kinematics after the ACL reconstruction. The position of the femoral foot print is well known [8–11]. There are several osseous landmarks, which define its anatomic position [12–14]. The biomechanics studies describe the kinematics of the knee joint after various types of the ACL reconstruction [15–18]. One of trends is the anatomic single-bundle (ASB) reconstruction. A cadaveric study describes that ASB reconstruction restores the rotational stability of the knee to the same extent as the double-bundle (DB) technique [15]. Another investigation describes that the DB reconstruction restores the rotational stability more than SB technique [19]. But, there is the absence of studies discussing the kinematics of the knee joint several years after the reconstruction or the rotational and anterior–posterior stability in weight-bearing condition in comparison with the contralateral healthy knee joint.
The objective of this study was to evaluate knee rotational and anterior–posterior stability at least 2 years after the ASB ACL reconstruction and the DB ACL reconstruction in comparison with the contralateral healthy knee joint. The Cincinnati, Lysholm and IKDC scores were analysed during 24 months after the operation.
Materials and methods
Between July 2011 and September 2012, 40 patients (40 knee joints) underwent the ACL reconstruction (23 men/17 women; 22 right/18 left knees) made by one senior surgeon. The average age of the patients was 27.5 years (range 17–42 years) (Tables 1, 2). All of them signed an informed consent on being included in prospective research. 20 patients had their ACL replaced by ASB technique using hamstring tendons, 20 patients had the DB reconstruction. The selection of patients for individual methods of the ACL replacement was done randomly using the permuted block randomization by Random Number Generator Software 7.0. Due to a minimal change in absolute values during the movement of the tibia against the femur (in mm or in degrees), the minimal sufficient sample size to detect the hypothesized effects was determined to N = 40 with the effect size of 90%, the power of 0.90 (β = 0.10) and α level 0.05. Demographic statistic parameters of both groups were similar.
The inclusion criteria were very strict. Only isolated complete ACL lesions were included. All other patients with associated injuries of other structures such as ligaments or meniscal lesions were excluded. The partially torn ACLs confirmed by arthroscopy were excluded, too. After the operation, the patients completed the Cincinnati, Lysholm and IKDC orthopaedics scores in 3th, 6th, 12th and 24th months.
Operative technique
After introduction of the patient into the general anaesthesia, the femur was fixed using a standard tight metal holder. Diagnostic arthroscopy was performed to confirm the isolated total rupture of the ACL and the grafts were harvested from the hamstring tendons.
During the ASB reconstruction, an 8-mm femoral tunnel was drilled into the medial surface of the lateral condyle of the femur. The anatomic position of the femoral attachment of the graft was determined by a calibrated arthroscopic hook. At 90° of knee flexion, the horizontal distance of the medial bone surface of the lateral condyle of the femur was measured. The tunnel was determined at lower 1/3 portion of the lateral intercondylar notch wall. The precise position of the femoral attachment was determined on the basis of the coordinate established by the Forsythe et al. [9] in the 43% of the distance from the most posterior part of the medial surface of the lateral condyle of the femur. This position was controlled by the arthroscopic camera situated in the AM portal. The tibial tunnel was drilled to the centre of the original footprint of the ACL. After the surgery, the position of the femoral tunnel was controlled by a CT scan and incorrectly placed cases were excluded from the study.
For the DB replacement, the 8-mm femoral bone tunnel for the AM bundle was located behind the lateral bifurcate ridge on the medial side of lateral femoral condyle. The 8-mm tibial bone tunnel for the AM bundle was located 14 mm in front of the PCL attachment slightly medially, as it was drilled in 55° angle from anteromedial side of the proximal tibia. The femoral attachment of the PL bundle was drilled between the lateral bifurcate ridge and the lateral intercondyle ridge. This tunnel was 6 mm wide. The tibial bone tunnel for the PL bundle was located 7 mm in front of PCL attachment slightly laterally, and drilled at 45° from medial side of the proximal tibia. All grafts in both groups were tonised using the dynamometer to 85 N and fixed with interference screws. No complications were found after the operation.
Experimental system
The optical computer navigation system OrthoPilot (Aesculap, Tuttlingen, Germany) was used to evaluate stability at the follow-up control. All measurements were taken on both the reconstructed and healthy knee. Tripods composed of three passives markers were fixed to the thigh and leg with stripes (Fig. 1). Measurement started with the patient in the standing position with both feet separated by 20 cm in neutral rotation (Fig. 2a). Then, the patient was asked to achieve 30° knee flexion (the investigator controlled the accuracy of the flexion on the screen of the computer). Afterwards, she/he performed under weight-bearing a maximal external trunk rotation (with the concomitant internal rotation of the tibia in the knee joint) and then returned to the neutral position (Fig. 2b). The same measurement was done for the internal trunk rotation (external rotation in the knee) (Fig. 2c). All measurements were repeated 3 times for each knee joint (operated and healthy). The deviation of the rotational movement was detected on the screen of the navigation. The anterior–posterior translation was analysed in the semi-sitting position with the arthrometer KT-1000 (Medronic, San Diego, California) in the 30°-flexed knee joint.
a The patient in the standing position with both feet separated by 20 cm in the neutral rotation. b The patient in the standing position with both feet separated by 20 cm in the internal rotation (IR). c The patient in the standing position with both feet separated by 20 cm in the external rotation (ER)
Statistical analysis
All data were statistically treated by STATISTICA 9.0 software. The description of the deviation of movement in degrees included mean, standard deviation and range for continuous variables. For determination of the statistically significant differences between the mean values, the non-parametric Wilcoxon test was used. The p value < 0.05 was considered statistically significant.
Source of funding
There were no financial resources used for this research.
Results
Stability of the knee joint
The mean follow-up was 27 months (range 24–33 months). All patients finished the rehabilitation programme during the first year after the reconstruction of the ACL.
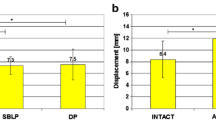
After the double-bundle (DB) reconstruction of the ACL, the mean external rotation of the tibia (ER) was 8.2° (range 5–11.6, SD 1.7) and the internal rotation (IR) was 10.2° (range 5.3–15.3, SD 2.4). In the contralateral healthy knee joint, ER was 8.5° (range 3.6–14.0, SD 2.3) and IR was 12.1° (range 7–19.6, SD 3.6). We did not find any statistically significant difference for the rotational laxity (external and internal rotation of the tibia after the DB reconstructions) of the ACL in comparison to the contralateral healthy knee joints (p > 0.05). The absolute values of the repeated measurements are in Table 1.
After the anatomic single-bundle (ASB) reconstruction, ER was 9.4° (range 5–16, SD 3.1) and IR was 13.1° (range 7–22.6, SD 4.1). In the contralateral healthy knee joint, ER was 7.7° (range 4–11.3, SD 2.1) and IR was 9.8° (range 6–16, SD 2.6). After the SB reconstruction, we found statistically significant difference in internal rotational stability between the reconstructed and healthy knees (p ˂ 0.05). External rotational stability was lower then in the contralateral healthy knee joints, but without the statistically significant difference (Table 1).
After the DB reconstruction of the ACL, the average value of tibia AP movement related to femur was 9.1 mm (min. 6 mm, max. 13 mm, SD 2.3), for the healthy knee was 7.7 mm (min. 6 mm, max. 12 mm, SD 0.9). There were no statistically relevant differences into the both groups (Table 2). For the ASB, the absolute data show no difference for the reconstructed and health group too (p = 0.285) (Table 2).
Scoring systems
The scoring systems show increasing of the absolutes values 2 years after the surgery (Figs. 3, 4, 5). There are no statistical differences between ASB and DB group for Cincinnati and IKDC scoring system, but for the Lysholm scoring system 24 months after the surgery, we confirmed the statistical differences between these groups (Tables 3, 4, 5).
Discussion
The rotational kinematics of the knee joint is still controversial after the reconstruction of the ACL. There are several studies demonstrating the higher efficiency of the DB reconstruction of the ACL in the restoration of the rotational movement, in comparison to the standard single-bundle (SB) technique. This hypothesis has been confirmed in experimental conditions and in vivo [15–18].
Ho et al. [15] have presented an in vitro study where they describe the improvement in the rotational stability of the knee joint while using a navigation system. The authors evaluated the kinematics for eight pairs of cadaveric knees in an ACL-intact condition, ACL-deficient condition after the cutting of the ACL, after the ASB reconstruction and after the DB reconstruction. The internal and external rotational stability was evaluated. They have concluded that the ASB ACL reconstruction and the DB technique can restore normal kinematics at the 30° of the knee flexion. A very similar research was made by Bedi et al. [16]. They used the computer navigation system for recording the kinematic changes after the ASB and DB reconstruction of the ACL in the cadaveric knee. In the results, they describe that the DB reconstruction of the ACL restores a pivot-shift manoeuver to a greater extent than the ASB technique.
In an in vivo study, Hofbauer et al. proved greater stability in the internal rotation of the knee joint after the DB reconstruction relatively to results of the SB reconstruction of the ACL [17]. The result of the study published by Song et al. shows the improvement of the combinatory rotational movement after the DB reconstruction with statistical difference [18]. They measured the biomechanics of the knee join after the SB and DB reconstructions of the ACL. In the ACL-intact knee, the combinatory rotational instability was 33.1°, after the DB reconstruction 23.3°. Before the SB reconstruction, the rotational movement was 35.1°, after the reconstruction 29.5°. But, these studies evaluate the kinematics of the knee joint perioperatively as we also demonstrated [20].
There are only a few studies which evaluate objectively the rotational kinematics of the knee joint 2 and more years after the reconstruction of the ACL. Gobbi et al. [21] demonstrate in their study no difference in the rotational laxity between the SB and DB reconstruction 3 years after the operation. They examined 60 patients divided into two groups. In the first group, they were 30 patients after SB reconstruction of the ACL; in the second group, 30 patients had a DB reconstruction. But they performed the rotational stability investigation only by clinical examination using the pivot-shift test. They did not find any difference between two techniques of the reconstruction. Similar results were published by Suomalainen et al. 5 years postoperatively [22].
In 2012, Hoshino et al. used dynamic stereo X-rays to performs radiographic images during the downhill treadmill running in comparison with the contralateral knee joint [23]. In comparison with the Gobbi study, they used the technical device for determine the difference in the axial rotation of the tibia after the SB and DB reconstructions of the ACL. In conclusion, they described a statistically significant difference between both techniques. They studied the rotational laxity (internal tibial stability) after the reconstruction of the ACL by these two techniques in comparison to the contralateral healthy knee joint as in our research. But, different to our study, they conclude that neither DB nor SB technique restores the rotational laxity of the knee joint as it is in the healthy knee. The absolute values were very similar to our research in the healthy knee; the IR was 7.7° in average.
Using the dynamic X-rays is one of possibilities to demonstrate the rotational instability. The other option is to use the navigation system to evaluate the kinematics of the knee joint in weight-bearing condition in comparison with the contralateral healthy knee joint. But, this technique is still in the early stages and the further clinical research is necessary. The use of the navigation system to evaluate the laxity of the knee joint was described by Chouteau et al. [24]. They used the navigation to control the laxity of the knee joint after the partial reconstruction of the ACL in comparison to the contralateral healthy knee joint.
There is no relevant study engaged in the objective analysis of the anterior–posterior stability of the knee joint after ASB and DB technique 2 years after the surgery. Hoshino et al. [23] compared the anterior–posterior stability after the standard single-bundle and double-bundle 2 years after the surgery. They concluded that there is a statistically relevant difference with the contralateral health knee joint for both groups.
Kondo et al. made a studysimilar to our research [25]. They compared the APT after the DB and ASB reconstruction of the ACL in the cadavers. They concluded the same AP instability after both the techniques of reconstruction. But, they did not compare the stability of the knee joint with the contralateral knee joint.
The measurement of the objective function of the knee joint is difficult. They are several studies that analysed the function of the knee joint after various types of the reconstruction of the ACL [26]. The triple-bundle replacement of the ACL is studied for example [27]. But the active rotational stability of the knee is (in the comparison with KT-1000 examination) influenced by the muscles surrounding the knee joint. The reconstruction of the ACL and the amount of the muscles restore the proprioception of the knee and improve the function of the joint during weight-bearing and sport activities.
The advantage of the presented study is the use of a precise device to evaluate the stability of the knee joint after the ACL reconstruction in the weight-bearing condition and comparing it to the contralateral healthy knee joint. The 2-year follow-up and the normal quality of life of all patients are also the positives, because we can demonstrate the kinematics of the knee joint in the standard conditions during the normal weight bearing.
The data show that the DB reconstruction of the ACL restores the rotational stability of the knee joint without any statistically significant difference in comparison to the contralateral healthy knee (p > 0.05). The anterior–posterior stability of the knee joint is restored to the same extent as the contralateral knee joint following the DB and ASB reconstruction of the ACL. The main finding of this study is that the internal rotational stability of the knee joint after the anatomic ASB technique is not sufficient.
References
Mommersteegi TJA. The fibre bundle anatomy of human cruciate ligaments. J Anat. 1995;187:461–71.
Girgis FG. The cruciate ligaments of the knee joint-anatomical, functional and experimental analysis. Clin Orthop. 1975;106:216–31.
Kaya A. Evaluation of the two bundles of the anterior cruciate ligament with 1.5 T magnetic resonance imaging. Acta Orthop Traumatol Turc. 2010;44(1):54–62.
Lorenz S. Radiologic evaluation of the insertion sites of the 2 functional bundles of the anterior cruciate ligament using 3-dimensional computed tomography. Am J Sports Med. 2009;37(12):2368–76.
Colombet P. Morphology of anterior cruciate ligament attachments for anatomic reconstruction: a cadaveric dissection and radiographic study. Arthroscopy. 2006;22(9):984–92.
Hart R. Hamstring versus quadriceps tendon graft in double-bundle anterior cruciate ligament reconstruction. Acta Chir Ort Traum Čechoslovaca. 2010; 77:296–303.
Petersen W. Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res. 2010;454:35–47.
Steckel H. Arthroscopic evaluation of the ACL double bundle structure. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):782–85.
Forsythe B. The location of femoral and tibial tunnels in anatomic double-bundle anterior cruciate ligament reconstruction analyzed by three-dimensional computed tomography models. J Bone Jt Surg Am. 2010;92:1418–26.
Martins CAQ. The concept of anatomic anterior cruciate ligament reconstruction. Oper Tech Sports Med. 2008;16:104–15.
Kopf S. A systematic review of the femoral origin and tibial insertion morphology of the ACL. Knee Surg Sports Traumatol Arthrosc. 2009;17:213–19.
Zantop T. Tunnel positioning of anteromedial and posterolateral bundles in anatomic anterior cruciate ligament reconstruction anatomic and radiographic findings. Am J Sports Med. 2008;36(1):65–72.
Ferretti M. Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy. 2007;23(11):1218–25.
Purnell ML. Anterior cruciate ligament insertions on the tibia and femur and their relationships to critical bony landmarks using high-resolution volume-rendering computed tomography. Am J Sports Med. 2008;36(11):2083–90.
Ho JY. Equal Kinematics Between Central Anatomic Single-Bundle and Double-Bundle Anterior Cruciate Ligament Reconstructions. Arthroscopy. 2009; 25(5):464–72.
Bedi A. A comparison of the effect of central anatomical single-bundle anterior cruciate ligament reconstruction and double-bundle anterior cruciate ligament reconstruction on pivot-shift kinematics. Am J Sports Med. 2010;38(9):1788–94.
Hofbauer M. Rotational and translational laxity after computer-navigated single- and double-bundle anterior cruciate ligament reconstruction. Knee Surf Sports Traumatol Arthrosc. 2010;18:1201–7.
Song EK. Prospective comparative study of anterior ligament reconstruction using the double-bundle and single bundle technique. Am J Sports Med. 2009;37(1705):1705–11.
Komzák M. AM bundle controls the anterior–posterior and rotational stability to a greater extent than the PL bundle—a cadaver study. Knee. 2013;20(6):551–5.
Komzák M. Does the posterolateral bundle influence rotational movement more than the anteromedial bundle in anterior cruciate ligament reconstruction?: a clinical study. J Bone Jt Surf Br. 2012;94(10):1372–6.
Gobbi A. Single versus double-bundle ACL reconstruction: is there any difference in stability and function at 3-year followup? Clin Orthop Relat Res. 2012;470(3):824–34.
Suomalainen P. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomised study with 5-year results. Am J Sports Med. 2012;40(7):1511–18.
Hoshino Y. Can joint contact dynamics be restored by anterior cruciate ligament reconstruction? Clin Orthop Relat Res. 2013;427:2924–31.
Chouteau J. Knee rotational laxity and proprioceptive function 2 years after partial ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):762–6.
Kondo E. Biomechanical comparison of anatomic double-bundle, anatomic single-bundle, and nonanatomic single-bundle anterior cruciate ligament reconstructions. Am J Sports Med. 2011;39(2):279–88.
Filbay SR. Health-related quality of life after anterior cruciate ligament reconstruction. A systematic review. Am J Sports Med. 2014;42(5):1247–55.
Mae T. Immediate postoperative anterior knee stability: double- versus triple-bundle anterior cruciate ligament reconstructions. Arthroscopy. 2013;29(2):213–19.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Martin Komzák, Radek Hart, Martin Feranec, Petr Šmíd, and Radka Kocová declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Komzák, M., Hart, R., Feranec, M. et al. In vivo knee rotational stability 2 years after double-bundle and anatomic single-bundle ACL reconstruction. Eur J Trauma Emerg Surg 44, 105–111 (2018). https://doi.org/10.1007/s00068-017-0769-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0769-7