Abstract
High-risk pituitary adenomas are aggressive. They show clinical and imaging features similar to those of carcinomas, including infiltration of the surrounding brain structures, but lack cerebrospinal or systemic metastases. In addition, they display distinct behavior, including tendency for fast growth and frequent recurrences, which are difficult to control. The term “high-risk” adenoma was first introduced in the 4th edition of the World Health Organization Classification of Endocrine Tumors in 2017. Five defined adenoma types belong to this category, including sparsely granulated somatotroph, lactotroph in men, Crooke cell, silent corticotroph, and plurihormonal PIT-1 positive adenomas. The morphological and immunohistochemical characteristics of high-risk adenomas are herein described in detail. In addition, the clinical features and the treatment options are presented. This review focuses on predictive markers assessed by immunohistochemistry, which help clinicians to design the appropriate treatment strategies for high-risk adenomas. Somatostatin receptor status predicts effectiveness of postsurgical treatment with somatostatin analogs, and MGMT expression predicts response to treatment with temozolomide. This comprehensive review presents the clinical and pathological features of high-risk pituitary adenomas, underlines the contribution of immunohistochemistry, and emphasizes the leading role of pathology in the design of optimal clinical management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pituitary carcinomas, which are very rare accounting for 0.1–0.2% of all pituitary tumors, have distinctive malignant behavior with established craniospinal or systemic metastases [1]. Apart from carcinomas, 35% of pituitary adenomas show similar features, including infiltration of the cavernous and sphenoid sinuses but lack systemic metastases [2]. Clinicians often use the term “aggressive” adenomas, referring to their abnormal clinical behavior, including local infiltrative features, tendency to fast growth, and frequent recurrences, all of which are difficult to control [3, 4]. Alternatively, the term “refractory” pituitary adenoma is used to define the aggressive nature of an adenoma resistant to conventional treatment modalities such as surgery, pharmaceutical therapies, or radiation [5, 6]. The term “high-risk adenomas” was first introduced in the 4th edition of the World Health Organization (WHO) Classification of Tumors of Endocrine Organs in 2017 to define certain histological adenoma types with clinical aggressive characteristics. These include the following types: sparsely granulated somatotroph, lactotroph in men, Crooke cell, silent corticotroph, and plurihormonal PIT-1 positive adenomas (Table 1). The WHO classification is based on histology and immunohistochemistry for pituitary hormones and other specific diagnostic markers, such as cytokeratins and transcription factors. Meanwhile, after more than 10 years of research, the diagnostic significance of Ki-67 and p53 protein has not been established [7]. As a rule, high-risk adenomas show a high Ki-67 proliferation index [8]. However, a large series of aggressive pituitary tumors has revealed that Ki-67 and p53 cannot distinguish aggressive pituitary tumors from pituitary carcinomas, and there were no significant differences in clinical parameters [9]. Therefore, at present, no validated histological and molecular prognostic markers exist to identify pituitary neoplasms with clinically aggressive behavior. Instead, assessment of invasion using MRI and, even better, by direct intraoperative observation is very important [8]. A clinicopathological grading system, not based solely on histological grounds but also considering as a scoring factor invasion observed on MRI, may predict tumor progression [10]. A study using the same scoring system has revealed that invasion, Ki-67, and tumor type were the only independent prognostic factors of disease-free survival. However, it has not been proved whether p53 represents an independent factor of aggressive behavior [11]. A practical algorithm to predict postsurgical recurrence and progression also taking into consideration the histological type has recently been reported [12]. High-risk adenomas require appropriate treatment strategies to control progression and high recurrence rate, particularly after incomplete surgical resection. Therefore, precise classification with subtyping of pituitary neoplasms is crucial. Currently, the most important immunohistochemical markers predicting response to treatment with somatostatin analogs and temozolomide (TMZ) are somatostatin receptors (sstrs) and O6-methylguanine-DNA methyltransferase (MGMT), respectively.
This comprehensive review presents the clinical and pathological features of high-risk pituitary adenomas and highlights the need to identify and separate these well-defined aggressive histological variants. In addition, it underlines the importance and the leading role of pathology in the assessment of predictive markers, which help to design the appropriate type of treatment. The incorporated gallery of figures illustrates the main histological and immunohistochemical characteristics of each high-risk adenoma type. The WHO Classification of Tumors of Endocrine Organs provides updates incorporating new information based on recently accumulated knowledge. A proposal to replace the term “pituitary adenomas” with “pituitary neuroendocrine tumors (pit-NETs),” issued after the publication of the 4th WHO edition [13, 14], created an impact followed by intense discussions [15,16,17]. Nevertheless, emerging issues, such as attempts to change the nomenclature of endocrine tumors, will be revisited and discussed in the consensus meeting of the panelists for the next (5th) edition of the WHO Classification of Tumors of Endocrine Organs.
High-risk adenomas
Sparsely granulated somatotroph adenomas
Sparsely granulated somatotroph adenomas (SGSAs) on histology are morphologically chromophobic. They are characterized by the presence of easily defined, round, cytoplasmic fibrous bodies which dislocate the nucleus to the cell periphery, forming a crescent-like shape (Fig. 1A) [18]. On immunohistochemistry, they correspond to low molecular weight cytokeratins, mostly 7/8 (clone CAM 5.2) and 18 (Fig. 1B) [19]. SGSAs usually demonstrate focal and less intense reactivity for growth hormone (GH) in contrast to densely granulated somatotroph adenomas (DGSAs), which show strong and extensive immunoreactivity for GH throughout the cytoplasm. SGSAs occur at a rate of approximately 35% of surgical series, although a subset of adenomas referred to as intermediate type consists of cells with a cell mixture of different granulation patterns [20, 21]. From the clinical point of view, SGSAs represent a distinct subgroup with more aggressive behavior. Compared to DGSAs, they occur in patients younger than 50 years of age with a slight preponderance in females [20, 22, 23]. They also have a lower remission rate in response to surgery, increased proliferation rate, and a tendency to regrow after surgical excision, and they are more difficult to operate on [18, 22, 24,25,26,27]. As a rule, SGAs have a worse prognosis as compared to DGAs [11, 28]. However, there is one publication that reports no significant statistical differences in postsurgical remission between the two subtypes in the studied material [21]. In addition, they are generally larger and are associated with a higher frequency of suprasellar extension and cavernous sinus invasion [25].
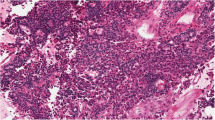
A Sparsely granulated somatotroph adenoma with fibrous bodies displacing the nucleus to the periphery of the cytoplasm (H&E, 25 ×). B Immunohistochemistry of sparsely granulated somatotroph adenoma for low molecular weight keratin, revealing dot-like cytoplasmic immunoreactivity to fibrous bodies (25 ×). C Chromophobic lactotroph adenoma (H&E, 25 ×). D Lactotroph adenoma immunoreactive for PRL with characteristic paranuclear localization (25 ×)
The reason that DGSAs respond better than SGSAs to the administration of somatostatin analogs is that most of them have a mutation in the α-subunit of Gs proteins and also have higher sstr2 mRNA levels [26, 29, 30]. In a study investigating the granulation pattern of somatotroph adenomas in conjunction with response to treatment with somatostatin analogs, no mutations were found in a total of 30 SGSAs included in the study [25]. Therefore, for the treatment of residual tumor, separation of SGSAs form the DGSAs is of clinical significance, given that the former show a lower response to somatostatin analogs and are more sensitive to treatment with GH antagonists [25, 31]. A prevalence of sstr2a was found in DGSAs compared to other subtypes [30]. SGSAs showed lower sstr2 expression compared to DGSA and are less responsive to somatostatin analogs [21, 24]. This is why SGSAs may respond better to pasireotide (SOM 230), a multi-receptor targeted somatostatin analog binding sstr1, sstr2, and sstr3, its highest affinity being for sstr5, which is significantly expressed in SGSAs [32]. Therefore, evaluation of sstr profile in somatotroph adenoma subtypes is important in the postsurgical management of acromegaly.
During the last decade, efforts were made using radiologic parameters to identify and separate DGSAs from SGSAs preoperatively. Based on radiologic features, SGSAs are associated with higher MRI T2-weighted signal ratio and are more frequently invasive. These features may distinguish SGSAs from DGSAs preoperatively, helping clinicians to identify candidates for preoperative medical treatment and neurosurgeons to decide on surgical strategies [21, 27, 33]. This promising approach could be useful for postsurgical treatment with somatostatin analogs. It has been demonstrated that patients with DGSAs who have preoperatively received such treatment have a better clinical and hormonal response compared to those patients harboring SGSAs [34]. Moreover, radiomic features extracted from contrast-enhancing and total tumor portions from MRI T2-weighted signal were used to evaluate the granulation pattern of somatotroph adenomas, based on a least absolute shrinkage and selection operator logistic regression model. These features may serve as useful biomarkers to predict the granulation pattern of somatotroph adenomas [35]. However, the validity of the latter radiologic features is still under investigation.
There is little information regarding the response of somatotroph adenomas to treatment with TMZ [36]. In a study including 197 different histological subtypes of pituitary adenomas, the substantial majority of somatotroph adenomas showed low MGMT expression. However, the authors do not provide any specific information regarding SGSAs and DGSs [37]. Another study reports low to absent MGMT immunoreactivity in SGSAs, indicating response to treatment with TMZ in the case of unsuccessful conventional treatment [38]. This probably reflects successful treatment of these adenomas with other conventional, less aggressive modalities.
Lactotroph adenomas in men
Lactotroph adenomas (prolactinomas) in men are mostly chromophobic (Fig. 1C), composed of large, sparsely granulated cells, negative for periodic acid-Schiff (PAS) reaction. Immunohistochemistry for prolactin (PRL) usually displays characteristic paranuclear localization, known as the Golgi pattern (Fig. 1D) [18, 24]. These are mostly macroadenomas, with suprasellar extension in up to 80% of cases, often presenting with mass effect symptoms, due to expansible growth and compression of the adjacent brain structures and invasion of the cavernous and sphenoid sinus [39, 40]. Visual field defects occur in about 45% of patients and sexual disorders, gynecomastia, and hypopituitarism develop in approximately 35% of cases [32, 33, 40, 41]. Most patients develop hypogonadism, which is associated primarily with low testosterone levels and in some cases with partial hypopituitarism [42]. Giant adenomas are rare, accounting for 1–5% of all lactotroph adenomas: they are mainly diagnosed in men between 20 and 50 years of age, with a male to female ratio of about 9:1 [39, 42]. The large tumor size in males is probably related to subtle clinical symptoms, such as decreased libido and erectile dysfunction, leading to delayed diagnosis [43]. In contrast, because of early development of galactorrhea-amenorrhea in women of reproductive age, typically these patients present with microprolactinomas. The tumor size and PRL levels in men are significantly higher than those in women, with the tumors growing rapidly and often invading the cavernous sinus. The majority of giant lactotroph adenomas respond to treatment with dopamine agonists (DAs), including long-term cabergoline [44]. However, large tumors, particularly in men, are less responsive and often resistant to DAs [42, 45, 46]. Lactotroph adenomas associated with multiple endocrine neoplasia type 1 (MEN-1) have a worse clinical prognosis [47]. Loss of chromosome 11 in PRL-producing adenomas, associated with MEN-1, has been reported in young male patients [48, 49].
Several studies have documented the successful antitumor effect of TZM on aggressive lactotroph adenomas in men, resulting in clinical improvement and significant reduction of serum PRL levels [50,51,52,53]. These adenomas have the highest response rate to TMZ. According to a review of the published case series, aggressive lactotroph adenomas respond best to TMZ, demonstrating an approximately 50% response rate [52]. A systematic report also showed that TMZ therapy was effective, achieving tumor shrinkage in 76% of patients with highly aggressive lactotroph adenomas not responding to dopamine agonist and other treatments, including surgery and radiotherapy [44]. Lactotroph adenomas are more likely to have low MGMT expression compared to other adenoma types [54]. A strong correlation between MGMT-negative staining and sensitivity to TMZ was reported in 15 out of 20 lactotroph adenomas [55]. In addition, they show an inverse correlation between MGMT immunostaining and MGMT promoter methylation, indicating that patients with such adenomas may be candidates for treatment with TMZ [50, 56]. However, some patients exhibit loss of MSH2 and mismatch repair genes, leading to rapid development of resistance to TMZ [54]. Lastly, acquired TMZ resistance mechanisms have been implicated the transformation of an aggressive lactotroph adenoma into carcinoma [57].
Silent corticotroph adenomas
Silent corticotroph adenomas show identical morphology on histochemistry for PAS staining and immunohistochemistry for ACTH with their functioning counterparts. They are subclassified into densely granulated (type 1) and sparsely granulated (type 2), which are acidophilic and chromophobic, respectively. The cells of the sparsely granulated variant show deposition of hyaline material corresponding to low molecular weight cytokeratins, forming a perinuclear and partly paranuclear halo. They are both positive for PAS reaction (Fig. 2A) and immunopositive for adrenocorticotropic hormone (ACTH) (Fig. 2B). Silent corticotroph adenomas lack clinical signs or symptoms of Cushing’s syndrome, the cortisol levels are within normal limits, and they may show only minor elevations of serum ACTH levels. Subtype 1 and 2 adenomas present differences with respect to sex, with a ratio of 1.4:1 versus 6:1 between males and females, respectively [58]. The majority of silent corticotroph adenomas have a clinically aggressive course and are refractory to conventional therapy, with high progression and recurrence rates. Silent corticotroph adenoma may transform into carcinoma, as described previously [59]. These clinical and pathological features underline the need for long-term follow-up [58, 60]. Sublassification of corticotroph adenomas into types 1 and 2 according to their granulation pattern is important in terms of clinical behavior, recurrences, and treatment outcome. Type 2 adenoma displays a more prominent proliferation rate and more frequent invasion [61]. Given the absence of hypercortisolemia, no Crook hyaline changes are noted in the corticotroph cells of the normal adenohypophysial parenchyma tissue fragments, often included in the histology specimen. Galectin-3 is the only currently available immunohistochemical marker to distinguish functioning from silent corticotroph adenomas. In contrast to functioning adenomas, galectin-3 is absent in the substantial majority of the silent ones [62]. Its infrequent expression in silent corticotroph adenomas suggests an alteration of galectin-3 and/or of its gene function [63].
A Silent corticotroph adenoma positive for PAS stain (10 ×). B Sparsely granulated silent corticotroph adenoma immunoreactive for ACTH (10 ×). C Crooke cells with massive perinuclear or paranuclear cytoplasmic depositions of hyaline material (25 ×). D Functioning Crooke adenoma showing cytoplasmic and nuclear immunoreactivity for galectin-3 (25 ×)
In a recent study, the mRNA levels of sstrs were determined by real-time reverse transcription-polymerase chain reaction (RT-PCR). sstr1 and sstr2 mRNA levels were higher in silent than in functioning corticotroph adenomas, while sstr5 mRNA levels were about 14-fold higher in functioning than in silent ones [64]. The fact that sstr1 and sstr2 mRNA levels were significantly higher in silent than in functioning corticotroph adenomas justifies treatment with somatostatin analogs and, in particular, application of the most effective novel long-acting-pasireotide, which displays a higher affinity to a wide range of sstr types [65].
Corticotroph adenomas respond better to TMZ, with an approximately 50% response rate [52]. Therefore, TMZ could be effective in the treatment of refractory silent corticotroph adenomas [66]. TMZ in combination with capecitabine showed a high response in a case series of four patients with aggressive, functioning, and silent corticotroph adenomas. Three of these cases (75%) exhibited complete or partial response to the treatment [5].
Crooke cell adenomas
Crooke cell adenomas belong to a rare variant of corticotroph adenomas with a distinct histopathological pattern and clinical behavior. They produce ACTH, presenting either as functioning, which causes Cushing’s disease, or silent [67]. Adenoma cells display a characteristic massive accumulation of hyaline, forming a donut-like perinuclear ring (Fig. 2C), which displaces the ACTH-storing secretory granules to the cell periphery. On immunohistochemistry, the hyaline material corresponds to low molecular weight cytokeratin filaments. Crooke cell adenomas are aggressive, as compared to classic corticotroph adenomas, with a high risk of morbidity and mortality. They show invasion of the adjacent tissues, with a tendency to recur after reoperation and/or radiotherapy [66, 68]. In addition, they may progress to carcinoma [69, 70]. Most of them are functional macroadenomas, typically affecting middle-aged women, with only a few reported clinically silent cases [4, 71]. The presence of nuclear immunoreactivity for galectin-3 in functioning Crooke cell adenomas is in keeping with their aggressive behavior (Fig. 2D) [62]. For some unexplained reason, however, their proliferation index, assessed by Ki-67, is low, at approximately 1% [66, 72]. Crooke cell adenomas rarely occur in pediatric patients [73]. In young populations, silent adenomas may present with delayed puberty [71]. These adenomas may have sstrs; however, treatment with somatostatin analogs and octreotide LAR may not be effective. The same is true for dopamine agonists such as cabergoline [66].
Clinically aggressive Crooke adenomas with low or absent MGMT expression are responsive to treatment with TMZ [66, 72, 74, 75]. MGMT is not the sole molecular factor determining sensitivity to TMZ administration. The expression of mismatch repair gene homologous protein MSH6 serves as an alternative predictive marker for aggressive pituitary adenomas. A study evaluating the role and clinical significance of MSH6 by immunohistochemistry has reported a positive correlation between MSH6 expression and response to TMZ. Two Crooke cell adenomas, included in this study, both positive for MSH6 and one of them negative for MGMT, responded to TMZ treatment. Interestingly, in the above study no significant correlation of MGMT, Ki-67, and p53 with the efficacy of TMZ was noted [75].
Plurihormonal PIT-1 positive adenomas
Plurihormonal PIT-1 positive adenomas, originally called silent subtype 3, are extremely rare neoplasms originating from the PIT-1 lineage [76]. Histologically, they are chromophobic, poorly differentiated, and negative on PAS staining and are composed of large polygonal to spindle-shaped cells [76, 77]. On immunohistochemistry, they may display reactivity for various pituitary hormones, including GH, PRL, thyroid-stimulating hormone (TSH), and α-subunit (Fig. 3A) [76, 78]. The most important diagnostic feature, however, is immunopositivity for PIT-1 transcription factor (Fig. 3B), which is also highly expressed in other functioning and silent adenomas secreting GH, TSH, and α-subunit [77, 79, 80]. In addition, they are also focally positive for estrogen receptors and GATA3 [81]. Accurate diagnosis, based on histology, is extremely difficult and may require confirmation with electron microscopic studies. The ultrastructural hallmark of this adenoma type is the presence of abundant nuclear spheridia. The cells are monomorphous and undifferentiated and contain sparse secretory granules of 50–210 nm [76]. Plurihormonal PIT-1-positive adenomas at the time of diagnosis are large or giant, with cavernous sinus invasion and occasional involvement of the clivus [77]. They mostly occur in young individuals, especially women, and are often associated with particularly clinically aggressive behavior with high persistence rate, recurrences in approximately 50% of cases, and lower rates of disease-free survival [25, 76,77,78]. Even though they may produce more than one of the pituitary hormone types, in their substantial majority, they remain silent, although some cases may be associated with hyperthyroidism, acromegaly, or hyperprolactinemia [77].
A PIT-1 plurihormonal adenoma, with focal immunoreactivity for alpha-subunit (10 ×). B PIT-1 plurihormonal adenoma showing nuclear immunoreactivity for PIT-1 transcription factor (40 ×). C Intense and complete, linear cytoplasmic distribution of immunohistochemical expression for sstr2 in a somatotroph adenoma, indicating response to treatment with somatostatin analogs (10 ×). D Lactotroph adenoma with extensive MGMT expression, predicting no response to treatment with TMZ (25 ×)
The presence of sstrs in some of these adenomas may predict response to somatostatin analogs, contributing to long-term control in patients with residual tumor mass. A recent study has demonstrated that thyrotroph adenomas highly express sstr2A, sstr2B, sstr3, and sstr5 [82]. These findings are in keeping with the presence of sstr2A in 89% of silent thyrotroph adenomas reported previously [83]. The latter observations might be important for plurihormonal PIT-1-positive adenomas, producing TSH expressing sstrs. As a rule, administration of octreotide and lanreotide to thyrotroph adenomas leads to reduction of TSH secretion and normalization of TSH blood levels in more than 80% of patients [84]. In another retrospective study, treatment with somatostatin analogs in seven patients with TSH-secreting adenomas led to normalization of free thyroid hormones and TSH levels and to reduction of adenoma volume in six of them [85].
In a study including eight silent, clinically aggressive plurihormonal PIT-1-positive adenomas, six of them (75%) lacked MGMT immunoreactivity. This finding suggests potential efficacy of management with administration of TMZ [86]. Another study reported MGMT promoter methylation in 42% of 12 of these silent adenomas, while all the methylated ones had low MGMT immunoreactivity. It therefore seems that patients with these adenomas may respond to treatment with TMZ [87].
Predictive markers and the role of pathology
Somatostatin analogs and evaluation of sstrs
Somatostatin is a tetradecapeptide which inhibits endocrine and exocrine cell secretion and proliferation. Somatostatin exerts its effects via specific sstrs, distributed throughout the cell membrane, which have high affinity to natural somatostatin [88]. Synthetic somatostatin analogs are currently used to treat various pituitary adenomas. Among the five types of sstrs, sstr2 and sstr5 are the most important, although novel somatostatin analogs show wide binding activity with other sstr types [89]. For somatotroph adenomas, targeted treatment with somatostatin analogs is the first-line therapeutic option. This option might also be appropriate for plurihormonal PIT-1-positive adenomas producing GH, or TSH, which more likely express sstrs. Large adenomas fail to be removed completely, and the remaining residual part requires additional treatment. For postsurgical treatment, the status of adenomas expressing sstrs is recognized as a reliable marker to predict the outcome of treatment with somatostatin analogs [21, 82, 90]. These drugs may be effective even for SGSAs, which respond less successfully to treatment [21]. To ensure and maximize the expected therapeutic result, sstrs should be carefully evaluated before starting the treatment. Several methods are available to detect sstrs, such as mRNA, real-time PCR, and immunohistochemistry. As a rule, every method has advantages and disadvantages. Total mRNA extraction of sstrs provides high-quality material, whereas quantitative analysis using real-time reverse transcription-polymerase chain reaction analysis of sstrs provides reliable information [91]. Techniques based on sstr mRNA analysis require high-quality mRNA from fresh tissue. However, the whole extracted mRNA may be derived from tissue fragments of nontumorous adenohypophysial parenchyma, often included in surgical specimens. Therefore, evaluation of sstr mRNA status cannot be considered for the prediction of the therapeutic outcome [82, 90]. Due to the fact that in the majority of routine cases only formalin-fixed paraffin-embedded tissue is available, immunohistochemical evaluation of sstrs is the method of choice. The technique, which is suitable even for archival material, allows assessment of density and distribution pattern of membrane-active sstrs. The currently available highly sensitive monoclonal antibodies for sstrs enable high-resolution analysis and correlation to tissue morphology. Sstr immunostaining localized on the cell membrane is crucial to predict response to treatment, highlighting the importance of somatostatin analogs for therapeutic management [92]. Therefore, for prediction of therapeutic efficacy, immunohistochemical evaluation relies on the membrane sstr status, while the internalized receptor component within the cytoplasm must be ignored. For the assessment of sstr membranous immunopositivity, a four-scale scoring system has been proposed based on the pattern of membranous sstr distribution, similar to that initiated for evaluation of Her-2/neu membrane distribution in breast carcinomas (Table 2). The 10% threshold for sstr staining is used for evaluation in the scoring system, because estimation below this threshold is not dependable. The criteria of this scoring system are well enough defined to make it easy and reproducible for application in routine pathology so as to ensure consistent results [82]. According to previous studies, sstr expression in more than 10% of a cell population is sufficient to predict response to treatment with somatostatin analogs. The staining intensity reflects the amount of the receptor protein: thus, scores 2 + and 3 + , as defined in the scoring system and corresponding to a high density of sstr protein, should be considered of clinical importance (Fig. 3C). In contrast, a weak staining intensity corresponding to low sstr levels predicts negative or low response to treatment [93, 94]. The cytoplasmic immunoreactivity of sstrs, if present, is not a technical artifact but corresponds to the internalized sstr component. Another scoring system, correlating sstr immunohistochemistry with octreoscan scintigraphy, in other neuroendocrine tumors, like gastroenteropancreatic, also takes into account cytoplasmic localization of sstr. The scoring system is important for the evaluation of the efficacy of treatment with somatostatin analogs [95, 96]. Optimization of working dilutions and selection of the type of applied immunohistochemical protocol should be carefully tested and designed in each laboratory in order to obtain reliable and consistent results.
TMZ and evaluation of MGMT
To control progression and symptoms of high-risk adenomas resistant to conventional pharmaceutical drugs, surgery, or/and radiation, more advanced therapeutic modalities are required. TMZ is an oral alkylating chemotherapeutic agent that has been found to be effective in the treatment of such adenomas. Administration of TMZ can be a chemotherapy option when conventional treatments fail to maintain remission. Response to treatment is evident based on reduction in tumor volume, arrest of tumor growth, and prolonged survival [97]. In most cases, there is a strong association between negative MGMT immunostaining and excellent response to TMZ. Although TMZ may deplete low MGMT stores, high MGMT expression indicates absence of response (Fig. 3D) [98, 99]. Lack of standardization of the criteria used to evaluate the clinical response rate has generated controversial results [99]. While treatment with TMZ is effective in about 50% of patients, it is not effective for long-term control of aggressive adenomas [52]. The reported absence of correlation between promoter methylation and MGMT immunoreactivity status suggests complex underlying regulatory mechanisms [87]. Unfortunately, as demonstrated by several studies, no correlation between MGMT with Ki-67 and p53 has been detected [54, 66, 72, 75]. It is generally agreed that the gold standard criterion to select candidate patients with aggressive adenomas for TMZ treatment is immunohistochemistry for MGMT. However, some cases that are negative for MGMT do not respond to treatment. Due to inconsistency of MGMT expression and unavailability of other treatment modalities, some clinicians disregard MGMT status and proceed directly to administration of TMZ. The issue of whether MGMT represents the best predictive marker is controversial and still remains a subject of debate. There are several technical reasons that may explain the lack of response [56, 100,101,102]. In a recent study, only one of the 25 pituitary adenomas analyzed was positive for MGMT when immunohistochemistry was carried out without the use of a retrieval protocol. However, repeated immunohistochemistry with application of retrieval protocols disclosed MGMT positivity in another three initially presumed negative adenomas. The above study illustrates the implication of technical drawbacks of MGMT immunoreactivity that may lead to false negative results [101]. Formaldehyde, which is widely considered as the standard tissue fixative, might cause technical problems in immunohistochemistry, due to the formation of chemical dialdehyde bonds sequestering the antigen sites [103]. To overcome this problem, several pretreatment techniques, leading to unmasking of hidden antigen sites, are available. Pathologists need to experiment with various unmasking protocols and select the most appropriate before introducing MGMT immunohistochemistry for clinical application [102, 104]. Other technical problems that may also result in failure include inappropriate (delayed or prolonged) tissue fixation of adenoma tissue samples, and duration of paraffin tissue block storage. Furthermore, lack of a standard scoring system for counting MGMT positive nuclei and interobserver or intraobserver variations constitute additional obstacles to determining MGMT expression with accuracy [102, 105]. Lastly, low sensitivity of the antibody or the detection system used may lead to inconsistent immunohistochemical results. As would be expected, all these pre-analytical and post-analytical problems deter some clinicians from relying on MGMT immunohistochemistry. Given that TMZ administration should be restricted to selected patients with potential for response to treatment, MGMT expression by immunohistochemistry using the appropriate antigen retrieval protocol is strongly recommended [101].
MGMT promoter methylation and MSH6 expression represent alternative markers predicting response to treatment with TMZ [56, 75, 87, 97].
Emerging novel treatment modalities
Some high-risk, refractory aggressive-invasive adenomas that are resistant also to TMZ require more advanced treatment modalities [6, 106, 107].
Vascular endothelial factor (VEGF) inhibits angiogenesis, resulting in the suppression of tumor growth. Anti-VEGF was applied either as monotherapy or in combination with TMZ in two patients with corticotroph adenomas, one of them silent type 2 progressing to carcinoma. Anti-VEGF treatment stopped tumor progression for 26 months and 5-years follow-up, respectively. It should be noted that both adenomas were strongly immunoreactive for VEGF. Therefore, VEGF may serve as a predictive marker for anti-VEGF treatment [59, 107]. In another study, a corticotroph carcinoma was treated successfully with combined TMZ and anti-VEGF, resulting in 5 years of progression-free follow-up [108].
Epidermal growth factor receptor (EGFR)-targeting tyrosine kinase inhibitor has been used to treat two resistant lactotroph macroadenomas as well as an aggressive corticotroph adenoma that progressed to carcinoma [107, 109, 110]. The therapeutic effectiveness of EGFR tyrosine kinase inhibitor in corticotroph adenomas was found to be related to nuclear expression of EGFR [110]. The presence of ubiquitin-specific protease 8 mutations in up to two-thirds of patients with corticotroph adenomas may underlie the increase in EGFR signaling [111]. However, in another study of aggressive lactotroph adenomas, EGFR and ErbB2 immunohistochemical expression was not detectable in three of the four cases studied, and no correlation was found with treatment response [112].
The anti-proliferative effect of mTOR inhibitors has been demonstrated in pituitary cell lines and primary cultures [113]. Administration of mTOR inhibitors results in decreased protein synthesis, reduced cell growth, and cell cycle arrest. An oral mTOR inhibitor drug in combination with other treatment modalities was tested in six patients with aggressive lactotroph and corticotroph adenomas. Three of them, one with lactotroph and two with corticotroph adenomas, showed transient stability for 5 to 12 months [114,115,116]. However, more studies are needed to clarify the usefulness of mTOR inhibitors to treat patients with highly aggressive-refractory adenomas that failed to respond to other treatment modalities, including TMZ.
Programmed death 1 (PD-1) blockade has achieved robust responses in various malignancies. PD-L1 and CD8 + tumor-infiltrating lymphocytes (TILs) represent predictive markers for this immunotherapy. A recent study of 191 pituitary adenomas reported that PD-L1 is frequently expressed in functioning adenomas with aggressive behavior. In addition, a correlation was noted between positive CD8 + TIL expression and elevated blood level of PRL, GH, ACTH, and cortisol. PD-L1 expression was also correlated with immunostaining for PRL and GH and a higher Ki-67 index, while expression of CD8 positive TILs was correlated with immunostaining for PRL [117]. In a series of 48 functioning and silent aggressive pituitary tumors, the PD-L1 RNA and protein expression was studied. Significantly increased PD-L1 was observed in functioning pituitary compared to non-functioning adenomas. In addition, recurrent adenomas harbored lower levels of PD-L1 mRNA compared to primary ones [118]. A single case report described successful immunotherapy treatment of pituitary lactotroph macroadenoma [119]. Another case of corticotroph carcinoma treated consecutively with anti-CTLA-4 and anti-PD-L1 monoclonal antibodies showed a 59% and 92% decrease of the primary tumor and liver metastasis volume, respectively, in a 6-month follow-up [120]. It seems that immunotherapy based on checkpoint inhibitors may hold promise in the treatment of high-risk refractory adenomas and carcinomas.
Lastly, peptide receptor radionuclide therapy (PRRT) represents a promising option as third-line treatment strategy for aggressive-refractory pituitary adenomas and carcinomas. According to recent reports, PRRT resulted in growth arrest, tumor shrinkage, and clinical or biochemical improvement in four out of 13 patients with aggressive pituitary neoplasms, including two giant prolactinomas, one silent corticotroph adenoma, and one carcinoma with metastasis [121].
Conclusions
High-risk pituitary adenomas are well-defined morphological types with clinically aggressive features. Precise histological classification requires immunohistochemistry for pituitary hormones and cytokeratins to identify high-risk adenoma types. In addition, assessment of predictive markers by immunohistochemistry plays an important clinical role in pathology, contributing to achieving the maximum of the expected effectiveness of treatment. Our aim in presenting the technical drawbacks of immunohistochemistry was to shed light on possible discrepancies in the outcome of therapy. In summary, immunohistochemistry should be carefully evaluated by an experienced pathologist.
References
Kaltsas GA, Nomikos P, Kontogeorgos G, Buchfelder M, Grossman AB (2005) Diagnosis and management of pituitary carcinomas. J Clin Endocrinol Metab 90(5):3089–3099. https://doi.org/10.1210/jc.2004-2231
Hansen TM, Batra S, Lim M, Burger PC, Salvatori R, Wand G, Quinones-Hinojosa A, Kleinberg L, Redmond KJ (2014) Invasive adenoma and pituitary carcinoma: a SEER database analysis. Neurosurg Rev 37(2):279–286. https://doi.org/10.1007/s10143-014-0525-y
Colao A, Grasso LF, Pivonello R, Lombardi G (2011) Therapy of aggressive pituitary tumors. Expert Opin Pharmacother 12(10):1561–1570. https://doi.org/10.1517/14656566.2011.568478
Di Ieva A, Rotondo F, Syro LV, Cusimano MD, Kovacs K (2014) Aggressive pituitary adenomas-diagnosis and emerging treatments. Nat Rev Endocrinol 10(7):423–435. https://doi.org/10.1038/nrendo.2014.64
Zacharia BE, Gulati AP, Bruce JN, Carminucci AS, Wardlaw SL, Siegelin M, Remotti H, Lignelli A, Fine RL (2014) High response rates and prolonged survival in patients with corticotroph pituitary tumors and refractory Cushing disease from capecitabine and temozolomide (CAPTEM): a case series. Neurosurgery 74(4):E447–E455; discussion E455. https://doi.org/10.1227/NEU.0000000000000251
Dai C, Liang S, Sun B, Kang J (2020) The progress of immunotherapy in refractory pituitary adenomas and pituitary carcinomas. Front Endocrinol (Lausanne) 11:608422. https://doi.org/10.3389/fendo.2020.608422
Osamura RY, Lopes MBS, Grossman A, Kontogeorgos G, Trouillas J (2017) Tumours of the pituitary gland. Introduction. In: Lloyd RV, Osamura RY, Klöppel G, Rosai J (eds) WHO Classification of Tumours of Endocrine Organs, vol 10, 4th edn. IARC, Lyon, p 13
Osamura R, Grossman A, Korbonits M, Kovacs K, Lopes MBS, Matsuro A, Trouillas J (2017) Pituitary gland: pituitary adenoma. In: Lloyd RV, Osamura RY, Klöppel G, Rosai J (eds) WHO Classification of Tumours of Endocrine Organs, vol 10, 4th edn. IARC, Lyon, pp 14–18
McCormack A, Dekkers OM, Petersenn S, Popovic V, Trouillas J, Raverot G, Burman P (2018) ESE survey collaborators. Treatment of aggressive pituitary tumours and carcinomas: results of a European Society of Endocrinology (ESE) survey. Eur J Endocrinol 178(3):265–276. https://doi.org/10.1530/EJE-17-0933
Trouillas J, Roy P, Sturm N, Dantony E, Cortet-Rudelli C, Viennet G, Bonneville JF, Assaker R, Auger C, Brue T et al (2013) A new prognostic clinicopathological classification of pituitary adenomas: a multicentric case-control study of 410 patients with 8 years post-operative follow-up. Acta Neuropathol 126:123–135. https://doi.org/10.1007/s00401-013-1084-y
Asioli S, Righi A, Iommi M, Baldovini C, Ambrosi F, Guaraldi F, Zoli M, Mazzatenta D, Faustini-Fustini M, Rucci P, Giannini C, Foschini MP (2019) Validation of a clinicopathological score for the prediction of post-surgical evolution of pituitary adenoma: retrospective analysis on 566 patients from a tertiary care centre. Eur J Endocrinol 180(2):127–134. https://doi.org/10.1530/EJE-18-0749
Guaraldi F, Zoli M, Righi A, Gibertoni D, Marino Picciola V, Faustini-Fustini M, Morandi L, Bacci A, Pasquini E, Mazzatenta D, Asioli S (2020) A practical algorithm to predict postsurgical recurrence and progression of pituitary neuroendocrine tumours (PitNET)s. Clin Endocrinol (Oxf) 93(1):36–43. https://doi.org/10.1111/cen.14197
Villa C, Vasiljevic A, Jaffrain-Rea ML, Ansorge O, Asioli S, Barresi V, Chinezu L, Gardiman MP, Lania A, Lapshina AM, Poliani L, Reiniger L, Righi A, Saeger W, Soukup J, Theodoropoulou M, Uccella S, Trouillas J, Roncaroli F (2019) A standardised diagnostic approach to pituitary neuroendocrine tumours (PitNETs): a European Pituitary Pathology Group (EPPG) proposal. Virchows Arch 475(6):687–692. https://doi.org/10.1007/s00428-019-02655-0
Asa SL, Asioli S, Bozkurt S, Casar-Borota O, Chinezu L, Comunoglu N, Cossu G, Cusimano M, Delgrange E, Earls P, Ezzat S, Gazioglu N, Grossman A, Guaraldi F, Hickman RA, Ikeda H, Jaffrain-Rea ML, Karavitaki N, Kraljević I, La Rosa S, Manojlović-Gačić E, Maartens N, McCutcheon IE, Messerer M, Mete O, Nishioka H, Oz B, Pakbaz S, Pekmezci M, Perry A, Reiniger L, Roncaroli F, Saeger W, Söylemezoğlu F, Tachibana O, Trouillas J, Turchini J, Uccella S, Villa C, Yamada S, Yarman S (2020) Pituitary neuroendocrine tumors (PitNETs): nomenclature evolution, not clinical revolution. Pituitary 23(3):322–325. https://doi.org/10.1007/s11102-019-01015-0
Ho KKY, Fleseriu M, Wass J, van der Lely A, Barkan A, Giustina A, Casanueva FF, Heaney AP, Biermasz N, Strasburger C, Melmed S (2019) A tale of pituitary adenomas: to NET or not to NET. Pituitary Society position statement. Pituitary 22:569–573. https://doi.org/10.1007/s11102-019-00988-2
Ho K, Fleseriu M, Kaiser U, Salvatori R, Brue T, Lopes MB, Kunz P, Molitch M, Camper SA, Gadelha M, Syro LV, Laws E, Reincke M, Nishioka H, Grossman A, Barkan A, Casanueva F, Wass J, Mamelak A, Katznelson L, van der Lely AJ, Radovick S, Bidlingmaier M, Boguszewski M, Bollerslev J, Hoffman AR, Oyesiku N, Raverot G, Ben-Shlomo A, Fowkes R, Shimon I, Fukuoka H, Pereira AM, Greenman Y, Heaney AP, Gurnell M, Johannsson G, Osamura RY, Buchfelder M, Zatelli MC, Korbonits M, Chanson P, Biermasz N, Clemmons DR, Karavitaki N, Bronstein MD, Trainer P, Melmed S (2021) Pituitary neoplasm nomenclature workshop: does adenoma stand the test of time? J Endocr Soc 5(3):bvaa205. https://doi.org/10.1210/jendso/bvaa205
Giustina A. Pituitary adenoma…nomen omen? (2021) Endocrine, Jun 10, Online ahead of print. https://doi.org/10.1007/s12020-021-02785-z
Kovacs K, Horvath E (1986) Tumors of pituitary gland. Atlas of tumor pathology, 2nd series, fascicle 21. AFIP, Washington (DC)
Sano T, Ohsims T, Yamada S (1991) Expression of glycoprotein hormones and intracytoplsmic distribution of cytokeratin in growth hormone-producing pituitary adenomas. Path Res Pract 187(5):530–533. https://doi.org/10.1016/S0344-0338(11)80135-4
Akirov A, Asa SL, Amer L, Shimon I, Ezzat S (2019) The clinicopathological spectrum of acromegaly. J Clin Med 8(11):1962. https://doi.org/10.3390/jcm8111962
Swanson AA, Erickson D, Donegan DM, Jenkins SM, Van Gompel JJ, Atkinson JLD, Erickson BJ, Giannini C (2021) Clinical, biological, radiological, and pathological comparison of sparsely and densely granulated somatotroph adenomas: a single center experience from a cohort of 131 patients with acromegaly. Pituitary 24(2):192–206. https://doi.org/10.1007/s11102-020-01096-2
Obari A, Sano T, Ohyama K, Kudo E, Qian ZR, Yoneda A, Rayhan N, Mustafizur Rahman M, Yamada S (2008) Clinicopathological features of growth hormone-producing pituitary adenomas: difference among various types defined by cytokeratin distribution pattern including a transitional form. Endocr Pathol 19(2):82–91. https://doi.org/10.1007/s12022-008-9029-z
Brzana J, Yedinak CG, Gultekin SH, Delashaw JB, Fleseriu M (2013) Growth hormone granulation pattern and somatostatin receptor subtype 2A correlate with postoperative somatostatin receptor ligand response in acromegaly: a large single center experience. Pituitary 16(4):490–498. https://doi.org/10.1007/s11102-012-0445-1
Asa SL (2011) Tumors of the pituitary gland. 2nd series. AFIP, Washington (DC)
Larkin S, Reddy R, Karavitaki N, Cudlip S, Wass J, Ansorge O (2013) Granulation pattern, but not GSP or GHR mutation, is associated with clinical characteristics in somatostatin-naive patients with somatotroph adenomas. Eur J Endocrinol 168(4):491–419. https://doi.org/10.1530/EJE-12-0864
Kiseljak-Vassiliades K, Xu M, Mills TS, Smith EE, Silveira LJ, Lillehei KO, Kerr JM, Kleinschmidt- DeMasters BK, Wierman ME (2015) Differential somatostatin receptor (SSTR) 1–5 expression and downstream effectors in histologic subtypes of growth hormone pituitary tumors. Mol Cell Endocrinol 5(417):73–83. https://doi.org/10.1016/j.mce.2015.09.016
Heng L, Liu X, Jia D, Guo W, Zhang S, Gao G, Gong L, Qu Y (2021) Preoperative prediction of granulation pattern subtypes in GH-secreting pituitary adenomas. Clin Endocrinol (Oxf) 95(1):134–142. https://doi.org/10.1111/cen.14465
Chatzellis E, Alexandraki KI, Androulakis II, Kaltsas G (2015) Aggressive pituitary tumors. Neuroendocrinol 101:87–104. https://doi.org/10.1159/000371806
Landis CA, Masters SB, Spada A, Pace AM, Bourne HR, Vallar L (1989) GTPase inhibiting mutations activate the alpha chain of Gs and stimulate adenylyl cyclase in human pituitary tumours. Nature 340(6236):692–696. https://doi.org/10.1038/340692a0
Kato M, Inoshita N, Sugiyama T, Tani Y, Shichiri M, Sano T, Yamada S, Hirata Y (2012) Differential expression of genes related to drug responsiveness between sparsely and densely granulated somatotroph adenomas. Endocr J 59(3):221–228. https://doi.org/10.1507/endocrj.ej11-0177
Mete O, Asa SL (2013) Therapeutic implications of accurate classification of pituitary adenomas. Sem Diagn Pathol 30(3):158–164. https://doi.org/10.1053/j.semdp.2013.06.002
Mayr B, Buslei R, Theodoropoulou M, Stalla GK, Buchfelder M, Schofl C (2013) Molecular and functional properties of densely and sparsely-granulated GH-producing pituitary adenomas. Eur J Endocrinol 169(4):391–400. https://doi.org/10.1530/EJE-13-0134
Potorac I, Petrossians P, Daly AF, Alexopoulou O, Borot S, Sahnoun-Fathallah M, Castinetti F, Devuyst F, Jaffrain-Rea ML, Briet C, Luca F, Lapoirie M, Zoicas F, Simoneau I, Diallo AM, Muhammad A, Kelestimur F, Nazzari E, Centeno RG, Webb SM, Nunes ML, Hana V, Pascal-Vigneron V, Ilovayskaya I, Nasybullina F, Achir S, Ferone D, Neggers SJ, Delemer B, Petit JM, Schöfl C, Raverot G, Goichot B, Rodien P, Corvilain B, Brue T, Schillo F, Tshibanda L, Maiter D, Bonneville JF, Beckers A (2016) T2-weighted MRI signal predicts hormone and tumor responses to somatostatin analogs in acromegaly. Endocr Relat Cancer 23(11):871–881. https://doi.org/10.1530/ERC-16-0356
Ezzat S, Kontogeorgos G, Redelmeier DA, Horvath E, Harris AG, Kovacs K (1995) In vivo responsiveness of morphological variants of growth hormone-producing pituitary adenomas to octreotide. Eur J Endocrinol 133(6):686–690. https://doi.org/10.1530/eje.0.1330686
Park YW, Kang Y, Ahn SS, Ku CR, Kim EH, Kim SH, Lee EJ, Kim SH, Lee SK (2020) Radiomics model predicts granulation pattern in growth hormone-secreting pituitary adenomas. Pituitary 23(6):691–700. https://doi.org/10.1007/s11102-020-01077-5
Batisse M, Raverot G, Maqdasy S, Durando X, Sturm N, Montoriol PF, Kemeny JL, Chazal J, Trouillas J, Tauveron I (2013) Aggressive silent GH pituitary tumor resistant to multiple treatments, including temozolomide. Cancer Invest 31(3):190–196. https://doi.org/10.3109/07357907.2013.775293
Wang Y, Li J, Tohti M, Hu Y, Wang S, Li W, Lu Z, Ma C (2014) The expression profile of Dopamine D2 receptor, MGMT and VEGF in different histological subtypes of pituitary adenomas: a study of 197 cases and indications for the medical therapy. J Exp Clin Cancer Res 33(1):56. https://doi.org/10.1186/s13046-014-0056-y
Zuhur SS, Tanik C, Karaman Ö, Velet S, Çil E, Öztürk FY, Özkayalar H, Müslüman AM, Altuntaş Y (2011) MGMT immunoexpression in growth hormone-secreting pituitary adenomas and its correlation with Ki-67 labeling index and cytokeratin distribution pattern. Endocrine 40(2):222–227. https://doi.org/10.1007/s12020-011-9485-y
Maiter D, Delgrange E (2014) Therapy of endocrine disease: the challenges in managing giant prolactinomas. Eur J Endocrinol 170(6):R213–R227. https://doi.org/10.1530/EJE-14-0013
Pérez Pinzón J, González-Devia D, Kattah Calderón W, López Panqueva RDP, Jiménez Hakim E (2019) Unusual course of an aggressive pituitary prolactinoma: case report and review of the literature. Case Rep Neurol 11(1):148–156. https://doi.org/10.1159/000499702
Kars M, Dekkers OM, Pereira AM, Romijn JA (2010) Update in prolactinomas. Neth J Med 68(3):104–112
Shimon I (2019) Giant prolactinomas. Neuroendocrinology 109(1):51–56. https://doi.org/10.1159/000495184
Delgrange E, Vasiljevic A, Wierinckx A, François P, Jouanneau E, Raverot G, Trouillas J (2015) Expression of estrogen receptor alpha is associated with prolactin pituitary tumor prognosis and supports the sex-related difference in tumor growth. Eur J Endocrinol 172(6):791–801. https://doi.org/10.1530/EJE-14-0990
Almalki MH, Aljoaib NN, Alotaibi MJ, Aldabas BS, Wahedi TS, Ahmad MM, Alshahrani F (2017) Temozolomide therapy for resistant prolactin-secreting pituitary adenomas and carcinomas: a systematic review. Hormones (Athens) 16(2):139–149. https://doi.org/10.14310/horm.2002.1729
Colao A, Sarno AD, Cappabianca P, Briganti F, Pivonello R, Somma CD, Faggiano A, Biondi B, Lombardi G (2003) Gender differences in the prevalence, clinical features and response to cabergoline in hyperprolactinemia. Eur J Endocrinol 148(3):325–331. https://doi.org/10.1530/eje.0.1480325
Sahakian N, Castinetti F, Dufour H, Graillon T, Romanet P, Barlier A, Brue T, Cuny T (2019) Clinical management of difficult to treat macroprolactinomas. Expert Rev Endocrinol Metab 14(3):179–192. https://doi.org/10.1080/17446651.2019.1596024
Salenave S, Ancelle D, Bahougne T, Raverot G, Kamenický P, Bouligand J, Guiochon-Mantel A, Linglart A, Souchon PF, Nicolino M, Young J, Borson-Chazot F, Delemer B, Chanson P (2015) Macroprolactinomas in children and adolescents: factors associated with the response to treatment in 77 patients. J Clin Endocrinol Metab 100(3):1177–1186. https://doi.org/10.1210/jc.2014-3670
Stratakis CA, Schussheim DH, Freedman SM, Keil MF, Pack SD, Agarwal SK, Skarulis MC, Weil RJ, Lubensky IA, Zhuang Z, Oldfield EH, Marx SJ (2000) Pituitary macroadenoma in a 5-year-old: an early expression of multiple endocrine neoplasia type 1. J Clin Endocrinol Metab 85(12):4776–4780. https://doi.org/10.1210/jcem.85.12.7064
Kontogeorgos G, Kapranos N, Tzavara I, Thalassinos N, Rologis D (2001) Monosomy of chromosome 11 in pituitary adenoma in a patient with familial multiple endocrine neoplasia type 1. Clin Endocrinol (Oxf) 54(1):117–120. https://doi.org/10.1046/j.1365-2265.2001.01031.x
Kovacs K, Horvath E, Syro LV, Uribe H, Penagos LC, Ortiz LD, Fadul CE (2007) Temozolomide therapy in a man with an aggressive prolactin-secreting pituitary neoplasm: morphological findings. Hum Pathol (1):185–189. Erratum in: Hum Pathol 38(3):526. https://doi.org/10.1016/j.humpath.2006.07.014
Syro LV, Uribe H, Penagos LC, Ortiz LD, Fadul CE, Horvath E, Kovacs K (2006) Antitumour effects of temozolomide in a man with a large, invasive prolactin-producing pituitary neoplasm. Clin Endocrinol (Oxf) 65(4):552–553. https://doi.org/10.1111/j.1365-2265.2006.02653.x
Halevy C, Whitelaw BC (2017) How effective is temozolomide for treating pituitary tumours and when should it be used? Pituitary 20(2):261–266. https://doi.org/10.1007/s11102-016-0745-y
Zampetti B, Simonetti G, Attanasio R, Silvani A, Cozzi R (2018) Effective long-term temozolomide rechallenge in a macroprolactinoma. Endocrinol Diabetes Metab Case Rep 18-0092. https://doi.org/10.1530/EDM-18-0092
Bengtsson D, Schrøder HD, Andersen M, Maiter D, Berinder K, Feldt Rasmussen U, Rasmussen ÅK, Johannsson G, Hoybye C, van der Lely AJ, Petersson M, Ragnarsson O, Burman P (2015) Long-term outcome and MGMT as a predictive marker in 24 patients with atypical pituitary adenomas and pituitary carcinomas given treatment with temozolomide. J Clin Endocrinol Metab 100(4):1689–1698. https://doi.org/10.1210/jc.2014-4350
Whitelaw BC, Dworakowska D, Thomas NW, Barazi S, Riordan-Eva P, King AP, Hampton T, Landau DB, Lipscomb D, Buchanan CR, Gilbert JA, Aylwin SJ (2012) Temozolomide in the management of dopamine agonist-resistant prolactinomas. Clin Endocrinol (Oxf) 76(6):877–886. https://doi.org/10.1111/j.1365-2265.2012.04373.x
McCormack AI, McDonald KL, Gill AJ, Clark SJ, Burt MG, Campbell KA, Braund WJ, Little NS, Cook RJ, Grossman AB, Robinson BG, Clifton-Bligh RJ (2009) Low 06-methylguanine-DNA methyltransferase [p1] (mgmt) expression and response to temozolomide in aggressive pituitary tumors. Clin Endocrinol (Oxf) 71(2):226–233. https://doi.org/10.1111/j.1365-2265.2008.03487.x
Murakami M, Mizutani A, Asano S, Katakami H, Ozawa Y, Yamazaki K, Ishida Y, Takano K, Okinaga H, Matsuno A (2011) A mechanism of acquiring temozolomide resistance during transformation of atypical prolactinoma into prolactin-producing pituitary carcinoma: case report. Neurosurg 68:E1761–E1767. https://doi.org/10.1227/NEU.0b013e318217161a
Scheithauer BW, Jaap AJ, Horvath E, Kovacs K, Lloyd RV, Meyer FB, Laws ER Jr, Young WF Jr (2000) Clinically silent corticotroph tumors of the pituitary gland. Neurosurgery 47(3):723–729; discussion 729–730. https://doi.org/10.1097/00006123-200009000-00039
Moshkin O, Syro LV, Scheithauer BW, Ortiz LD, Fadul CE, Uribe H, Gonzalez R, Cusimano M, Horvath E, Rotondo F, Kovacs K (2011) Aggressive silent corticotroph adenoma progressing to pituitary carcinoma: the role of temozolomide therapy. Hormones (Athens) 10(2):162–167. https://doi.org/10.14310/horm.2002.1307
Xu Z, Ellis S, Lee CC, Starke Lee Vance M, Lopes MB, Sheehan J (2014) Silent corticotroph adenomas after stereotactic radiosurgery: a case-control study. Int J Radiat Oncol Biol Phys 90(4):903–910. https://doi.org/10.1016/j.ijrobp.2014.07.013
Nishioka H, Inoshita N, Mete O, Asa SL, Hayashi K, Takeshita A, Fukuhara N, Yamaguchi-Okada M, Takeuchi Y, Yamada S (2015) The complementary role of transcription factors in the accurate diagnosis of clinically nonfunctioning pituitary adenomas. Endocr Pathol 26(4):349–355. https://doi.org/10.1007/s12022-015-9398-z
Thodou E, Argyrakos T, Kontogeorgos G (2007) Galectin-3 as a marker distinguishing functioning from silent corticotroph adenomas. Hormones (Athens) 6(3):227–232
Jin L, Riss D, Ruebel K, Kajita S, Scheithauer BW, Horvath E, Kovacs K, Lloyd RV (2005) Galectin-3 expression in functioning and silent ACTH-producing adenomas. Endocr Pathol 16(2):107–114. https://doi.org/10.1385/ep:16:2:107
Tateno T, Kato M, Tani Y, Oyama K, Yamada S, Hirata Y (2009) Differential expression of somatostatin and dopamine receptor subtype genes in adrenocorticotropin (ACTH)-secreting pituitary tumors and silent corticotroph adenomas. Endocr J 56(4):579–584. https://doi.org/10.1507/endocrj.k08e-186
Ben-Shlomo A, Schmid H, Wawrowsky K, Pichurin O, Hubina E, Chesnokova V, Liu NA, Culler M, Melmed S (2009) Differential ligand-mediated pituitary somatostatin receptor subtype signaling: implications for corticotroph tumor therapy. J Clin Endocrinol Metab 94(11):4342–4350. https://doi.org/10.1210/jc.2009-1311
Tanaka S, Yamamoto M, Morita M, Takeno A, Kanazawa I, Yamaguchi T, Yamada S, Inoshita N, Oki Y, Kurosaki M, Sugimoto T (2019) Successful reduction of ACTH secretion in a case of intractable Cushing’s disease with pituitary Crooke’s cell adenoma by combined modality therapy including temozolomide. Endocr J 66(8):701–708. https://doi.org/10.1507/endocrj.EJ18-0547
Felix IA, Horvath E, Kovacs K (1981) Massive Crooke’s hyalinization in corticotroph cell adenomas of the human pituitary: a histological, immunocytological and electron microscopic study of three cases. Acta Neurochir (Wien) 58(3–4):235–243. https://doi.org/10.1007/BF01407130
George DH, Scheithauer BW, Kovacs K, Horvath E, Young WF Jr, Lloyd RV, Meyer FB (2003) Crooke’s cell adenoma of the pituitary: an aggressive variant of corticotroph adenoma. Am J Surg Pathol 27(10):1330–1336. https://doi.org/10.1097/00000478-200310000-00005
Heaney AP (2011) Clinical review: pituitary carcinoma: difficult diagnosis and treatment. J Clin Endocrinol Metab 96(12):3649–3660. https://doi.org/10.1210/jc.2011-2031
Heaney A (2014) Management of aggressive pituitary adenomas and pituitary carcinomas. J Neurooncol 117(3):459–468. https://doi.org/10.1007/s11060-014-1413-6
Giri D, Roncaroli F, Sinha A, Didi M, Senniappan S (2017) Silent Crooke’s cell corticotroph adenoma of the pituitary gland presenting as delayed puberty. Endocrinol Diabetes Metab Case Rep 16-0153. https://doi.org/10.1530/EDM-16-0153
Asimakopoulou A, Tzanela M, Kontogeorgos KA, G, Tsagarakis S, (2014) Long-term remission in an aggressive Crooke cell adenoma of the pituitary, 18 months after discontinuation of treatment with temozolomide. Clin Case Rep 2(1):1–3. https://doi.org/10.1002/ccr3.39
Tatsi C, Stratakis CA (2020) Aggressive pituitary tumors in the young and elderly. Rev Endocr Metab Disord 21(2):213–223. https://doi.org/10.1007/s11154-019-09534-8
Ortiz LD, Syro LV, Scheithauer BW, Rotondo F, Uribe H, Fadul CE, Horvath E, Kovacs K (2012) Temozolomide in aggressive pituitary adenomas and carcinomas. Clinics (Sao Paulo, Brazil) 67(Suppl 1):119–123. https://doi.org/10.6061/clinics/2012(sup01)20
Hirohata T, Asano K, Ogawa Y, Takano S, Amano K, Isozaki O, Iwai Y, Sakata K, Fukuhara N, Nishioka H, Yamada S, Fujio S, Arita K, Takano K, Tominaga A, Hizuka N, Ikeda H, Osamura RY, Tahara S, Ishii Y, Kawamata T, Shimatsu A, Teramoto A, Matsuno A (2013) DNA mismatch repair protein (MSH6) correlated with the responses of atypical pituitary adenomas and pituitary carcinomas to temozolomide: the national cooperative study by the Japan Society for Hypothalamic and Pituitary Tumors. J Clin Endocrinol Metab 98(3):1130–1136. https://doi.org/10.1210/jc.2012-2924
Horvath E, Kovacs K, Smyth HS, Cusimano M, Singer W (2005) Silent adenoma subtype 3 of the pituitary-immunohistochemical and ultrastructural classification: a review of 29 cases. Ultrastruct Pathol 29(6):511–524. https://doi.org/10.1080/01913120500323514
Mete O, Gomez-Hernandez K, Kucharczyk W, Ridout R, Zadeh G, Gentili F, Ezzat S, Asa SL (2016) Silent subtype 3 pituitary adenomas are not always silent and represent poorly differentiated monomorphous plurihormonal Pit-1 lineage adenomas. Mod Pathol 29(2):131–142. https://doi.org/10.1038/modpathol.2015.151
Erickson D, Scheithauer B, Atkinson J, Horvath E, Kovacs K, Lloyd RV, Young WF Jr (2009) Silent subtype 3 pituitary adenoma: a clinicopathologic analysis of the Mayo Clinic experience. Clin Endocrinol (Oxf) 71(1):92–99. https://doi.org/10.1111/j.1365-2265.2008.03514.x
Osamura RY, Tahara S, Komatsubara K, Itoh Y, Kajiwara H, Kurotani R, Sanno N, Teramoto A (1999) Pit-1 positive alpha-subunit positive nonfunctioning human pituitary adenomas: a dedifferentiated GH cell lineage? Pituitary 1(3–4):269–271. https://doi.org/10.1023/a:1009954409469
Osamura RY, Egashira N, Kajiya H, Takei M, Tobita M, Miyakoshi T, Inomoto C, Takekoshi S, Teramoto A (2009) Pathology, pathogenesis and therapy of growth hormone (GH)-producing pituitary adenomas: technical advances in histochemistry and their contribution. Acta Histochem Cytochem 42(4):95–104. https://doi.org/10.1267/ahc.09004
Mete O, Asa SL (2012) Clinicopathological correlations in pituitary adenomas. Brain Pathol 22(4):443–453. https://doi.org/10.1111/j.1750-3639.2012.00599.x
Thodou E, Kontogeorgos G (2020) Somatostatin receptor profile in pituitary thyrotroph adenomas. Clin Neurol Neurosurg 195:105865. https://doi.org/10.1016/j.clineuro.2020.105865
Wang EL, Qian ZR, Yamada S, Rahman MM, Inosita N, Kageji T, Endo H, Kudo E, Sano T (2009) Clinicopathological characterization of TSH-producing adenomas: special reference to TSH-immunoreactive but clinically non-functioning adenomas. Endocr Pathol 20(4):209–220. https://doi.org/10.1007/s12022-009-9094-y
Kuhn JM, Arlot S, Lefebvre H, Caron P, Cortet-Rudelli C, Archambaud F, Chanson P, Tabarin A, Goth MI, Blumberg J, Catus F, Ispas S, Beck-Peccoz P (2000) Evaluation of the treatment of thyrotropin-secreting pituitary adenomas with a slow release formulation of the somatostatin analog lanreotide. J Clin Endocrinol Metab 85(4):1487–1491. https://doi.org/10.1210/jcem.85.4.6548
Rimareix F, Grunenwald S, Vezzosi D, Rivière LD, Bennet A, Caron P (2015) Primary medical treatment of thyrotropin-secreting pituitary adenomas by first-generation somatostatin analogs: a case study of seven patients. Thyroid 25(8):877–882. https://doi.org/10.1089/thy.2015.0041
Fealey ME, Scheithauer BW, Horvath E, Erickson D, Kovacs K, McLendon R, Lloyd RV (2010) MGMT immunoexpression in silent subtype 3 pituitary adenomas: possible therapeutic implications. Endocr Pathol 21(3):161–165. https://doi.org/10.1007/s12022-010-9120-0
Salehi F, Scheithauer BW, Kros JM, Lau Q, Fealey M, Erickson D, Kovacs K, Horvath E, Lloyd RV (2011) MGMT promoter methylation and immunoexpression in aggressive pituitary adenomas and carcinomas. J Neurooncol 104(3):647–657. https://doi.org/10.1007/s11060-011-0532-6
Patel YC (1999) Somatostatin and its receptor family. Front Neuroendocrinol 20(3):157–198. https://doi.org/10.1007/s10555-011-9293-0
Schmid HA, Schoeffter P (2004) Functional activity of the multiligand analog SOM230 at human recombinant somatostatin receptor subtypes supports its usefulness in neuroendocrine tumors. Neuroendocrinology 80(Suppl 1):47–55. https://doi.org/10.1159/000080741
Reubi JC (2003) Peptide receptors as molecular targets for cancer diagnosis and therapy. Endocr Rev 24(4):389–427. https://doi.org/10.1210/er.2002-0007
Mizutani G, Nakanishi Y, Watanabe N, Honma T, Obana Y, Seki T, Ohni S, Nemoto N (2012) Expression of somatostatin receptor (SSTR) subtypes (SSTR-1, 2A, 3, 4 and 5) in neuroendocrine tumors using real-time RT-PCR method and immunohistochemistry. Acta Histochem Cytochem 45(3):167–176. https://doi.org/10.1267/ahc.12006
Oda Y, Tanaka Y, Naruse T, Sasanabe R, Tsubamoto M, Funahashi H (2002) Expression of somatostatin receptor and effects of somatostatin analog on pancreatic endocrine tumors. Surg Today 32(8):690–694. https://doi.org/10.1007/s005950200128
Körner M, Waser B, Schonbrunn A, Perren A, Reubi JC (2012) Somatostatin receptor subtype 2a immunohistochemistry using a new monoclonal antibody selects tumors suitable for in vivo somatostatin receptor targeting. Am J Surg Pathol 36(2):242–252. https://doi.org/10.1097/PAS.0b013e31823d07f3
Stueven AK, Kayser A, Wetz C, Amthauer H, Wree A, Tacke F, Wiedenmann B, Roderburg C, Jann H (2019) Somatostatin analogues in the treatment of neuroendocrine tumors: past, present and future. Int J Mol Sci 20(12):3049. https://doi.org/10.3390/ijms20123049
Volante M, Brizzi MP, Faggiano A, La Rosa S, Rapa I, Ferrero A, Mansueto G, Righi L, Garancini S, Capella C, De Rosa G, Dogliotti L, Colao A, Papotti M (2007) Somatostatin receptor type 2A immunohistochemistry in neuroendocrine tumors: a proposal of scoring system correlated with somatostatin receptor scintigraphy. Mod Pathol 20(11):1172–1182. https://doi.org/10.1038/modpathol.3800954
Diakatou E, Alexandraki KI, Tsolakis AV, Kontogeorgos G, Chatzellis E, Leonti A, Kaltsas GA (2015) Somatostatin and dopamine receptor expression in neuroendocrine neoplasms: correlation of immunohistochemical findings with somatostatin receptor scintigraphy visual scores. Clin Endocrinol (Oxf) 83(3):420–428. https://doi.org/10.1111/cen.12775
Bush ZM, Longtine JA, Cunningham T, Schiff D, Jane JA Jr, Vance ML, Thorner MO, Laws ER Jr, Lopes MB (2010) Temozolomide treatment for aggressive pituitary tumors: correlation of clinical outcome with O(6)-methylguanine methyltransferase (MGMT) promoter methylation and expression. J Clin Endocrinol Metab 95(11):E280-290. https://doi.org/10.1210/jc.2010-0441
Raverot G, Sturm N, de Fraipont F, Muller M, Muller M, Salenave S, Caron P, Chabre O, Chanson P, Cortet-Rudelli C, Assaker R, Dufour H, Gaillard S, François P, Jouanneau E, Passagia JG, Bernier M, Cornélius A, Figarella-Branger D, Trouillas J, Borson-Chazot F, Brue T (2010) Temozolomide treatment in aggressive pituitary tumors and pituitary carcinomas: a French multicenter experience. J Clin Endocrinol Metab 95(10):4592–4599. https://doi.org/10.1210/jc.2010-0644
Syro LV, Rotondo F, Camargo M, Ortiz LD, Serna CA, Kovacs K (2018) Temozolomide and pituitary tumors: current understanding, unresolved issues, and future directions. Front Endocrinol (Lausanne) 9:318. https://doi.org/10.3389/fendo.2018.00318
Micko ASG, Wöhrer A, Höftberger R, Vila G, Marosi C, Knosp E, Wolfsberger S (2017) MGMT and MSH6 immunoexpression for functioning pituitary macroadenomas. Pituitary 20(6):643–653. https://doi.org/10.1007/s11102-017-0829-3
Kontogeorgos G, Thodou E, Koutourousiou M, Kaltsas G, Seretis A (2019) MGMT immunohistochemistry in pituitary tumors: controversies with clinical implications. Pituitary 22(6):614–619. https://doi.org/10.1007/s11102-019-00993-5
Kontogeorgos G, Thodou E (2019) Is MGMT the best marker to predict response of temozolomide in aggressive pituitary tumors? Alternative markers and prospective treatment modalities. Hormones (Athens) 18(4):333–337. https://doi.org/10.1007/s42000-019-00145-1
Kapranos N, Kontogeorgos G, Frangia K, Kokka E (1997) Effect of fixation on interphase cytogenetic analysis by direct fluorescence in situ hybridization on cell imprints. Biotech Histochem 72(3):148–151. https://doi.org/10.3109/10520299709082229
Micko ASG, Höftberger R, Wöhrer A, Millesi M, Knosp E, Wolfsberger S (2018) MGMT assessment in pituitary adenomas: comparison of different immunohistochemistry fixation chemicals. Pituitary 21(3):266–273. https://doi.org/10.1007/s11102-018-0862-x
McCormack AI, Wass JA, Grossman AB (2011) Aggressive pituitary tumours: the role of temozolomide and the assessment of MGMT status. Eur J Clin Invest 41(10):1133–1148. https://doi.org/10.1111/j.1365-2362.2011.02520.x
Dworakowska D, Grossman AB (2018) Aggressive and malignant pituitary tumours: state-of-the-art. Endocr Relat Cancer 25(11):R559–R575. https://doi.org/10.1530/ERC-18-0228
Ortiz LD, Syro LV, Scheithauer BW, Ersen A, Uribe H, Fadul CE, Rotondo F, Horvath E, Kovacs K (2012) Anti-VEGF therapy in pituitary carcinoma. Pituitary 15(3):445–449. https://doi.org/10.1007/s11102-011-0346-8
Touma W, Hoostal S, Peterson RA, Wiernik A, SantaCruz KS, Lou E (2017) Successful treatment of pituitary carcinoma with concurrent radiation, temozolomide, and bevacizumab after resection. J Clin Neurosci 41:75–77. https://doi.org/10.1016/j.jocn.2017.02.052
Cooper O, Mamelak A, Bannykh S, Carmichael J, Bonert V, Lim S, Cook-Wiens G, Ben-Shlomo A (2014) Prolactinoma ErbB receptor expression and targeted therapy for aggressive tumors. Endocrine 46(2):318–327. https://doi.org/10.1007/s12020-013-0093-x
Fukuoka H, Cooper O, Ben-Shlomo A, Mamelak A, Ren SG, Bruyette D, Melmed S (2011) EGFR as a therapeutic target for human, canine, and mouse ACTH-secreting pituitary adenomas. J Clin Invest 121(12):4712–4721. https://doi.org/10.1172/JCI60417
Ben-Shlomo A, Cooper O (2017) Role of tyrosine kinase inhibitors in the treatment of pituitary tumours: from bench to bedside. Curr Opin Endocrinol Diabetes Obes 24(4):301–305. https://doi.org/10.1097/MED.0000000000000344
Cooper O, Bonert VS, Rudnick J, Pressman BD, Lo J, Salvatori R, Yuen KCJ, Fleseriu M, Melmed S (2021) EGFR/ErbB2-targeting lapatinib therapy for aggressive prolactinomas. J Clin Endocrinol Metab 106(2):e917–e925. https://doi.org/10.1210/clinem/dgaa805
Cerovac V, Monteserin-Garcia J, Rubinfeld H, Buchfelder M, Losa M, Florio T, Paez-Pereda M, Stalla GK, Theodoropoulou M (2010) The somatostatin analogue octreotide confers sensitivity to rapamycin treatment on pituitary tumor cells. Can Res 70(2):666–674. https://doi.org/10.1158/0008-5472.CAN-09-2951
Sajjad EA, Zieliński G, Maksymowicz M, Hutnik Ł, Bednarczuk T, Włodarski P (2013) mTOR is frequently active in GH-secreting pituitary adenomas without influencing their morphopathological features. Endocr Pathol 24(1):11–19. https://doi.org/10.1007/s12022-012-9230-y
Donovan LE, Arnal AV, Wang SH, Odia Y (2016) Widely metastatic atypical pituitary adenoma with mTOR pathway STK11 (F298L) mutation treated with everolimus therapy. CNS Oncol 5(4):203–209. https://doi.org/10.2217/cns-2016-0011
Zhang D, Way JS, Zhang X, Sergey M, Bergsneider M, Wang MB, Yong WH, Heaney AP (2019) Effect of everolimus in treatment of aggressive prolactin-secreting pituitary adenomas. J Clin Endocrinol Metab 104(6):1929–1936. https://doi.org/10.1210/jc.2018-02461
Wang PF, Wang TJ, Yang YK, Yao K, Li Z, Li YM, Yan CX (2018) The expression profile of PD-L1 and CD8(+) lymphocyte in pituitary adenomas indicating for immunotherapy. J Neurooncol 139(1):89–95. https://doi.org/10.1007/s11060-018-2844-2
Mei Y, Bi WL, Greenwald NF, Du Z, Agar NY, Kaiser UB, Woodmansee WW, Reardon DA, Freeman GJ, Fecci PE, Laws ER Jr, Santagata S, Dunn GP, Dunn IF (2016) Increased expression of programmed death ligand 1 (PD-L1) in human pituitary tumors. Oncotarget 7(47):76565–76576
Hazrati SM, Aghazadeh J, Mohtarami F, Abouzari M, Rashidi A (2006) Immunotherapy of prolactinoma with a T helper 1 activator adjuvant and autoantigens: a case report. NeuroImmunoModulation 13(4):205–208. https://doi.org/10.1159/000100405
Lin AL, Jonsson P, Tabar V, Yang TJ, Cuaron J, Beal K, Cohen M, Postow M, Rosenblum M, Shia J, DeAngelis LM, Taylor BS, Young RJ, Geer EB (2018) Marked response of a hypermutated ACTH-secreting pituitary carcinoma to ipilimumab and nivolumab. J Clin Endocrinol Metab 103(10):3925–3930. https://doi.org/10.1210/jc.2018-01347
Giuffrida G, Ferraù F, Laudicella R, Cotta OR, Messina E, Granata F, Angileri FF, Vento A, Alibrandi A, Baldari S, Cannavò S (2019) Peptide receptor radionuclide therapy for aggressive pituitary tumors: a monocentric experience. Endocr Connect 8(5):528–535. https://doi.org/10.1530/EC-19-0065
Funding
This work was financially supported in part by the Pituitary Research Society.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research involving human participants and/or animals
This article does not contain studies with human participants or animals.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kontogeorgos, G., Thodou, E., Osamura, R.Y. et al. High-risk pituitary adenomas and strategies for predicting response to treatment. Hormones 21, 1–14 (2022). https://doi.org/10.1007/s42000-021-00333-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-021-00333-y