Abstract
MGMT promoter hypermethylation of aggressive pituitary adenomas and pituitary carcinomas and low protein expression are implicated in improved response to treatment with temozolomide (TMZ). The aim of the present study was to investigate MGMT promoter methylation and immunoexpression in an aggressive subset of pituitary adenomas and carcinomas. Our material consisted of 12 silent subtype 3 (SS3) adenomas, 10 primary carcinomas, and 4 disseminated metastases. Two different tissue samples of 7 of the 12 SS3 adenomas and all carcinomas were analyzed for MGMT promoter methylation and immunohistochemical expression of MGMT. Immunoexpression was assessed semi-quantitatively as a percentage of immunoreactive nuclei. Overall 33% of carcinomas exhibited homogenous MGMT methylation in tumor and metastatic specimens. Low immunohistochemical MGMT expression was noted in 50% of carcinomas. Overall, 42% of the SS3 adenomas exhibited MGMT promoter methylation. MGMT immunostaining was predominantly negative (92%), with homogenous immunostaining results across different samples. Whereas all the methylated SS3 adenomas had low MGMT immunoreactivity, five unmethylated adenomas exhibited absent/low MGMT expression. There was no relationship between methylation status and MGMT immunoexpression was not apparent. MGMT methylation and low immunohistochemical expression seen in a subset of carcinomas and SS3 adenomas, suggesting that a subset of tumors may respond to treatment with TMZ. Heterogeneous MGMT methylation status in SS3 adenomas and the lack of concordance between methylation and immunohistochemical expression of MGMT suggest complex regulatory mechanisms, highlighting the need for improved methods in the research on a correlation between MGMT changes and response to TMZ.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pituitary neoplasms are typically benign, slow-growing lesions. Only a subset behaves more aggressively and necessitates protracted treatment, including repeat surgery and adjuvant therapy, often with little success. Among more aggressive adenomas, the uncommon SS3 variant, a form of plurihormonal adenoma, is particularly so, tending to invade and recur, often necessitating multimodality treatment. Pituitary carcinomas, although extremely rare, pose a particular therapeutic challenge since treatment options for such multiply recurring, metastasizing pituitary tumors are limited.
Recent reports of the successful use of temozolomide (TMZ) as a therapeutic agent in the treatment of aggressive pituitary tumors refractory to other treatment modalities are promising [1–10]. Response to TMZ therapy is known to be closely related to expression levels of O-6-methylguanine-DNA methyltransferase (MGMT), a DNA repair enzyme [11, 12]. MGMT interrupts the therapeutic action of TMZ by removing the O6-guanine alkyl groups induced by treatment, thus repairing TMZ-induced DNA damage and counteracting its therapeutic effect. As such, low-level MGMT immunoexpression is correlated with TMZ response. Low MGMT levels are also associated with a longer disease-free and overall survival in gliomas [11, 12]. Although several recent reports of aggressive pituitary tumors successfully treated with TMZ have shown absent or low immunohistochemical expression of MGMT to be a factor, some patients whose tumors exhibited higher MGT levels also experienced clinical improvement and tumor reduction following TMZ treatment [13, 14].
MGMT gene promoter methylation is associated with suppressed MGMT protein levels [15]. Thus, it is thought to be one of the proposed mechanisms underlying absent or low MGMT expression. Indeed, MGMT methylation has been correlated with improved response to TMZ and longer patient survival [12]. MGMT promoter methylation attenuates tumoral binding of transcription factors and initiation of replication [16–19], resulting in absent or decreased levels of MGMT protein expression. Improved success of TMZ therapy has been well documented in glioblastoma (GBM) exhibiting MGMT promoter methylation [20]. Hegi et al. found MGMT methylation to be a favorable prognostic indicator in TMZ-treated patients with GBMs exhibiting promoter hypermethylation, survival being prolonged by 55% [12]. Preusser et al. also found MGMT promoter methylation status to be associated with longer patient survival [21]. Interestingly, MGMT promoter methylation status is also associated with higher tumor grade and invasiveness as well as poor prognosis in most human neoplasms studied. These include GBM, various sarcomas, non-small cell lung carcinoma, carcinomas of bladder, cervix, prostate and salivary gland, as well as other tumors including pituitary neoplasms [3, 22–29]. In cell culture, Nakasu et al. recently found loss of MGMT expression to be correlated to anaplastic transformation of astrocytomas [30]. Whether MGMT promoter methylation status and MGMT immunohistochemical expression are correlated remains unclear, with several studies reporting a positive association and other finding a lack of correlation [13, 14]. In one study of GBMs, MGMT methylation was associated with prolonged patient survival, but no such relationship with MGMT immunohistochemical expression was observed [21]. Similar observations were noted with respect to non-small cell lung carcinomas [31]. A recent report by Hamilton et al. found heterogeneous MGMT promoter methylation within the same GBM, when using formalin fixed paraffin embedded (FFPE) tumor tissue [32]. This raised questions about the reliability of current methods for the detection of MGMT methylation and treatment planning.
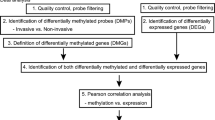
The aim of the present study was to investigate (a) MGMT promoter methylation status in SS3 adenomas and pituitary carcinoma, (b) immunohistochemical expression of MGMT in these two aggressive and therapy-resistant tumor groups, (c) the potential utility of TMZ as a therapeutic agent, (d) the correlation of MGMT immunoexpression and promoter methylation in terms of tumor homogeneity, and (e) examine MGMT methylation status and immunoexpression in matched primary and metastatic pituitary carcinomas.
Materials and methods
Our material consisted of 12 SS3 pituitary adenomas and 10 pituitary carcinomas. All tumors were identified in the Mayo Clinic Anatomic Pathology Database archives, Rochester, MN. All patients had undergone transsphenoidal resection of the primary between the years 1988 to 1994. The SS3 adenomas consisted of a subset of 12 adenomas in which ample tissue was available for methylation analysis, from our recent clinicopathological study [33]. Specimens were 10% neutral formalin-fixed, routinely processed, paraffin-embedded, and cut at 5 μm. Routine stains applied included hematoxylin and eosin (H&E), periodic acid-Schiff (PAS), and the Gomori reticulin method. Immunohistochemical characterization of adenohypophysial hormone content was performed using the streptavidin–biotin-peroxidase complex method seeking growth hormone (GH), prolactin (PRL), adrenocorticotropin (ACTH), thyroid stimulating hormone (TSH), luteinizing hormone (LH), follicle-stimulating hormone (FSH), as well as the alpha subunit of glycoprotein hormones. All SS3 adenomas had been ultrastructurally diagnosed [33]. Distant metastases were histologically documented in all carcinomas. MGMT immunodetection utilized a mouse monoclonal antibody (MT 3.1, Thermofisher, Fremont, CA; dilution 1:50). Antibody sources, clonality and dilutions as well as control methods have been previously reported.
Patient and tumor characteristics for both the SS3 pituitary adenomas and carcinomas were retrieved from our previously reported studies [33, 34]. As previously reported, all tumors had been studied for MGMT immunoexpression [34, 35]. Seven of the 12 SS3 adenomas and 6 of the 10 carcinomas had sufficient tissue for determination of intratumoral heterogeneity, MGMT immunoexpression and of MGMT promoter methylation. Additionally, in 6 of the 10 carcinomas, both the primary tumor and the metastasis were available for IHC immunohistochemical study. In one carcinoma case, both the primary tumor and a brain metastasis were quantitatively sufficient for methylation analysis. In yet another carcinoma, methylation was analyzed in two different metastases (jugular lymph node and triceps muscle) (Table 1).
Microscopy
MGMT immunoreactivity was evaluated microscopically under 10 high-powered fields (×200) by three observers (FS, BWS, and KK). Areas of optimal immunoreactivity with highest tumoral and vascular MGMT staining and minimal background reactivity were considered representative and used to estimate percentage immunopositivity. MGMT immunostaining was assessed as a percent immunopositive tumoral nuclei; cytoplasmic immunoreactivity was regarded as non-specific. Percentages registered were <10%, 10–25%, 25–50%, 50–75%, or 75%.
Methylation-Specific Multiplex Ligation-Dependent Probe Amplification (MS-MLPA) for MGMT
The MS-MLPA probe mix used (ME011; MRC Holland, Amsterdam, the Netherlands) includes 21 probe sequences containing a HhaI recognition site, which yields information about the methylation status of the target sequences. In addition, eight control probe sequences are used which are not influenced by the methylation-sensitive restriction enzyme HhaI digestion. The probes containing a HhaI recognition site should only generate a signal if the DNA target is methylated and cannot be digested. The probe mix has been developed to detect CpG island methylation of six mismatch repair genes and includes three specific probes for semiquantitative hypermethylation detection of the MGMT promoter region. This MS-MLPA assay for MGMT promoter hypermethylation of gliomas was performed as described earlier by Jeuken et al. with minor modifications [36]. For fragment analysis, PCR products were separated by capillary gel electrophoresis (ABI PRISM 3130xl, Applied Biosystems, Foster City, CA, USA) and quantified using the GeneMarker software version 1.7 (SoftGenetics, State College, PA, USA).
MS-MLPA data analysis
The MS-MLPA results were normalized by dividing the peak height of each MGMT probe signal by the mean peak height of the eight control fragments within the same sample. To estimate the fraction of methylated MGMT promoter DNA, normalized values of each MGMT probe of digested DNA samples were divided by normalized values of corresponding undigested DNAs. Methylation analyses were performed in duplicate and the average ratios of both experiments for each probe were calculated. For the promoter hypermethylation detection of MGMT, we used the MGMT 2 probe from the probe mix only. This probe is located near the widely used CpG island region for MGMT promoter hypermethylation detection by Methylation-Specific PCR (MS-PCR), and hypermethylation of this region has been found to be an independent predictor for the response to TMZ in gliomas [12, 20, 37, 38]. Beside that, the MGMT 2 probe had the best assay reproducibility in our hands (Spearman’s rho 0.658, P < 0.001) in comparison with the two other MGMT probes (MGMT 1 probe Spearman’s rho 0.448, P = 0.032 and MGMT 3 probe Spearman’s rho 0.431, P = 0.040). When the MGMT digested/MGMT undigested ratio of probe MGMT 2 is below 0.30, the MGMT promoter fragment is considered non-methylated as described earlier by Worsham et al. and Chen et al. for their MS-MLPA assay [39, 40].
Statistical analysis methods
To investigate correlations between MGMT immunoexpression and promoter methylation status as well as potential associations between patient age, sex, tumor recurrence and invasiveness, statistical analyses applied test included Pearson correlation, Student’s t-test, and Fisher’s exact test in the SPSS statistical program.
Results
Clinical data
Carcinomas
Based on availability of sufficient tissue for methylation analysis, 10 of 30 carcinomas were included in the study. Pituitary carcinoma diagnosis was made upon histologic documentation of metastases involving a variety of sites, including brain, tentorium, spinal cord, vertebrae, jugular lymph nodes, oral submucosa, buccal mucosa, liver, ovaries, sternocleidomastoid and triceps muscles, and the femur. Average time to diagnosis of metastatic sites was 6.7 years (median, 5; range, 1–16 years). The hormonal immunophenotype of the carcinomas included 5 PRL, 3 ACTH, 1 GH, and 1 TSH-producing tumor. Further clinicopathologic data regarding these cases may be found in Lau et al. [34].
Silent Subtype III
The 12 SS3 adenomas studied included tumors of eight male and four female patients (mean age, 35 years; median, 34; range, 17–74). Three of the 12 SS3 adenomas studied presented as “particularly aggressive” tumors based on the large size (≥4 cm) and at least one of the following parameters: multiple pituitary surgeries, external beam radiation therapy, and persistence of tumor despite multimodality treatment. One patient had multiple endocrine neoplasia type 1 (MEN1), presenting with pituitary tumor, hyperparathyroidism, and multiple neuroendocrine pancreatic tumors. Symptoms upon presentation of the SS3 adenomas included mass effect as well as endocrine dysfunction (Table 2). Hypopituitarism, including adrenal insufficiency (3/12) and hypogonadism (5/12), was found in 6 of 12 patients (Table 2). As expected, no preoperative diabetes insipidus was noted. One incidentally discovered SS3 adenoma was included in the study. Further information regarding this series is summarized in a previously published study of our series of SS3 adenomas. [33].
Measuring greater than 2 cm, all 12 SS3 pituitary adenomas were macroadenomas. Intraoperatively and/or by neuroimaging (MRI/CT) invasion of dura, cavernous sinus and/or sphenoid sinus was evident in seven cases. A complete transsphenoidal resection was achieved in eight instances. Postoperatively, 1 patient had a CSF leak, which was managed successfully. Reversal of hypopituitarism was noted in 3 patients, but 4 patients developed postoperative hypopituitarism. At 5 years follow-up, 2 patients were found to have recurrent tumor, which necessitated repeat surgery after a latency of 4 years in both instances. Of the remaining 10 patients, 6 had persistent tumor, necessitating adjuvant radiation and/or medical therapy. Radiation therapy was administered in 6 patients, one of which was treated prophylactically to prevent tumor recurrence.
Molecular data
Carcinomas
In 2 of 10 cases, MGMT promoter methylation was investigated in two different specimens, i.e. from different metastatic sites where available. Fully 9 of the 10 specimens exhibited homogenous tumoral methylation (Table 2). Three of the nine (33%) pituitary carcinomas demonstrated MGMT promoter methylation; six tumors were unmethylated and one yielded no results. In two cases, methylation status was identical in primary tumors and their respective metastases both being unmethylated.
MGMT immunoexpression was low (<10%) in five specimens and high, defined as >10% in five carcinomas (range 0–90%). Similar to the observed promoter methylation homogeneity, MGMT immunostaining strengths (low vs. high) were consistent between different sections of the same specimen studied. In only one instance, liver metastases exhibited variable MGMT immunoreactivity (5% in one liver metastasis and 35% in two others) (Table 1). In two cases wherein ample tissue was available, MGMT immunostaining was consistent in the primary pituitary carcinoma and/or their distant metastases (Table 1). Promoter methylation was present in two cases with strong MGMT immunostaining. In addition, four of the unmethylated carcinomas demonstrated weak MGMT immunoreactivity. Thus, the Chi-squared test revealed no statistically significant correlation between methylation status and MGMT immunostaining (Table 3).
SS3 pituitary adenomas
Overall, MGMT promoter methylation was observed in 2 of 12 (16.7%) of SS3 adenomas, 6 adenomas exhibiting an unmethylated promoter, and 3 showing methylation heterogeneity in samples of the same tumor (Table 2). Inclusive of the three adenomas exhibiting heterogeneous methylation, fully 42% of SS3 pituitary adenomas showed promoter methylation. In 7 of the 12 tumors studied, two different paraffin embedded samples were available for promoter methylation analysis. Of these, three exhibited heterogeneous methylation status (Table 2). One of the three clinically more aggressive SS3 pituitary adenomas demonstrated lack of promoter methylation, whereas the other two showed heterogeneous methylation status.
MGMT immunohistochemical staining was negative/low in 11/12 SS3 adenomas, 10 being fully negative. In one tumor, the MGMT immunostaining index was 20%, a value considered high. All three of the clinically aggressive SS3 adenomas displayed absent/low MGMT immunoreactivity. Immunohistochemical staining being low in five of the methylated and six of the unmethylated tumors, there was no association between the two parameters.
Correlations
By Fisher’s exact test, no correlation was found between methylation status and gender, but there was a preponderance of females among methylated carcinomas (3 of 4) and among unmethylated SS3 adenomas (4 of 5). Immunoexpression of MGMT did not differ significantly between males and females, although of the four tumors with higher MGMT immunopositivity, three were in female patients. No correlation was found between patient age and methylation status in either tumor type.
With respect to endocrine activity of the tumors, there was no preponderance of MGMT promoter methylation in PRL versus ACTH carcinomas. Similarly, SS3 pituitary adenomas showed variable promoter methylation and MGMT staining across their various hormone immunoprofiles.
In the one case, both the primary pituitary carcinoma and its brain metastasis showed identical MGMT promoter methylation status (unmethylated).
Discussion
The present study resulted in several key findings. These included (a) MGMT promoter methylation occurs in a significant subset of pituitary carcinomas and SS3 adenomas, (b) among carcinomas, MGMT promoter methylation status in primary lesions and their respective metastases, carcinomas demonstrate an identical methylation status, (c) MGMT promoter methylation status is homogenous in paraffin-embedded tissue of carcinomas, but not in SS3 pituitary adenomas, (d) methylation status is not concordant with MGMT immunoexpression, (e) MGMT immunoreactivity is primarily negative in most SS3 adenomas.
Epigenetic silencing of MGMT via methylation of its promoter is associated with higher tumor grade and with prognosis in several human neoplasms [3, 22–29]. Accordingly, we report MGMT promoter methylation in 33% of pituitary carcinomas and in 42% of SS3 adenomas. Our results indicate higher rates of MGMT immunonegativity than those reported by Bello et al. who found 22% of 23 non-functioning adenomas and 25% of 12 functioning adenomas to exhibit MGMT promoter methylation. Whether the methylated tumors were particularly aggressive or not was not stated, but the differences observed by us may be due to the aggressive nature of the subset of adenomas included in our study. In keeping with our findings, Raverot et al. recently reported MGMT methylation in 2 of 7 (43%) of aggressive pituitary adenoma/carcinomas examined [14]. On the other hand, McCormack et al. found MGMT promoter methylation in only 4 of 46 (9%) of nonfunctioning pituitary adenomas studied; no data regarding aggressive tumoral behavior and its relation to MGMT methylation was available [41].
Our results are also in keeping with most studies showing MGMT epigenetic silencing in higher grade and more aggressive tumors arising outside the pituitary gland [22, 23]. Piperi et al. reported MGMT promoter methylation in 59% of the 17 GBMs studied, and that a correlation existed between methylation status and patient survival, thus suggesting methylation is a prognostic indicator [22]. Similarly, Kim et al. observed MGMT promoter hypermethylation in 34% of the 63 soft tissue sarcomas, there being a strong correlation with tumor stage, grade, and aggressive behavior [23]. We have shown considerable MGMT promoter methylation in at least 50% of SS3 adenomas, tumors behaving more aggressively than other pituitary adenoma subtypes. This is entirely in keeping with the role of MGMT in DNA damage repair, tumor development and progression pathways [42]. Lastly, the recent finding of MGMT promoter methylation in 33% of a series of carcinomas investigated is in accordance with prior studies of human carcinomas [43].
Our results are promising as MGMT promoter methylation status has been shown to be a positive prognostic indicator in TMZ therapy of glioblastomas [12]. It is of note, however, that a subset of these tumors not methylated do respond to TMZ therapy, an observation challenging the notion that MGMT promoter methylation as an indication for TMZ treatment. Indeed, two recent studies of MGMT promoter methylation and TMZ response in eight aggressive adenomas and pituitary carcinomas found no association between promoter methylation status and TMZ response [13, 14]. Thus, our findings must be interpreted with caution. The validity of MGMT promoter methylation in the selection of patients for TMZ treatment remains controversial and an active area of research.
Frequently proposed explanations for this observed disparity are two-fold. Firstly, heterogeneous MGMT methylation within tumors confounds sampling of tissue for methylation determination. Secondly, technical limitations of promoter methylation analysis in formalin-fixed, paraffin-embedded tissue since DNA changes may be induced by tissue processing [32]. The recent study of Hamilton et al. compared MGMT promoter methylation status in frozen and paraffin-embedded tumor tissue using three different tumor samples obtained by stereotactic biopsy. The authors found MGMT methylation status to be heterogeneous in one paraffin-embedded tissue using MS-PCR, whereas frozen tumor tissue yielded homogenous methylation status regardless of biopsy site [32]. Furthermore, 4 of the 12 GBMs studied showed inconsistent promoter methylation status when comparing frozen and paraffin-embedded tumor samples. These findings are in keeping with the report of [44], demonstrating inconsistent MGMT promoter methylation status in 2 of 14 tumors examined when both frozen and formalin-fixed, paraffin-embedded tissue from different tumor sites were assessed. Our report of heterogeneous intra-tumoral MGMT methylation status in 3 of the 12 formalin-fixed, paraffin-embedded SS3 adenomas is in keeping with these various reports, and underscores the need to develop a uniform, reliable MGMT methylation detection technique. The answer may lie in utilization of frozen tissue. Indeed, it is reassuring that frozen samples yield consistent results in many studies of GBMs. Corroborating the findings of Hamilton et al., Cao et al. observed consistent methylation results in frozen biopsy samples from 37 sites in 12 GBMs [45]. Grasbon-Frodl et al. also found homogenous inter-sample methylation status using frozen tissue from 25 GBMs [46]; intra-sample methylation was heterogeneous in only one instance. As well, Parkinson et al. showed predominantly intra-tumoral homogeneity in 7 GBMs examined, with 2 MGMT methylation sites exhibiting variable methylation status in frozen samples [47]. Thus, it appears that frozen tumor tissue yields more homogenous MGMT promoter methylation results than formalin-fixed, paraffin-embedded tumor samples. To our knowledge, no such investigation of pituitary tumors has been undertaken.
Our finding of heterogeneous MGMT methylation in a number of pituitary tumors studied highlights the need for multi-sampling of tumor tissue. The present study found that in 3 of the 16 pituitary carcinoma/adenomas (19%) wherein two tumor samples were assessed, promoter methylation was heterogeneous; all three were SS3 adenomas. Whereas MGMT promoter methylation heterogeneity in GBM has been reported by several investigators, only one such study focused upon pituitary tumors, namely nonfunctioning adenomas [41]. Our findings are in keeping with those of McCormack et al. who found four methylated non-functioning pituitary adenomas all formalin-fixed and paraffin-embedded to be heterogeneously so [41]. Furthermore, we draw attention to technical limitations of the MSP method that may underlie false negative results. For example, Kitange et al. reported the presence of nearly 100 potential MGMT methylation CpG dinucleotide sites, of which the MSP-PCR method detects only those near the transcription initiation site [48]. This finding underscores the need for more sensitive methylation detection techniques. A cell culture investigation of pituitary adenoma cell lines response to treatment with TMZ showed differential therapeutic effect in the three cell lines examined [49]. It will be important to determine MGMT methylation status and immunohistochemical expression in such cell lines to establish whether a relationship exists between TMZ efficacy and MGMT methylation and/or protein status. It is possible that the mechanism of TMZ response in pituitary tumors is different from that seen in GBMs, and more detailed cellular and clinical studies are needed to elucidate on the pathways via which TMZ elicits its therapeutic effects in pituitary tumors.
In addition to its potential value as a therapeutic indicator and prognostic marker, MGMT methylation status is implicated in tumorigenesis. To investigate the role of MGMT methylation in tumor metastasis, we examined methylation status in primary pituitary carcinomas and their respective metastasis to several tissues, finding for the first time that MGMT methylation status is consistent in matched primary and disseminated metastases. Our findings are concordant with those of Wu et al., who recently observed consistent MGMT methylation status between primary and metastatic lung carcinomas [43]. Although primary and metastatic tumors are shown to be heterogeneous in their molecular profiles [43, 50, 51] we found that MGMT methylation (2 of 2 cases) and immunoexpression (4 of 5 cases) were concordant in the investigated primary carcinomas and their metastases. To our knowledge, only one other study has examined primary and metastatic pituitary carcinoma in terms of molecular profiles [52]. Zahedi et al. found that an ACTH primary carcinoma and its metastases differed in their clonal composition. The metastases demonstrated a loss-to-retention pattern at two distinct loci (IFNA and D22S156) compared to the primary pituitary carcinoma [52]. Clearly, further molecular characterization of primary and metastatic pituitary carcinomas will shed light on the mechanisms involved in pituitary tumorigenesis, progression, and metastasis.
Immunohistochemical detection of MGMT has been explored as a rapid means of predicting response to treatment with TMZ in patients with GBMs as well as small numbers of pituitary adenomas and carcinomas. We report absent or low (<10%) MGMT immunoexpression in 5 of 10 pituitary carcinomas and in 8 of 12 SS3 adenomas, figures considerably higher than those reported in two other series of pituitary adenomas. Previously, our group found MGMT immunonegativity in 78% of the 23 SS3 adenomas studied [35]. We believe our frequent finding of particularly low-level MGMT expression compared to others is a reflection of the more aggressive nature of SS3 adenomas comprising the bulk of tumors in our study [3, 41, 53]. Indeed, several reports have found particularly low levels of MGMT immunostaining in more aggressive tumors [43].
Widhalm et al. [53] found absent or low MGMT immunoreactivity to be present in 50% of pituitary tumors re-growing following surgical removal whereas only 24% of tumors not undergoing postoperative growth had low MGMT immunoexpression. Similarly, Takeshita et al. found absent/low MGMT immunopositivity in all 7 Crooke’s cell adenomas as studied compared to 25% of conventional ACTH-secreting pituitary adenomas. Crooke cell pituitary adenomas are a particularly aggressive subset of corticotrophic tumors presenting with Cushing disease [3]. It is of note that lower MGMT immunoexpression was correlated with shorter time to re-operation among re-growing tumors. On the other hand, such an association was not found by McCormack et al. in their investigation of MGMT immunoexpression in 88 pituitary adenomas; the authors found 13% of all tumors to show low MGMT immunoexpression but no association with tumor recurrence or invasiveness. It was noted, however, that PRL adenomas showed significantly lower MGMT immunoreactivity than other adenoma subtypes, a finding in keeping with their more aggressive behavior [43].
In summary, our finding of more frequent low-level MGMT immunoreactivity in aggressive and metastatic pituitary tumors is in accordance with most reports, and suggests fundamental molecular differences between indolent and aggressive tumors. Whether MGMT immunoexpression levels are causal or secondary to tumor progression remains unclear and requires further investigation. Regardless, low MGMT immunoreactivity is suggestive of a successful response to TMZ treatment. Although case reports and small series of TMZ-treated pituitary tumors have shown an association between TMZ response and low-level MGMT immunoreactivity, this is not always the case [1–10]. At the time of the present study, we retrieved 12 reported cases and a series of 8 patients with aggressive pituitary neoplasms where MGMT staining and TMZ treatment results were reported. Of these cases, 5 had significant MGMT immunoreactivity, but a positive response to TMZ treatment as determined by tumor shrinkage and clinical improvement [5]. In one instance, an oncocytic gonadotroph adenoma showing 30–50% MGMT immunoreactivity underwent shrinkage with clinical improvement after treatment [4]. On the other hand, a GH-secreting pituitary tumor showing strong MGMT was associated with a lack of response to TMZ therapy [41].
Preusser et al. [21] reported significant inter-observer variability as a factor affecting validity of MGMT immunoexpression estimates as a prognostic factor in their study of 146 GBM patients treated with TMZ. In addition, they reported a lack of correlation between MGMT methylation status and immunoreactivity [21]. Our study also found that methylation status is not closely associated with MGMT immunoexpression; 2 of the 3 methylated carcinomas showed strong MGMT immunopositivity and 6 unmethylated SS3 adenomas showed absent or low-level MGMT immunopositivity. The discordance between MGMT methylation status and protein immunoexpression may be due either to technical factors outlined or to as yet unknown regulatory molecular mechanisms. For example, NF-kappa-B was recently found to regulate MGMT expression independent of MGMT promoter methylation status [54]. In addition, p53 regulates MGMT protein expression in human astrocytic glioma cells regardless of its methylation status [55]. A clear understanding of MGMT regulatory mechanisms is essential in order to optimize the use of temozolomide as a therapeutic agent.
That MGMT methylation is not closely correlated with its protein expression as detected by immunohistochemistry is not surprising given the outlined issues regarding technical considerations, including tissue sampling and fixation, as well as the sensitivity of MSP in the detection of MGMT methylation. There may be yet unknown MGMT methylation and/or expression regulatory mechanisms that result in its variable expression profiles. The issue of the utility of MGMT immunohistochemical expression as a predictive factor for treatment with TMZ remains an active area of research.
In summary, the present study is the first to show concordant methylation status in the one case of the primary and metastatic pituitary carcinoma examined. Whether MGMT plays a direct role in tumor metastasis remains to be elucidated.
References
Byrne S, Karapetis C, Vrodos N (2009) A novel use of temozolomide in a patient with malignant prolactinoma. J Clin Neurosci 16:1694–1696
Hagen C, Schroeder HD, Hansen S, Hagen C, Andersen M (2009) Temozolomide treatment of a pituitary carcinoma and two pituitary macroadenomas resistant to conventional therapy. Eur J Endocrinol 161:631–637
Takeshita A, Inoshita N, Taguchi M, Okuda C, Fukuhara N, Oyama K, Ohashi K, Sano T, Takeuchi Y, Yamada S (2009) High incidence of low O(6)-methylguanine DNA methyltransferase expression in invasive macroadenomas of Cushing’s disease. Eur J Endocrinol 161:553–559
Syro LV, Scheithauer BW, Ortiz LD, Fadul CE, Horvath E, Rotondo F, Kovacs K (2009) Effect of temozolomide in a patient with recurring oncocytic gonadotrophic pituitary adenoma. Hormones (Athens) 8:303–306
Syro LV, Uribe H, Penagos LC, Ortiz LD, Fadul CE, Horvath E, Kovacs K (2006) Antitumour effects of temozolomide in a man with a large, invasive prolactin-producing pituitary neoplasm. Clin Endocrinol (Oxf) 65:552–553
Moyes VJ, Alusi G, Sabin HI, Evanson J, Berney DM, Kovacs K, Monson JP, Plowman PN, Drake WM (2009) Treatment of Nelson’s syndrome with temozolomide. Eur J Endocrinol 160:115–119
Mohammed S, Kovacs K, Mason W, Smyth H, Cusimano MD (2009) Use of temozolomide in aggressive pituitary tumors: case report. Neurosurgery 64:E773–E774; discussion E774
Debono M, Bridgewater C, Ross R, Newell-Price J (2008) Treating an aggressive prolactinoma in a patient with MEN 1: beneficial response to temozolomide. Endocr Abstr 15:188
Kovacs K, Horvath E, Syro LV, Uribe H, Penagos LC, Ortiz LD, Fadul CE (2007) Temozolomide therapy in a man with an aggressive prolactin-secreting pituitary neoplasm: Morphological findings. Hum Pathol 38:185–189
Kovacs K, Scheithauer BW, Lombardero M, McLendon RE, Syro LV, Uribe H, Ortiz LD, Penagos LC (2008) MGMT immunoexpression predicts responsiveness of pituitary tumors to temozolomide therapy. Acta Neuropathol 115:261–262
Chinot OL, Barrie M, Fuentes S, Eudes N, Lancelot S, Metellus P, Muracciole X, Braguer D, Ouafik L, Martin PM, Dufour H, Figarella-Branger D (2007) Correlation between O6-methylguanine-DNA methyltransferase and survival in inoperable newly diagnosed glioblastoma patients treated with neoadjuvant temozolomide. J Clin Oncol 25:1470–1475
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, Bromberg JE, Hau P, Mirimanoff RO, Cairncross JG, Janzer RC, Stupp R (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003
Bush ZM, Longtine JA, Cunningham T, Schiff D, Jane JA Jr, Vance ML, Thorner MO, Laws ER Jr, Lopes MB (2010) Temozolomide treatment for aggressive pituitary tumors: correlation of clinical outcome with O6-methylguanine methyltransferase (MGMT) promoter methylation and expression. J Clin Endocrinol Metab 95:E280–290
Raverot G, Sturm N, de Fraipont F, Muller M, Salenave S, Caron P, Chabre O, Chanson P, Cortet-Rudelli C, Assaker R, Dufour H, Gaillard S, Francois P, Jouanneau E, Passagia JG, Bernier M, Cornelius A, Figarella-Branger D, Trouillas J, Borson-Chazot F, Brue T (2010) Temozolomide treatment in aggressive pituitary tumors and pituitary carcinomas: a French multicenter experience. J Clin Endocrinol Metab 95:4592–4599
Esteller M, Hamilton SR, Burger PC, Baylin SB, Herman JG (1999) Inactivation of the DNA repair gene O6-methylguanine-DNA methyltransferase by promoter hypermethylation is a common event in primary human neoplasia. Cancer Res 59:793–797
Soejima H, Zhao W, Mukai T (2005) Epigenetic silencing of the MGMT gene in cancer. Biochem Cell Biol 83:429–437
Pieper RO (1997) Understanding and manipulating O6-methylguanine-DNA methyltransferase expression. Pharmacol Ther 74:285–297
Tano K, Shiota S, Collier J, Foote RS, Mitra S (1990) Isolation and structural characterization of a cDNA clone encoding the human DNA repair protein for O6-alkylguanine. Proc Natl Acad Sci USA 87:686–690
Day RS III, Ziolkowski CH, Scudiero DA, Meyer SA, Lubiniecki AS, Girardi AJ, Galloway SM, Bynum GD (1980) Defective repair of alkylated DNA by human tumour and SV40-transformed human cell strains. Nature 288:724–727
Hegi ME, Diserens AC, Godard S, Dietrich PY, Regli L, Ostermann S, Otten P, Van Melle G, de Tribolet N, Stupp R (2004) Clinical trial substantiates the predictive value of O-6-methylguanine-DNA methyltransferase promoter methylation in glioblastoma patients treated with temozolomide. Clin Cancer Res 10:1871–1874
Preusser M, Charles Janzer R, Felsberg J, Reifenberger G, Hamou MF, Diserens AC, Stupp R, Gorlia T, Marosi C, Heinzl H, Hainfellner JA, Hegi M (2008) Anti-O6-methylguanine-methyltransferase (MGMT) immunohistochemistry in glioblastoma multiforme: observer variability and lack of association with patient survival impede its use as clinical biomarker. Brain Pathol 18:520–532
Piperi C, Themistocleous MS, Papavassiliou GA, Farmaki E, Levidou G, Korkolopoulou P, Adamopoulos C, Papavassiliou AG (2010) High incidence of MGMT and RARbeta promoter methylation in primary glioblastomas: association with histopathological characteristics, inflammatory mediators and clinical outcome. Mol Med 16:1–9
Kim JI, Suh JT, Choi KU, Kang HJ, Shin DH, Lee IS, Moon TY, Kim WT (2009) Inactivation of O6-methylguanine-DNA methyltransferase in soft tissue sarcomas: association with K-ras mutations. Hum Pathol 40:934–941
Jarmalaite S, Jankevicius F, Kurgonaite K, Suziedelis K, Mutanen P, Husgafvel-Pursiainen K (2008) Promoter hypermethylation in tumour suppressor genes shows association with stage, grade and invasiveness of bladder cancer. Oncology 75:145–151
Terra AP, Murta EF, Maluf PJ, Caballero OL, Brait M, Adad SJ (2007) Aberrant promoter methylation can be useful as a marker of recurrent disease in patients with cervical intraepithelial neoplasia grade III. Tumori 93:572–579
Williams MD, Chakravarti N, Kies MS, Maruya S, Myers JN, Haviland JC, Weber RS, Lotan R, El-Naggar AK (2006) Implications of methylation patterns of cancer genes in salivary gland tumors. Clin Cancer Res 12:7353–7358
Schagdarsurengin U, Gimm O, Dralle H, Hoang-Vu C, Dammann R (2006) CpG island methylation of tumor-related promoters occurs preferentially in undifferentiated carcinoma. Thyroid 16:633–642
Kawaguchi K, Oda Y, Saito T, Yamamoto H, Takahira T, Kobayashi C, Tamiya S, Tateishi N, Iwamoto Y, Tsuneyoshi M (2006) DNA hypermethylation status of multiple genes in soft tissue sarcomas. Mod Pathol 19:106–114
Brabender J, Usadel H, Metzger R, Schneider PM, Park J, Salonga D, Tsao-Wei DD, Groshen S, Lord RV, Takebe N, Schneider S, Holscher AH, Danenberg KD, Danenberg PV (2003) Quantitative O(6)-methylguanine DNA methyltransferase methylation analysis in curatively resected non-small cell lung cancer: associations with clinical outcome. Clin Cancer Res 9:223–227
Nakasu S, Fukami T, Jito J, Matsuda M (2007) Prognostic significance of loss of O6-methylguanine-DNA methyltransferase expression in supratentorial diffuse low-grade astrocytoma. Surg Neurol 68:603–608 discussion 608-9
Cooper WA, Kohonen-Corish MR, Chan C, Kwun SY, McCaughan B, Kennedy C, Sutherland RL, Lee CS (2008) Prognostic significance of DNA repair proteins MLH1, MSH2 and MGMT expression in non-small-cell lung cancer and precursor lesions. Histopathology 52:613–622
Hamilton MG, Roldan G, Magliocco A, McIntyre JB, Parney I, Easaw JC (2010) Determination of the methylation status of MGMT in different regions within glioblastoma multiforme. J Neurooncol. doi:10.1007/s11060-010-0307-5
Erickson D, Scheithauer B, Atkinson J, Horvath E, Kovacs K, Lloyd RV, Young WF Jr (2009) Silent subtype 3 pituitary adenoma: a clinicopathologic analysis of the Mayo Clinic experience. Clin Endocrinol (Oxf) 71:92–99
Lau Q, Scheithauer B, Kovacs K, Horvath E, Syro LV, Lloyd R (2010) MGMT immunoexpression in aggressive pituitary adenoma and carcinoma. Pituitary 13:367–379
Fealey ME, Scheithauer BW, Horvath E, Erickson D, Kovacs K, McLendon R, Lloyd RV (2010) MGMT immunoexpression in silent subtype 3 pituitary adenomas: possible therapeutic implications. Endocr Pathol 21:161–165
Jeuken JW, Cornelissen SJ, Vriezen M, Dekkers MM, Errami A, Sijben A, Boots-Sprenger SH, Wesseling P (2007) MS-MLPA: an attractive alternative laboratory assay for robust, reliable, and semiquantitative detection of MGMT promoter hypermethylation in gliomas. Lab Invest 87:1055–1065
Esteller M, Garcia-Foncillas J, Andion E, Goodman SN, Hidalgo OF, Vanaclocha V, Baylin SB, Herman JG (2000) Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med 343:1350–1354
Paz MF, Yaya-Tur R, Rojas-Marcos I, Reynes G, Pollan M, Aguirre-Cruz L, Garcia-Lopez JL, Piquer J, Safont MJ, Balana C, Sanchez-Cespedes M, Garcia-Villanueva M, Arribas L, Esteller M (2004) CpG island hypermethylation of the DNA repair enzyme methyltransferase predicts response to temozolomide in primary gliomas. Clin Cancer Res 10:4933–4938
Worsham MJ, Chen KM, Tiwari N, Pals G, Schouten JP, Sethi S, Benninger MS (2006) Fine-mapping loss of gene architecture at the CDKN2B (p15INK4b), CDKN2A (p14ARF, p16INK4a), and MTAP genes in head and neck squamous cell carcinoma. Arch Otolaryngol Head Neck Surg 132:409–415
Chen K, Sawhney R, Khan M, Benninger MS, Hou Z, Sethi S, Stephen JK, Worsham MJ (2007) Methylation of multiple genes as diagnostic and therapeutic markers in primary head and neck squamous cell carcinoma. Arch Otolaryngol Head Neck Surg 133:1131–1138
McCormack AI, McDonald KL, Gill AJ, Clark SJ, Burt MG, Campbell KA, Braund WJ, Little NS, Cook RJ, Grossman AB, Robinson BG, Clifton-Bligh RJ (2009) Low O6-methylguanine-DNA methyltransferase (MGMT) expression and response to temozolomide in aggressive pituitary tumours. Clin Endocrinol (Oxf) 71:226–233
Sharma S, Salehi F, Scheithauer BW, Rotondo F, Syro LV, Kovacs K (2009) Role of MGMT in tumor development, progression, diagnosis, treatment and prognosis. Anticancer Res 29:3759–3768
Wu PF, Kuo KT, Kuo LT, Lin YT, Lee WC, Lu YS, Yang CH, Wu RM, Tu YK, Tasi JC, Tseng HM, Tseng SH, Cheng AL, Lin CH (2010) O(6)-Methylguanine-DNA methyltransferase expression and prognostic value in brain metastases of lung cancers. Lung Cancer 68:484–490
Juillerat-Jeanneret L, Bernasconi CC, Bricod C, Gros S, Trepey S, Benhattar J, Janzer RC (2008) Heterogeneity of human glioblastoma: glutathione-S-transferase and methylguanine-methyltransferase. Cancer Invest 26:597–609
Cao VT, Jung TY, Jung S, Jin SG, Moon KS, Kim IY, Kang SS, Park CS, Lee KH, Chae HJ (2009) The correlation and prognostic significance of MGMT promoter methylation and MGMT protein in glioblastomas. Neurosurgery 65:866–875 discussion 875
Grasbon-Frodl EM, Kreth FW, Ruiter M, Schnell O, Bise K, Felsberg J, Reifenberger G, Tonn JC, Kretzschmar HA (2007) Intratumoral homogeneity of MGMT promoter hypermethylation as demonstrated in serial stereotactic specimens from anaplastic astrocytomas and glioblastomas. Int J Cancer 121:2458–2464
Parkinson JF, Wheeler HR, Clarkson A, McKenzie CA, Biggs MT, Little NS, Cook RJ, Messina M, Robinson BG, McDonald KL (2008) Variation of O(6)-methylguanine-DNA methyltransferase (MGMT) promoter methylation in serial samples in glioblastoma. J Neurooncol 87:71–78
Kitange GJ, Carlson BL, Mladek AC, Decker PA, Schroeder MA, Wu W, Grogan PT, Giannini C, Ballman KV, Buckner JC, James CD, Sarkaria JN (2009) Evaluation of MGMT promoter methylation status and correlation with temozolomide response in orthotopic glioblastoma xenograft model. J Neurooncol 92:23–31
Sheehan J, Rainey J, Nguyen J, Grimsdale R, Han S (2010) Temozolomide-induced inhibition of pituitary adenoma cells. J Neurosurg 114:354–358
Wu JM, Fackler MJ, Halushka MK, Molavi DW, Taylor ME, Teo WW, Griffin C, Fetting J, Davidson NE, De Marzo AM, Hicks JL, Chitale D, Ladanyi M, Sukumar S, Argani P (2008) Heterogeneity of breast cancer metastases: comparison of therapeutic target expression and promoter methylation between primary tumors and their multifocal metastases. Clin Cancer Res 14:1938–1946
Vecchi M, Confalonieri S, Nuciforo P, Vigano MA, Capra M, Bianchi M, Nicosia D, Bianchi F, Galimberti V, Viale G, Palermo G, Riccardi A, Campanini R, Daidone MG, Pierotti MA, Pece S, Di Fiore PP (2008) Breast cancer metastases are molecularly distinct from their primary tumors. Oncogene 27:2148–2158
Zahedi A, Booth GL, Smyth HS, Farrell WE, Clayton RN, Asa SL, Ezzat S (2001) Distinct clonal composition of primary and metastatic adrencorticotrophic hormone-producing pituitary carcinoma. Clin Endocrinol (Oxf) 55:549–556
Widhalm G, Wolfsberger S, Preusser M, Woehrer A, Kotter MR, Czech T, Marosi C, Knosp E (2009) O(6)-methylguanine DNA methyltransferase immunoexpression in nonfunctioning pituitary adenomas: are progressive tumors potential candidates for temozolomide treatment? Cancer 115:1070–1080
Lavon I, Fuchs D, Zrihan D, Efroni G, Zelikovitch B, Fellig Y, Siegal T (2007) Novel mechanism whereby nuclear factor kappaB mediates DNA damage repair through regulation of O(6)-methylguanine-DNA-methyltransferase. Cancer Res 67:8952–8959
Blough MD, Zlatescu MC, Cairncross JG (2007) O6-methylguanine-DNA methyltransferase regulation by p53 in astrocytic cells. Cancer Res 67:580–584
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salehi, F., Scheithauer, B.W., Kros, J.M. et al. MGMT promoter methylation and immunoexpression in aggressive pituitary adenomas and carcinomas. J Neurooncol 104, 647–657 (2011). https://doi.org/10.1007/s11060-011-0532-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-011-0532-6