Key summary points
Do patients receiving polypharmacy benefit from interventions by hospital pharmacists, individually or as part of a multidisciplinary team?
AbstractSection FindingsSome beneficial effects were found of pharmacist interventions in 15 of 26 studies, specifically on hospital readmission, visits to the emergency department and healthcare costs.
AbstractSection MessageEvidence in favour of hospital pharmacist interventions in polymedicated older patients is scarce. Well-designed studies, with clearly defined interventions, outcomes and follow-up times should be conducted in the future to define the role of pharmacists in the geriatric team.
Abstract
Purpose
To identify the evidence that supports the effect of interventions made by hospital pharmacists, individually or in collaboration with a multidisciplinary team, in terms of healthcare outcomes, a more effective utilization of resources and lower costs in older polymedicated inpatients.
Methods
We searched the following databases: MEDLINE, EMBASE and the Cochrane Library. We also conducted a hand search by checking the references cited in the primary studies and studies included in reviews identified during the process of research. Four review authors working by pairs searched for studies, extracted data, and drew up the results tables.
Results
Twenty-six studies were included in the review. In 13 of them pharmacists carried out their intervention exclusively while the patients were in hospital, whereas in 13 interventions were delivered during admission and after hospital discharge. Outcomes identified were mortality, length of stay, visits to the emergency department, readmissions and reported quality of life, among others. Pharmacist interventions were found to be beneficial in fifteen studies, specifically on hospital readmissions, visits to the emergency department and healthcare costs.
Conclusion
There is no hard evidence demonstrating the effectiveness of hospital pharmacist interventions in older polymedicated patients. Mortality does not show as a relevant outcome. Other health care outcomes, such as hospital readmissions, visits to the emergency department and healthcare costs, seem to be more relevant and amenable to change. Interventions that include pharmacists in multidisciplinary geriatric teams seem to be more promising that isolated pharmacist interventions. Interventions prolonged after hospital discharge seem to be more appropriate that interventions delivered only during hospital admission. Better-designed studies should be conducted in the future to provide further insight into the effect of hospital pharmacist interventions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
It was not until 1989 that Hepler and Strand introduced the term pharmaceutical care [1]. The new term brought about a major transformation in clinical pharmacy practice. From that moment onwards, the work of pharmacists is gradually transforming into a more cooperative and patient-centred effort aimed at obtaining specific and positive results to enhance patients’ quality of life (QoL). In this sense, close cooperation between clinical pharmacists and other healthcare specialists, especially physicians and nurses, and with patients and their relatives, are mandatory to succeed in many pharmaceutical interventions, beyond the usual role of pharmacist to ensure that patients properly take their medications as prescribed and avoid any harmful effects.
At first, the value of pharmacists was only measured through simple and intermediate outcomes such as reduction of medication errors [2], avoidance of drug misuse [3], prevention of adverse drug reactions [4], and minimization of the potential for unnecessary anticholinergic burden [5]. Furthermore, the benefits of pharmacist interventions were also measured in terms of cost savings and the generation of economic value [6,7,8]. This value was not related to pharmacists’ daily everyday activities, such as medication reconciliation, counselling, or drug review. Indeed, as pharmacists walked out their pharmacy departments and started to collaborate with other healthcare providers and to join multidisciplinary teams, their value started to become noteworthy. Pharmacist-led interventions in multidisciplinary teams in hospital settings seem to improve clinical outcomes [9]. For example, their work has a positive impact on clinical outcomes and healthcare-resource utilization, reducing the number of hospitals visits [10] and mortality [11], and improving QoL or other patient-reported outcomes [12]. Their value has also been recognised in the care of non-hospitalised patients [13], in long-term care settings [14], and even in the delivery of home visits [15, 16].
In the case of older patients, the contribution made by pharmacists could be significant. Ageing places individuals at risk of multi-morbidity due to associated physiological and pathological changes and increases their chances of being prescribed multiple medications [17]. This increases their risk of developing adverse reactions, drug-drug interactions or adherence problems, all of them issues that pharmacists feel comfortable dealing with. Ageing is also associated with pharmacokinetic and pharmacodynamic changes [18]. Drugs and their formulations usually differ in liberation, absorption, distribution, metabolism, and clearance patterns and pharmacists are the experts to consult. Moreover, tools have been developed to review treatments administered to older patients to make prescriptions safer and more effective [19, 20]. In this regard, pharmacists have demonstrated their skill in applying these tools [21, 22]. For all the reasons above, pharmacists are in a unique position to improve heath and QoL in this particular population. Although the literature is scarce in this regard, some systematic reviews have been conducted to look into the impact that pharmacists exert on the lives of older patients [8, 23, 24]. In general, studies in this area are of low-to-medium quality, and underpowered to estimate the contribution of pharmacists to older patients’ hard health outcomes such as mortality or hospital readmission, as many pharmacists fulfil their role as members of multidisciplinary teams. This issue remains clearly unexplored. Moreover, the exact interventions conducted by pharmacists in different studies are heterogeneous, which makes it difficult to determine which interventions produce the best results in complex older patients [25].
This scoping review seeks to identify and discuss the evidence that supports the effect of the interventions made by hospital pharmacists, either individually or as part of a multidisciplinary team, in terms of better healthcare outcomes, a more effective utilization of resources and lower costs in older polymedicated inpatients.
Methods
A scoping review was conducted according to the guidelines set out in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) extension for Scoping Reviews (PRISMA-ScR) [26].
First, the research question was formulated following the PICO(d) format, as shown in Table 1.
Literature search strategy
A search was launched in MEDLINE (through OvidSP, all PubMed), EMBASE (Elsevier), and the Cochrane Library (Wiley). All databases were searched from inception to the 3rd March 2020. The search strategy is described in Appendix 1. The search was not filtered by language.
We did not register a review protocol for the search.
Selection of studies and data extraction
Studies were selected based on the criteria established in the PICO question (Table 1).
Duplicate references across the different literature databases were deleted. Title and abstract screening were undertaken in pairs by four independent reviewers to detect studies matching the inclusion criteria. In a second round, full-text articles were reviewed by four reviewers working in pairs to obtain the final set of studies to be included. In addition, a manual search was performed by reviewing the references in the narrative or systematic reviews found in the literature search. Discrepancies were discussed and resolved by a third reviewer.
A data extraction sheet was designed to collect the information of interest from the included studies. A pilot extraction process was performed to test this extraction sheet. This was done by the reviewers that would subsequently perform the final extraction process. Once the data extraction sheet was ready, three of the review authors collected the data from the selected studies and filled out the extraction sheet. Two review authors summarised the collected information by grouping the results of the included studies by setting, intervention performed, and outcome assessed. No formal quality assessment of the included studies was carried out as this is not mandatory when conducting a scoping review.
Results
Results of the literature search
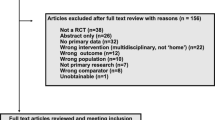
The systematic search resulted in the identification of 3982 references, 166 of which were selected following title and abstract screening. After the full-text review process, 21 references were included, corresponding to 20 studies. Seven further references were included from hand searching [27,28,29,30,31,32,33]. Again, two of these references came from the same study but reported different outcomes [30, 34]. Finally, 26 studies were included in the review (see Fig. 1).
Included studies
The characteristics of the included studies are detailed in Tables 2 and 3.
Setting
After data extraction, the included studies were classified into two main groups according to the setting where the intervention was performed. Studies classified under the acute care group included interventions delivered during hospitalization. In studies classified under the transitional care group, interventions were delivered during hospitalization and after hospital discharge.
Interventions delivered by setting
Acute setting
In 13 studies, hospital pharmacists delivered the interventions only while patients were in hospital. The most frequent interventions were medication reconciliation at admission (11 out of 13 studies) [30, 32,33,34,35,36,37,38,39,40,41], comprehensive medication review during hospitalization (10 out of 13 studies) [30, 32,33,34,35,36,37,38, 40,41,42], and counselling at hospital discharge, delivering a discharge summary to the patient [33, 40, 41, 43], to the patients’ general practitioner (GP) [35, 37, 44, 45] and to the GP and/or to the community pharmacist (CP) [32, 36, 38] (10 out of 13 studies) [30, 32,33,34,35,36,37,38, 40, 41, 43,44,45].
Pharmacists delivered their interventions individually, i.e. without being part of a team, in nine studies [30, 33,34,35, 40, 42,43,44,45], in which the hospital pharmacist made drug recommendations to the attending physician. In another three studies, the pharmacist was part of a multidisciplinary team [37, 38, 41]. In a single study, pharmacy technicians were also part of the multidisciplinary team together with hospital pharmacists [32]; in one, the hospital pharmacist worked along with a clinical pharmacologist [39] and in one, the hospital pharmacist worked in collaboration with the GP and the CP [36].
Transition from the acute care setting to the community
Thirteen studies assessed interventions conducted by the hospital pharmacist during transition of care from the hospital to the community [10, 27,28,29, 31, 46,47,48,49,50,51,52,53]. During hospitalization, pharmacists performed some interventions as drug reconciliation at admission [10, 28, 48, 52] or after admission [31, 46], and medication management, including medication review and giving advice on potential drug-related adverse events and drug–drug interactions [10, 27, 28, 31, 46, 48, 52]. Other interventions conducted at discharge included medication reconciliation [10, 28, 31, 49], a patient interview giving counsel on discharge medication and on how to prevent or manage drug problems [10, 28, 29, 31, 47, 49, 53], and sending a discharge summary to the GP or CP [48, 50,51,52,53].
After discharge, interventions consisted of: follow-up phone calls by the hospital pharmacist [10, 28, 29, 31, 48, 51, 52] or by other member of the team [46] in eight studies, and personal follow-up by pharmacist [47, 49, 53] or by a nurse [52] in four studies. During follow-up, pharmacists made drug-related recommendations, provided counselling, and reinforced adherence [31, 47, 48, 50, 53]. Contact with the GP in case any problems were detected or if changes to the medication were required was done by the pharmacist in six studies [10, 31, 47, 50, 51, 53] and by some other member of the team in an additional study [27]. In two studies, the pharmacist met with the patient’s responsible team if there were any problems related with the patients’ drug treatment [46, 50].
The drug treatment was followed by a hospital pharmacist in seven studies [10, 28, 29, 31, 48, 49, 52], a community pharmacist in two [47, 50] and by other members of the team in four studies [27, 46, 51, 52].
The hospital pharmacist was part of a multidisciplinary team in seven studies [28, 29, 31, 46, 47, 51, 52]. The composition of the team varied among the different studies: in some it comprised the hospital physician [31, 52], or the patient’s GP [29] or patient’s GP and patient’s community nurse [46, 51], a community pharmacist [47] or a study care coordinator (SCC) [28]; in other, the hospital pharmacist was considered an external expert who provided advice and formulated recommendations when asked to do so, or was called on to address a specific issue [27], in five studies [10, 48,49,50, 53] pharmacists worked on their own.
Outcomes
The included studies reported on a wide variety of health-related and economic outcomes. Detailed information for every considered outcome is showed in Tables 2 and 3 (only numerical information of the statistically significant outcomes is reported).
A. Outcomes resulting from interventions in the acute care setting.
I. Effects of clinical pharmacist interventions during the index hospitalization.
1. Length of hospital stay (LOS):
Ten out of 13 studies measured the length of the index hospitalization. Only one study found a LOS reduction in the intervention group compared to the control group [32]. Eight studies showed no differences in LOS between the study groups [30, 34, 36, 39,40,41,42, 44, 45]. In one study, LOS was longer in the intervention group than in the control group [38].
2. In-hospital mortality:
Five studies assessed in-hospital mortality finding no differences during the index hospitalization [30, 34, 35, 40, 42].
II. Residual effects of clinical pharmacist interventions after discharge (without any intervention by the clinical pharmacist after discharge)
1. Hospital readmission:
Ten out of 13 studies assessed hospital readmission rates during the follow-up period (after discharge). Three studies found a significant reduction in the number of hospital readmissions in the intervention group: two at one month [41, 43], one at 2 months [43] and one at 12 months follow-up [32]. Five studies did not find any difference in the number of readmissions: three at one month [36, 40, 42], three at 3 months [35, 39, 40], and one at 12 months’ follow-up [37]. Finally, two studies counted the number of patients with a medication-related readmission, after 30 days from discharge, no differences were found regarding the hospital readmission rate between groups [40], and after 1 year from discharge, the median time until a first readmission was no longer in the intervention group, but the risk for drug-related readmission was higher under standard care [33].
2. Visits to the emergency department (ED):
Six out of 13 studies calculated the number of ED visits after discharge. One study found a reduction in the number of ED visits in the intervention group [41] at one-month post-discharge, whereas two studies did not find any significant differences [39, 42]. Three studies did not observe a reduction in the number of ED visits in the intervention group at 3 months post-discharge [35, 39, 40]. Only one study considered the number of patients visiting the ED but who did not require further hospitalization and found a significant reduction [35]. One study did not find a reduction of ED visits in the intervention group at 12 months of post-discharge [37].
3. All cause hospital readmissions:
Only one study considered all cause hospital readmissions including both hospital readmissions and ED visits during the post-discharge period [38]. The authors observed a statistically significant reduction in number of readmissions at 3 months for the intervention group. However, there were no differences between groups at 6 months of post-discharge.
4. Visits to a healthcare provider:
Three studies assessed changes in the number of visits to a healthcare provider after hospital discharge. Only one study found a significant reduction in the number of visits to the GP and to outpatient clinics in the intervention group at one-month post-discharge [36]. The other two studies did not find any differences in the number of visits to the GP at one-month post-discharge [40], or at 3 months of post-discharge [39, 40].
5. Quality of life:
Four studies assessed post-discharge QoL. One study found a significant QoL improvement (measured with the EQ-5D questionnaire) [54] at three months post-discharge [35] but another study did not [39]. One study found a significantly better health-related QoL in the intervention group at 6 months’ follow-up measured by self-rated global health (answering the question, “In your opinion, how is your state of health?”), but not when measured by the EQ-5D [44, 45]. One study found a significant improvement in SF-36 score [55] in the intervention group as compared to the control group at one-month post-discharge, but only with regard to body pain and physical function [36].
6. Mortality:
Six out of 13 studies assessed mortality after discharge. No study found a significant reduction in mortality after the index intervention at any of the time points assessed: 1 month [36, 40], 3 months [35, 39, 40] and 12 months [32, 37].
B. Outcomes resulting from the interventions delivered during transition of care
1. Length of hospital stay:
Eight out of 13 studies assessed LOS [27,28,29, 46, 47, 50,51,52]. In four, the authors did not find statistically significant differences in LOS during the index hospitalization [28, 50,51,52]. Regarding the LOS of the readmissions after discharge, two studies found a statistically significant reduction in LOS at 30, 90 and 180 days [46] and at 12 months [52]. However, two studies did not find a reduction in LOS of readmissions after discharge at 3 months [29] and 6 months [29, 47] for the patients received pharmacist care.
In a third study, the number of days in hospital was higher for the group of patients assigned to the geriatric assessment team (including a geriatrician, a social worker, a nurse) than for those assigned to usual inpatient care during their hospital stay [27].
2. Hospital readmission:
Ten studies assessed all-cause hospital readmissions [10, 28, 29, 31, 46,47,48,49, 52, 53] and two studies assessed drug-related readmissions (DRR) [10, 48]. Interventions delivered in the community setting lasted from one day to 6 months after discharge and the follow-up times lasted up to 12 months after discharge. Three studies showed a statistically significant reduction in hospital readmission rates during the intervention period of 2–3 weeks [53], 1 month [10, 46], 3 months [10, 46] and 6 months [46] after discharge. Two studies did not find a reduction in hospital readmission rates during the intervention period of 2 months [50] and 3 months [29] after discharge. Four studies showed that the reduction in hospital readmissions persisted at one month [28, 31, 46, 52], at 3 months [53], and at 12 months [52] from discharge, spite of the end of the intervention in the community setting. By other hand, four studies did not find a persistent reduction on hospital readmissions at 2 months [28], 6 months [29, 47] and 12 months [48] after discharge.
Similarly, one study found a reduction in DRR at 12 months from the beginning of the intervention [48], while other study did not find DRR neither at one nor 6 months after discharge [10].
3. Visits to the emergency department:
Five studies measured the impact of pharmacist interventions on the number of visits to the ED. In two of them authors found a statistically significant reduction in the number of visits to the ED for the duration of intervention [10, 46], and at 6 months [10]. When the impact of the intervention was measured during the follow-up period the results were variable [28, 46, 48, 50, 52]. Only two studies found the effect of the intervention to persist in the longer term: one of them at 6 months [46] and the other at 12 months [48].
4. Visits to the GP or to a specialist outpatient clinic:
Of the four studies that looked into this outcome, [27, 46, 47, 53] only one showed a statistically significant reduction in unplanned visits to the GP for the intervention group [53].
5. Mortality:
There were no studies showing significant differences in the number of deaths during follow-up. This outcome was included in six studies [10, 27, 46,47,48, 51].
6. Quality of life:
QoL was measured in three studies [27, 47, 49]. One study used the British adaptation of the general well-being questionnaire designed to assess the impact of pharmaceutical treatment on QoL in older patients, but no differences were found between the groups at 3 and 6 months [47]. Two studies used the SF-36 questionnaire to measure health-related QoL [27, 49]. In one, there was no significant difference between patient groups in the SF-36 subscales at discharge, except for the vitality subscale [49]. In the other study, patients assigned to inpatient geriatric units showed significantly greater improvement in the scores for four of the eight SF-36 subscales at discharge. The scores on the SF-36′s mental health subscale also improved after 1 year [27].
C. Economic outcomes
Eight of the 26 studies reported economic outcomes. Healthcare costs were measured in different ways across the studies, including the cost of health services, hospitalization days or visits to outpatient clinics [27, 29, 32, 34, 45, 46, 48, 51]. In three studies, the cost of pharmacist interventions was also calculated to obtain the final balance in cost savings [45, 46, 48]. Only one study performed a cost-effectiveness analysis in a subgroup of patients where the EQ-5D utility scores had been calculated. The authors calculated a cost of €10,912 for the intervention group and of €9,290 for the control group. Intervention patients gained 0.0035 QALYs, which amounts to an incremental cost-effectiveness ratio per QALY of more than €460,000 in that group [45]. Five studies found a reduction in healthcare cost measured as cost-effectiveness of pharmacist intervention [34], cost savings per patient [32], inpatient readmission charges [29], total costs of intervention and hospital services utilization [46] and cost of hospital care [48]. In three studies, the authors did not find differences between study groups on hospital charges [51], costs of health care services [27], direct costs, reimbursed drugs and cost for the intervention [45].
Discussion
This scoping review intends to show the state of the art of hospital pharmacist interventions during and after hospitalization in different health outcomes in polymedicated older patients. There is enough evidence of the beneficial role that hospital pharmacists can play in reducing medication-related problems [37, 48], improving drug adherence [38, 53, 56] and the patients’ understanding of their medication as well as other aspects related to pharmacotherapy and drug safety. However, evidence is not so strong when it comes to other health outcomes or the use of healthcare resources. Intermediate results (improved drug regimens) are only relevant if they have an impact on more relevant health outcomes, such as mortality, QoL, or healthcare utilization.
Our findings were heterogeneous both in the characteristics of the intervention and on the impact on outcomes. Some studies explored the impact of simple interventions with few professionals involved [25, 45, 57, 58], while other planned complex interventions where the pharmacist was part of a geriatric interdisciplinary team [25, 28]. In other studies, pharmacists only acted on demand [56, 59]. Globally, interventions developed by a pharmacist within a multidisciplinary team seem to provide greater benefits in terms of clinical outcomes and economic results than those carried out by individual pharmacists. In these multidisciplinary teams, with the collaboration of the hospital pharmacist, significant reductions were achieved in visits to the ED, visits to the primary care physician, hospital readmission rates [28, 32, 38, 41, 53] and length of hospital stay [32, 46]. Making pharmacists part of the geriatric team seems to be the most productive way to impact on outcomes, although studies comparing teams with a and without a pharmacist in intermediate and final outcomes are lacking.
Given the heterogeneity of the findings, it is not easy to establish whether there is any single type of pharmacist intervention that is associated with a higher rate of success in terms of specific health outcomes. Medication reconciliation is the most frequent intervention at admission and at discharge; review of drugs is most common during admission; and advice and education is typical in the discharge phase. In addition, in transition of care studies, telephone reinforcement is usually carried out after discharge and the CP or GP are usually contacted to report changes in treatment. In our review, data did not allow to compare different interventions or the intensity of combined interventions. Other reviews that focussed on single component interventions, treatment review [60], medication counselling prior to discharge [61] or deprescription [62] did not find positive results. It has to be remembered that the success of pharmacist-led interventions depends on cooperation with prescribing physicians. In general, evidence shows that highly-complex multifaceted pharmacist-led interventions delivered from admission through to discharge obtain the best results in reducing hospital visits [28, 48, 53], LOS [44, 49] and DDR [48]. Very few studies have measured the degree of acceptance of such interventions; this may be an interesting aspect to be looked into in future analysis [63]. Further research is also required to provide an answer to whether multifaceted interventions are more effective than single-faceted interventions. This would contribute to a clearer definition of pharmacist interventions.
We found no evidence that any pharmacist intervention reduces mortality at any time point. These results were also found in other studies [8, 9, 25, 60]. This may be related to the high complexity of the patients studied, often with limited life expectancies, where the aim of care is usually to preserve or improve QoL or maintain function. In such patients, mortality may not be an outcome to use to test the effect of interventions, as agreed by others [64].
QoL is considered a relevant patient-reported outcome for many health care interventions. It may also be an indirect measure of unreported side effects of drug therapy, so it is worth exploring in interventions assessing drug use. We found some evidence that pharmacist interventions could improve QoL after hospital discharge. However, the number of studies is small and only two QoL instruments (EQ-5D and SF-36) were used. Specific instruments for drug-related QoL that include a range of medicine-related issues with potential impact on patients’ day-to-day lives [65] may need to be developed in order to better understand impact of pharmacy (and other) interventions on QoL.
Health care use is a relevant outcome both for patients and care systems. In practise, it is usually measured with hospital length of stay, readmissions, visits to the emergency department or visits to other health care providers. We found variable results of pharmacist interventions on such outcomes. The outcome with more positive studies were readmission rates, especially in studies where pharmaceutical care was continued after hospital discharge in cooperation with other professionals (GP, nurse, community pharmacist). This suggests that, to obtain satisfactory results, interventions must be maintained over time and should not be limited to the hospitalization period. Several previous reviews showed that the long-term effects of interventions are limited, and very few studies have found that pharmacist interventions are able to reduce the number of ED visits [23, 60, 66]. When considering the effect of interventions on hospital length of stay, only three studies out of 18 included in this review showed a significant shortening. These unsatisfactory results could be due to the fact that such outcome is not ideal to determine the effectiveness of pharmaceutical interventions. Using medication-related hospital readmissions may be more relevant [8, 60], but such readmissions are ill-defined and studies using this outcome are mostly negative. The field is probably ready for an international multicentre trial to define if a standardised pharmaceutical intervention continued after discharge does reduce hospital use.
Another interesting aspect is to determine if the results obtained by interventions are maintained over the time. In the different studies found the effect of the intervention lasts between 1 and 12 months. If the intervention is carried out continuously, it does seem reasonable to measure its effect in terms of health outcomes over time. However, for interventions carried out only in the hospital setting it seem logical to expect that their effects will disappear soon. In addition, it must be remembered that health and function of older patients with complex conditions may change rapidly during follow-up.
Finally, economic outcomes were evaluated in eight studies, five of them showing a reduction in healthcare costs. Cost analysis tends to be complex and, although the results are generally in favour of pharmacist interventions, the relevance of such cost reductions is unclear. The reasons for this are twofold. First, the evaluated outcomes in different studies were heterogeneous and cannot be pooled. Second, none of the included studies had an economic variable as their main outcome, which means that they were not specifically designed to evaluate such outcomes. Post-discharge readmissions of older adults due to drug effects is estimated to cost the UK National Health Service £396 million annually, of which £243 million are potentially preventable [67]. Some authors suggest that, although pharmacist interventions can be cost-effective, the matter requires further evaluation as an inappropriate estimation of input costs usually leads to an overestimation of cost savings, rendering it impossible to make an informed decision regarding the true value of pharmacist interventions in this regard [6, 9, 68, 69].
Our scoping review has some strengths: it was conducted following a systematic search process, which can be replicated; used several key databases supplemented by hand search of the literature; only included RCTs and controlled prospective studies; used pairs along all the review process; and piloted data extraction. It has also some limitations. The risk of bias of the included studies was not assessed, as a critical appraisal of the risk of bias is not considered mandatory in scoping reviews [26, 70]. Also, it includes a wide range of interventions, which are hard to aggregate.
It can be concluded that there is no hard evidence demonstrating the effectiveness of hospital pharmacist interventions in older polymedicated patients. Some ways forward to improve research in this area seem to arise from the review. First, mortality does not show as a relevant outcome of pharmacist interventions in older complex patients. Other health care outcomes, such as hospital readmissions, seem to be more relevant and amenable to change. Frailty, functional and mental outcomes, relevant in most areas of geriatric research, merit exploration as outcome measures for intervention studies on drugs. Moreover, patient-reported outcome, including QoL, need to be considered using well-validated methods. Interventions that include pharmacists in multidisciplinary geriatric teams seem to be more promising that isolated pharmacist interventions. Also, interventions prolonged after hospital discharge seem to be more appropriate that interventions delivered only during hospital admission. Standardization of interventions in future research would allow for comparison between studies performed in different countries and settings. Better-designed studies, with clearly-defined interventions, outcomes and follow-up times should be conducted in the future to provide further insight into the effect of pharmacist interventions.
References
Hepler CD, Strand LM (1990) Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm 47(3):533–543
Bergkvist A, Midlov P, Hoglund P, Larsson L, Bondesson A, Eriksson T (2009) Improved quality in the hospital discharge summary reduces medication errors–LIMM: Landskrona integrated medicines management. Eur J Clin Pharmacol 65(10):1037–1046
Bergkvist A, Midlöv P, Höglund P, Larsson L, Eriksson T (2009) A multi-intervention approach on drug therapy can lead to a more appropriate drug use in the elderly. LIMM-Landskrona Integrated Medicines Management. J Eval Clin Pract 15(4):660–667
Tecklenborg S, Byrne C, Cahir C, Brown L, Bennett K (2020) Interventions to reduce adverse drug event-related outcomes in older adults: a systematic review and meta-analysis. Drugs Aging 37(2):91–98
Van der Meer HG, Wouters H, Pont LG, Taxis K (2018) Reducing the anticholinergic and sedative load in older patients on polypharmacy by pharmacist-led medication review: a randomised controlled trial. BMJ Open 8(7):e019042
Mi X, Su X, Jin Z, Zeng L, Li Z, Wang X et al (2020) Economic evaluations of clinical pharmacy services in China: a systematic review. BMJ Open 10(1):e034862
De Rijdt T, Willems L, Simoens S (2008) Economic effects of clinical pharmacy interventions: a literature review. Am J Health Syst Pharm 65(12):1161–1172
Kiesel E, Hopf Y (2018) Hospital pharmacists working with geriatric patients in Europe: a systematic literature review. Eur J Hosp Pharm 25(e1):e74–e81
Skjot-Arkil H, Lundby C, Kjeldsen LJ, Skovgards DM, Almarsdottir AB, Kjolhede T et al (2018) Multifaceted pharmacist-led interventions in the hospital setting: a systematic review. Basic Clin Pharmacol Toxicol 123(4):363–379
Ravn-Nielsen LV, Duckert M-L, Lund ML, Henriksen JP, Nielsen ML, Eriksen CS et al (2018) Effect of an in-hospital multifaceted clinical pharmacist intervention on the risk of readmission: a randomized clinical trial. JAMA Intern Med 178(3):375–382
Reguant F, Arnau A, Lorente JV, Maestro L, Bosch J (2019) Efficacy of a multidisciplinary approach on postoperative morbidity and mortality of elderly patients with hip fracture. J Clin Anesth 53:11–19
Graabaek T, Kjeldsen LJ (2013) Medication reviews by clinical pharmacists at hospitals lead to improved patient outcomes: a systematic review. Basic Clin Pharmacol Toxicol 112(6):359–373
de Barra M, Scott CL, Scott NW, Johnston M, de Bruin M, Nkansah N et al (2018) Pharmacist services for non-hospitalised patients. Cochrane Database Syst Rev 9:013102
Sadowski C, Fedorak V, Simpson SH, Charrois T, Storie D, Chambers T (2010) Contributions of home-based medication reviews in the elderly: a systematic review. J Am Geriatr Soc 58:S52–S53
Wagle KC, Skopelja EN, Campbell NL (2018) Caregiver-based interventions to optimize medication safety in vulnerable elderly adults: a systematic evidence-based review. J Am Geriatr Soc 66(11):2128–2135
Abbott RA, Moore DA, Rogers M, Bethel A, Stein K, Coon JT (2020) Effectiveness of pharmacist home visits for individuals at risk of medication-related problems: a systematic review and meta-analysis of randomised controlled trials. BMC Health Serv Res 20(1):39
Von Buedingen F, Hammer MS, Meid AD, Müller WE, Gerlach FM, Muth C (2018) Changes in prescribed medicines in older patients with multimorbidity and polypharmacy in general practice. BMC Fam Pract 19(1):131
Mangoni AA, Jackson SHD (2004) Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol 57(1):6–14
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P (2015) STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 44(2):213–218
By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel (2019) American Geriatrics Society 2019 updated AGS beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc 67(4):674–694
Calvo-Salazar RA, David M, Zapata-Mesa MI, Rodríguez-Naranjo CM, Valencia-Acosta NY (2018) Problemas relacionados con medicamentos que causan ingresos por urgencias en un hospital de alta complejidad. Farm Hosp 42(6):228–233
Tasaka Y, Tanaka A, Yasunaga D, Asakawa T, Araki H, Tanaka M (2018) Potential drug-related problems detected by routine pharmaceutical interventions: safety and economic contributions made by hospital pharmacists in Japan. J Pharm Health Care Sci 4:33
Van der Linden L, Hias J, Walgraeve K, Flamaing J, Tournoy J, Spriet I (2020) Clinical pharmacy services in older inpatients: an evidence-based review. Drugs Aging 37(3):161–174
Kalim R, Mcmahon N, Ryder S (2019) 113 Pharmacist interventions at discharge and the quality of older patients’ care: a systematic review. Age Ageing 48(S3):iii17–iii65
Acosta-Garcia H, Alfaro-Lara ER, Sanchez-Fidalgo S, Sevilla-Sanchez D, Delgado-Silveira E, Juanes-Borrego A et al (2020) Intervention effectiveness by pharmacists integrated within an interdisciplinary health team on chronic complex patients. Eur J Public Health 30(5):886–899
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D et al (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169(7):467–473
Cohen HJ, Feussner JR, Weinberger M, Carnes M, Hamdy RC, Hsieh F et al (2002) A controlled trial of inpatient and outpatient geriatric evaluation and management. N Engl J Med 346(12):905–912
Koehler BE, Richter KM, Youngblood L, Cohen BA, Prengler ID, Cheng D et al (2009) Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med 4(4):211–218
Lipton HL, Bird JA (1994) The impact of clinical pharmacists’ consultations on geriatric patients’ compliance and medical care use: a randomized controlled trial. Gerontologist 34(3):307–315
O’Sullivan D, O’Mahony D, O’Connor MN, Gallagher P, Gallagher J, Cullinan S et al (2016) Prevention of adverse drug reactions in hospitalised older patients using a software-supported structured pharmacist intervention: a cluster randomised controlled trial. Drugs Aging 33(1):63–73
Rottman-Sagebiel R, Cupples N, Wang CP, Cope S, Pastewait S, Braden H et al (2018) A pharmacist-led transitional care program to reduce hospital readmissions in older adults. Fed Pract 35(12):42–50
Scullin C, Scott MG, Hogg A, McElnay JC (2007) An innovative approach to integrated medicines management. J Eval Clin Pract 13(5):781–788
Lenssen R, Schmitz K, Griesel C, Heidenreich A, Schulz JB, Trautwein C et al (2018) Comprehensive pharmaceutical care to prevent drug-related readmissions of dependent-living elderly patients: a randomized controlled trial. BMC Geriatr 18(1):135
Gallagher J, O’Sullivan D, McCarthy S, Gillespie P, Woods N, O’Mahony D et al (2016) Structured pharmacist review of medication in older hospitalised patients: a cost-effectiveness analysis. Drugs Aging 33(4):285–294
Van der Linden L, Decoutere L, Walgraeve K, Milisen K, Flamaing J, Spriet I et al (2017) Combined use of the rationalization of home medication by an adjusted STOPP in older patients (RASP) list and a pharmacist-led medication review in very old inpatients: impact on quality of prescribing and clinical outcome. Drugs Aging 34(2):123–133
Stowasser DA, Collins DM, Stowasser M (2002) A randomised controlled trial of medication liaison services: patient outcomes. J Pharm Pract Res 32(2):133–140
Spinewine A, Swine C, Dhillon S, Lambert P, Nachega JB, Wilmotte L et al (2007) Effect of a collaborative approach on the quality of prescribing for geriatric inpatients: a randomized, controlled trial. J Am Geriatr Soc 55(5):658–665
Makowsky MJ, Koshman SL, Midodzi WK, Tsuyuki RT (2009) Capturing outcomes of clinical activities performed by a rounding pharmacist practicing in a team environment: the COLLABORATE study [NCT00351676]. Med Care 47(6):642–650
Lisby M, Thomsen A, Nielsen LP, Lyhne NM, Breum-Leer C, Fredberg U et al (2010) The effect of systematic medication review in elderly patients admitted to an acute ward of internal medicine. Basic Clin Pharmacol Toxicol 106(5):422–427
Graabaek T, Hedegaard U, Christensen MB, Clemmensen MH, Knudsen T, Aagaard L (2019) Effect of a medicines management model on medication-related readmissions in older patients admitted to a medical acute admission unit-A randomized controlled trial. J Eval Clin Pract 25(1):88–96
Dedhia P, Kravet S, Bulger J, Hinson T, Sridharan A, Kolodner K et al (2009) A quality improvement intervention to facilitate the transition of older adults from three hospitals back to their homes. J Am Geriatr Soc 57(9):1540–1546
Cossette B, Ethier J, Joly-Mischlich T, Bergeron J, Ricard G, Brazeau S et al (2017) Reduction in potentially inappropriate medication use in elderly inpatients: a pragmatic randomized controlled trial. J Am Geriatr Soc 65:S109–S110
Sanchez Ulayar A, Gallardo Lopez S, Pons Llobet N, Murgadella Sancho A, Campins Bernadas L, Merino MR (2012) Pharmaceutical intervention upon hospital discharge to strengthen understanding and adherence to pharmacological treatment. Farm Hosp 36(3):118–123
Bladh L, Ottosson E, Karlsson J, Klintberg L, Wallerstedt SM (2011) Effects of a clinical pharmacist service on health-related quality of life and prescribing of drugs: a randomised controlled trial. BMJ Qual Saf 20(9):738–746
Wallerstedt SM, Bladh L, Ramsberg J (2012) A cost-effectiveness analysis of an in-hospital clinical pharmacist service. BMJ Open 2(1):e000329
Low LL, Tan SY, Ng MJM, Tay WY, Ng LB, Balasubramaniam K et al (2017) Applying the integrated practice unit concept to a modified virtual ward model of care for patients at highest risk of readmission: a randomized controlled trial. PLoS ONE 12(1):e0168757
Nazareth I, Burton A, Shulman S, Smith P, Haines A, Timberall H (2001) A pharmacy discharge plan for hospitalized elderly patients: a randomized controlled trial. Age Ageing 30(1):33–40
Gillespie U, Alassaad A, Henrohn D, Garmo H, Hammarlund-Udenaes M, Toss H et al (2009) A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med 169(9):894–900
Basger BJ, Moles RJ, Chen TF (2015) Impact of an enhanced pharmacy discharge service on prescribing appropriateness criteria: a randomised controlled trial. Int J Clin Pharm 37(6):1194–1205
Crotty M, Rowett D, Spurling L, Giles LC, Phillips PA (2004) Does the addition of a pharmacist transition coordinator improve evidence-based medication management and health outcomes in older adults moving from the hospital to a long-term care facility? results of a randomized, controlled trial. Am J Geriatr Pharmacother 2(4):257–264
Fretwell MD, Raymond PM, McGarvey ST, Owens N, Traines M, Silliman RA et al (1990) The senior care study: a controlled trial of a consultative/unit-based geriatric assessment program in acute care. J Am Geriatr Soc 38(10):1073–1081
Torisson G, Minthon L, Stavenow L, Londos E (2013) Multidisciplinary intervention reducing readmissions in medical inpatients: a prospective, non-randomized study. Clin Interv Aging 8:1295–1304
Al-Rashed SA, Wright DJ, Roebuck N, Sunter W, Chrystyn H (2002) The value of inpatient pharmaceutical counselling to elderly patients prior to discharge. Br J Clin Pharmacol 54(6):657–664
EuroQol Group (1990) EuroQol - a new facility for the measurement of health-related quality of life. Health Policy 16(3):199–208
Ware JE jr, Snow KK, Kosinski M, Gandek B (1997) New England Medical Center, The Health Institute. SF-36 Health Survey: Manual and interpretation guide. Boston, Mass.: The Health Institute, New England Medical Center
Leguelinel-Blache G, Castelli C, Roux-Marson C, Bouvet S, Andrieu S, Cestac P et al (2018) Impact of collaborative pharmaceutical care on in-patients’ medication safety: study protocol for a stepped wedge cluster randomized trial (MEDREV study). Trials 19(1):19
Campins L, Serra-Prat M, Gózalo I, López D, Palomera E, Agustí C et al (2017) Randomized controlled trial of an intervention to improve drug appropriateness in communitydwelling polymedicated elderly people. Fam Pract 34(1):36–42
Juanes A, Garin N, Mangues MA, Herrera S, Puig M, Faus MJ et al (2018) Impact of a pharmaceutical care programme for patients with chronic disease initiated at the emergency department on drug-related negative outcomes: a randomised controlled trial. Eur J Hosp Pharm 25(5):274–280
Sanon M, Hwang U, Abraham G, Goldhirsch S, Richardson LD, GEDI WISE Investigators (2019) ACE model for older adults in ED. Geriatrics (Basel) 4(1):24
Christensen M, Lundh A (2016) Medication review in hospitalised patients to reduce morbidity and mortality. Cochrane Database Syst Rev 2:CD008986
Capiau A, Foubert K, Van der Linden L, Walgraeve K, Hias J, Spinewine A et al (2020) Medication counselling in older patients prior to hospital discharge: a systematic review. Drugs Aging 37(9):635–655
Thillainadesan J, Gnjidic D, Green S, Hilmer SN (2018) Impact of deprescribing interventions in older hospitalised patients on prescribing and clinical outcomes: a systematic review of randomised trials. Drugs Aging 35(4):303–319
Romero-Ventosa EY, Samartín-Ucha M, Martín-Vila A, Martínez-Sánchez ML, Rey Gómez-Serranillos I, Pineiro-Corrales G (2016) Multidisciplinary teams involved: detection of drug-related problems through continuity of care. Farm Hosp 40(6):529–543
Akpan A, Roberts C, Bandeen-Roche K, Batty B, Bausewein C, Bell D et al (2018) Standard set of health outcome measures for older persons. BMC Geriatr 18(1):36
Katusiime B, Corlett S, Reeve J, Krska J (2016) Measuring medicine-related experiences from the patient perspective: a systematic review. Patient Relat Outcome Meas 7:157–171
Gutiérrez Valencia M, Martínez Velilla N, Lacalle Fabo E, Beobide Telleria I, Larrayoz Sola B, Tosato M (2016) Intervenciones para optimizar el tratamiento farmacológico en ancianos hospitalizados: una revisión sistemática. Rev Clínica Esp 216(4):205–221
Parekh N, Ali K, Stevenson JM, Davies JG, Schiff R, Van der Cammen T et al (2018) Incidence and cost of medication harm in older adults following hospital discharge: a multicentre prospective study in the UK: incidence and cost of medication harm in older adults. Br J Clin Pharmacol 84(8):1789–1797
Kwak A, Moon YJ, Song Y-K, Yun H-Y, Kim K (2019) Economic impact of pharmacist-participated medication management for elderly patients in nursing homes: a systematic review. Int J Environ Res Public Health 16(16):2955
Dawoud DM, Smyth M, Ashe J, Strong T, Wonderling D, Hill J et al (2019) Effectiveness and cost effectiveness of pharmacist input at the ward level: a systematic review and meta-analysis. Res Social Adm Pharm 15(10):1212–1222
Sucharew H (2019) Methods for research evidence synthesis: the scoping review approach. J Hosp Med 14(7):416
Acknowledgements
The authors would like to thank Noelia Álvarez-Díaz for her contribution to this review as a librarian, for designing the literature search strategy and for conducting the literature search itself.
Author information
Authors and Affiliations
Contributions
All authors: eligibility criteria, review the final manuscript. AC-P, ED-S, MV-D-P, MM-G: study selection, peer review of articles, data extraction from studies. MV-D-P: manual search of articles, writing of the introduction, summary, writing and design of figure 1. MM-G: writing the discussion and tables 2 and 3. AC-P: writing of results, writing and design of tables 2 and 3. ED-S: Writing methodology, results, discussion, summary, tables 1, 2 and 3 and design of figure 1. Responsible for submitting the article.
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no competing interest.
Ethics approval
The ethical approval and the informed consent is not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Delgado-Silveira, E., Vélez-Díaz-Pallarés, M., Muñoz-García, M. et al. Effects of hospital pharmacist interventions on health outcomes in older polymedicated inpatients: a scoping review. Eur Geriatr Med 12, 509–544 (2021). https://doi.org/10.1007/s41999-021-00487-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00487-3