Abstract
Background
Polypharmacy and potentially inappropriate medications (PIMs) are prevalent in older adults in hospital, and are associated with negative outcomes including adverse drug reactions, falls, confusion, hospitalisation and death. Deprescribing may reduce inappropriate polypharmacy and use of inappropriate medications.
Objective
The aim of this systematic review was to investigate the efficacy of deprescribing interventions in older inpatients to reduce PIMs and impact on clinical outcomes.
Methods
Ovid MEDLINE, Embase, Informit, International Pharmaceutical Abstracts, Scopus, PsycINFO, the Cochrane Central Register of Controlled Trials (CENTRAL) and CINAHL were searched for randomised controlled trials (RCTs) from 1996 to April 2017. RCTs reporting on deprescribing interventions to reduce PIMs in older hospitalised adults were eligible. Data were extracted, and study quality assessed. The primary outcome was reduction in PIMs. Where available, clinically relevant outcomes were assessed.
Results
Nine RCTs (n = 2522 subjects) met the inclusion criteria. Deprescribing interventions were either pharmacist-led (n = 4), physician-led (n = 4) or multidisciplinary team-led (n = 1). Seven of the nine studies reported a statistically significant reduction in PIMs in the intervention group. There was no change in one study where there were zero PIMs on admission and discharge, and in the other study a reduction in PIMs that was not statistically significant was observed. There was significant heterogeneity in outcome measures and reporting. Few studies reported on the impact of deprescribing interventions on clinical outcomes. Reported clinical outcomes included drug-related problems (n = 3), quality of life (n = 2), mortality (n = 3), hospital readmissions (n = 4), falls (n = 3) and functional status (n = 2). Most studies reported a benefit in the intervention group that was not statistically significant. No notable harm was observed in the intervention group. There was a high risk of bias in the included studies.
Conclusions
The evidence available suggests that deprescribing interventions in hospital are feasible, generally effective at reducing PIMs and safe. However, the current evidence is limited, of low quality and the impact on clinical outcomes is unclear.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The use of potentially inappropriate medications and the associated harm is a growing issue among older adults. |
Deprescribing interventions in older adults can be successfully implemented in the hospital setting. |
The quality of evidence on deprescribing interventions is low, and impact on clinical outcomes is uncertain, but implementing deprescribing interventions in hospitals appears beneficial in terms of reducing inappropriate prescribing. |
1 Introduction
Hospital admissions for older Australians are increasing rapidly as the population ages. People aged 65 years and over, who constitute 15% of Australia’s population, accounted for 41% of hospitalisations and 49% of patient days in 2014–2015 [1]. Clinicians are looking after an older population with increased prevalence of multimorbidity and polypharmacy [2,3,4,5]. Polypharmacy (the use of five or more medications) is associated with a high prevalence of potentially inappropriate medications (PIMs), defined as medications for which risk of an adverse drug event is likely to outweigh clinical benefits, and measured using a range of expert consensus or pharmacological tools [6, 7]. A recent Australian study on the prevalence of PIMs in older hospitalised patients found 54.8% were on one or more PIM at admission, and 26.8% were on multiple PIMs [8]. The use of multiple medications is associated with an increased risk of adverse drug events, falls, confusion, functional decline, hospitalisation, increased healthcare costs and death [9,10,11,12].
The term deprescribing first appeared in the literature in 2003 [13], and has been defined as “the process of withdrawal of an inappropriate medication, supervised by a health care professional with the goal of managing polypharmacy and improving outcomes” [14]. Deprescribing interventions include pharmacist-led medication reviews, physician-led interventions, prescriber education programmes, multidisciplinary interventions and clinical decision support systems [15, 16]. There is a growing evidence base for deprescribing. Studies have included those evaluating the impact of a deprescribing intervention on both specific drug classes and general polypharmacy across different patient settings.
The first systematic review on the topic by Iyer et al. examined 31 withdrawal trials of specific drug classes in people aged 65 years and older [17]. They concluded that some medications could be safely withdrawn with benefits, including reduction in falls, and improved cognition after withdrawal of psychotropic medications [17]. However, limitations to their study methodology included single-author screening and no formal assessment of the quality of the studies. There have been Cochrane reviews of withdrawing specific drug classes including psychotropic agents and proton pump inhibitors [18, 19]. Two recent systematic reviews of both non-randomised and randomised deprescribing trials across heterogeneous settings found deprescribing reduced medication use, and there was no significant effect on all-cause mortality or hospitalisations [16, 20]. Overall, most deprescribing trials and systematic reviews conclude these interventions are safe and feasible. The impact on patient-relevant outcomes such as mortality, hospitalisations, falls and cognition has not been consistently demonstrated. Limitations of these studies include short follow-up periods, low to moderate quality methodology and significant heterogeneity in the clinical settings and interventions.
Hospitalisation presents a valuable opportunity to review and address polypharmacy in the context of the individual’s morbidities and goals of care. A recent Australian study found that 89% of older inpatients were willing to stop one or more of their regular medications, and 95% were willing to stop statins if their doctor said they could [21]. The multidisciplinary team in hospital can facilitate the assessment of the patient’s function and disabilities, including possible effects of medication use. The hospital encounter provides an opportunity for the consulting physician to take the lead in medication management and communicate changes to the general practitioner to ensure sustainable changes [22]. There is also an opportunity to perform multidisciplinary pharmaceutical review with hospital pharmacists working closely with doctors and other healthcare professionals. To date, systematic reviews investigating the impact of deprescribing interventions have mostly included trials with elderly patients in primary care or residential aged-care facilities [16, 20]. A recent Cochrane review of ten randomised controlled trials (RCTs) investigating the impact of in-hospital medication review on mortality and morbidity was not focussed on deprescribing interventions [23]. The review included studies focused on identification of hospital medication errors and medication adherence. Most studies did not look at reduction of PIMs or polypharmacy as an outcome [23]. However, there are also challenges in the hospital setting. Admissions may be too short to implement and monitor for any harmful effects of deprescribing, and long-term follow up may not always be possible. The aim of this systematic review was to investigate the effectiveness of deprescribing interventions in older hospitalised patients on prescribing and clinical outcomes.
2 Methods
2.1 Protocol and Registration
This systematic review was registered on PROSPERO (CRD42017060236) and can be accessed at http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017060236, and was conducted in adherence with PRISMA [24].
2.2 Eligibility Criteria
2.2.1 Types of Studies
Only RCTs, in English, from 1 January 1996 up to and including the commencement of the search in April 2017 were included.
2.2.2 Types of Participants
Interventions that targeted an older population with a median age of 65 years and over, and were implemented in the hospital setting, were included. Studies that included a younger population were included if the majority of subjects were aged 65 years and over.
2.2.3 Types of Interventions
Studies that implemented any intervention aimed at reduction of PIMs including electronic and non-electronic deprescribing interventions, pharmacist-led medication reviews, physician-led interventions, prescriber education programmes, multidisciplinary interventions and clinical decision support systems were included. The comparison intervention was usual care.
2.2.4 Types of Outcome Measures
The primary outcome was reduction in PIMs. Measures included the number of PIMs, change in PIMs or other measures of PIMs reported at both baseline and follow-up; for example, reduction in PIMs as measured by methods including the Drug Burden Index (DBI) [25], Medication Appropriateness Index (MAI) [26], Screening Tool of Older Persons’ Potentially Inappropriate Prescriptions (STOPP) criteria [27] and updated Beers list [6].
Secondary outcome measures of clinical relevance were also assessed including mortality, falls, cognitive function, adverse drug withdrawal events, quality of life and hospitalisations.
2.3 Information Sources and Search Strategy
Studies were identified by searching electronic databases Ovid MEDLINE, Embase, Informit, International Pharmaceutical Abstracts, Scopus, PsycINFO, the Cochrane Central Register of Controlled Trials (CENTRAL) and CINAHL. Databases were searched from 1996 to April 2017. The reference lists of all included studies and relevant reviews were manually searched for additional studies. Key search terms are shown in Table 1. The MEDLINE search strategy is detailed in Appendix S1 in the Electronic Supplementary Material (ESM).
2.4 Study Selection
The studies retrieved were screened for potential inclusion independently by two authors (JT, SG). When the eligibility was unclear, it was discussed with the senior investigator (SH).
2.5 Data Extraction and Synthesis
The primary investigator (JT) extracted the data using a pre-agreed data extraction form. Extracted information included author, country, publication year, study type, setting, population characteristics, type of intervention and control, follow-up details, recruitment and study completion rates, impact of intervention on PIMs and other clinically relevant outcomes. The data were summarised in tables. In the event of missing or unclear data, the original authors were contacted. Three study authors were contacted for further information. One author responded and provided the requested data. Due to the high heterogeneity in the type of deprescribing intervention, measure of PIMs and reported outcome data, a meta-analysis could not be undertaken.
2.6 Risk of Bias Assessment
The Cochrane Risk of Bias Assessment Tool was used to assess the quality of all included RCTs and was performed by the primary investigator, JT, and reviewed by co-author DG [28].
3 Results
3.1 Study Selection
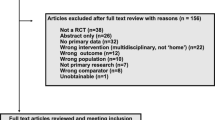
A total of 2915 records were retrieved from the electronic databases. After removal of duplicates, 2106 abstracts and titles were screened for eligibility. Full-text articles were sought and screened for 67 articles that appeared to meet the inclusion criteria. Further studies were not found after manual search of systematic reviews and references of included studies. Nine RCTs were included in the systematic review [29,30,31,32,33,34,35,36,37]. The study selection process and reasons for exclusion are summarised in Fig. 1.
3.2 Characteristics of Included Studies
3.2.1 Participants and Setting
The details of the included trials are summarised in Table 2. There was a total of 2522 participants across the nine included studies (range 114–409 participants per study). The main inclusion criterion in all studies was hospitalised patients who were elderly (criteria ranged from aged ≥ 60 to ≥ 80 years), except one study that included all ages. In this one study, 17 of the 164 intervention subjects, and 24 of the 181 control subjects, were aged < 65 years, and the overall median age was 82 years, ranging from 35 to 99 years [29]. Mean or median age was reported in eight of the nine studies, and ranged from 74.5 to 86.7 years [29,30,31,32,33, 35,36,37]. Frailty or risk of frailty was an inclusion criterion in two studies [30, 34]. One study excluded patients with dementia [33] while one study excluded patients with severe dementia [34]. There were 250 participants with dementia or cognitive impairment at baseline among 1491 participants in the five studies that reported on this characteristic [30,31,32, 35, 37]. Participants in all studies were inpatients, with five studies undertaken on the medical or surgical wards [29,30,31,32, 34] and four studies on the geriatric ward [33, 35,36,37].
3.2.2 Intervention Type
Four studies were pharmacist-led [29, 32, 35, 36], four were physician-led [30, 31, 33, 37] and one was a multidisciplinary team-led deprescribing intervention [34]. Among the four pharmacist-led studies, two studies specified the use of a specific tool to identify PIMs as part of the comprehensive medication review [29, 36]. In the other two pharmacist-led intervention studies and the multidisciplinary team-led deprescribing study, a comprehensive medication review was undertaken but no specific PIMs screening tools were utilised as part of the deprescribing intervention [32, 34, 35]. Among the four physician-led interventions studies, the STOPP criteria were applied in two studies [30, 31] and the ‘Fit fOR The Aged’ (FORTA) list was applied in two studies [33, 37]. A computer support system was employed in one study to perform the medication review [29]. Standard care was either usual care by the medical or surgical team [29, 31, 32, 34] or usual geriatric care [30, 33, 35,36,37].
3.2.3 Primary Outcome
In all studies, impact of the deprescribing intervention on PIMs was measured in the intervention and control groups. In eight of the nine studies, impact on PIMs was the primary outcome [29,30,31,32,33, 35,36,37] and in one study the primary outcome was adverse drug reactions (ADRs) [34]. The average duration of hospital stay ranged from 6 to 20 days for both the control and intervention groups across the five studies that provided this data. Some studies measured the reduction in PIMs beyond discharge, including at 3 months [35], 2, 4 and 6 months post-discharge [31] and 1 year post-discharge [30, 34]. Impact on PIMs was assessed using a variety of criteria including STOPP criteria [30,31,32], MAI [31, 32, 34, 35], three drug-specific quality indicators established by the Swedish National Board of Health and Welfare [29], Beer’s criteria [35], FORTA [33, 37] and the Rationalization of home medication by an Adjusted STOPP in older Patients (RASP) list [36]. The six studies that used explicit criteria to identify PIMs used the same criteria to measure impact on PIMs [29,30,31, 33, 36, 37].
3.2.4 Other Reported Outcomes
All nine studies reported the impact of the deprescribing intervention on at least one clinical outcome, summarised in Table 2. Reported clinical outcomes included drug-related problems (n = 3) [29, 34, 37], quality of life (n = 2) [29, 36], mortality (n = 3) [31, 35, 36], hospital readmissions (n = 4) [31, 32, 35, 36], falls (n = 3) [31, 33, 36, 37] and functional status (n = 2) [33, 37].
3.3 Risk of Bias Within Studies
The nine included RCTs were assessed using the Cochrane Risk of Bias Assessment Tool, summarised in Table 3. The Cochrane Risk of Bias tool was applied at the study level, and included a measure of outcome bias (detection bias related to blinding), as shown in Table 3. Two studies reported adequate sequence generation [31, 34] and three reported concealment of allocation [29, 31, 32]. The bias associated with blinding of participants and personnel was rated high in most studies, reflecting the nature of the intervention. Five studies were judged to be at low risk of attrition bias as they reported similar rates of drop outs in the control and intervention groups for similar reasons [31,32,33, 35, 36]. Six of the nine studies were registered in a trial registry [29, 31,32,33, 36, 37]. One study was a post-hoc analysis and was thus rated as high risk of reporting bias [32].
3.4 Outcomes of Included Studies
3.4.1 Primary Outcome Results—Reduction in PIMs
Where the mean (standard deviation [SD]) or median (interquartile range [IQR]) number of PIMs per patient in the intervention and control groups at admission and discharge were not reported, the first author of the study was contacted via email. We contacted three study authors and a response was received from one [37]. Mean (SD) number of PIMs per patient at admission and discharge in the intervention and control groups was available for five studies, and ranged from 0.29 (0.56) to 1.4 (1.5) in the intervention group and 0.35 (0.73) to 1.5 (1.5) in the control group at admission, and ranged from 0.03 (0.17) to 0.9 (1.0) in the intervention group and from 0.04 (0.21) to 1.7 (1.5) in the control group at discharge [29, 32, 34, 35, 37]. Median (IQR) number of PIMs per patient in the intervention and control groups at admission and discharge was reported in three studies, and ranged from 0 (0–1) to 3 (2–5) at admission in both the intervention and control groups, and ranged from 0 (0–0) to 1 (0–5) in the intervention group, and from 0 (0–2) to 2 (1–3) in the control group at discharge [32, 33, 36].
The impact of interventions on PIMs use across all included studies is summarised in Table 2, and where mean number of PIMs per patient was reported (n = 5), these results are shown in Fig. 2. In the three studies that compared the change in PIMs from admission to discharge between intervention and control group, a statistically significant reduction in PIMs was found [32, 34, 37]. These studies included a pharmacist-led medication review with no specific tool [32], a pharmacist review as part of a Geriatric Evaluation and Management (GEM) service with no specific tool [34], and a physician-led intervention using FORTA [37]. In the other six studies that analysed the intergroup difference in PIMs at discharge, a significant reduction in the intervention group was reported in three of the six studies [30, 31, 36]. In the three studies that reported no statistically significant intergroup difference in number of PIMs, there was a significant reduction in the number of PIMs from admission to discharge within the intervention group in one study [35], a non-significant reduction in PIMs observed in the study by Bladh et al. [29], and no change in the study by Michalek et al. where the mean number of PIMs was zero at admission and discharge in both the control and intervention groups [33].
Four studies used MAI to provide a summated score [31, 32, 34, 35], summarised in Appendix S2 in the ESM. Two of the four studies that performed a between-group analysis of the change in the mean summated MAI score per patient reported a statistically significant improvement in the intervention group compared with usual care [32, 34]. Four studies reported on reduction in PIMs beyond discharge with mixed results [30, 31, 34, 35]. Gallagher et al. reported that in the intervention group, the proportion of patients with at least one PIM remained statistically significantly lower at 2, 4 and 6 months post-discharge [31]. Dalleur et al. observed a lower proportion of PIMs had been restarted in the intervention group at 12 months, though the difference was not statistically significant [30]. Schmader et al. reported a slight increase in the number of PIMs in the intervention group compared with the control group at 12 months [34]. Spinewine et al. found a trend toward higher maintenance rates in the intervention group that was not statistically significant [35].
3.4.2 Secondary Outcomes Results
Secondary outcome results are summarised in tables in Appendix S3 in the ESM.
Medication-related problems Drug-related problems including ADRs were assessed in three studies [29, 34, 37], but in one study this outcome was only measured in the intervention group [29]. In the study by Schmader et al. the deprescribing intervention did not result in a significant difference in ADRs between the groups [34]. Wehling et al. reported a significant reduction in the incidence of ADRs in the intervention group compared with the control group post-intervention [37].
Health-related quality of life Health-related quality of life was assessed in two studies [29, 36]. Bladh et al. found no intergroup difference at 6 months in the self-rated global health and the EuroQol 5-dimension questionnaire (EQ-5D) [29]. Van der Linden et al. reported a statistically significant improvement in the EQ-5D scores of the intervention group compared with the control group [36].
Mortality Mortality was reported in three of the nine studies at different follow-up periods [31, 35, 36]. Deprescribing interventions to reduce PIMs were not associated with significant changes in mortality.
Hospitalisations Four studies measured hospital readmissions [31, 32, 35, 36]. Three studies reported no difference in hospitalisations [31, 35, 36], and in the other study, which analysed the association between scores for MAI and STOPP and total readmissions, no significant association was detected [32].
Falls Three studies reported the impact on falls as an outcome at discharge [33, 36, 37], and one study reported falls at 6 months post-discharge [31]. A statistically significant reduction in falls was reported in one study [33].
Functional status Two studies assessed functional status using the Barthel index [33, 37], and one study reported a significant improvement in function at discharge [37].
4 Discussion
Inappropriate medication prescribing is prevalent in older inpatients. Hospitalisation presents a valuable opportunity to deprescribe PIMs in the context of the individual’s morbidities and goals of care. This systematic review assessed the impact of deprescribing interventions on prescribing and clinical outcomes in older patients in the hospital setting. Seven of the nine included studies reported a statistically significant reduction in PIMs in the intervention group [29,30,31,32, 34, 36, 37] and no study showed an increase in PIMs. Across the four studies that analysed the effect beyond hospital discharge, the results were mixed.
Few systematic reviews have focussed on the impact of deprescribing interventions on PIMs. A recently updated Cochrane review on the impact of interventions on appropriate use of polypharmacy reported an overall reduction in inappropriate medication usage following intervention [38]. However, only three of the twelve included controlled trials were in an inpatient setting. The findings of this systematic review are useful for the multidisciplinary care team in hospital as it provides evidence that deprescribing interventions can be implemented in the acute hospital setting in medical and surgical wards, and can reduce PIMs, which are associated with several adverse effects.
The number of studies in this systematic review was too small to comment on variation in outcome according to intervention type. Only three of the nine studies compared reduction in PIMs from admission to discharge between intervention and control group [32, 34, 37]. All three studies reported a statistically significant reduction in PIMs, even though they employed different deprescribing interventions and tools. Other systematic reviews evaluating the impact of deprescribing interventions on PIMs have largely focussed on studies implementing pharmacist-led interventions in heterogenous settings [38, 39]. Studies comparing the efficacy of different deprescribing interventions on reduction of PIMs are lacking. In addition, it would be important for future studies to provide more complete descriptions of deprescribing interventions using the recently published TIDieR checklist [40]. Detailed reporting of trial interventions will allow replication of these interventions in future studies across other settings, and enable healthcare professionals to translate these interventions into routine clinical care.
As the evidence for the efficacy and safety of deprescribing grows, future studies should focus on developing and evaluating models of care that incorporate deprescribing guidelines and multidisciplinary care. Future work in this area could include developing and evaluating the use of computerised clinical decision support systems to facilitate clinicians to identify and deprescribe PIMs. For example, clinical decision support systems have been developed for the Beers criteria through a mobile application called ‘iGeriatrics’, the STOPP/START criteria through the STRIP assistant [41] and there is a software version of the DBI that calculates the DBI and generates a report for treating physicians [42].
This review also assessed the impact of deprescribing interventions on clinical outcomes. None of the studies were powered to evaluate these secondary clinical outcomes. Drug-related problems including ADRs were reported in three studies [29, 34, 37], health-related quality of life in two studies [29, 36], mortality in three studies [31, 35, 36], hospital readmissions in four studies [31, 32, 35, 36], falls in three studies [31, 33, 36, 37] and functional status using the Barthel index in two studies [33, 37]. In general, the results were mixed. The mortality rate was lower in the intervention group at follow-up, but the results were not statistically significant [31, 35, 36]. There was no significant impact on readmission rates [31, 32, 35, 36]. A number of recent meta-analyses on the impact of deprescribing interventions in various settings on mortality and readmissions have been published, with all reporting no significant improvement [16, 20, 23]. In this systematic review of hospital-based deprescribing studies, no strong evidence was found for an effect on clinical outcomes. This could be resolved by adequately powered studies designed to specifically evaluate clinically relevant and patient-centred endpoints such as quality of life and functional status.
4.1 Strengths and Limitations
This is the first systematic review to specifically investigate the impact of deprescribing interventions on prescribing outcomes for older patients in hospital. A comprehensive search strategy was undertaken with two reviewers independently screening all results retrieved by searching eight large databases. However, as there is no MeSH term for ‘deprescribing’, a broad search strategy was utilised which yielded a high number of results. The search was limited to studies in English and published after 1995, and further search terms were used to exclude irrelevant studies as detailed in Sect. 2.
Due to significant heterogeneity in intervention type and outcome measures, a meta-analysis could not be undertaken. Missing data could not be retrieved for some studies. Conclusions on efficacy by intervention type could not be made due to small numbers of studies with similar interventions and similar outcome measures. Most studies had short-term follow up, and thus the long-term impact of interventions is still unclear. This review included only RCTs. However, the quality of the included trials varied. Randomisation was adequate in two of the nine studies [31, 34]. Only five of the nine studies were powered for the primary outcome [30, 31, 35,36,37]. None of the studies were powered to examine the secondary outcomes. The presence of a high risk of bias should be considered when interpreting the results of this review.
Since the protocol for this systematic review was registered, the TIDieR checklist for systematic reviews has been published [43]. The TIDieR checklist was developed in response to the incomplete reporting of intervention details in many trials and subsequent systematic reviews of trials. Application of the TIDieR checklist to this systematic review may have enabled better descriptions and comparisons of the deprescribing interventions. In terms of limitations to the scope of this systematic review, reduction of PIMs is only one part of a comprehensive medication review to optimise quality use of medicines in older patients.
5 Conclusions
Our findings suggest that deprescribing interventions targeted at older adults admitted to hospital can reduce PIMs. The interventions appear to be safe and in some cases may be feasible to implement into usual care. However, the impact on clinical outcomes is unclear and the current evidence is weak and of low quality. Most of the studies were relatively recent and reflect the growing activity in this field. It should be noted that PIMs are a surrogate outcome, and reduction of PIMS is only one part of a comprehensive medication review to optimise prescribing for older adults. Therefore, future studies should be powered to evaluate clinically relevant outcomes including functional status, falls, rehospitalisation, and mortality. In addition to building evidence on the outcomes, translation of the study findings into routine clinical care should be explored using implementation studies.
References
Australian Institute of Health and Welfare. Australia’s hospitals 2014–2015 at a glance. Health Services Series, No. 70. Catalogue No. HSE 175 Canberra, Australia; 2016.
Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel J-P, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–54.
Garin N, Koyanagi A, Chatterji S, Tyrovolas S, Olaya B, Leonardi M, et al. Global multimorbidity patterns: a cross-sectional, population-based, multi-country study. J Gerontol A Biol Sci Med Sci. 2016;71(2):205–14.
Held FP, Blyth F, Gnjidic D, Hirani V, Naganathan V, Waite LM, et al. Association rules analysis of comorbidity and multimorbidity: the concord health and aging in men project. J Gerontol A Biol Sci Med Sci. 2016;71(5):625–31. https://doi.org/10.1093/gerona/glv181.
Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10(4):430–9.
American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227–46. https://doi.org/10.1111/jgs.13702.
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–8. https://doi.org/10.1093/ageing/afu145.
Ni Chroinin D, Neto HM, Xiao D, Sandhu A, Brazel C, Farnham N, et al. Potentially inappropriate medications (PIMs) in older hospital in-patients: prevalence, contribution to hospital admission and documentation of rationale for continuation. Australas J Ageing. 2016;35(4):262–5.
Beer C, Hyde Z, Almeida OP, Norman P, Hankey GJ, Yeap BB, et al. Quality use of medicines and health outcomes among a cohort of community dwelling older men: an observational study. Br J Clin Pharmacol. 2011;71(4):592–9.
Gnjidic D, Hilmer SN, Blyth FM, Naganathan V, Waite L, Seibel MJ, et al. Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol. 2012;65(9):989–95.
Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57–65.
Wallace E, McDowell R, Bennett K, Fahey T, Smith SM. Impact of potentially inappropriate prescribing on adverse drug events, health related quality of life and emergency hospital attendance in older people attending general practice: a prospective cohort study. J Gerontol A Biol Sci Med Sci. 2017;72(2):271–7.
Woodward MC. Deprescribing: achieving better health outcomes for older people through reducing medications. J Pharm Pract Res. 2003;33(4):323–8.
Reeve E, Gnjidic D, Long J, Hilmer S. A systematic review of the emerging definition of ‘deprescribing’ with network analysis: implications for future research and clinical practice. Br J Clin Pharmacol. 2015;80(6):1254–68.
Gnjidic D, Le Couteur DG, Kouladjian L, Hilmer SN. Deprescribing trials: methods to reduce polypharmacy and the impact on prescribing and clinical outcomes. Clin Geriatr Med. 2012;28(2):237–53.
Page AT, Clifford RM, Potter K, Schwartz D, Etherton-Beer CD. The feasibility and effect of deprescribing in older adults on mortality and health: a systematic review and meta-analysis. Br J Clin Pharmacol. 2016;82(3):583–623.
Iyer S, Naganathan V, McLachlan AJ, Le Couteur DG. Medication withdrawal trials in people aged 65 years and older. Drugs Aging. 2008;25(12):1021–31.
Boghossian TA, Rashid FJ, Welch V, Rojas-Fernandez C, Moayyedi P, Pottie K, et al. Deprescribing versus continuation of chronic proton pump inhibitor use in adults. Cochrane Database Syst Rev. 2015;16(3):CD011969. https://doi.org/10.1002/14651858.cd011969.pub2.
Declercq T, Petrovic M, Azermai M, Vander Stichele R, De Sutter A, van Driel ML, et al. Withdrawal versus continuation of chronic antipsychotic drugs for behavioural and psychological symptoms in older people with dementia. Cochrane Database Syst Rev. 2013;28(3):CD007726. https://doi.org/10.1002/14651858.cd007726.pub2.
Johansson T, Abuzahra ME, Keller S, Mann E, Faller B, Sommerauer C, et al. Impact of strategies to reduce polypharmacy on clinically relevant endpoints: a systematic review and meta-analysis. Br J Clin Pharmacol. 2016;82(2):532–48.
Qi K, Reeve E, Hilmer SN, Pearson S-A, Matthews S, Gnjidic D. Older peoples’ attitudes regarding polypharmacy, statin use and willingness to have statins deprescribed in Australia. Int J Clin Pharm. 2015;37(5):949–57. https://doi.org/10.1007/s11096-015-0147-7.
Chan B, Reeve E, Matthews S, Carroll PR, Long JC, Held F, et al. Medicine information exchange networks among healthcare professionals and prescribing in geriatric medicine wards. Br J Clin Pharmacol. 2017;83(6):1185–96. https://doi.org/10.1111/bcp.13222.
Christensen M, Lundh A. Medication review in hospitalised patients to reduce morbidity and mortality. Cochrane Database Syst Rev. 2016;2:Cd008986. https://doi.org/10.1002/14651858.cd008986.pub3.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Hilmer SN, Mager DE, Simonsick EM, et al. A drug burden index to define the functional burden of medications in older people. Arch Intern Med. 2007;167(8):781–7. https://doi.org/10.1001/archinte.167.8.781.
Hanlon JT, Schmader KE, Samsa GP, Weinberger M, Uttech KM, Lewis IK, et al. A method for assessing drug therapy appropriateness. J Clin Epidemiol. 1992;45(10):1045–51.
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–8. https://doi.org/10.1093/ageing/afu145.
Higgins JPT, Altman DG, Sterne JAC. Chapter 8: assessing risk of bias in included studies. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. (updated March 2011). ed: The Cochrane Collaboration, 2011.
Bladh L, Ottosson E, Karlsson J, Klintberg L, Wallerstedt SM. Effects of a clinical pharmacist service on health-related quality of life and prescribing of drugs: a randomised controlled trial. BMJ Qual Saf. 2011;20(9):738–46. https://doi.org/10.1136/bmjqs.2009.039693.
Dalleur O, Boland B, Losseau C, Henrard S, Wouters D, Speybroeck N, et al. Reduction of potentially inappropriate medications using the STOPP criteria in frail older inpatients: a randomised controlled study. Drugs Aging. 2014;31(4):291–8. https://doi.org/10.1007/s40266-014-0157-5.
Gallagher PF, O’Connor MN, O’Mahony D. Prevention of potentially inappropriate prescribing for elderly patients: a randomized controlled trial using STOPP/START criteria. Clin Pharmacol Ther. 2011;89(6):845–54. https://doi.org/10.1038/clpt.2011.44.
Gillespie U, Alassaad A, Hammarlund-Udenaes M, Mörlin C, Henrohn D, Bertilsson M, et al. Effects of pharmacists’ interventions on appropriateness of prescribing and evaluation of the instruments’(MAI, STOPP and STARTs’) ability to predict hospitalization–analyses from a randomized controlled trial. PLoS One. 2013;8(5):e62401.
Michalek C, Wehling M, Schlitzer J, Frohnhofen H. Effects of ‘Fit fOR The Aged’ (FORTA) on pharmacotherapy and clinical endpoints-a pilot randomized controlled study. Eur J Clin Pharmacol. 2014;70(10):1261–7. https://doi.org/10.1007/s00228-014-1731-9.
Schmader KE, Hanlon JT, Pieper CF, Sloane R, Ruby CM, Twersky J, et al. Effects of geriatric evaluation and management on adverse drug reactions and suboptimal prescribing in the frail elderly. Am J Med. 2004;116(6):394–401. https://doi.org/10.1016/j.amjmed.2003.10.031.
Spinewine A, Swine C, Dhillon S, Lambert P, Nachega JB, Wilmotte L, et al. Effect of a collaborative approach on the quality of prescribing for geriatric inpatients: a randomized, controlled trial. J Am Geriatr Soc. 2007;55(5):658–65. https://doi.org/10.1111/j.1532-5415.2007.01132.x.
Van der Linden L, Decoutere L, Walgraeve K, Milisen K, Flamaing J, Spriet I, et al. Combined use of the rationalization of home medication by an adjusted STOPP in older patients (RASP) list and a pharmacist-led medication review in very old inpatients: impact on quality of prescribing and clinical outcome. Drugs Aging. 2017;34(2):123–33. https://doi.org/10.1007/s40266-016-0424-8.
Wehling M, Burkhardt H, Kuhn-Thiel A, Pazan F, Throm C, Weiss C, et al. VALFORTA: a randomised trial to validate the FORTA (Fit fOR The Aged) classification. Age Ageing. 2016;45(2):262–7. https://doi.org/10.1093/ageing/afv200.
Patterson SM, Cadogan CA, Kerse N, Cardwell CR, Bradley MC, Ryan C, et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.cd008165.pub3.
Walsh KA, O’Riordan D, Kearney PM, Timmons S, Byrne S. Improving the appropriateness of prescribing in older patients: a systematic review and meta-analysis of pharmacists’ interventions in secondary care. Age Ageing. 2016;45(2):201–9. https://doi.org/10.1093/ageing/afv190.
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. https://doi.org/10.1136/bmj.g1687.
Meulendijk MC, Spruit MR, Drenth-van Maanen AC, Numans ME, Brinkkemper S, Jansen PAF, et al. Computerized decision support improves medication review effectiveness: an experiment evaluating the STRIP assistant’s usability. Drugs Aging. 2015;32(6):495–503. https://doi.org/10.1007/s40266-015-0270-0.
Kouladjian L, Gnjidic D, Chen TF, Hilmer SN. Development, validation and evaluation of an electronic pharmacological tool: the drug burden index calculator(c). Res Soc Adm Pharm. 2016;12(6):865–75. https://doi.org/10.1016/j.sapharm.2015.11.002.
Hoffmann TC, Oxman AD, Ioannidis JP, Moher D, Lasserson TJ, Tovey DI, et al. Enhancing the usability of systematic reviews by improving the consideration and description of interventions. BMJ. 2017;358:j2998. https://doi.org/10.1136/bmj.j2998.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was used in the preparation of this manuscript. However, the findings will inform NSW Health Translational Research Grant 274, ‘Reducing Inappropriate Polypharmacy in Older Inpatients’, chief investigator Sarah Hilmer.
Conflict of interest
Janani Thillainadesan, Danijela Gnjidic, Sarah Green and Sarah Hilmer declare that they have no conflicts of interest relevant to the content of this review.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Thillainadesan, J., Gnjidic, D., Green, S. et al. Impact of Deprescribing Interventions in Older Hospitalised Patients on Prescribing and Clinical Outcomes: A Systematic Review of Randomised Trials. Drugs Aging 35, 303–319 (2018). https://doi.org/10.1007/s40266-018-0536-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-018-0536-4