Abstract
Purpose of Review
Comorbid insomnia and sleep apnea (COMISA) is prevalent and carries significant morbidity but lacks a standardized diagnostic and therapeutic approach. Through a critical evaluation of the literature, we propose a novel approach to COMISA that incorporates the underlying etiology and existence of different phenotypes in this disorder.
Recent Findings
A low arousal threshold and/or hyperarousability may underlie the development of COMISA. Pretreatment symptoms may serve as baseline predictors of response to positive airway pressure therapy in COMISA and differentiate insomnia secondary to OSA from independent insomnia. A variety of therapeutic strategies for COMISA have been put forward with evidence supporting the use of monotherapy or combined therapy in the appropriate clinical setting.
Summary
Patients with either OSA or insomnia must be effectively screened for both disorders based on presenting symptoms and response to therapy. Recognition of the underlying etiology of COMISA and the different COMISA phenotypes can guide therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The co-occurrence of insomnia and obstructive sleep apnea (OSA) was first described in 1973 by Guilleminault and colleagues [1]. However, it was not until Krakow et al. reported in 2001 that approximately 50% of OSA patients also had insomnia symptoms that research on this phenomenon began to accelerate [2•]. Despite the realization that this comorbidity has major implications for disease-related outcomes, it remains underrecognized and currently lacks a standardized diagnostic approach and treatment algorithm [3, 4]. The absence of an accepted nosology for this disorder, noting in the medical literature the terminology used includes OSA-insomnia [5], complex insomnia [6], and comorbid insomnia and OSA among others, contributes to these variances in research and clinical practice. The term “COMISA” for comorbid insomnia and sleep apnea appropriately conveys the presence of both conditions in a memorable and unifying term. In this paper, we highlight the clinical features of COMISA and its frequent association with behavioral medicine disorders. The diagnostic and therapeutic strategies to date and the barriers to appropriate diagnosis and treatment will be reviewed. Finally, a novel approach to diagnosing and treating this increasingly recognized disorder in sleep medicine will be proposed.
Obstructive Sleep Apnea and Insomnia
OSA is one of the most common sleep disorders and affects 3–7% of adults [7]. It is characterized by repetitive apneas and hypopneas caused by upper airway collapse during sleep that result in oxygen desaturations, arousals, and sleep fragmentation. The severity of OSA is determined by the number of apneas and hypopneas per hour of sleep, or apnea-hypopnea index (AHI) [8]. Common symptoms of OSA include daytime sleepiness, snoring, sensations of gasping or choking, and witnessed breathing interruptions during sleep [9••]. There are findings that support different presentations of OSA. Ye et al. described three clusters of OSA patients (disturbed sleep, minimally symptomatic, and excessive daytime sleepiness) with the “disturbed sleep” cluster manifesting primarily as insomnia symptoms [10]. Traditionally, the diagnosis of OSA is made by an overnight in-lab polysomnogram (PSG); however, home sleep apnea testing (HSAT) that focuses solely on diagnosing sleep-disordered breathing (SDB) is increasingly utilized. In patients with OSA and insomnia, the American Academy of Sleep Medicine recommends PSG as opposed to HSAT [11]. This distinction is important as patients with primarily OSA symptoms also need to be assessed for insomnia symptoms to ensure appropriate diagnostic testing.
Symptoms of insomnia include difficulty in initiating and/or maintaining sleep, associated with significant daytime impairment [8]. Chronic insomnia disorder is defined as symptoms at least three times a week for at least 3 months [8]. Insomnia is the most common sleep complaint among adults [12] and approximately 20–30% of US adults have experienced insomnia symptoms [13, 14]. Prevalence of chronic insomnia disorder is estimated to be between 6 and 10% [14, 15]. The diagnosis of insomnia requires a clinical evaluation including a sleep, medical, and psychiatric history. Objective testing, such as PSG and actigraphy, is not routinely used in patients with insomnia symptoms, except to rule out SDB or sleep-related movement disorders [15, 16]. However, the PSG variables of sleep onset latency (SOL) (≥ 31 min), wakefulness after sleep onset (WASO) (≥ 31 min), and sleep efficiency (SE) (< 85%) can indicate underlying insomnia, even in the setting of mild OSA [17].
Comorbid Insomnia and Obstructive Sleep Apnea
Insomnia can be comorbid with a number of psychiatric and sleep disorders, and historically, it was thought to be a consequence of the primary disorder, which has likely contributed to underdiagnosis of COMISA [18]. However, insomnia can persist after treatment of the primary disorder and responds to insomnia-specific therapy [18, 19]. Nomenclature has been updated to reflect this and insomnia is now considered “comorbid” in such cases [12].
Prevalence of COMISA
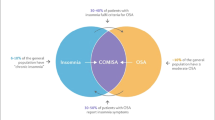
The prevalence is difficult to establish as there is marked variability in rates of COMISA diagnoses between studies, ranging from 10.7% [20] to 88% [17]. This variability exists because of different diagnostic methods and populations assessed. Regarding diagnostic methods, studies have assessed patients initially diagnosed with OSA for insomnia or insomnia patients with OSA, whereas more recent studies have assessed for COMISA at initial presentation. Comorbid insomnia among patients with OSA was similar in the primary care population (34%) and middle-aged women (23–31%) [21, 22]. A recent study reported that COMISA was present in 29.2% of patients at a Korean sleep center referred for PSG [23•]. Studies in specific populations, such as older adults, military personnel, and sexual assault victims, show large variations in prevalence. For example, given the high rates of insomnia [24] and sleep apnea [25] in the elderly, it is estimated as many as 2 million older adults in the USA may have COMISA [26•]. Further, military personnel and veterans have higher rates of COMISA (38.2–88%) than general sleep clinic populations [17, 27, 28]. Krakow et al. estimated the rate of OSA in female sexual assault victims to be 52% [29]. In populations with prior traumatic experiences, there are higher rates of psychiatric disorders including anxiety, depression, and post-traumatic stress disorder (PTSD). These psychiatric disorders are associated with both insomnia [30,31,32,33] and OSA [34, 35], providing a basis that specific patient populations are at higher risk of developing COMISA.
Underlying Etiology of COMISA
The relationship between OSA and insomnia is complex, as both are typically viewed as distinct sleep disorders. However, studies suggest that these two disorders may be interrelated, as opposed to independent. The OSA and insomnia relationship is described as bidirectional and causal, with OSA contributing to the development of insomnia (primarily maintenance insomnia) and insomnia exacerbating OSA [9••]. Repeated awakenings from SDB can condition a patient to develop insomnia. The converse is not viewed the same, as insomnia is not typically considered a contributor to SDB. However, there is an evolving line of scientific evidence that individuals with a low arousal threshold (LAT) and/or elevated loop gain are predisposed to developing SDB [36•]. The LAT is an important non-anatomical factor which can contribute to the pathogenesis of OSA in as many as one third of OSA patients [37,38,39]. Specifically, frequent transitions from sleep to wake (as can occur with initiation insomnia and associated cortical arousals) can result in ventilatory overshoot while awake. As the LAT patient transitions back to sleep, either a frank central apnea or central hypopnea ensues, resulting in increasing the CO2 level to the sleep ventilatory threshold; this can become repetitive, particularly in those with high loop gain [40]. Cortical arousals, which can be induced from multiple stimuli, are initially protective of maintaining airway patency when there is airway closure [41]. Conversely, repeated arousals, whether respiratory or non-respiratory in nature, can result in the aforementioned pattern of breathing instability. This provides a basis that not only can OSA cause maintenance insomnia, but insomnia, through increased arousability [42, 43], may result in the development or exacerbation of OSA.
Clinical Impact of COMISA
Patients with COMISA report greater sleep disturbances than patients with either disorder alone [44]. They also have worse health-related quality of life (QOL), sleep-related functional outcomes, and mental health outcomes [5, 45,46,47,48]. Interestingly, there is evidence that the negative effects of COMISA on fatigue and QOL may impact males more than females [49]. Not surprisingly, objective sleep is degraded in patients with COMISA compared to insomnia or OSA alone. For example, veterans with COMISA have more indicators of poor sleep including reduced total sleep time (TST) and longer SOL, despite a lower AHI, compared to veterans with OSA alone [4]. Poor objective sleep has been reported in military personnel with COMISA who had lower SE, increased SOL, decreased TST, and increased WASO compared to patients with insomnia or OSA alone [17, 27]. Along those lines, Li et al. compared PSG variables of patients with insomnia alone to patients with COMISA. They demonstrated that patients with COMISA had worse objective sleep quality with increased N1 sleep, decreased N3 sleep, and increased arousal indices [50]. These findings are consistent with those observed by and Krakow et al. and Smith et al. comparing patients with COMISA and those with OSA alone [2•, 5]. Lee et al. found significantly decreased TST, SE, and SOL in males but not in females with COMISA compared to OSA alone [49]. Further, Cho et al. found that COMISA patients had increased SOL, decreased TST, increased WASO, and decreased SE compared to patients with OSA alone despite no difference in AHI between these groups [23•]. These objective sleep derangements may contribute to the overall morbidity of COMISA but this relationship warrants further investigation [23•].
Despite what little is known regarding the etiological relationship between insomnia and OSA, the co-occurrence of these sleep disorders challenges traditional treatment approaches [51]. Growing evidence indicates that insomnia is a risk factor for poor positive airway pressure (PAP) therapy adherence [1]. Insomnia symptoms, both at presentation and at follow-up, in OSA patients predict worse PAP usage [52•, 53]. Wallace et al. compared sleep characteristics and PAP adherence in veterans diagnosed with COMISA to those with OSA alone [53]. Patients with early and late insomnia symptoms had worse PAP adherence at 6 months compared to veterans without insomnia symptoms. Another prospective study assessing 73 patients with OSA receiving PAP therapy found patients who were less complaint with treatment (< 4 h/night) reported greater insomnia symptoms [54]. Lam et al. assessed insomnia in a PAP alternatives clinic with the insomnia severity index (ISI). In this cohort of 172 OSA patients who were intolerant of either PAP or oral appliance treatment, 56.8% were found to have clinically significant insomnia [55]. Thus, there are a number of studies which associate COMISA with decreased PAP adherence compared to OSA alone. What is unknown is how much insomnia impacts PAP adherence or whether intolerance of PAP is a potential marker of a distinct COMISA phenotype [9••].
Treatment of OSA also appears to impact insomnia symptoms in patients with COMISA. In a study of 705 adults with OSA, Bjornsdottir et al. examined changes in insomnia symptoms before and after PAP treatment [52•]. While symptoms of middle (maintenance) insomnia decreased after 2 years of PAP treatment, initial and late insomnia persisted and were associated with poor PAP adherence. This study provides further support that different phenotypes of COMISA may exist depending on symptomatology. In this case, frequent middle of the night awakenings was predictive of PAP adherence. OSA with associated early and late insomnia may represent a different COMISA phenotype altogether, one that would benefit from addressing insomnia concomitantly or prior to initiation of PAP [56]. These findings reinforce the need for additional studies to determine whether treatment of insomnia (either with cognitive behavioral therapy for insomnia [CBT-I] or pharmacotherapy) would lead to improved PAP usage and overall improved outcomes in COMISA.
COMISA and Associated Psychiatric Disorders
A number of studies have compared the behavioral medicine disorders associated with COMISA in relation to having either OSA or insomnia alone [5, 23•, 27, 45, 49, 57,58,59,60]. In these studies, COMISA was nearly always associated with worse overall sleep quality, mood, and depressive symptoms and higher rates of behavioral medicine comorbidities. Although specific behavioral health diagnoses were not reported, Krakow et al. found that patients with COMISA reported more cognitive-emotional symptoms (i.e., depression and anxiety), more psychiatric disorders, and more mental symptoms than patient with OSA alone [2•]. Similarly, Krell and Kapur reported that patients with COMISA were more likely to report a psychiatric diagnosis [58]. Several studies have compared the rate and/or severity of specific behavioral health diagnoses in patients with COMISA compared to insomnia or OSA alone (Table 1). In a study conducted in military personnel, Mysliwiec et al. found those with COMISA were significantly more likely to have depression, PTSD, and > 2 behavioral medicine disorders than patients with either insomnia or OSA alone [27]. In another study, they found increased rates of depression and anxiety in military personnel with COMISA compared to those with mild OSA alone [17]. Smith et al. assessed the clinical impact of COMISA versus OSA alone and found that patients with COMISA had worse anxiety, depression, stress, and mood disturbance symptoms [5]. Similarly, in a large population-based sample of US adults, Hayley et al. found an increased likelihood of reporting depression in COMISA patients than patients who did not report sleep disorders. After adjusting for confounding variables, COMISA patients were also more likely to report depression than patients with insomnia or OSA alone [45]. In a study in veterans, El-Solh et al. evaluated the response to PAP of 36 patients with COMISA and PTSD compared to 36 patients with OSA and PTSD. The veterans with COMISA were more likely to have depression, increased PTSD symptoms, and decreased sleep quality and daytime functioning compared to veterans with OSA alone. Notably, the COMISA patients also demonstrated significantly lower PAP adherence [57]. Yang et al. assessed and compared the psychological and behavioral outcomes in 88 male patients with OSA only, insomnia only, and COMISA using PSG and questionnaires. In patients in the COMISA and insomnia-only groups, higher levels of presleep arousal, anxiety, and depression were reported than in patients in the OSA-only group [60]. In a study characterizing the clinical profile of Australian men previously undiagnosed with OSA, greater prevalence and severity of depressive symptoms were reported in patients with COMISA, compared to those with OSA or insomnia symptoms alone [59]. These patients also reported increased daytime dysfunction and reduced sleep quality, as well as low subscale scores on functional health and well-being health-related QOL outcomes on the 36-item short form (SF-36) survey. In a study by Lee et al. comparing gender differences in patients with OSA, the presence of insomnia symptoms had negative effects on depression and anxiety in males. Interestingly, this result was not found in females and was negated in males when gender-by-insomnia interaction was taken into consideration [49]. Finally, Cho et al. found a higher rate of depressive mood in a cohort of Korean patients with COMISA compared to OSA alone. Worse sleep quality may contribute to mood disturbance as COMISA patients had objectively worse sleep than patients with OSA alone, noting there was no significant difference in AHI between groups [23•].
Diagnostic Challenges of COMISA
There are currently three major approaches to diagnosing COMISA:
-
1.
Consider a diagnosis of COMISA in OSA patients on PAP with continued symptoms of initiation and terminal (early morning) insomnia. Maintenance insomnia tends to improve with PAP treatment, suggesting that it is a consequence of OSA [52•]. However, initiation and terminal insomnia do not necessarily improve with PAP, suggesting that patients with these subtypes of insomnia should be further evaluated for COMISA [52•].
-
2.
Evaluate patients with insomnia for OSA when they have OSA risk factors or are refractory to treatment with either CBT-I or pharmacotherapy. The risk factors for OSA in insomnia patients include male sex (especially in insomnia patients < 55 years old), post-menopausal women, snoring, and elevated BMIs [50]. In insomnia patients, higher AHI is associated with worse sleep quality and reduction in perceived sleep; thus, it is reasonable to evaluate patients who are refractory to insomnia treatment for OSA [50].
-
3.
A less often used method involves using the PSG to diagnose OSA and simultaneously using the ISI to diagnose insomnia before treatment is started [53, 61]. Because the last four questions of the ISI ask about symptoms that could be shared by OSA and insomnia, these studies suggest using just the first three questions (nocturnal symptoms) for diagnosis of insomnia. These questions have been shown to be a reliable measure of insomnia severity [62, 63]. However, it is not established what numerical cutoff should be applied for the first three questions, as scores of both 4 and 6 were utilized [50, 59].
To date, these diagnostic approaches have not been adequate as a majority of COMISA patients go undiagnosed for a variety of reasons, including a lack of a standardized approach [4]. Diagnosis of COMISA is complicated by a fact that the two disorders share many of the same symptoms. Fatigue, frequent awakenings, non-restorative sleep, and difficulty in maintaining sleep are just a few. Further, complicating a COMISA diagnosis is a fact that once patients are diagnosed with either insomnia or OSA, evaluation for the other diagnosis may not be pursued. In OSA patients who are non-adherent to PAP, assessment for insomnia is not routine or recommended and over half of these patients may have clinically significant insomnia [55]. In patients with insomnia, OSA may be present but is often overlooked. For instance, Fung et al. performed HSAT on 435 veterans with insomnia and found that almost half (46.7%) had an AHI of ≥ 15/h [64]. Additionally, in a large clinical population of 1035 treatment-seeking insomnia patients, 42% reported a sleep-related breathing disorder as another reason for their evaluation [65]. Along those lines, Krakow et al. reported that in 20 “classic” insomnia patients who underwent in-lab attended PSGs, 90% of the awakenings were the result of SDB [66]. While limited by size, this study provides some evidence to suggest that the nocturnal symptoms reported by patients may not help categorize their disorder. Unfortunately, many times the symptoms a patient perceives, as opposed to objective findings, drive the evaluation and ultimately diagnosis.
Another barrier to diagnosing COMISA is that, unlike many disorders, there is no classic presentation. A patient’s symptomatology and disease course can be quite variable [9••]. We propose that COMISA patients manifest as one of three phenotypes and recognition of these variable presentations will aid in diagnosis and treatment. The first phenotype encompasses patients with mild OSA (AHI < 15/h) and insomnia. These patients may also have an accompanying disorder of hyperarousal, such as PTSD or anxiety, though not necessarily. The insomnia complaints in this population, often early and/or late insomnia, will typically predominate and be refractory to PAP therapy [52•]. These patients may be younger and thinner than the other COMISA phenotypes, and the OSA in this group is often caused by LAT with or without high loop gain [41, 67] and/or hyperarousal [5, 43, 68,69,70,71]. The second phenotype represents patients with moderate to severe OSA (AHI > 15/h), maintenance insomnia complaints, and few other comorbidities. These patients, typically with higher AHIs, often present with complaints consistent with SDB as well as frequent nocturnal awakenings; they typically respond well to PAP and have improved maintenance insomnia [52•, 61]. For this second phenotype, it is reasonable to deduce that the insomnia originated secondary to the SDB [3, 72, 73]. Finally, the third phenotype encompasses patients with moderate to severe OSA with insomnia who do not respond to PAP or are non-adherent. In this group, the insomnia does not improve with PAP usage and it is reasonable to conclude that insomnia is independent of the SDB [26•]. These patients can be challenging to identify and they may present with complaints of SDB, insomnia, or both [26•]. Classifying patients into phenotypes or clusters by their symptomatology, which has been performed in insomnia, may guide tailored therapy and enhance patient care [74].
COMISA Therapy
The ideal treatment regimen for COMISA remains theoretical due to a lack of randomized controlled trials. Despite this, there is consensus that COMISA is more difficult to treat than either OSA or insomnia alone [75••]. Therapy may be guided, to a large extent, by which disease is diagnosed first and whether or not the insomnia is felt to be independent of the SDB or interrelated to it. Making this determination from symptoms prior to therapy can be difficult [76]. For this reason, research on treatment of COMISA has generally focused on treating insomnia and sleep apnea independently or in a stepwise fashion rather than simultaneously. Prior studies on the treatment of COMISA have been reviewed in detail elsewhere [75••]. Below is a summary of the currently proposed therapeutic strategies and a discussion of the challenges to effective implementation.
Positive Airway Pressure Therapy in COMISA
PAP remains the first-line recommendation and most widely used treatment for OSA [72]. Acceptance and usage of PAP is variable with estimates of non-adherence to use of at least 4 h per night ranging from 29 to 83% [77]. The presence of insomnia can worsen PAP adherence [28, 51, 52•, 54, 78] and COMISA patients likely require more time and effort to tolerate PAP compared to patients with OSA alone [2•, 79]. In theory, the addition of a mask may lead to physical discomfort and worsen a patient’s insomnia [80]. Despite this, several studies have demonstrated improvement in both insomnia and OSA symptoms in COMISA patients using PAP therapy alone [52•, 56, 61, 79, 81,82,83]. Importantly, a one-size-fits-all approach may not be appropriate. Krakow et al. reported that advanced modes of non-invasive ventilation, including adaptive servo-ventilation, may prove beneficial in patients intolerant of PAP [79, 83]. It may also be important to find baseline characteristics of COMISA patients that predict insomnia that responds to PAP therapy including frequent nocturnal awakenings [52•] and higher AHI [61]. Such characteristics are potential indicators that insomnia may be secondary to OSA and thus more likely to respond to PAP therapy. Further research is needed to determine additional features of COMISA patients that predict responsiveness of insomnia symptoms to PAP or aid in tailoring therapy.
Insomnia Therapy in COMISA
The mainstays of insomnia treatment remain CBT-I and sedative medications [16]. CBT-I is an effective therapy for insomnia with behavioral components including stimulus control and sleep restriction that target the maladaptive processes underlying insomnia [15, 84, 85]. As a non-pharmacologic approach without side effects, when available, it is recommended as first-line therapy for insomnia over the use of hypnotic medications [16, 86]. Although earlier research on the use of CBT-I in COMISA patients demonstrated conflicting results [87,88,89], more recent studies support its effectiveness in treating this patient population [90•, 91•]. In a randomized controlled trial, Fung et al. found that CBT-I improved SOL and sleep quality in veterans with insomnia with and without untreated mild OSA [91•]. Whether or not insomnia is secondary to OSA may influence the efficacy of CBT-I in COMISA patients [92]. Arousals from SDB causing fragmented sleep may contribute to wakefulness and sleep-state misperception that would seem unlikely to respond to CBT-I alone [52•, 66, 93]. However, in a retrospective review of 455 patients with insomnia, Sweetman et al. found that CBT-I significantly improved insomnia symptoms and daytime functioning at 3 months with no difference in improvement between patients with or without comorbid sleep apnea, regardless of OSA severity [90•]. This finding suggests that few patients in the cohort were suffering from insomnia exclusively secondary to OSA and that CBT-I can improve insomnia in COMISA patients prior to PAP [94]. Interestingly, sleep restriction did not increase sleepiness post-treatment in the COMISA patients. An important limitation of the study was that the patients studied sought therapy for insomnia rather than OSA. The presenting complaint and COMISA phenotype may very well influence treatment response [93, 95].
Studies on the use of hypnotic therapy alone to treat COMISA are limited, with one case study reporting no symptomatic improvement [93]. In patients with insomnia, hypnotics have been shown to improve sleep outcomes such as TST and SOL and may be useful when CBT-I alone is ineffective [96]. In patients with OSA, hypnotics appear to be safe for those patients initiating PAP and may improve PAP adherence in those reporting difficulty initiating and maintaining sleep [9••]. Several classes of hypnotics exist, each with variable therapeutic impact on insomnia and OSA symptoms. Benzodiazepines increase sleep duration [97, 98] but may worsen sleep apnea by reducing upper airway muscle tone and decreasing ventilatory response to hypoxia [99,100,101], though the effect is likely modest and may be insignificant [102]. However, the myriad of side effects caused by benzodiazepines, particularly in the elderly population, limits their widespread applicability in the COMISA population [16, 103]. The popular GABAergic non-benzodiazepine agents, including zolpidem and eszopiclone, have less impact on respiration and appear to facilitate PAP adherence [104, 105]. There is evidence that non-benzodiazepine agents may increase the arousal threshold and improve AHI in patients with LAT [38], though not all studies have supported this finding [106]. The antidepressant trazodone also increases the arousal threshold in patients with OSA and LAT [37] and has been shown to lower their AHI [107]. Based on these findings, some groups advocate for the use of these medications to treat OSA as part of a non-PAP therapeutic strategy [38, 108]. Presumably, patients with comorbid insomnia would benefit from the soporific effects of these medications.
Combined Insomnia and OSA Treatment in COMISA
Although therapy focusing on either insomnia or OSA in COMISA is frequently recommended [9••, 76, 109], several studies have examined combined or stepwise treatment approaches [26•, 56, 87, 89, 110, 111]. The majority of these studies utilized CBT-I in combination with OSA treatment in a small cohort [56, 87, 89] or case study [111] and found that combined treatment improved patient symptomatology more than individual therapy for insomnia or OSA. This was true whether treatment was performed in sequence [56, 87, 89, 110] or while simultaneously adapting to PAP [111]. One study featured a multidisciplinary approach beginning with PAP or CBT-I depending on presenting symptomatology and cross-referring to the alternate treatment if there were residual symptoms. Patients showed improvement on several self-reported sleep parameters and measures of daytime function and were satisfied with their therapy [110]. In another study, Gooneratne et al. analyzed the effect of the melatonin agonist ramelteon in patients with SDB and insomnia symptoms. In an older population starting PAP therapy, they found objective decreases in SOL with use of ramelteon compared to placebo [26•]. There were no significant differences in AHI or PAP adherence. For patients with severe disease or medical or psychiatric comorbidities, it is reasonable to consider a combined treatment approach to ensure therapy for either disorder is not delayed. This must be done with the knowledge that treatment of one disorder (insomnia or OSA) may negatively impact therapy for the other disorder [80].
There may be a role for non-PAP-based OSA therapies in COMISA patients. Guilleminault et al. treated patients with COMISA in a randomized crossover study with surgery for OSA followed by CBT-I or CBT-I preceding surgery. Participants in both groups experienced clinical improvement. However, the group that initially had surgery fared slightly better as some patients had resolution of their sleep disturbances with surgical treatment alone and declined CBT-I [87]. Oral appliance therapy is an established treatment for OSA and may also be considered in COMISA patients [112, 113]. In one study, the presence of insomnia symptoms limited the efficacy of oral appliance therapy [114]. Newer therapies for OSA, including hypoglossal nerve stimulation, can also be used in COMISA patients with or without CBT-I, though evidence is lacking in this population. Given the limited studies of non-PAP-based OSA therapies in COMISA, further studies are required to better address the many COMISA patients who are PAP intolerant.
The literature to date is not robust enough to make a definitive recommendation about combined therapy for COMISA. It is also not known whether combined therapy, if utilized, should be started concomitantly or in sequence. Several ongoing trials exploring combined approaches versus monotherapy for COMISA may answer these questions and help standardize future treatment [115,116,117,118].
Developing an Effective Diagnostic and Therapeutic Approach to COMISA
Recognition that different phenotypes of COMISA exist is important but not enough to effectively diagnose this disorder. A standardized diagnostic approach is needed. Our recommended multidisciplinary diagnostic and therapeutic approach emphasizes earlier diagnosis and treatment by integrating PSG findings, questionnaires, and clinical interviews. Patients with insomnia symptoms at presentation and no risk factors for OSA can begin treatment for insomnia. Insomnia patients who are refractory to treatment (CBT-I and/or pharmacotherapy) should be given an in-lab PSG to screen for OSA, noting that an HSAT would not be adequate in this population lacking a high pretest probability for OSA. COMISA is diagnosed in those insomnia patients with an AHI > 5/h. Patients with a high pretest probability of OSA and no insomnia symptoms or comorbidities can undergo HSAT. Patients with symptoms of OSA who have comorbid medical and behavioral medicine disorders should receive an in-lab PSG. The in-lab PSG variables can be especially helpful in diagnosing insomnia in patients who may be at higher risk for COMISA [17, 23•, 27, 50]. We recommend all OSA patients be screened for insomnia with an ISI. Based on previous research, we propose a threshold of 15 on the ISI score with at least 6 of those points coming from the first 3 (nocturnal) questions [53, 63]. COMISA is diagnosed in OSA patients when they meet the ISI threshold. Additionally, evaluating patients for comorbid disorders of hyperarousal is an important part of the evaluation and will help guide treatment. Patients may then be divided into one of three phenotypes as discussed above.
Therapy for COMISA should be driven by the specific patient phenotype (Fig. 1). For all COMISA patients, a healthy lifestyle and, if appropriate, weight loss are encouraged [119]. Additionally, in patients with the first phenotype (mild OSA and insomnia), CBT-I can be considered as monotherapy. In these patients, insomnia is presumed to be the driving force behind the patient’s symptomatology and is not the result of OSA manifestations, which would be unlikely to respond to CBT-I [92]. CBT-I is effective therapy for insomnia and may eliminate the indication for PAP in almost half of patients with mild SDB [91•]. While PAP therapy can be introduced concomitantly, it may serve to exacerbate the insomnia [80] and is often viewed as embarrassing, burdensome, and expensive [120]. Moreover, CBT-I techniques such as sleep restriction do not appear to worsen sleepiness in COMISA patients [90•]. If CBT-I does not ameliorate the patient’s symptoms, conventional PAP therapy, an oral appliance, or even pharmacotherapy (non-benzodiazepine receptor agonists) can be considered, particularly if LAT is present [37, 38, 108]. Although OSA is a risk factor for increased cardiovascular morbidity, delaying PAP therapy in patients with mild OSA for several weeks to determine if CBT-I is efficacious is not likely to result in significant morbidity [121,122,123].
Proposed treatment algorithm for COMISA based on phenotype. aFor insomnia in COMISA, we propose a threshold of 15 on the ISI score with at least 6 of those points coming from the first 3 (nocturnal) questions. bDisorders of hyperarousal include anxiety and PTSD. cOSA therapy may include PAP, oral appliance, or surgical techniques. dIn-lab titration performed to optimize PAP settings, try advanced modes of non-invasive ventilation, and determine if other underlying disorders exist. AHI apnea-hypopnea index, CBT-I cognitive behavioral therapy for insomnia, COMISA comorbid insomnia and obstructive sleep apnea, ISI insomnia severity index, OSA obstructive sleep apnea, PAP positive airway pressure
In patients with the second and third COMISA phenotypes, PAP therapy should be initiated with close follow-up. These phenotypes, which both feature moderate-severe OSA with insomnia symptoms, cannot be distinguished without assessment of treatment response. The second phenotype has clinical improvement of SDB and insomnia with initiation of PAP. In these patients, OSA is driving the insomnia and both tend to resolve with treatment. Often, these patients will complain of middle (maintenance) insomnia with frequent awakenings [52•], but this alone cannot reliably predict the phenotype as there is significant overlap in early, middle, or late insomnia complaints in patients with COMISA [10, 17]. Concomitant treatment of insomnia with either CBT-I or hypnotics in these patients’ results in unnecessary expenditure of valuable resources and, in the case of hypnotics, exposes patients to potentially harmful side effects [124, 125]. Patients with the third COMISA phenotype will have an inadequate clinical response to PAP. This may consist of PAP intolerance or persistent fatigue and insomnia symptoms despite adequate PAP usage. It may be difficult to distinguish whether OSA or insomnia is the dominant disease in the third phenotype but additional therapy with CBT-I or possibly hypnotics will be required to address the insomnia component and facilitate PAP tolerance. An in-lab PAP titration may also be considered to determine optimal PAP settings, try advanced modes of non-invasive ventilation [79, 83], and determine if other underlying disorders exist.
Although not a COMISA phenotype, disorders of hyperarousal (anxiety or PTSD) frequently accompany COMISA [27, 57, 60, 126] and a therapeutic strategy for these patients deserves attention. There is a paucity of treatment data in this population. In fact, these patients have been excluded from COMISA study samples [73]. However, given the overall disease severity, it is reasonable to use concomitant PAP and CBT-I or hypnotic therapy as initial treatment. This is particularly true when the OSA is moderate-severe as PAP alone is unlikely to address the degree of hyperarousal the patient is experiencing. If there is an inadequate clinical response to therapy, the addition of a hypnotic or performing an in-lab titration may be considered. More research on therapy in COMISA patients and this patient population in particular is needed to optimize treatment regimens.
Conclusion
COMISA is a prevalent but overlooked and understudied disorder in sleep medicine. Frequent arousals from either OSA or insomnia in patients with LAT may explain the underlying etiology of COMISA. Patients with COMISA have worse daytime symptoms as well as poorer subjective and objective sleep than those with either disorder alone. Further, patients with COMISA appear to have higher rates and severity of behavioral health disorders including anxiety, depression, and PTSD. Thus, appropriate recognition and treatment of both insomnia and OSA in a patient with COMISA is paramount. The best way to do this is unknown as a standardized approach does not exist due to a paucity of evidence. Based on the literature to date, we propose that any diagnostic approach in COMISA should be multidisciplinary and integrate PSG findings, questionnaires, and clinical interviews. All OSA patients should be screened for insomnia using the nocturnal questions from the ISI. Likewise, insomnia patients with OSA symptoms or those without OSA symptoms who are refractory to insomnia therapy should undergo a PSG to evaluate for occult SDB. Recognizing that different phenotypes of COMISA exist will help guide treatment that may include monotherapy or combined therapy, depending on the phenotype and presence or absence of associated behavioral health disorders. Further research is needed to validate and build upon this approach.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Guilleminault C, Eldridge FL, Dement WC. Insomnia with sleep apnea: a new syndrome. Science. 1973;181(4102):856–8.
• Krakow B, Melendrez D, Ferreira E, Clark J, Warner TD, Sisley B, et al. Prevalence of insomnia symptoms in patients with sleep-disordered breathing. Chest. 2001;120(6):1923–9. This was the first study to estimate the prevalence of insomnia symptoms in patients with sleep-disordered breathing.
Al-Jawder SE, Bahammam AS. Comorbid insomnia in sleep-related breathing disorders: an under-recognized association. Sleep Breath. 2012;16(2):295–304. https://doi.org/10.1007/s11325-011-0513-1.
Brock MS, Mysliwiec V. Comorbid insomnia and sleep apnea: a prevalent but overlooked disorder. Sleep Breath. 2018;22(1):1–3. https://doi.org/10.1007/s11325-018-1628-4.
Smith S, Sullivan K, Hopkins W, Douglas J. Frequency of insomnia report in patients with obstructive sleep apnoea hypopnea syndrome (OSAHS). Sleep Med. 2004;5(5):449–56. https://doi.org/10.1016/j.sleep.2004.03.005.
Krakow B, Melendrez D, Pedersen B, Johnston L, Hollifield M, Germain A, et al. Complex insomnia: insomnia and sleep-disordered breathing in a consecutive series of crime victims with nightmares and PTSD. Biol Psychiatry. 2001;49(11):948–53.
Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136–43. https://doi.org/10.1513/pats.200709-155MG.
American Academy of Sleep Medicine. The international classification of sleep disorders, diagnostic and coding manual. 3rd ed. Westchester: American Academy of Sleep Medicine; 2014.
•• Luyster FS, Buysse DJ, Strollo PJ Jr. Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6(2):196–204. This article examines early studies on the prevalence and treatment of co-occuring insomnia and OSA.
Ye L, Pien GW, Ratcliffe SJ, Bjornsdottir E, Arnardottir ES, Pack AI, et al. The different clinical faces of obstructive sleep apnoea: a cluster analysis. Eur Respir J. 2014;44(6):1600–7. https://doi.org/10.1183/09031936.00032314.
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of sleep medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479–504. https://doi.org/10.5664/jcsm.6506.
National Institutes of H. National Institutes of Health State of the Science Conference statement on Manifestations and Management of Chronic Insomnia in Adults, June 13-15, 2005. Sleep. 2005;28(9):1049–57.
Ford ES, Cunningham TJ, Giles WH, Croft JB. Trends in insomnia and excessive daytime sleepiness among U.S. adults from 2002 to 2012. Sleep Med. 2015;16(3):372–8. https://doi.org/10.1016/j.sleep.2014.12.008.
Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111.
Morin CM, Benca R. Chronic insomnia. Lancet. 2012;379(9821):1129–41. https://doi.org/10.1016/S0140-6736(11)60750-2.
Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4(5):487–504.
Mysliwiec V, Matsangas P, Baxter T, McGraw L, Bothwell NE, Roth BJ. Comorbid insomnia and obstructive sleep apnea in military personnel: correlation with polysomnographic variables. Mil Med. 2014;179(3):294–300. https://doi.org/10.7205/MILMED-D-13-00396.
Sanchez-Ortuno MM, Edinger JD. Cognitive-behavioral therapy for the management of insomnia comorbid with mental disorders. Curr Psychiatry Rep. 2012;14(5):519–28. https://doi.org/10.1007/s11920-012-0312-9.
Morgenthaler T, Kramer M, Alessi C, Friedman L, Boehlecke B, Brown T, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American academy of sleep medicine report. Sleep. 2006;29(11):1415–9.
Cronlein T, Geisler P, Langguth B, Eichhammer P, Jara C, Pieh C, et al. Polysomnography reveals unexpectedly high rates of organic sleep disorders in patients with prediagnosed primary insomnia. Sleep Breath. 2012;16(4):1097–103. https://doi.org/10.1007/s11325-011-0608-8.
Bailes S, Rizzo D, Baltzan M, Grad R, Pavilanis A, Creti L, et al. Manifestations of insomnia in sleep apnea: implications for screening and treatment. Behav Sleep Med. 2016;14(4):429–41. https://doi.org/10.1080/15402002.2015.1017098.
Kline CE, Irish LA, Buysse DJ, Kravitz HM, Okun ML, Owens JF, et al. Sleep hygiene behaviors among midlife women with insomnia or sleep-disordered breathing: the SWAN sleep study. J Women’s Health (Larchmt). 2014;23(11):894–903. https://doi.org/10.1089/jwh.2014.4730.
• Cho YW, Kim KT, Moon HJ, Korostyshevskiy VR, Motamedi GK, Yang KI. Comorbid insomnia with obstructive sleep apnea: clinical characteristics and risk factors. J Clin Sleep Med. 2018;14(3):409–17. https://doi.org/10.5664/jcsm.6988. This study reported objective findings of worse sleep in patients with COMISA and found a higher rate of depressive mood in COMISA patients compared to OSA alone.
Gooneratne NS, Gehrman PR, Nkwuo JE, Bellamy SL, Schutte-Rodin S, Dinges DF, et al. Consequences of comorbid insomnia symptoms and sleep-related breathing disorder in elderly subjects. Arch Intern Med. 2006;166(16):1732–8. https://doi.org/10.1001/archinte.166.16.1732.
Young T, Shahar E, Nieto FJ, Redline S, Newman AB, Gottlieb DJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the sleep heart health study. Arch Intern Med. 2002;162(8):893–900.
• Gooneratne NS, Gehrman P, Gurubhagavatula I, Al-Shehabi E, Marie E, Schwab R. Effectiveness of ramelteon for insomnia symptoms in older adults with obstructive sleep apnea: a randomized placebo-controlled pilot study. J Clin Sleep Med. 2010;6(6):572–80. This study demonstrated that hypnotic therapy can improve obvjective sleep onset latency in older adults starting PAP for OSA.
Mysliwiec V, Gill J, Lee H, Baxter T, Pierce R, Barr TL, et al. Sleep disorders in US military personnel: a high rate of comorbid insomnia and obstructive sleep apnea. Chest. 2013;144(2):549–57. https://doi.org/10.1378/chest.13-0088.
Wallace DM, Vargas SS, Schwartz SJ, Aloia MS, Shafazand S. Determinants of continuous positive airway pressure adherence in a sleep clinic cohort of South Florida Hispanic veterans. Sleep Breath. 2013;17(1):351–63. https://doi.org/10.1007/s11325-012-0702-6.
Krakow B, Germain A, Tandberg D, Koss M, Schrader R, Hollifield M, et al. Sleep breathing and sleep movement disorders masquerading as insomnia in sexual-assault survivors. Compr Psychiatry. 2000;41(1):49–56.
Jansson-Frojmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008;64(4):443–9. https://doi.org/10.1016/j.jpsychores.2007.10.016.
Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40(8):700–8. https://doi.org/10.1016/j.jpsychires.2006.07.008.
Ohayon MM, Roth T. Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res. 2003;37(1):9–15.
McLay RN, Klam WP, Volkert SL. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from military deployments. Mil Med. 2010;175(10):759–62.
Colvonen PJ, Masino T, Drummond SP, Myers US, Angkaw AC, Norman SB. Obstructive sleep apnea and posttraumatic stress disorder among OEF/OIF/OND veterans. J Clin Sleep Med. 2015;11(5):513–8. https://doi.org/10.5664/jcsm.4692.
Orr JE, Smales C, Alexander TH, Stepnowsky C, Pillar G, Malhotra A, et al. Treatment of OSA with CPAP is associated with improvement in PTSD symptoms among veterans. J Clin Sleep Med. 2017;13(1):57–63. https://doi.org/10.5664/jcsm.6388.
• Eckert DJ, White DP, Jordan AS, Malhotra A, Wellman A. Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am J Respir Crit Care Med. 2013;188(8):996–1004. https://doi.org/10.1164/rccm.201303-0448OC. This study found that abnormalities in nonanatomic traits (loop gain, arousal threshold) are present in most patients with OSA.
Eckert DJ, Malhotra A, Wellman A, White DP. Trazodone increases the respiratory arousal threshold in patients with obstructive sleep apnea and a low arousal threshold. Sleep. 2014;37(4):811–9. https://doi.org/10.5665/sleep.3596.
Eckert DJ, Owens RL, Kehlmann GB, Wellman A, Rahangdale S, Yim-Yeh S, et al. Eszopiclone increases the respiratory arousal threshold and lowers the apnoea/hypopnoea index in obstructive sleep apnoea patients with a low arousal threshold. Clin Sci (Lond). 2011;120(12):505–14. https://doi.org/10.1042/CS20100588.
Younes M. Role of arousals in the pathogenesis of obstructive sleep apnea. Am J Respir Crit Care Med. 2004;169(5):623–33. https://doi.org/10.1164/rccm.200307-1023OC.
Eckert DJ, Jordan AS, Merchia P, Malhotra A. Central sleep apnea: pathophysiology and treatment. Chest. 2007;131(2):595–607. https://doi.org/10.1378/chest.06.2287.
Eckert DJ, Younes MK. Arousal from sleep: implications for obstructive sleep apnea pathogenesis and treatment. J Appl Physiol (1985). 2014;116(3):302–13. https://doi.org/10.1152/japplphysiol.00649.2013.
Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, et al. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14(1):19–31. https://doi.org/10.1016/j.smrv.2009.04.002.
Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Med Rev. 2010;14(1):9–15. https://doi.org/10.1016/j.smrv.2009.05.002.
Bianchi MT, Williams KL, McKinney S, Ellenbogen JM. The subjective-objective mismatch in sleep perception among those with insomnia and sleep apnea. J Sleep Res. 2013;22(5):557–68. https://doi.org/10.1111/jsr.12046.
Hayley AC, Williams LJ, Venugopal K, Kennedy GA, Berk M, Pasco JA. The relationships between insomnia, sleep apnoea and depression: findings from the American National Health and Nutrition Examination Survey, 2005-2008. Aust N Z J Psychiatry. 2015;49(2):156–70. https://doi.org/10.1177/0004867414546700.
Wallace DM, Wohlgemuth WK. Does race-ethnicity moderate the relationship between CPAP adherence and functional outcomes of sleep in US veterans with obstructive sleep apnea syndrome? J Clin Sleep Med. 2014;10(10):1083–91. https://doi.org/10.5664/jcsm.4106.
Bjornsdottir E, Janson C, Gislason T, Sigurdsson JF, Pack AI, Gehrman P, et al. Insomnia in untreated sleep apnea patients compared to controls. J Sleep Res. 2012;21(2):131–8. https://doi.org/10.1111/j.1365-2869.2011.00972.x.
Tasbakan MS, Gunduz C, Pirildar S, Basoglu OK. Quality of life in obstructive sleep apnea is related to female gender and comorbid insomnia. Sleep Breath. 2018; https://doi.org/10.1007/s11325-018-1621-y.
Lee MH, Lee SA, Lee GH, Ryu HS, Chung S, Chung YS, et al. Gender differences in the effect of comorbid insomnia symptom on depression, anxiety, fatigue, and daytime sleepiness in patients with obstructive sleep apnea. Sleep Breath. 2014;18(1):111–7. https://doi.org/10.1007/s11325-013-0856-x.
Li Z, Li Y, Yang L, Li T, Lei F, Vgontzas AN, et al. Characterization of obstructive sleep apnea in patients with insomnia across gender and age. Sleep Breath. 2015;19(2):723–7. https://doi.org/10.1007/s11325-015-1121-2.
Wickwire EM, Smith MT, Birnbaum S, Collop NA. Sleep maintenance insomnia complaints predict poor CPAP adherence: a clinical case series. Sleep Med. 2010;11(8):772–6. https://doi.org/10.1016/j.sleep.2010.03.012.
• Bjornsdottir E, Janson C, Sigurdsson JF, Gehrman P, Perlis M, Juliusson S, et al. Symptoms of insomnia among patients with obstructive sleep apnea before and after two years of positive airway pressure treatment. Sleep. 2013;36(12):1901–9. https://doi.org/10.5665/sleep.3226. This study determined baseline predictors of insomnia symptoms (frequent awakening complaints) that would improve following treatment with PAP.
Wallace DM, Sawyer AM, Shafazand S. Comorbid insomnia symptoms predict lower 6-month adherence to CPAP in US veterans with obstructive sleep apnea. Sleep Breath. 2018;22(1):5–15. https://doi.org/10.1007/s11325-017-1605-3.
Pieh C, Bach M, Popp R, Jara C, Cronlein T, Hajak G, et al. Insomnia symptoms influence CPAP compliance. Sleep Breath. 2013;17(1):99–104. https://doi.org/10.1007/s11325-012-0655-9.
Lam AS, Collop NA, Bliwise DL, Dedhia RC. Validated measures of insomnia, function, sleepiness, and nasal obstruction in a CPAP alternatives clinic population. J Clin Sleep Med. 2017;13(8):949–57. https://doi.org/10.5664/jcsm.6692.
Krakow B, Melendrez D, Lee SA, Warner TD, Clark JO, Sklar D. Refractory insomnia and sleep-disordered breathing: a pilot study. Sleep Breath. 2004;8(1):15–29. https://doi.org/10.1007/s11325-004-0015-5.
El-Solh AA, Adamo D, Kufel T. Comorbid insomnia and sleep apnea in veterans with post-traumatic stress disorder. Sleep Breath. 2018;22(1):23–31. https://doi.org/10.1007/s11325-017-1618-y.
Krell SB, Kapur VK. Insomnia complaints in patients evaluated for obstructive sleep apnea. Sleep Breath. 2005;9(3):104–10. https://doi.org/10.1007/s11325-005-0026-x.
Lang CJ, Appleton SL, Vakulin A, McEvoy RD, Wittert GA, Martin SA, et al. Co-morbid OSA and insomnia increases depression prevalence and severity in men. Respirology. 2017;22(7):1407–15. https://doi.org/10.1111/resp.13064.
Yang CM, Liao YS, Lin CM, Chou SL, Wang EN. Psychological and behavioral factors in patients with comorbid obstructive sleep apnea and insomnia. J Psychosom Res. 2011;70(4):355–61. https://doi.org/10.1016/j.jpsychores.2010.12.005.
Glidewell RN, Renn BN, Roby E, Orr WC. Predictors and patterns of insomnia symptoms in OSA before and after PAP therapy. Sleep Med. 2014;15(8):899–905. https://doi.org/10.1016/j.sleep.2014.05.001.
Savard MH, Savard J, Simard S, Ivers H. Empirical validation of the Insomnia Severity Index in cancer patients. Psychooncology. 2005;14(6):429–41. https://doi.org/10.1002/pon.860.
Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307.
Fung CH, Martin JL, Dzierzewski JM, Jouldjian S, Josephson K, Park M, et al. Prevalence and symptoms of occult sleep disordered breathing among older veterans with insomnia. J Clin Sleep Med. 2013;9(11):1173–8. https://doi.org/10.5664/jcsm.3162.
Krakow B, Ulibarri VA. Prevalence of sleep breathing complaints reported by treatment-seeking chronic insomnia disorder patients on presentation to a sleep medical center: a preliminary report. Sleep Breath. 2013;17(1):317–22. https://doi.org/10.1007/s11325-012-0694-2.
Krakow B, Romero E, Ulibarri VA, Kikta S. Prospective assessment of nocturnal awakenings in a case series of treatment-seeking chronic insomnia patients: a pilot study of subjective and objective causes. Sleep. 2012;35(12):1685–92. https://doi.org/10.5665/sleep.2244.
Edwards BA, Eckert DJ, McSharry DG, Sands SA, Desai A, Kehlmann G, et al. Clinical predictors of the respiratory arousal threshold in patients with obstructive sleep apnea. Am J Respir Crit Care Med. 2014;190(11):1293–300. https://doi.org/10.1164/rccm.201404-0718OC.
Fernandez-Mendoza J, Vela-Bueno A, Vgontzas AN, Ramos-Platon MJ, Olavarrieta-Bernardino S, Bixler EO, et al. Cognitive-emotional hyperarousal as a premorbid characteristic of individuals vulnerable to insomnia. Psychosom Med. 2010;72(4):397–403. https://doi.org/10.1097/PSY.0b013e3181d75319.
Varkevisser M, Van Dongen HP, Kerkhof GA. Physiologic indexes in chronic insomnia during a constant routine: evidence for general hyperarousal? Sleep. 2005;28(12):1588–96.
Joiner TE Jr, Steer RA, Beck AT, Schmidt NB, Rudd MD, Catanzaro SJ. Physiological hyperarousal: construct validity of a central aspect of the tripartite model of depression and anxiety. J Abnorm Psychol. 1999;108(2):290–8.
Woodward SH, Murburg MM, Bliwise DL. PTSD-related hyperarousal assessed during sleep. Physiol Behav. 2000;70(1–2):197–203.
Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263–76.
Mendes MS, dos Santos JM. Insomnia as an expression of obstructive sleep apnea syndrome--the effect of treatment with nocturnal ventilatory support. Rev Port Pneumol (2006). 2015;21(4):203–8. https://doi.org/10.1016/j.rppnen.2014.11.002.
Crawford MR, Chirinos DA, Iurcotta T, Edinger JD, Wyatt JK, Manber R, et al. Characterization of patients who present with insomnia: is there room for a symptom cluster-based approach? J Clin Sleep Med. 2017;13(7):911–21. https://doi.org/10.5664/jcsm.6666.
•• Sweetman AM, Lack LC, Catcheside PG, Antic NA, Chai-Coetzer CL, Smith SS, et al. Developing a successful treatment for co-morbid insomnia and sleep apnoea. Sleep Med Rev. 2017;33:28–38. https://doi.org/10.1016/j.smrv.2016.04.004. This article explores the theoretical mechanistic relationships between comorbid insomnia and OSA and discusses previous treatment attempts.
Lichstein KL. Secondary insomnia: a myth dismissed. Sleep Med Rev. 2006;10(1):3–5. https://doi.org/10.1016/j.smrv.2005.10.001.
Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173–8. https://doi.org/10.1513/pats.200708-119MG.
Smith S, Dunn N, Douglas J, Jorgensen G. Sleep onsent insomnia is associated with reduced adherence to CPAP therapy. Sleep Biol Rythms. 2009;7:A74.
Krakow B, McIver ND, Ulibarri VA, Nadorff MR. Retrospective, nonrandomized controlled study on autoadjusting, dual-pressure positive airway pressure therapy for a consecutive series of complex insomnia disorder patients. Nat Sci Sleep. 2017;9:81–95. https://doi.org/10.2147/NSS.S120048.
Cherniack NS. Sleep apnea and insomnia: sleep apnea plus or sleep apnea minus. Respiration. 2005;72(5):458–9. https://doi.org/10.1159/000087667.
Krakow B, Lowry C, Germain A, Gaddy L, Hollifield M, Koss M, et al. A retrospective study on improvements in nightmares and post-traumatic stress disorder following treatment for co-morbid sleep-disordered breathing. J Psychosom Res. 2000;49(5):291–8.
Nguyen XL, Rakotonanahary D, Chaskalovic J, Fleury B. Insomnia related to sleep apnoea: effect of long-term auto-adjusting positive airway pressure treatment. Eur Respir J. 2013;41(3):593–600. https://doi.org/10.1183/09031936.00080011.
Krakow BUV, Romero E, Rhomas RJ, McIver N. Adaptive servo-ventilation therapy in a case series of patients with co-morbid insomnia and sleep apnea. J Sleep Disord Treat Care. 2013;2(1) https://doi.org/10.4172/2325-9639.1000107.
Trauer JM, Qian MY, Doyle JS, Rajaratnam SM, Cunnington D. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med. 2015;163(3):191–204. https://doi.org/10.7326/M14-2841.
Morin CM, Hauri PJ, Espie CA, Spielman AJ, Buysse DJ, Bootzin RR. Nonpharmacologic treatment of chronic insomnia. An American Academy of Sleep Medicine review. Sleep. 1999;22(8):1134–56.
Mitchell MD, Gehrman P, Perlis M, Umscheid CA. Comparative effectiveness of cognitive behavioral therapy for insomnia: a systematic review. BMC Fam Pract. 2012;13:40. https://doi.org/10.1186/1471-2296-13-40.
Guilleminault C, Davis K, Huynh NT. Prospective randomized study of patients with insomnia and mild sleep disordered breathing. Sleep. 2008;31(11):1527–33.
Guilleminault C, Palombini L, Poyares D, Chowdhuri S. Chronic insomnia, premenopausal women and sleep disordered breathing: part 2. Comparison of nondrug treatment trials in normal breathing and UARS post menopausal women complaining of chronic insomnia. J Psychosom Res. 2002;53(1):617–23.
Melendrez DC, Krakow BJ, Johnston L, Sisley B, Warner TD. A prospective study on the treatment of “complex insomnia”-insomnia plus sleep disordered breathing in a small series of crime victims with PTSD. Sleep. 2001;24:A120–A120.
• Sweetman A, Lack L, Lambert S, Gradisar M, Harris J. Does comorbid obstructive sleep apnea impair the effectiveness of cognitive and behavioral therapy for insomnia? Sleep Med. 2017;39:38–46. https://doi.org/10.1016/j.sleep.2017.09.003. This study determined that CBT-I is effective at treating insomnia in the presence of comorbid OSA
• Fung CH, Martin JL, Josephson K, Fiorentino L, Dzierzewski JM, Jouldjian S, et al. Efficacy of cognitive behavioral therapy for insomnia in older adults with occult sleep-disordered breathing. Psychosom Med. 2016;78(5):629–39. https://doi.org/10.1097/PSY.0000000000000314. This study determined that the effect of CBT-I is similar for older veterans with and without untreated mild OSA.
Lichstein KLMC, Wilson NM. Secondary insomnia: diagnostic issues, cognitive-behavioral treatment, and future directions. In: Perlis M, Lichstein KL, editors. Treating sleep disorders: Principles and practice of behavioral sleep medicine; 2003. p. 286–304.
An H, Chung S. A case of obstructive sleep apnea syndrome presenting as paradoxical insomnia. Psychiatry Investig. 2010;7(1):75–8. https://doi.org/10.4306/pi.2010.7.1.75.
Lack L, Sweetman A. Diagnosis and treatment of insomnia comorbid with obstructive sleep apnea. Sleep Med Clin. 2016;11(3):379–88. https://doi.org/10.1016/j.jsmc.2016.05.006.
Glidewell RN, Moorcroft WH, Lee-Chiong T Jr. Comorbid insomnia: reciprocal relationships and medication management. Sleep Med Clin. 2010;5(4):627–46. https://doi.org/10.1016/j.jsmc.2010.08.012.
Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Clinical Guidelines Committee of the American College of P. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125–33. https://doi.org/10.7326/M15-2175.
Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Meta-analysis of benzodiazepine use in the treatment of insomnia. CMAJ. 2000;162(2):225–33.
Riemann D, Perlis ML. The treatments of chronic insomnia: a review of benzodiazepine receptor agonists and psychological and behavioral therapies. Sleep Med Rev. 2009;13(3):205–14. https://doi.org/10.1016/j.smrv.2008.06.001.
Sloan EPSC. Hypnotics should never be used in patients with sleep apnea. J Psychosom Res. 1992;37:59–65.
Berry RB, Kouchi K, Bower J, Prosise G, Light RW. Triazolam in patients with obstructive sleep apnea. Am J Respir Crit Care Med. 1995;151(2 Pt 1):450–4. https://doi.org/10.1164/ajrccm.151.2.7842205.
Dolly FR, Block AJ. Effect of flurazepam on sleep-disordered breathing and nocturnal oxygen desaturation in asymptomatic subjects. Am J Med. 1982;73(2):239–43.
Camacho ME, Morin CM. The effect of temazepam on respiration in elderly insomniacs with mild sleep apnea. Sleep. 1995;18(8):644–5.
Wang PS, Bohn RL, Glynn RJ, Mogun H, Avorn J. Hazardous benzodiazepine regimens in the elderly: effects of half-life, dosage, and duration on risk of hip fracture. Am J Psychiatry. 2001;158(6):892–8. https://doi.org/10.1176/appi.ajp.158.6.892.
Lettieri CJ, Shah AA, Holley AB, Kelly WF, Chang AS, Roop SA, et al. Effects of a short course of eszopiclone on continuous positive airway pressure adherence: a randomized trial. Ann Intern Med. 2009;151(10):696–702. https://doi.org/10.7326/0003-4819-151-10-200911170-00006.
Berry RB, Patel PB. Effect of zolpidem on the efficacy of continuous positive airway pressure as treatment for obstructive sleep apnea. Sleep. 2006;29(8):1052–6.
Smith PR, Sheikh KL, Costan-Toth C, Forsthoefel D, Bridges E, Andrada TF, et al. Eszopiclone and zolpidem do not affect the prevalence of the low arousal threshold phenotype. J Clin Sleep Med. 2017;13(1):115–9. https://doi.org/10.5664/jcsm.6402.
Smales ET, Edwards BA, Deyoung PN, McSharry DG, Wellman A, Velasquez A, et al. Trazodone effects on obstructive sleep apnea and non-REM arousal threshold. Ann Am Thorac Soc. 2015;12(5):758–64. https://doi.org/10.1513/AnnalsATS.201408-399OC.
Owens RL, Edwards BA, Eckert DJ, Jordan AS, Sands SA, Malhotra A, et al. An integrative model of physiological traits can be used to predict obstructive sleep apnea and response to non positive airway pressure therapy. Sleep. 2015;38(6):961–70. https://doi.org/10.5665/sleep.4750.
Ong JC, Crisostomo MI. The more the merrier? Working towards multidisciplinary management of obstructive sleep apnea and comorbid insomnia. J Clin Psychol. 2013;69(10):1066–77. https://doi.org/10.1002/jclp.21958.
Ong JC, Crawford MR, Kong A, Park M, Cvengros JA, Crisostomo MI, et al. Management of obstructive sleep apnea and comorbid insomnia: a mixed-methods evaluation. Behav Sleep Med. 2017;15(3):180–97. https://doi.org/10.1080/15402002.2015.1087000.
Wickwire EM Jr, Schumacher J, Richert AC Jr, Sinan Baran A, Roffwarg HP. Combined insomnia and poor CPAP compliance: a case study and discussion. Clin Case Stud. 2008;7(4):267–86.
Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med. 2015;11(7):773–827.
Wickwire EM, Collop NA. Insomnia and sleep-related breathing disorders. Chest. 2010;137(6):1449–63.
Machado MA, de Carvalho LB, Juliano ML, Taga M, Do Prado LB, do Prado GF. Clinical co-morbidities in obstructive sleep apnea syndrome treated with mandibular repositioning appliance. Respir Med. 2006;100(6):988–95.
Ong JC. Multidisciplinary approach to the treatment of insomnia and comorbid sleep apnea. Clinical Trials Identifier: NCT01785303. Northwestern University; 2013.
Goonerante NS. Understanding the sleep apnea/insomnia interaction: a CPAP/sham-CPAP trial. Clinical Trials Identifier: NCT01824472. University of Pennsylvania: National Institutes of Health; 2012.
Catcheside PG, Douglas JA. Treating insomnia co-morbid with obstructive sleep apnoea: a randomized controlled clinical effectiveness trial. NHMRC identifier: 1049591. Flinders University of South Australia: National Health and Medical Research Council.
Crawford MR, Turner AD, Wyatt JK, Fogg LF, Ong JC. Evaluating the treatment of obstructive sleep apnea comorbid with insomnia disorder using an incomplete factorial design. Contemp Clin Trials. 2016;47:146–52. https://doi.org/10.1016/j.cct.2015.12.017.
Tuomilehto HP, Seppa JM, Partinen MM, Peltonen M, Gylling H, Tuomilehto JO, et al. Lifestyle intervention with weight reduction: first-line treatment in mild obstructive sleep apnea. Am J Respir Crit Care Med. 2009;179(4):320–7. https://doi.org/10.1164/rccm.200805-669OC.
Almeida FR, Henrich N, Marra C, Lynd LD, Lowe AA, Tsuda H, et al. Patient preferences and experiences of CPAP and oral appliances for the treatment of obstructive sleep apnea: a qualitative analysis. Sleep Breath. 2013;17(2):659–66. https://doi.org/10.1007/s11325-012-0739-6.
Guo J, Sun Y, Xue LJ, Huang ZY, Wang YS, Zhang L, et al. Effect of CPAP therapy on cardiovascular events and mortality in patients with obstructive sleep apnea: a meta-analysis. Sleep Breath. 2016;20(3):965–74. https://doi.org/10.1007/s11325-016-1319-y.
Barbe F, Duran-Cantolla J, Sanchez-de-la-Torre M, Martinez-Alonso M, Carmona C, Barcelo A, et al. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;307(20):2161–8. https://doi.org/10.1001/jama.2012.4366.
Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–53. https://doi.org/10.1016/S0140-6736(05)71141-7.
Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017;13(2):307–49. https://doi.org/10.5664/jcsm.6470.
Buscemi N, Vandermeer B, Friesen C, Bialy L, Tubman M, Ospina M, et al. The efficacy and safety of drug treatments for chronic insomnia in adults: a meta-analysis of RCTs. J Gen Intern Med. 2007;22(9):1335–50. https://doi.org/10.1007/s11606-007-0251-z.
Rezaeitalab F, Mokhber N, Ravanshad Y, Saberi S, Rezaeetalab F. Different polysomnographic patterns in military veterans with obstructive sleep apnea in those with and without post-traumatic stress disorder. Sleep Breath. 2018;22(1):17–22. https://doi.org/10.1007/s11325-017-1596-0.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Matthew Brock, Shannon Foster, Vida Motamedi, and Vincent Mysliwiec declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Sleep and Otolaryngology
All work was performed at Wilford Hall Ambulatory Surgical Center, JBSA-Lackland, TX 78236.
The opinions and assertions in this manuscript are those of the authors and do not represent those of the Department of the Air Force, Department of the Army, Department of Defense, or the USA government.
Rights and permissions
About this article
Cite this article
Brock, M.S., Foster, S.N., Motamedi, V. et al. COMISA (Comorbid Insomnia and Sleep Apnea): a Practical Approach. Curr Sleep Medicine Rep 4, 255–267 (2018). https://doi.org/10.1007/s40675-018-0127-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40675-018-0127-2