Abstract
Objectives
The aim of this study is to better understand patients’ perspectives and preferences about treatment with continuous positive airway pressure (CPAP) and oral appliance (OA) devices for obstructive sleep apnea.
Methods
The current study used qualitative analysis of four focus group sessions with current CPAP and OA users. Twenty-two participants with OSA who currently use either CPAP or OA participated in the sessions at the University of British Columbia.
Results
Five topics from the focus group sessions were descriptively analyzed using NVivo software: goals and expectations of treatment, benefits of treatment for bed partners, side effects and inconveniences of CPAP, side effects and inconveniences of OA, and factors impacting treatment choice. In order of most to least frequently mentioned, patients expressed six expectations of treatment: improved health, apnea elimination, improved sleep, reduced fatigue, reduced snoring, and bed-partner benefits. The most to least mentioned factors impacting treatment choice were device effectiveness, transportability, embarrassment, and cost.
Conclusions
This qualitative study showed that many factors impact patients’ experience with their treatment device and that their treatment needs are not only physical but also relate to their lifestyle. This preliminary study provides treatment characteristics and attributes necessary to develop a quantitative questionnaire study, to assist in the selection of therapy, weighing the relative importance of patient and OSA treatment characteristics on treatment preference and adherence. Matching therapy to patient preferences may help identify the most appropriate treatment, and this may achieve greater likelihood of adherence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is the most common respiratory sleep disorder, and has important health and safety consequences including daytime sleepiness, increased risk of motor vehicle crashes, diminished neurocognitive function, hypertension, cardiovascular diseases, and death [1–5]. Appropriate treatment ameliorates many of these adverse consequences [5], stressing the importance of treatment adherence.
The two most common therapies used to treat OSA are (1) continuous positive airway pressure (CPAP), which consists of a device attached to the patient that has a plastic tube that blows compressed air into the airway during sleep, and (2) oral appliances (OA), which are dental splints used to keep the mandible in an advanced and closed position during sleep. While both therapies improve airway patency and reduce upper airway collapse during sleep [6], they differ in cost (CPAP usually is more expensive), efficacy (CPAP is usually more efficacious than OA in acute situations), adherence, and side effects [7].
There are many factors that affect adherence to treatment including treatment method, social and economic factors, the healthcare system/team, characteristics of the disease, patient-related factors, and the patient’s partner and family. Poor patient adherence is related to poor health outcomes and increased health care costs [8]. In order to improve adherence, a patient-centered treatment approach is crucial.
Acquiring insight into the patient’s perspectives about attributes of a potential treatment modality (e.g., comfort of the device, efficacy, side effects) can provide vital information to practitioners to help inform the choice of optimal treatment. Medical treatment plans developed with patient participation usually result in improved treatment adherence and a higher quality of life [9]. OSA patients’ perspectives are therefore important to inform the development of an evidence-based management model that is sensitive to patient preferences for treatment and would contribute to contemporary self-management discourse in OSA.
A patient-tailored therapy requires patient involvement in planning and decision-making in their treatment. Patients may become frustrated if their preferences are not taken into account [10]. Independent of patient preferences and expectations, practitioners normally select CPAP as the first choice in treatment. However, adherence to CPAP may be suboptimal. An improved understanding of patient preferences and the factors that influence decision-making about OSA devices may improve adherence. Also, a better understanding of how a patient’s lifestyle fits with different treatments and patient concerns and beliefs about treatment could aid in selecting a long-term therapy that is well suited to the individual patient. Due to the lack of studies related to patient preferences in the OSA field, we believe there is inadequate consideration of patients’ preferences in OSA management.
To better understand the experience of using CPAP and OA devices and the factors that influence patients’ choice of treatments, the current study used qualitative analysis of focus groups conducted with OSA patients who currently use one of the devices. This study was designed to evoke personal OSA and treatment experiences as means to “put flesh on the bones” of our understanding about these issues and complement existing knowledge about CPAP and OA. Focus groups are an effective way to gain insight about patients’ perspectives and experiences because the groups provide a forum in which targeted populations have the opportunity to provide in-depth opinions about a specific topic. They are also an efficient method for obtaining information from participants who share important characteristics [11, 12]. Focus groups play an important role in hypothesis-generating and questionnaire development. The first step in the development of discrete choice experiments is the identification of treatment characteristics and attributes. Focus group results have been extensively used to identify such attributes in chronic disease therapies such as diabetes and obesity [13, 14]. Thus, the primary objective of focus groups is to describe characteristic to be used in questionnaires which can quantitatively measure patient preferences for different attributes of OSA treatment.
The interaction between the participants may lead to the emergence of a wider range of ideas and opinions than would normally be seen in a one to one interview. The primary purpose of this study was to understand the experience of CPAP and OA users, as well as the factors that influence a patient’s choice of treatments.
Methods
Focus groups
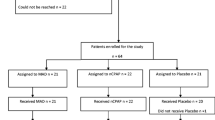
We conducted four focus groups between June and October 2009 with OSA patients who used either an OA or CPAP. Patients who self-reported as currently using an oral appliance or a CPAP on most of the nights were invited to the study. A member of our research team with expertise in OSA (FA) attended all of the focus groups. Sessions lasted between 45 and 90 min. There was one group of all CPAP users (n = 3), one of all OA users (n = 3), and two with a mix of CPAP and OA users (n = 15). The number of focus groups was determined by the principle of “saturation,” which corresponds to when the information gathered during the discussions became repetitive. Participants in all groups may have previously used the alternative treatment and these participants were able to comment on both treatments. Additionally, one interview was conducted with a CPAP user and the same questions were posed in the interview as in the focus groups (total of 22 patients in the study, in five groups). The sessions were audio recorded and transcribed. The interview and focus groups were analyzed together and are referred to collectively as the focus groups.
During the focus group sessions, the moderator posed questions and directed conversation to address topics including (1) the expected benefits of the treatment, (2) side effects and other negative aspects of using the treatment, (3) benefits of treatment for bed partners, and (4) the factors that impact the patient’s choice of treatment. The full set of questions can be found in the focus group guide in the Appendix. Demographic information was collected about the participants’ age, relationship status, occupation, extended health coverage, and whether or not they had a bed partner.
Participant recruitment
Participants were recruited from the University of British Columbia Sleep Apnea Clinic. To participate in the study, participants had to be at least 19 years old, a patient at the UBC Sleep Clinic, currently being treated for OSA, and able to understand English and provide informed consent.
Analysis
Transcripts from the focus groups were imported into NVivo 8 (QSR International), a qualitative research computer program, for thematic coding and analysis. The focus groups were qualitatively described [15], using broad thematic codes developed a priori from the focus group questions and subthemes that were developed based on the content of the focus groups. A trained coder applied the codes to the transcripts. All coding was reviewed by a senior qualitative scientist. Analyses were performed to identify common themes, and exemplary quotes were selected that best characterized the opinions and experiences reflected within each theme.
Ethics approval was obtained from Vancouver Coastal Health and UBC Behavioural Research Ethics Boards; all patients provided written informed consent prior to enrolling in the study.
Results
Twenty-two patients with OSA participated in five focus groups. Participants had a mean age of approximately 60 years and the majority had extended health coverage, were married or living with someone, and had a bed partner (Table 1). The specific occupations provided by participants were categorized based on the US Department of Labor standard occupational classification system [16]. On average, participants using OA had a higher baseline sleepiness score (Epworth Sleepiness Scale, ESS), a lower baseline apnea hypopnea index (AHI) score, and more years using their current treatment device compared to participants using CPAP (Table 2). All 13 patients who were on oral appliance therapy had been previously prescribed and used CPAP. One patient in the CPAP group had used an oral appliance for 5.4 years prior to CPAP use.
Five main themes emerged from the focus group discussions, three of which had associated subthemes (Table 3). Subthemes are listed by the number of focus groups in which the subtheme was mentioned. Additionally, subthemes are also ordered by the number of times that the subtheme was mentioned during the discussions; these numbers are not included because they are less concise owing to the fact that an individual may have commented on a subtheme multiple times and potentially biasing the relative importance of a subtheme as measured by the number of references. Each theme is described below, along with exemplary statements from focus group participants. The statements are direct quotations; when necessary, words have been inserted for clarification and these are indicated with [ ] around the additions.
Expected benefits
Participants expressed six benefits that they hoped to achieve by using a sleep apnea treatment including, from most to least frequently mentioned, improved health (especially prevention of heart disease and strokes), eliminated/reduced apnea, uninterrupted/improved sleep, reduced daytime fatigue, terminated/reduced snoring, and benefits to bed partner.
Side effects/inconveniences of CPAP and OA
Despite participants’ overall satisfaction with the CPAP and OA, a substantial number of side effects and other negative aspects of the treatments were indicated in the focus groups. These negative aspects of using the devices are summarized in Table 2. The top five complaints for each device are described in further detail below.
Five most frequently mentioned negative aspects of CPAP
The primary criticism of CPAP is the discomfort associated with its use. Generally, use of the device was described as uncomfortable. Common complaints about CPAP were that it made the users too hot, left marks on the face, limited the users’ mobility and prohibited them from sleeping on their side or stomach, and leaked air which then blew into the users’ eyes.
“I’ve been using the CPAP mask for—I think it’s about a year but I’m not positive. I can’t stand the thing. I find that it blows all up in around my eyes throughout the night and find my range of motion from my neck is—I’m often stiff in my neck because it holds—makes it so stiff. I do use it.”
The CPAP machine was described as noisy and there were complaints that the excessive noise disturbed both the users and bed partners.
The poor fit of the CPAP mask contributed to the general discomfort of using the device. Numerous participants mentioned that the mask did not fit properly and, in addition to discomfort, this resulted in leaking air and the need to readjust the mask during the night—both of which disrupted the users’ sleep.
“So I find that I spend a lot of my night doing these little adjustments throughout the evening. So it’s impacting my sleep. I mean, I’m able then to fall back asleep quite quickly, but, you know, I hear that annoying escape of the air and then have to adjust and so it’s—I’m not getting a continuous sleep.”
Several CPAP users experienced feelings of claustrophobia from the mask. One participant described panic attacks associated with wearing the mask:
“[With CPAP] I had tremendous panic attacks. Well, they found out in a hurry, because they put it on here and I just—it was horrid. Like, I just ripped it off and I just was panicking and, like, it was awful.”
Users of CPAP devices described cleaning the CPAP as a hassle. The main annoyance of the cleaning process, as voiced by the participants, was the need to use filtered water. Some participants had tried using unfiltered water despite the instructions to the contrary, and found that the device developed a build up of sediments. A CPAP user described the cleaning process, saying:
“There is a lot of small fussy stuff associated with the CPAP machine. Filling the reservoir and washing it, which I don’t do every night, but fairly often. It’s a chore like flossing, I mean, you know, various other things.”
Five most frequently mentioned negative aspects of OA
The primary complaint about the OA is the impact it has on the user’s bite. Participants described the consequences of their shifted bite, including frequently biting their lips and cheeks and chipping their teeth. Others indicated that their dentists had noticed a problem with their shifting bite.
OA users described pain with the device, but the pain was minimal and occurred when the device was first used or when it was used infrequently. Participants identified this as an adjustment period, with the discomfort subsiding after getting used to the device.
“If you’re not wearing it all the time, certainly the first night that you put it in, your teeth are sore in the morning. And I find I don’t sleep as well, I’m a bit restless that first night, just because of the—it’s a bit uncomfortable if you have to adjust to it being in place.”
No one talked about on-going pain with the device when used regularly.
Users were disappointed in the durability of the device and the frequency with which the device needed to be repaired or replaced. Participants’ estimates of the life of an OA ranged from 1.5 to 3 years. Associated with the poor durability was the expense and inconvenience of doing repairs or getting replacement devices.
“Well, they break down, you know, after awhile they break down in the, you know, either the wire on the top breaks or it becomes undone on the back or the plastic just deteriorates and, you know, chunks off.”
Participants described some inconvenience associated with cleaning the OA, which was perceived as a nuisance rather than a major concern. Additionally, there appeared to be some uncertainty about the best way to clean the device and which cleaning products were most effective and efficient.
Some participants perceived the use of the OA as contributing to gum disease and cavities. In some cases, dentists have told the OA users that the device promotes these problems, whereas other users speculated on this association based on their own experiences.
Among the less frequently mentioned factors impacting treatment choice was a concern about the impact on the user’s bite from wearing the OA. This impact would not necessarily lead participants to select CPAP but it would be something they considered when making their treatment selection.
Benefit of treatment for bed partners
As indicated above, the least frequently mentioned benefit that patients hope to achieve with treatment is benefits for their bed partners. Nonetheless, participants did indicate that their bed partners are benefiting. The primary impact of treatment on bed partners is improved sleep, principally because of a reduction or elimination of snoring by the patient but also because the patient has less thrashing around in his sleep and is not experiencing episodes of apnea—all of which are extremely disruptive for bed partners. The disruption for bed partners and ensuing benefit of treatment was described by a participant who said:
“Cause there is the benefit to [the bed partner], at least you’re not snoring, so you’re not disrupting their sleep. Or you’re not stopping breathing for 20 seconds, up to a minute and they’re wondering if you’re going to gasp and get going again.”
With the patient receiving treatment, the bed partners were described as having an improved quality of life, being happier, better rested, and willing to sleep in the same bed as the patient.
Factors impacting choice of treatment
The following describes the factors impacting treatment choice that were mentioned in all five of the focus groups (Table 2). Participants stressed the importance of the treatments’ effectiveness for their choice of devices, as well as in their satisfaction with the device and their continued use of it. Clearly, none of the other aspects of the treatments matter if the devices do not provide significant improvement of their condition. The importance of effectiveness was evident in a participant’s comment that he would be willing to pay the cost of the CPAP because of its greater effectiveness than the OA:
“There was no guarantee that the extended health would cover [the CPAP]. But I was willing to, because it was more effective.”
Others simply stated that effectiveness was the most important or only factor driving their choice of devices.
Participants had a preference for a transportable device that is small and easy to pack for traveling. This appeared to be especially important for participants who do travel that requires minimal baggage, such as for camping, hiking, or motorcycle trips. For frequent business travelers, a small device was favored because it could be packed in carry-on luggage. As well, one participant mentioned that he would like a device that could be used on a plane.
In selecting an OSA treatment, participants preferred a device that does not make them feel embarrassed when using it around friends or bed partners. Some participants felt a need to keep their use of the CPAP a secret and concerns were voiced about using it with new bed partners. The OA was seen as preferable to the CPAP with respect to using it around others.
“And so, like, I don’t know anybody who is in a new relationship who would stick one of those things [the CPAP] to their face, you know. It’s just not too appealing. But the oral appliance is not a big deal…Don’t even know it’s there.”
Cost was a factor in selecting a treatment and both OA and CPAP were perceived by participants as expensive. Some participants indicated that their choice would be influenced by which treatment was covered by their extended health insurance. Others said that they were willing to pay whatever it costs for the treatment provided that the treatment is highly effective:
“We don’t have extended care. So—but as far as health, we would be certainly willing to pay for anything that would help.” Generally, participants would like to see the cost of the treatments come down and some speculated that more people would use them if they were more affordable.
Bed partners primarily influenced participants’ choice of treatment with respect to noise issues. This manifested itself in two types of preferences: a quieter treatment (i.e., oral appliance) or a treatment that was effective at reducing snoring (which could be either the OA or CPAP). One participant indicated that the CPAP satisfied the noise issues for his bed partner because his snoring was brought under control and his bed partner “appreciates that white noise” the machine makes.
For some participants, primarily those who travel to places without power, such as on camping or hiking trips, needing a power supply was a consideration in their decision-making. Similar to the power supply issue was the need to access hot water for use of the OA. Participants who engage in camping indicated that a lack of hot water was problematic for using the OA, although they suggested alternatives such as warming the device in their armpits.
Discussion
To our knowledge, this is the first study to evaluate CPAP and OA side by side as treatment options for OSA and that focused on the patients’ perspective about which therapy attributes are most important in selecting a therapy. Participants were generally pleased with the devices’ ability to reduce or eliminate OSA and associated symptoms, which were among the primary benefits being sought from treatment. Despite the effectiveness of the treatments, participants did voice a large number of negative aspects associated with using the devices, although participants were still committed to using a sleep apnea treatment. The side effects were consistent with those reported in other studies [17, 18]. The focus groups results yielded insights into the experience of using CPAP and OA for the treatment of sleep apnea. Given that there is a choice of treatments, the focus groups illustrate some of the factors that impacted which device the participants selected and this information can now be used in developing discrete choice experiment questionnaires and/or other quantitative evaluations on the impact of patient’s characteristics on treatment acceptance and adherence. The quantitative questionnaire should be tested in a newly diagnosed patient group to confirm these findings and ideally improve long-term treatment effectiveness.
Previous studies have described OA as having fewer side effects than CPAP, but in this study a nearly equal number of side effects were identified for the treatments. There were individual-level differences in the factors that impacted the participants’ choice for treatment. These differences may, in part, vary with the individual’s personality [19], lifestyle, perceived or real stigma associated with treatment, and financial status. The participants in our study were selected among OSA patients who currently receive treatment for their condition and are thus receptive to treatment. However, some OSA patients may be less inclined to adopt a treatment therapy because they are generally less willing to endure treatments with side effects or have a lesser ability to cope with undesirable complications of treatment [20]. Recognizing a patient’s willingness to accept different types of side effects may be of use to practitioners in selecting the most appropriate treatment for individual patients, but it is also important for practitioners to recognize that some patients may fail to comply with treatment regardless of the treatment selected if they have a predisposition for low adoption or adherence of medical treatments.
Previous studies found that lower socioeconomic status is negatively associated with adherence [21, 22]. Consistent with this finding, the participants in our study were adherent to treatment and assumed to be of moderate to high socioeconomic status. Although we did not collect information explicitly on income, information about the participants’ occupations are consistent with a stable financial situation. In our province, public health care covers the diagnosis of OSA but not the treatment; therefore, participants would either have extended health benefits that cover OSA treatment (68% had extended health coverage although it did not necessarily fully cover treatment) or the resources to pay out of pocket. Despite the presumed financial stability of our study participants, cost was identified as a factor in selecting a treatment, although both OA and CPAP were perceived as expensive. Further investigation is necessary to understand how patients weigh the cost of treatment against other attributes of OSA treatments.
This study has several limitations, some inherent to qualitative analysis. As is standard procedure in focus group analyses, all identifiers were removed from the transcripts so it is not possible to determine if comments on a particular theme are being made by multiple participants or repeatedly by one or a few individuals. Consequently, the frequency with which themes were mentioned does not necessarily reflect the relative importance of that theme across participants. The findings cannot be presumed to be representative of all OSA patients: despite reaching saturation, the number of subjects was small; all the participants lived in the same region and may have shared cultural factors; we assume that most patients in this sample had a reasonably stable financial condition given their occupational statuses; patients recruited to participate were compliant with their treatment therapies and thus we do not have the perspective of patients who use CPAP or OA on an intermittent basis or who discontinued treatment; there were more patients on OA than CPAP; male female distribution was not equivalent for both treatments and all patients in our study had the same referral source and thus we could not assess the role of physicians on adherence (which has been shown to be a factor in compliance [23, 24]). Another limitation of the current study is that compliance to treatment was not objectively measured. Since compliance monitors for oral appliances are only now being developed and are not commercially available in most countries, we have used only questions to assess compliance for both therapies. As an inclusion criteria, we have asked if they used their treatment most of the nights per week and most of the hours during sleep.
An important factor in the patient’s treatment choice is the practitioner’s influence on the patient decision. For our cohort of patients, CPAP was always prescribed first, as the main therapy. If patients were non-compliant to CPAP, then the physician disclosed the other treatment option, an oral appliance. We understand this is a limitation of the study and believe future studies are necessary to assess the impact of practitioners’ beliefs and their impact on treatment choices.
Despite the study limitations, insights derived from the focus groups about the factors that impact treatment choice and the experience of using the therapies could be used by practitioners to help patients select the best treatment to meet their physical and lifestyle needs and to better prevent and manage side effects, thus potentially improving adherence.
Conclusion
This is the first study comparing patients’ perspectives for CPAP and OA therapy using qualitative methods. Perceived negative effects of CPAP and OA were very different. There are many factors that impacted choice of treatment option, and patients seem to weigh factors differently than practitioners regarding choice of OSA treatment options. Practitioners need to be aware not only of the treatment qualities but also need a better understanding of the patient’s personality, lifestyle, and financial condition in order to prescribe a treatment that best meets the patient’s needs. Doing so may achieve greater likelihood of adherence.
References
Goncalves MA, Paiva T, Ramos E, Guilleminault C (2004) Obstructive sleep apnea syndrome, sleepiness, and quality of life. Chest 125(6):2091–2096
Young T, Skatrud J, Peppard PE (2004) Risk factors for obstructive sleep apnea in adults. JAMA 291(16):2013–2016
George CFP (2007) Sleep apnea, alertness, and motor vehicle crashes. Am J Respir Crit Care Med 176(10):954–956
Mulgrew AT, Nasvadi G, Butt A, Cheema R, Fox N, Fleetham JA, Ryan CF, Cooper P, Ayas NT (2008) Risk and severity of motor vehicle crashes in patients with obstructive sleep apnoea/hypopnoea. Thorax 63(6):536–541
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea–hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365(9464):1046–1053
Shapiro GK, Shapiro CM (2010) Factors that influence CPAP adherence: an overview. Sleep Breath 14:323–335
Ferguson KA, Cartwright R, Rogers R, Schmidt-Nowara W (2006) Oral appliances for snoring and obstructive sleep apnea: a review. Sleep 29(2):244–262
McCombs J, Nichol M, Newman C, Sclar D (1994) The costs of interrupting antihypertensive drug therapy in a Medicaid population. Med Care 32(3):214–226
Bansback NJ, Anis AH, Marra CA (2008) Patient reported outcomes for rheumatoid arthritis: where are we and where are we going? J Rheumatol 35(8):1482–1483
Sabaté E, WHO Adherence to Long Term Therapies Project, Global Adherence Interdisciplinary Network, World Health Organization, Dept. of Management of Noncommunicable Diseases (2003) Adherence to long-term therapies: evidence for action. World Health Organization, Geneva
Morgan DL (1988) Focus groups as qualitative research. Sage, Newbury Park
Macnaghten P, Myers G (2004) Focus groups. In: Seale C, Gobo G, Gubrium JF, Silverman D (eds) Qualitative research practice. Sage, London, pp 312–326
Roux L, Ubach C, Donaldson C, Ryan M (2004) Valuing the benefits of weight loss programs: an application of the discrete choice experiment. Obes Res 12(8):1342–1351
Ryan M (2004) Discrete choice experiments in health care. BMJ 328(7436):360–361
Sandelowski M (2000) Whatever happened to qualitative description? Res Nurs Heal 23(4):334–340
US Department of Labor (2010) Standard occupational classification. Bureau of Labor Statistics, available at http://www.bls.gov/soc/classification.htm. Accessed July 6, 2011
Brostrom A, Arestedt K, Nilsen P, Stromberg A, Ulander M, Svanborg E (2010) The side-effects to CPAP treatment inventory: the development and initial validation of a new tool for the measurement of side-effects to CPAP treatment. J Sleep Res 19(4):603–611
Almeida FR, Lowe AA (2009) Principles of oral appliance therapy for the management of snoring and sleep disordered breathing. Oral Maxillofac Surg Clin North Am 21(4):413–420
Brostrom A, Stromberg A, Ulander M, Fridlund B, Martensson J, Svanborg E (2009) Perceived informational needs, side-effects and their consequences on adherence—a comparison between CPAP treated patients with OSAS and healthcare personnel. Patient Educ Couns 74(2):228–235
Weaver TE (2006) Adherence to positive airway pressure therapy. Curr Opin Pulm Med 12(6):409–413
Platt A, Field S, Asch D, Chen Z, Patel N, Gupta R, Roche D, Gurubhagavatula I, Christie J, Kuna S (2009) Neighborhood of residence is associated with daily adherence to CPAP therapy. Sleep 32:799–806
Simon-Tuval T, Reuveni H, Greenberg-Dotan S, Oksenberg A, Tal A, Tarasiuk A (2009) Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep 32:545–552
Taylor S (2006) Health psychology. McGraw Hill, Toronto
Brostrom A, Nilsen P, Johansson P, Ulander M, Stromberg A, Svanborg E, Fridlund B (2009) Putative facilitators and barriers for adherence to CPAP treatment in patients with obstructive sleep apnea syndrome: a qualitative content analysis. Sleep Medicine 11(2):126–130
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Almeida, F.R., Henrich, N., Marra, C. et al. Patient preferences and experiences of CPAP and oral appliances for the treatment of obstructive sleep apnea: a qualitative analysis. Sleep Breath 17, 659–666 (2013). https://doi.org/10.1007/s11325-012-0739-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-012-0739-6