Abstract
Background
Hypercalcemia is highly prevalent in kidney transplant recipients with hyperparathyroidism. However, its long-term impact on graft function is uncertain.
Methods
We conducted a prospective cohort study investigating adverse graft outcomes associated with persistent hypercalcemia (free calcium > 5.2 mg/dL in ≥ 80% of measures) and inappropriately elevated intact parathyroid hormone (> 30 pg/mL) in kidney transplant recipients. Asymptomatic mild hypercalcemia was monitored unless complications developed.
Results
We included 385 kidney transplant recipients. During a 4-year (range 1–9) median follow-up time, 62% of kidney transplant recipients presented persistent hypercalcemia. Compared to kidney transplant recipients without hypercalcemia, there were no significant differences in graft dysfunction (10% vs. 12%, p = 0.61), symptomatic urolithiasis (5% vs. 3%, p = 0.43), biopsy-proven calcium deposits (6% vs. 5%, p = 1.0), fractures (6% vs. 4%, p = 0.64), and a composite outcome of urolithiasis, calcium deposits, fractures, and parathyroidectomy indication (16% vs. 13%, p = 0.55). In a subset of 76 kidney transplant recipients, subjects with persistent hypercalcemia had higher urinary calcium (median 84 [43–170] vs. 38 [24–64] mg/day, p = 0.03) and intact fibroblast growth factor 23 (median 36 [24–54] vs. 27 [19–40] pg/mL, p = 0.04), and lower 25-hydroxyvitamin D levels (11.3 ± 1.2 vs. 16.3 ± 1.4 ng/mL, p < 0.001). In multivariate analysis, pretransplant intact parathyroid hormone < 300 pg/mL was associated with a reduced risk of post-transplant hypercalcemia (OR 0.51, 95% CI 0.32–0.80).
Conclusions
Long-term persistent mild hypercalcemia (tertiary hyperparathyroidism) was frequent in kidney transplant recipients in our series. This condition presented with lower phosphate and 25-hydroxyvitamin D, and higher urinary calcium and intact fibroblast growth factor 23 levels compared to kidney transplant recipients without hypercalcemia, resembling a mild form of primary hyperparathyroidism. Despite these metabolic derangements, the risk of adverse graft outcomes was low.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Persistent hyperparathyroidism is a frequent complication in kidney transplant recipients, even with adequate kidney function [1,2,3,4,5]. There is significant controversy about the impact of persistent hyperparathyroidism after transplantation, with reports suggesting a slight increase in mortality and graft dysfunction rates. However, this association still needs to be clarified due to confounding factors such as comorbidities, dialysis vintage, delayed graft function, and imprecise assessment of calcium status using total calcium, among others [6].
Hypercalcemia is one of the mechanisms by which hyperparathyroidism after transplantation may increase the risk of adverse outcomes, including urolithiasis, fractures, graft dysfunction, vascular calcification, and even mortality [7, 8]. Elevated calcium is widely recognized as a “toxin” that could potentially cause direct damage to the graft due to its hemodynamic effects, the proclivity to enhance extra-skeletal calcium deposition, and the formation of kidney stones secondary to hypercalciuria, among other possible effects [9].
Assessing the hazards of hypercalcemia related to hyperparathyroidism in kidney transplant recipients is challenging. Previous cohorts presented many confounding factors, such as poor characterization of hypercalcemic kidney transplant recipients, limited post-transplant follow-up periods, incorrect use of albumin-adjusted formulas to assess calcium status [10], and widespread use of calcimimetics to treat hypercalcemia [5, 11].
We conducted a long-term observational cohort study to understand the effects of persistent hypercalcemia after transplantation and to assess the graft outcomes associated with hypercalcemia related to hyperparathyroidism in kidney transplant recipients.
Materials and methods
Study design and subjects
We conducted a prospective observational cohort study of kidney transplant recipients who underwent kidney transplantation between January 23, 2014, and February 6, 2023.
The study was conducted at Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán in Mexico City, Mexico. The institution’s transplant clinic measures biochemical parameters every 3–6 months after transplantation and annual or biannual intact parathyroid hormone (iPTH) measurements. In addition, every kidney transplant recipient undergoes at least one protocol graft biopsy during the first year (3rd and 12th months), and annual monitoring of donor-specific HLA-antibodies along with graft biopsy for those with de-novo donor-specific antibodies. Furthermore, a graft biopsy is performed when graft dysfunction is identified, which is characterized by serum creatinine > 20% of baseline or proteinuria.
Due to financial constraints and a lack of insurance coverage, cinacalcet is not readily available for patients with uncontrolled hyperparathyroidism in our institution. Therefore, the institutional protocol recommends subtotal parathyroidectomy before transplantation in patients with tertiary hyperparathyroidism [12, 13]. After transplantation, vitamin D, oral calcium, or thiazide diuretics are suspended when mild hypercalcemia (free [ionized] calcium 5.2–6.0 mg/dL) is present. If hypercalcemia persists after these interventions, watchful waiting is indicated unless symptoms or complications appear. In such cases, the attending physician may consider a parathyroidectomy.
We included all subjects aged 18 years or older who underwent kidney transplantation and had at least two iPTH and free or total calcium measurements before and after the procedure. We excluded kidney transplant recipients who developed hypercalcemia caused by malignancy, active tuberculosis, granulomatous diseases, or other causes unrelated to iPTH. Additionally, we excluded subjects diagnosed with primary hyperparathyroidism and those with graft dysfunction within 3 months after surgery.
The study’s primary objectives were to assess the rates of graft dysfunction, symptomatic urolithiasis (identified through clinical symptoms or CT evidence in the graft), graft calcium deposits (detected through graft biopsy), and fractures in kidney transplant recipients with persistent hyperparathyroidism and hypercalcemia. Graft dysfunction was operationally defined as a sustained estimated glomerular filtration rate (eGFR) below 30 mL/min/1.73 m2 for 3 months or longer, as determined using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) 2021 formula [14]. We selected this specific eGFR limit to minimize the potential confounding effects that could arise from poor allograft function on biochemical mineral metabolism measurements. A composite outcome was created to include urolithiasis, biopsy-proven calcium deposits, fractures, and a clinical indication of parathyroidectomy following kidney transplantation. Other graft outcomes of interest included a sustained ≥ 50% decrease in eGFR from nadir for 12 weeks and end-stage kidney disease (ESKD) defined as the initiation of long-term dialysis for ≥ 90 days, or eGFR < 15 mL/min/1.73 m2 sustained for ≥ 3 months.
Hypercalcemia due to persistent hyperparathyroidism (tertiary hyperparathyroidism) was defined as a free calcium level > 5.2 mg/dL and an inappropriately normal or elevated iPTH (> 30 pg/mL). We selected this definition because many cases of hyperparathyroidism with hypercalcemia present with normal iPTH levels, caused by an inappropriately unsuppressed parathyroid hormone in response to hypercalcemia [15, 16].
The cohort was categorized according to the presence of persistent hypercalcemia (≥ 80% of free calcium measurements during the follow-up period with hypercalcemia), transient hypercalcemia (≥ 2 consecutive free calcium measurements with hypercalcemia) that resolved after discontinuing medications, such as oral calcium, vitamin D supplementation, or thiazide diuretics, and no hypercalcemia (kidney transplant recipients who did not fulfill any of the previous definitions). In a subgroup of participants (n = 76), we measured several biomarkers of bone and mineral metabolism to be investigated as secondary outcomes, including 24-h urinary calcium levels, intact fibroblast growth factor 23, osteoprotegerin, osteocalcin, osteopontin, 25-hydroxyvitamin D, and interleukin-6.
The hospital Institutional Review Board (Comité de Ética en Investigación) approved the study (NMM-4220-22-23-1), which complies with the Helsinki Declaration. Participants who underwent biomarker assessment provided informed consent.
Assays
Serum free calcium was measured by the potentiometric method with ion-selective electrodes by ABL90 instruments standardized at pH 7.40 (Radiometer Medical, Copenhagen, Denmark). The reference range for free calcium was 4.3–5.2 mg/dL (1.07–1.3 mmol/L), with limits of 0.8–40.04 mg/dL (0.2–9.98 mmol/L). When free calcium was unavailable (n = 4158/9242, 45%), we utilized a formula validated in our center to estimate free calcium levels (free calcium (mmol/L) = 0.541 + (total calcium [mmol/L] * 0.441) − (serum albumin [g/L] * 0.0067) − (serum phosphate [mmol/L] * 0.0425) − (CO2 [mmol/L] * 0.003)) [17]. Total calcium was assayed using the Arsenazo III reagent colorimetric method (reference values 8.6–10.3 mg/dL [2.15–2.57 mmol/L], Beckman Coulter, Brea, CA, USA). Plasma iPTH was measured using an immunoradiometric assay (reference value 12–88 pg/mL [1.3–9.3 pmol/L], Beckman-Coulter, Brea, CA, USA). The concentrations of osteoprotegerin, intact fibroblast growth factor 23, osteocalcin, osteopontin, and interleukin-6 were determined using the Magpix system (HBNMAG-51K-04) and the xPonent 4.2 software (Luminex Corporation, Austin, TX, USA). Serum total 25-hydroxyvitamin D was measured via chemiluminescence using the Diasorin Liason assay (Saluggia, Italy). Bone mineral density was measured by dual-energy X-ray absorptiometry using a Lunar densitometer (Hologic QDR-4000). Protocol graft biopsies were performed in all patients at least once. A renal pathologist reviewed all biopsies and reported them according to the BANFF classification.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD) for normally distributed data and median with interquartile range (IQR) for non-normally distributed data; categorical variables are expressed as frequencies and percentages.
The primary measure of exposure was the presence of hypercalcemia during follow-up. Analysis of variance or non-parametric Wilcoxon tests were used to investigate the differences between groups according to the three observed free calcium trajectories. Cross-tabulated data were analyzed with chi-square or Fisher tests. Graft and survival curves were drawn using the Kaplan–Meier estimate and compared using the log-rank test. We performed a logistic regression analysis to assess predictors of persistent hypercalcemia. The levels of urinary calcium, 25-hydroxyvitamin D, and bone biomarkers between groups were compared with the T test or Mann–Whitney U test according to distribution. We calculated the area under the receiver operating characteristic curve (AUC) to identify pretransplant iPTH cut-offs to diagnose persistent hypercalcemia. We used the repeated measures model for statistical comparisons of repeated biochemical parameters between groups. All longitudinal analyses for free calcium and other biochemical measurements were censored when graft dysfunction occurred (eGFR < 30 mL/min/1.73 m2) or when a subject underwent parathyroidectomy. To analyze the risk associated with iPTH levels before transplantation, we categorized our cohort according to the iPTH goals proposed by Kidney Disease Improving Global Outcomes (KDIGO) (low, normal, or high according to iPTH < 2 ×, 2–9 ×, and > 9 × the upper reference limit, respectively) [18]. We compared the levels between the persistent hypercalcemia and non-hypercalcemia groups and between the iPTH strata for each biochemical parameter. We also evaluated the primary outcomes in subjects with overt hypercalcemic hyperparathyroidism (iPTH levels above the upper reference limit [> 88 pg/mL] and hypercalcemia [free calcium > 5.2 mg/dL]). The differences with 95% confidence intervals (CIs) and p values were estimated for the comparison. Multivariate analyses were adjusted for the following risk factors: age, sex, preoperative iPTH, free calcium, phosphate, dialysis type, and vintage. Analyses were conducted using SPSS 24.0 (IBM, Armonk, New York, USA) and GraphPad Prism 9.5.0 (GraphPad Software, San Diego, USA). A two-sided significance threshold was set at p < 0.05.
Results
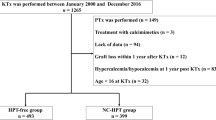
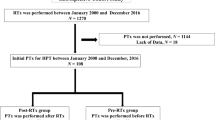
We included 385 of 409 subjects who underwent kidney transplantation at our institution. Patients who experienced early graft dysfunction (within 3 months of surgery) due to acute immunological rejection (n = 10) or vascular complications (n = 8), primary hyperparathyroidism (n = 4), and hypercalcemia not related to iPTH (n = 2) were excluded from the analysis. The median follow-up period was 4.1 (IQR 1–8.2, range 1–9) years, and the median total number of graft biopsies per subject was 3 (IQR 2–4). Before transplantation, calcitriol, cinacalcet, sevelamer, and calcium carbonate were prescribed in 137 (36%), 2 (0.5%), 67 (17%), and 91 (24%) kidney transplant recipients, respectively. The immunosuppression regimen included tacrolimus, mycophenolate mofetil, and prednisone in 373 (97%), 300 (78%), and 385 (100%) kidney transplant recipients, respectively.
Mild hypercalcemia (free calcium between 5.21 to 6.0 mg/dL) occurred in 50–70% of the cohort after 12 months of kidney transplantation, as documented by at least one measurement (Fig. 1). Among the kidney transplant recipients, we observed three patterns of calcium trajectory: normocalcemia (n = 76, 20%), persistent hypercalcemia (n = 240, 62%), and transient hypercalcemia (n = 69, 18%) that resolved after discontinuing medications, such as oral calcium, vitamin D supplementation, or thiazide diuretics. Table 1 presents the characteristics of the groups according to calcium trajectory. After transplantation, iPTH levels ≥ 2 × the upper reference limit (≥ 176 pg/mL) were detected in 22%, 21%, 3%, and 2% of kidney transplant recipients at 6, 12, 24, and 36 months of follow-up, respectively. However, in all cases of persistent hypercalcemia, the iPTH level was inappropriately normal or elevated (> 30 pg/mL) throughout the follow-up period. The median [IQR] levels of iPTH were significantly higher in kidney transplant recipients with persistent hypercalcemia compared to those without this finding after transplantation (113.5 [77.5–172.9] vs. 99.1 [63.7–142.1], p = 0.017). None of the subjects with persistent hypercalcemia received cinacalcet, and only 3 (0.1%) underwent parathyroidectomy due to symptomatic urolithiasis.
Although persistent hypercalcemia was a frequent finding following transplantation, the risk of adverse outcomes did not increase significantly during the follow-up period. Compared to those without persistent hypercalcemia, kidney transplant recipients with persistent hypercalcemia did not show significant differences in rates of graft dysfunction defined as a sustained eGFR below 30 mL/min/1.73 m2 (10% vs. 12%, p = 0.61), symptomatic urolithiasis (5% vs. 3%, p = 0.43), calcium deposits in graft biopsy (6% vs. 5%, p = 1.0), fractures (6% vs. 4%, p = 0.64), sustained decrease in eGFR ≥ 50% (4% vs. 4%, p = 1.0), and incidence of ESKD (3% vs 3%, p = 1.0). Of the 385 kidney transplant recipients, 57 (15%) experienced a composite outcome of urolithiasis, biopsy-proven calcium deposits, fractures, or an indication of parathyroidectomy. Nevertheless, the composite outcome was not statistically different between the two groups (38/240, 16%, vs. 19/145, 13%, p = 0.55). Figure 2 presents the odds ratios and 95% CIs for principal outcomes. Similarly, graft and overall survival rates did not differ significantly between the two groups (Fig. 3a and b). Moreover, 110 (29%) kidney transplant recipients developed overt hypercalcemic hyperparathyroidism (iPTH levels above the upper reference limit [> 88 pg/mL] and hypercalcemia [free calcium > 5.2 mg/dL]). These subjects did not have an increased risk of graft dysfunction (10% vs. 11%, p = 0.85), symptomatic urolithiasis (5% vs. 4%, p = 0.77), calcium deposits in graft biopsy (8% vs. 5%, p = 0.22), fractures (6% vs. 5%, p = 0.51), or the composite outcome (20% vs. 13%, p = 0.08) compared to those without hyperparathyroidism.
Forest plot of outcomes associated with hypercalcemia. Odds ratio and 95% confidence interval for each outcome. Graft dysfunction was defined as eGFR < 30 mg/mL/1.73 m2 for > 3 months. The composite outcome included urolithiasis, biopsy-proven calcium deposits, fractures, and an indication of parathyroidectomy after transplantation
We also measured urinary calcium, bone biomarkers, and 25-hydroxyvitamin D in a sample of 76 subjects from the original cohort. Compared to those without persistent hypercalcemia, kidney transplant recipients with persistent hypercalcemia showed higher levels of urinary calcium (median 84 [IQR 43–170] vs. 38 [IQR 24–64] mg/day, p = 0.03) and higher levels of intact fibroblast growth factor 23 (median 36 [IQR 24–54] vs. 27 [IQR 19–40] pg/mL, p = 0.04). In contrast, the group with persistent hypercalcemia had lower 25-hydroxyvitamin D levels (11.3 ± 1.2 vs. 16.3 ± 1.4 ng/mL, p < 0.001) and more cases with 25-hydroxyvitamin D < 12 ng/mL (25 [52%] vs 7 [25%], p < 0.001). Hypercalciuria > 230 mg/day was present in 10 (13%) kidney transplant recipients with persistent hypercalcemia. Supplementary Table 1 provides further details on the other studied biomarkers. Moreover, the group of kidney transplant recipients with persistent hypercalcemia exhibited slightly higher eGFRs during follow-up. In addition, phosphate levels were significantly lower in the group with persistent hypercalcemia compared to those without hypercalcemia at 12 (3.04 ± 0.56 vs. 3.37 ± 0.66 mg/dL, p < 0.0001), 24 (3.14 ± 0.57 vs. 3.41 ± 0.54 mg/dL, p < 0.0001), and 36 (3.05 ± 0.50 vs. 3.37 ± 0.68 mg/dL, p = 0.001) months after transplantation (Fig. 4). No differences in the femoral neck and lumbar spine bone mineral densities were observed between groups.
The cohort was also categorized based on iPTH levels before transplantation. The predictive performance of pretransplant iPTH levels for persistent hypercalcemia after transplantation was low, with an AUC-ROC of 0.61 (95% CI 0.55–0.67). Persistent hypercalcemia was observed in 36 (49%), 130 (63%), and 74 (72%) subjects with pretransplant iPTH levels of < 2 ×, 2–9 ×, and > 9 × the upper reference limit for iPTH, respectively. In a multivariate analysis adjusted for sex, age, dialysis vintage, baseline free calcium and phosphate levels, and diabetes, lower pretransplant levels of iPTH (< 300 pg/mL) were associated with a reduced risk of persistent hypercalcemia after transplantation (OR 0.51, 95% CI 0.32–0.80). In contrast, iPTH levels < 9 × the upper reference limit were not associated with a significant risk reduction of persistent hypercalcemia (OR 0.68, 95% CI 0.40–1.19).
Discussion
In this cohort of 385 kidney transplant recipients, almost two-thirds had persistent hypercalcemia due to hyperparathyroidism, lasting for many years after transplantation. Persistent hypercalcemia rates were high throughout the follow-up period, but symptoms were uncommon; therefore, they were usually left untreated. Although kidney transplant recipients with persistent hypercalcemia had a higher rate of complications in the composite outcome (urolithiasis, calcium graft deposits, fractures, and parathyroidectomy indication), the small number of occurrences did not result in statistically significant differences compared to non-hypercalcemic subjects.
Our cohort differs from previously published studies. Most of our patients had elevated iPTH levels before transplantation; nearly a third had extremely high iPTH levels (more than nine times above the upper reference limit). Moreover, only one-fifth of the kidney transplant recipients had both normocalcemia and iPTH within normal range after a median follow-up of 4 years, and they did not receive calcimimetics, calcitriol or active vitamin D. These characteristics differ from other cohorts, in which either a significant number of kidney transplant recipients received calcimimetics [5, 11], the follow-up time was less than 2 years, calcium status was not assessed by free calcium levels [4], or most subjects underwent transplantation with iPTH levels within the range recommended by the K-DIGO guidelines [3,4,5]. Treating hyperparathyroidism after a kidney transplant can be challenging, and cohort studies with treatment based on symptoms and other manifestations (wait-and-see strategy) are scarce [19].
It has been hypothesized that kidney transplant recipients with post-transplant hyperparathyroidism will eventually experience a reduction of the hyperplastic parathyroid tissue [20]. Furthermore, some authors have speculated that after transplantation, the calcium threshold for iPTH secretion may be modified due to changes in the calcium-sensing receptor expression in parathyroid cells, similar to that seen in patients with familial hypocalciuric hypercalcemia [2]. This condition may present with mild hypercalcemia with elevated iPTH levels, up to twice the upper reference limit, but without hypercalciuria or an increased risk of lithiasis or fractures. Another hypothesis suggests calcineurin inhibitors may increase bone resorption, leading to hypercalcemia [21]. At difference, our findings show that kidney transplant recipients with persistent mild hypercalcemia have inappropriate iPTH levels, low phosphate and 25-hydroxyvitamin D serum levels, and slightly elevated calciuria, a biochemical profile resembling mild primary hyperparathyroidism.
The increased intact fibroblast growth factor 23 levels in the persistent hypercalcemia group could be explained by a direct, positive effect exerted by calcium and iPTH, both stimulators of intact fibroblast growth factor 23 production [22, 23]. Among other causes, a sustained decrease in 25-hydroxyvitamin D synthesis could be attributed to the persistent elevations in intact fibroblast growth factor 23 levels in the hypercalcemic group [24] and to the effect of PTH on 1-alpha- hydroxylase, findings described in other kidney transplant recipient cohorts with hypercalcemia related to hyperparathyroidism [25]. Elevated intact fibroblast growth factor 23 levels and hypovitaminosis D could represent an adaptive response that reduces the severity of hypercalcemia and hypercalciuria, yet this mechanism may have long-term effects on bone density [26].
Even though urinary calcium values in kidney transplant recipients with persistent hypercalcemia were lower compared to subjects with high risk for urolithiasis (> 4 mg/kg), they were near the upper reference limit and significantly higher than in the kidney transplant recipients without persistent hypercalcemia. Urinary calcium levels > 230 mg/day, a cut-off value proposed by some authors as a predictor of urolithiasis in patients with primary hyperparathyroidism [27], were observed in 13% of kidney transplant recipients in the hypercalcemic group. It is possible that if subjects with persistent hypercalcemia underwent a 25-hydroxyvitamin D correction > 20 ng/mL (the recommended 25-hydroxyvitamin D target for many experts), their serum and urinary calcium levels would increase, thereby fulfilling the classic criteria for autonomous hyperparathyroidism (tertiary hyperparathyroidism) [28]. Although the risks associated with mild hypercalcemia following transplantation may be minor, they should be avoided. A successful transplantation program should aim for a zero de novo lithiasis rate, including calcium deposits in renal biopsies.
Achieving K-DIGO goals for controlling hyperparathyroidism before transplantation may not be sufficient to prevent post-transplant hypercalcemia. In our cohort, only pretransplant iPTH levels below 300 pg/mL were associated with a lower risk of hypercalcemia, in keeping with a recent report that found the same cut-off value associated with developing tertiary hyperparathyroidism after transplantation [29]. These findings suggest that aiming for lower pretransplant PTH levels, as recommended by the K-DOQI decades ago, could prevent hypercalcemia after transplantation [30].
Our study has limitations. Given the low number of patients who reached the various outcomes, the sample size may need to be expanded. Our statistical power was 41% for the composite outcome, notwithstanding criticisms of retrospective cohort power calculations [31]. Still, a study with 80% statistical power would need more than 1200 “untreated” hypercalcemic kidney transplant recipients, a number difficult to achieve, unless with multicenter or multinational trials, and extended follow-up periods.
Another limitation in our study is the possibility that some kidney transplant recipients with normocalcemia and slightly elevated iPTH could have been misclassified. We identified about one-fifth of subjects who experienced transient hypercalcemia, which occurred while taking vitamin D supplements or thiazides. It is known that patients with high iPTH and normocalcemia may have occult autonomous hyperparathyroidism that is only revealed when hypovitaminosis D is corrected [32]. As a result, the actual prevalence of hyperparathyroidism may be underestimated. Another limitation is the insufficient availability of dual-energy X-ray absorptiometry scan or imaging data to assess vascular calcification. Nevertheless, specific markers directly linked to the burden of calcification, such as osteoprotegerin [33], were not elevated in the group of patients with persistent hypercalcemia. Also, we did not measure 1,25-dihydroxy vitamin D, which some researchers reported to rise due to abnormal 1-alpha-hydroxylase activity in tubular graft cells, causing hypercalcemia [3].
In conclusion, following transplantation, persistent hypercalcemia mediated by tertiary hyperparathyroidism was a frequent finding. Even though the overall number of cases reaching the composite outcome of urolithiasis, graft calcifications, or fractures was higher in the group with persistent hypercalcemia, its incidence was low and did not achieve statistical significance compared to kidney transplant recipients without hypercalcemia. We must emphasize that hypercalcemia associated with hyperparathyroidism after kidney transplantation is a common and underdiagnosed problem, carrying a relatively low risk of adverse graft outcomes in the long term. However, while rare, severe consequences of this condition can potentially occur and must be prevented.
Data availability statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
Abbreviations
- KTR:
-
Kidney transplant recipient.
- IQR:
-
Interquartile range.
- PTH:
-
Parathyroid hormone.
- iPTH:
-
Intact parathyroid hormone.
- DSA:
-
Donor-specific HLA-antibodies.
- eGFR:
-
Estimated glomerular filtration rate.
- ESRD:
-
End stage renal disease
- iFGF23:
-
Intact fibroblast growth factor 23.
- OPG:
-
Osteoprotegerin.
- OC:
-
Osteocalcin.
- OPN:
-
Osteopontin.
- 25(OH)D:
-
25-Hydroxyvitamin D.
- IL-6:
-
Interleukin-6.
- BMD:
-
Bone mineral density.
- DEXA:
-
Dual-energy X-ray absorptiometry.
- CV:
-
Coefficient of variation.
- SD:
-
Standard deviation.
- ROC:
-
Receiver operating characteristic.
- AUC:
-
Area under the curve.
- URL:
-
Upper reference limit.
- CI:
-
Confidence interval.
- ALP:
-
Alkaline phosphatase.
- CKD:
-
Chronic kidney disease.
- ADPKD:
-
Autosomal dominant polycystic kidney disease.
- SLE:
-
Systemic lupus erythematosus.
- HLA:
-
Human leukocyte antigen
References
Brandenburg VM, Westenfeld R, Ketteler M (2004) The fate of bone after renal transplantation. J Nephrol 7:190–204
Reinhardt W, Bartelworth H, Jockenhövel F et al (1998) Sequential changes of biochemical bone parameters after kidney transplantation. Nephrol Dial Transplant 13:436–442. https://doi.org/10.1093/oxfordjournals.ndt.a027843
Alfieri C, Mattinzoli D, Messa P (2021) Tertiary, and postrenal transplantation hyperparathyroidism. Endocrinol Metab Clin N Am 50:649–662. https://doi.org/10.1016/j.ecl.2021.08.004
Evenepoel P, Claes K, Kuypers D, Maes B, Bammens B, Vanrenterghem Y (2004) Natural history of parathyroid function and calcium metabolism after kidney transplantation: a single-centre study. Nephrol Dial Transplant 19:1281–1287. https://doi.org/10.1093/ndt/gfh128
Wolf M, Weir MR, Kopyt N et al (2016) A prospective cohort study of mineral metabolism after kidney transplantation. Transplantation 100:184–193. https://doi.org/10.1097/TP.0000000000000823
Pihlstrøm H, Dahle DO, Mjøen G et al (2015) Increased risk of all-cause mortality and renal graft loss in stable renal transplant recipients with hyperparathyroidism. Transplantation 99:351–359. https://doi.org/10.1097/TP.0000000000000583
van der Plas WY, Gomes Neto AW, Berger SP et al (2021) Association of time-updated plasma calcium and phosphate with graft and patient outcomes after kidney transplantation. Am J Transplant 21:2437–2447. https://doi.org/10.1111/ajt.16457
Moe SM (2017) Calcium as a cardiovascular toxin in CKD-MBD. Bone 100:94–99. https://doi.org/10.1016/j.bone.2016.08.022
Çeltik A, Şen S, Yılmaz M et al (2016) The effect of hypercalcemia on allograft calcification after kidney transplantation. Int Urol Nephrol 48:1919–1925. https://doi.org/10.1007/s11255-016-1391-z
Ridefelt P, Helmersson-Karlqvist J (2017) Albumin adjustment of total calcium does not improve the estimation of calcium status. Scand J Clin Lab Investig 77:442–447. https://doi.org/10.1080/00365513.2017.1336568
Guerra R, Auyanet I, Fernández EJ et al (2011) Hypercalcemia secondary to persistent hyperparathyroidism in kidney transplant patients: analysis after a year with cinacalcet. J Nephrol 24:78–82. https://doi.org/10.5301/jn.2010.293
Ramírez-Sandoval JC (2020) Renal metabolic bone disease in the potential kidney transplant recipient. Rev Mex Traspl 9:68–74
Fonseca-Correa JI, Nava-Santana C, Tamez-Pedroza L et al (2021) Clinical factors associated with early and persistent hypocalcaemia after parathyroidectomy in patients on dialysis with severe hyperparathyroidism. Nephrology (Carlton) 26:408–419. https://doi.org/10.1111/nep.13854
Inker LA, Eneanya ND, Coresh J et al (2021) New creatinine- and cystatin C-based equations to estimate GFR without race. N Engl J Med 385:1737–1749. https://doi.org/10.1056/NEJMoa2102953
Bilezikian JP, Khan AA, Silverberg SJ et al (2022) International workshop on primary hyperparathyroidism. Evaluation and management of primary hyperparathyroidism: summary statement and guidelines from the fifth international workshop. J Bone Miner Res 37:2293–2314. https://doi.org/10.1002/jbmr.4677
Cusano NE, Bilezikian JP (2014) Parathyroid hormone in the evaluation of hypercalcemia. JAMA 312:680–681. https://doi.org/10.1001/jama.2014.9195
Ramirez-Sandoval JC, Diener-Cabieses P, Gutiérrez-Valle F et al (2022) Validation of an equation for free calcium estimation: accuracy improves after adjustment for phosphate and CO2. Int Urol Nephrol 54:2625–2635. https://doi.org/10.1007/s11255-022-03170-z
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group (2011) KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl 7:1–59. https://doi.org/10.1016/j.kisu.2017.04.001
Miedziaszczyk M, Lacka K, Tomczak O, Bajon A, Primke M, Idasiak-Piechocka I (2022) Systematic review of the treatment of persistent hyperparathyroidism following kidney transplantation. Biomedicines 11(1):25. https://doi.org/10.3390/biomedicines11010025
Bonarek H, Merville P, Bonarek M et al (1999) Reduced parathyroid functional mass after successful kidney transplantation. Kidney Int 56:642–649. https://doi.org/10.1046/j.1523-1755.1999.00589.x
Westeel FP, Mazouz H, Ezaitouni F et al (2000) Cyclosporine bone remodeling effect prevents steroid osteopenia after kidney transplantation. Kidney Int 58:1788–1796. https://doi.org/10.1046/j.1523-1755.2000.00341.x
Rayego-Mateos S, Doladé N, García-Carrasco A, Diaz-Tocados JM, Ibarz M, Valdivielso JM (2022) The increase in FGF23 induced by calcium is partially dependent on vitamin D signaling. Nutrients 14:2576. https://doi.org/10.3390/nu14132576
David V, Dai B, Martin A, Huang J, Han X, Quarles LD (2013) Calcium regulates FGF-23 expression in bone. Endocrinology 154:4469–4482. https://doi.org/10.1210/en.2013-1627
Dusso AS, Rodriguez M (2012) Enhanced induction of Cyp24a1 by FGF23 but low serum 24,25-dihydroxyvitamin D in CKD: implications for therapy. Kidney Int 82:1046–1049. https://doi.org/10.1038/ki.2012.273
Stavroulopoulos A, Cassidy MJ, Porter CJ, Hosking DJ, Roe SD (2007) Vitamin D status in renal transplant recipients. Am J Transplant 7:2546–2552. https://doi.org/10.1111/j.1600-6143.2007.01978.x
Perrin P, Caillard S, Javier RM et al (2013) Persistent hyperparathyroidism is a major risk factor for fractures in the five years after kidney transplantation. Am J Transplant 13:2653–2663. https://doi.org/10.1111/ajt.12425
Saponaro F, Cetani F, Mazoni L et al (2020) Hypercalciuria: its value as a predictive risk factor for nephrolithiasis in asymptomatic primary hyperparathyroidism? J Endocrinol Investig 43:677–682. https://doi.org/10.1007/s40618-019-01162-y
Bilezikian JP (2000) Primary hyperparathyroidism. When to observe and when to operate. Endocrinol Metab Clin N Am 29:465–478. https://doi.org/10.1016/s0889-8529(05)70146-8
Sutton W, Chen X, Patel P et al (2022) Prevalence and risk factors for tertiary hyperparathyroidism in kidney transplant recipients. Surgery 171:69–76. https://doi.org/10.1016/j.surg.2021.03.067
National Kidney Foundation (2003) K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis 42:S1–201
Levine M, Ensom MH (2001) Post hoc power analysis: an idea whose time has passed? Pharmacotherapy 21:405–409. https://doi.org/10.1592/phco.21.5.405.34503
Zavatta G, Clarke BL (2021) Normocalcemic primary hyperparathyroidism: need for a standardized clinical approach. Endocrinol Metab (Seoul) 36(3):525–535. https://doi.org/10.3803/EnM.2021.1061
Ramirez-Sandoval JC, Casanova I, Villar A, Gomez FE, Cruz C, Correa-Rotter R (2016) Biomarkers associated with vascular calcification in peritoneal dialysis. Perit Dial Int 36:262–268. https://doi.org/10.3747/pdi.2014.00250
Acknowledgements
We thank the study participants and Dr. Hugo E. Chávez-Chávez for help in coding subjects data for the period from 2012 through 2014.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
JCR-S: participated in all phases of the study: conception and design, patient recruitment and data acquisition, data analysis and interpretation, drafting of manuscript, revision and approval of final version. LM: participated in all phases of the study: conception and design, patient recruitment and data acquisition, data analysis and interpretation, drafting of manuscript, revision and approval of final version. GC-K: participated in data acquisition, data analysis and interpretation, drafting of manuscript, revision and approval of final version. ER-L: participated in patient recruitment and data acquisition and data analysis. NDP-C: participated in patient recruitment and data acquisition and data analysis. CC: participated in patient recruitment and data acquisition, data analysis, and contributed to new reagents or analytic tools. ENH-P: participated conception and design, patient recruitment and data acquisition, and data analysis and interpretation. NB-P: participated conception and design, patient recruitment and data acquisition, and data analysis and interpretation. VV-R: participated in the performance of the research. JMEL: participated in the performance of the research. RC-R: participated in conception and design, data analysis and interpretation, drafting of manuscript, revision and approval of final version. AAR-A: participated in conception and design, data analysis and interpretation, drafting of manuscript, revision and approval of final version. LEM-B: participated in conception and design, data analysis and interpretation, drafting of manuscript, revision and approval of final version.
Corresponding author
Ethics declarations
Conflict of interest
The results presented in this paper have not been published previously. The authors of this paper declare that the paper is original, is not plagiarized, is submitted for first publication in this journal, and has not been published or submitted for publication elsewhere, and that there is no affiliation with any organization with a direct or indirect financial interest in the subject matter discussed in the manuscript that may affect the reporting of the article submitted. No pharmaceutical or biotechnology company, foundation, or any other source participated in the design, monitoring, data collection, and analysis. Dr. Juan Carlos Ramírez-Sandoval is a member of the Review Board of Frontiers in medicine, has received honoraria from Bayer México, and has lectured for Abbvie, Amgen, Synthom, Bayer, and AstraZeneca. Dr. Ricardo Correa-Rotter is a member of the Review Board of Blood Purification, has received honoraria as consultant from AbbVie, AstraZeneca, GlaxoSmithKline, Bayer, and Boehringer Ingelheim, participates in research from: Boehringer Ingelheim, Baxter, AstraZeneca and has lectured for Amgen, AstraZeneca, Bayer, Boehringer Ingelheim and Sanofi. Luis E. Morales-Buenrostro has received honoraria from AstraZeneca, Boehringer Ingelheim, Sanofi, Asofarma, and Roche. Lluvia Marino Gabriel Cojuc-Konigsberg, Estefania Reul-Linares, Nathalie Desire Pichardo-Cabrera, Cristino Cruz, Elisa Naomi Hernández-Paredes, Nathan Berman-Parks, Vanesa Vidal Ruiz, Jonathan Mauricio Estrada Linares, and Alfredo A. Reza-Albarrán have no competing interest to declare.
Ethical approval
This study was approved by the local Human Research and Ethics Boards (NMM-4220-22-23-1) and adhered to the principles outlined in the 1964 Helsinki Declaration and its subsequent amendments.
Human and animal rights
This study does not contain any studies with animals performed by any of the authors.
Informed consent
Participants who underwent biomarker assessment provided informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ramirez-Sandoval, J.C., Marino, L., Cojuc-Konigsberg, G. et al. Long-term effects of hypercalcemia in kidney transplant recipients with persistent hyperparathyroidism. J Nephrol (2023). https://doi.org/10.1007/s40620-023-01815-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40620-023-01815-5