Abstract
Background
Thyroid cancer is one of the most common endocrine malignancies. Although the 10-year survival rate of differentiated thyroid cancer (DTC) is about 90% after conventional treatments, a small proportion of patients still suffer from tumor recurrence or drug resistance.
Objective
This review article summarizes recent researches and clinical trials related to target drugs that reduce mortality in thyroid cancer.
Methods
This is a review of the recent literature and clinical trials on the three main aspects including methylation genes in thyroid cancers, the relationship between BRAF mutation and gene methylation, target and dehypermethylation drugs in clinical trials.
Results
We propose new approaches to treating malignant thyroid cancer, based on advances in understanding the relationship between genetic and epigenetic changes in thyroid cancer. Although the effect of traditional treatment for thyroid cancer is relatively good, a small proportion of patients still suffer from tumor recurrence or drug resistance. Molecular targeted drugs and dehypermethylation drugs have more promising outcomes in aggressive thyroid cancer compared with conventional treatments.
Conclusion
Based on what was discussed in this review, we suggest that integration of epigenetic and targeted therapies into conventional treatments will reduce the occurrence of refractory radioiodine differentiated thyroid cancer and improve the outcomes in aggressive thyroid cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid cancer is the most common and a leading cause of death in endocrine malignancy [1, 2]. The conventional treatments of thyroid cancer include thyroidectomy, radioiodide therapy, and thyroid stimulating hormone (TSH) suppression treatment. Although the overall prognosis is relatively favorable, a small part of patients still suffer lymph-node metastasis, cancer recurrence, and drug resistance [3, 4].
Recent studies have found that epigenetic and genetic changes play important roles in thyroid cancer occurrence and progression [5]. In Pishkari’s review, they summarized miRNA dysregulation in different thyroid tumors; for instance, miR-146 was consistently and specifically overexpressed in papillary thyroid cancer (PTC), which could to distinguish PTC from other thyroid cancers. miR-221, miR-222, etc. are consistently overexpressed in follicular thyroid carcinoma (FTC). Their review suggested that miRNA could be a useful tool for a more accurate diagnosis of different types of thyroid cancers [6]. Many studies recognized that BRAF mutation play a vital role in thyroid cancer progression, moreover, among all gene mutations which accounts for 29–83% [7, 8]. Despite advances in gene targeting therapies, the development of inhibitors of mutant BRAF kinase, for example, as therapeutic agents, is stagnant due to resistance to the therapy. Many articles elucidate that a negative association between aberrant death-associated protein kinase (DAPK), SLC5A8, tissue inhibitor of metalloproteinase-3(TIMP3), thyroid stimulating hormone receptor (TSHR) methylations, and BRAF mutation. Their data suggested that aberrant methylation and consequent silencing of these genes may be an inducement in BRAF mutation-promoted tumorigenesis and progression of PTC [9,10,11,12]. DNA methylation alterations in promoter CPG island could regulate gene expression, maintain chromosome integrity, and control DNA recombination, etc. [13]. DNA methylations are heritable and reversible; it is speculated that target therapy may alter methylation status of genes to achieve the goal of tumor treatment which also explain for how environmental factors contribute to our individual phenotype and for susceptibilities to diseases like cancers, autoimmune diseases [14, 15]. Therefore, the study of DNA methylations has a great significance in pathogenesis, early diagnosis, and prognosis evaluation of cancer.
Growing evidence demonstrates that the role of DNA methylation is a vital component of cancer biology for regulating tumor progression. Methylation alterations have therapeutic potential in cancer management as they can be used as a prognostic biomarker or a therapeutic target [16,17,18]. In this review, the current methylation alternations investigated in thyroid cancer (TC) and their role as a therapeutic target will be discussed. Moreover, we will focus on the role of BRAF mutation and its relation to DNA methylations.
DNA methylations in thyroid cancer
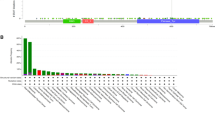
Aberrant methylations of tumor suppressor genes and thyroid-specific genes in thyroid tumors
DNA methylation is one of the most studied epigenetic modifications, which contributes to gene silencing. Members of the DNMT (including DNMT1, DNMT3A, DNMT3B, and DNMT3L) catalyze a methyl group (CH3) adding to 5′-carbon of cytosines [19]. As in other human tumors, aberrant methylations, which lead to inappropriate silencing of tumor suppressor genes, are widespread in thyroid tumors. Examples of these genes include RASSF1A, TIMP3, SLC5A8, DAPK, and retinoic acid receptor β2 (RARβ2) etc. [20] (Table 1). These tumor suppressor genes have well-established tumor-suppressing function through various mechanisms. It is, therefore, conceivable that silencing these genes through methylation could accelerate tumorigenesis and progression in thyroid cancer.
RASSF1A, the first member of Ras association domain family (RASSF), exert function as a negative regulator of cell proliferation through inhibiting G1/S-phase progression. The methylation frequency of RASSF1 in thyroid cancer patients is approximately 15–75%. Schagdarsurengin et al. [21] initially demonstrated that hypermethylation of RASSF1 stimulates tumor growth and the methylation frequency was higher in aggressive thyroid cancers compared with normal controls. A previous multicenter study demonstrated RASSF1A hypermethylation related to aggressive pathological features including lymph-node metastasis, invasion-to-adjacent tissues, and the volume of cancer increased [22]. Kunstman and his colleague [23] used MSP to detect the level of RASSF1 methylation in PTC, and then, they found the mean methylation level in PTC tissues was 8.9%, while 2.1% in normal tissues. Stephen et al. [24] discovered that RASSF1 was differentially methylated in classic tumor tissue compared with Hurthle cell cancer (p < 0.001). Thus, hypermethylation of RASSF1A may be an early event in pathogenesis of thyroid cancer and could be used as a biomarker for the early diagnosis.
Methylation of several tumor suppressor genes may promote tumorigenesis in PTC patients, including TIMP3, SLC5A8, and DAPK, as they are associated with poor pathological characteristics of PTC [20]. TIMP3 encodes a member of TIMP family molecules which inhibit the proteolytic activity of matrix metalloproteinases. Anania and his coworker [25] found that TIMP3 regulates migration and invasion, and promotes cancer onset in thyroid cancer. RARβ defined as potent regulators of epithelial cell growth and stimulate tumorigenesis. In treating metastatic or recurrent thyroid cancers, retinoic acid therapy can restore the iodine uptake ability and then improve the therapeutic effect of radioiodine therapy [26]. Phosphatase and tensin homologue deleted on chromosome 10 (PTEN) is a major negative regulator of the PI3K/Akt pathway. An epigenetic inactivating mechanism through aberrant methylation of PTEN gene exists in various thyroid tumors, particularly in FTC and anaplastic thyroid cancer (ATC) [27]. DAPK is a tumor suppressor protein. Abnormal expression of DAPK can block regular process of apoptosis and thus lead to tumorigenesis [28]. As their vital role in regulating cell proliferation, inhibiting the onset of tumors, many studies have enrolled them into the investigations regarding methylations in thyroid cancers. Hoque et al. used MSP to assess the methylation levels of RASSF1A, RARβ2, DAPK, and TIMP3 in thyroid cancer. Their study demonstrated that methylation-induced gene silencing appears to affect multiple genes in thyroid tissue and could be a useful tool for early diagnosis [29]. Mohammadi-asl [30] took P16, RASSF1A, and RARβ2 into study and then assessed their diagnostic and prognostic values in PTC; they found that combining the three genes together may be an useful molecular biomarkers in the early diagnosis. Their results interpreted potent utility of DNA methylation profiles to distinguish benign from malignant thyroid, which may contribute to enhance sensitivity and precision in the early diagnosis, also in the long-term aid in personalized clinical management and surveillance.
SLC5A8 is defined as a passive thyroid apical iodide transporter and Na+/short-chain fatty acid co-transporter; some studies noted that SLC5A8 is a tumor suppressor gene in colon cancer [31]. Although many studies have detected hypermethylation of SLC5A8 in thyroid cancer, the underlying mechanism of SLC5A8 hypermethylation which influences the occurrence of thyroid cancer is still unclear. Pora and his colleague [32] pointed out that SLC5A8 methylation was observed in 9 of 10 PTC while undetectable in the follicular adenoma (FA) samples. In addition, the low expression of SLC5A8 is correlated to BRAF V600E mutation, which suggested that SLC5A8 methylation stimulates carcinogenesis which may be through MAPK pathway.
Thyroid-specific genes including TSHR, TPO, NIS, TG, and so on, serve fundamental role in regulating thyroid cell proliferation, differentiation, and function, also in synthesizing and utilizing thyroid hormone. They are the basis for effective diagnosis, therapeutic management, of thyroid cancer, while their expressions are frequently decreased in ATC and then result in decreasing or absenting iodide uptake. Xing et al. [33] designed a trial to find the underlying molecular mechanisms of decreased expression of TSHR. Their result demonstrated that methylation of TSHR is responsible for silencing this gene. Some studies also detected methylation of NIS; for instance, Neumann and Galrao [34, 35] all found NIS hypermethylation in TC and hypomethylation in normal tissues. Galrao et al. [36] found a novel distal enhancer regulating the mRNA expression of NIS through DNA methylation which may be an early event in tumorigenesis.
DNA methylations are being novel research hotspots in recent years; many genes have been proposed using genome-wide methylation analysis, including WT1, EI24, STATs, and other signaling pathways. For example, T-cell receptor signaling pathway and Jak-Stat signaling pathway have been recognized [37, 38]. Methylation of these tumor suppressor genes in aggressive PTC provides strong evidence that methylation-induced silencing of these genes may contribute to PTC tumorigenesis; however, the underlying mechanisms of those genes and pathways are still unclear and need our efforts to clarify them.
BRAF mutation and its relationship to tumor suppressor and thyroid-specific genes methylation
BRAF mutation has been proved to be the most common genetic event in PTC onset, responsible for around 45% of adult cases, and causes constitutive activation of serine/threonine kinase [39, 40]. Several clinical studies suggested that BRAF mutation usually leads to aggressive clinicopathological characteristics and poor outcomes in PTC patients [41,42,43]. However, the molecular mechanisms involved in aggressive pathological characteristics of PTC bearing BRAF mutation are not clear. Recent studies of BRAF mutation and its relation to aberrant gene methylations in PTC seem to uncover this issue. These genes include RASSF1, TIMP3, SLC5A8, DAPK, and RARβ2 et al. (Table 2). BRAF mutation reduced the expression of thyroid-specific genes; for instance, NIS, TSHR, TG, and TPO expression was much lower in BRAF-mut tumor comparison with BRAF-wt group. This effect may alter the effectiveness of diagnostic or therapeutic use of radioiodine in BRAF-mut papillary thyroid cancer [44].
Xing et al. [45] first elaborated the inverse relationship between RASSF1 methylation and BRAF mutation. Their results demonstrated that the epigenetic alteration is the first step in oncogenesis and cancer progression. Many studies reported the association between aberrant DNA methylation profile and BRAF mutation in thyroid cancer. Hu et al. investigated the association between tumor suppressor genes methylation (TIMP3, SLC5A8, DAPK, and RARβ2) and aggressive clinicopathological characteristics and BRAF mutation in PTC. They first speculated that aberrant methylation of tumor suppressor genes may be an important step in BRAF mutation-induced aggressive PTC [46]. Hou et al. performed a genome-wide DNA methylation analysis to examine epigenetic mechanism involved in tumorigenesis of PTC stimulated by BRAF mutation. They revealed that BRAF V600E can promote PTC tumorigenesis by altering the metabolic and cellular functions of these genes through methylation [47]. Mosin et al. found that TSHR promoter methylation frequency is about 2.74-fold more in BRAF-mut patients compared with BRAF-wt patients, and depicted a positive connection between TSHR and MAP Kinase Pathway [48]. In Liu’s [49] study, they showed the restorability of the expression of iodide-metabolizing genes by suppressing BRAF/MAP kinase pathway which regulate iodide-metabolizing genes through aberrant methylation. Yong et al. later found that BRAF mutation inhibits NIS expression by upregulating the expression of DNA methyltransferase 1 which upregulate the methylation of NIS, thus leading to NIS gene silence. This is a potent mechanism involved in down-regulating NIS expression in PTC [50].
Although many molecular mechanisms about aberrant gene methylations linked to aggressive tumor characteristics and BRAF mutation in PTC patients have been proposed, the convincing evidence remains to be found. However, these results provide clinical implications such as preoperative diagnosis, therapeutic targets especially promising in conditions where BRAF V600E inhibitors failed due to drug resistance.
Target therapies for thyroid cancer
Although thyroid cancer is relatively indolent and has good prognosis, almost all ATC patients cannot uptake iodine, 10–20% DTC patients have aggressive features including metastasis, recurrence, and radioiodine refractory due to tumor dedifferentiation. Thus, the conventional treatments and chemotherapy such as thyroidectomy, radioiodine treatment, doxorubicin monotherapy, or doxorubicin combine with cisplatin, which have yielded low-treatment effect and associated with significant side effects [51]. Therefore, new targeted therapeutic methods are urgently needed. There have many different targeted therapies utilized in thyroid cancer (Table 3), some not showing any success but others demonstrating a significant amount of potential.
Sorafenibis, a multi-tyrosine inhibitor, which inhibits VEGFR1, VEGFR2, VEGFR3, RET, Flt3, c-KIT, and mutant BRAFV600E, has been accepted by FDA for radioiodine-resistant metastatic DTC [52]. From a systematic review, we obtained that the overall clinical benefit (PR and SD responses) was 93% for MTC (medullary thyroid carcinoma) and about 79% for DTC (differentiated thyroid carcinoma); more than 70% of patients suffered from hand–foot syndrome and diarrhea. What’s worse, sorafenib is a VEGF inhibitor which leads to cardiovascular toxicity [53]. Although treating progressive DTC or MTC patients with sorafenib is a promising method, the side effects are frequently occurred and leaded to dose reduction or discontinuation.
Clinical trials with non-selective BRAF inhibitor, sorafenib, demonstrated a limited clinical efficacy in dedifferentiated thyroid cancer when given as monotherapy as the non-selective nature of sorafenib [54]. Selective BRAF inhibitors have demonstrated promising results in clinical trials, such as vemurafenib [55] and dabrafenib in BRAF mutation-positive metastatic melanoma [56].
Vemurafenib is a selective BRAF kinase inhibitor and already adopted by FDA for the treatment of advanced-stage melanoma. In a first-in-human phase I study of vemurafenib, a total of 26 of the 32 melanoma patients harboring the BRAFV600E mutation had a response (81% of patients). It is particularly encouraging in light of the high disease burden in radioiodine refractory patients [57]. As the elucidated efficacy of selective BRAF inhibitor in melanoma, many articles devoted to evaluating the clinical effects in non-melanoma therioma with BRAFV600E mutation. Kim et al. completed the first phase I clinical trial in progressive, metastatic PTC bearing the BRAFV600E mutation. Although they found a promising clinical activity in patients with metastatic PTC, the main defect of this experiment is the small sample. A clear conclusion should be confirmed by a large sample and a large-scale randomized trial [58]. A multicenter phase II clinical trial enrolled patients who harboring BRAF mutation and refractory to radioiodine take vemurafenib orally twice daily. Although the clinical trial result showed vemurafenib has antitumor activity, result also showed about 38.5% of patients which have partial response, and the grade 3 or 4 adverse events occurred in 65% patients [59].
Vemurafenib has dramatically changed the therapeutic landscape, but the adverse effects such as fatigue, anorexia, and arthralgias, were 71, 65, and 59%, respectively. In Ramona’s retrospective review, the rates of adverse effects (AEs) requiring drug discontinuation, drug interruption, and dose reductions were 23, 73, and 23%, respectively [60].
Dabrafenib is a potent ATP-competitive selective inhibitor of BRAF kinase. Dabrafenib has been recognized a more selectively BRAF inhibitor compared with vemurafenib; therefore, dabrafenib was well tolerated, more mild, and manageable toxicity compared with vemurafenib. In a phase I clinical trial, dabrafenib demonstrated a promising clinical activity in Japanese thyroid patients with BRAF mutation but remain suffer AEs such as alopecia, pyrexia, arthralgia, and leukopenia [61]. There are also several clinical trials to test the ability of dabrafenib in treating patients with recurrent thyroid cancer or resensitize iodine-refractory PTC patients to radioactive iodine therapy (NCT01723202 and NCT10534897).
These results are quiet favorable; however, just like all inhibitors, resistance ultimately develops. Required resistance to BRAF mutation inhibition is a great therapeutic challenge in progressive thyroid cancer patients. Thus, identifying and understanding the underlying mechanisms that alleviate inhibitors resistance are significant to improve treatment effects. As we mentioned above, BRAF mutation leaded to aberrant gene methylation, and then resulted in thyroid-specific and tumor suppressor genes silencing; demethylating agents may reverse the malignant cell phenotype.
De-hypermethylation drugs
Methylation of DNA is catalyzed by a group of enzymes called DNA methyl transferases (DNMTs). Today, DNMTs inhibitors can be divided into two categories: one is nucleoside DNMT inhibitors, including azacitidine and decitabine; the other is non-nucleoside DNMT inhibitors, such as hydralazine, MG98, which are being investigated as demethylation drugs. However, up to date, only azacitidine and decitabine are approved only for treating myelodysplastic syndromes (MDS), not approved for treating solid tumor [62]. Indeed, it was reported that demethylating agent like decitabine is able to restore NIS and TSHR expression in human thyroid carcinoma cell lines [63].
Moreover, preclinical studies in thyroid patients harboring BRAF mutation showed that inhibiting the DNMTs can restore the expression of NIS while did not need knock-out BRAF mutation [64]. Furthermore, a preclinical studies in ATC cell lines indicated that treatment with DNMT inhibitor (decitabine) could upregulate the expression of MAGEA4 which is a potential target for T-cell receptor (TCR)-based immunotherapy [65], thus modifying the immune system which is a potential new function for demethylating agents that treat aggressive PTC patients. DNMT inhibitors are potent target therapeutic drugs; therefore, many clinical trials are designed to investigate the efficacy of azacitidine or decitabine in treating patients with metastatic PTC or FTC unresponsive to radioiodine.
A phase II clinical trial is studying how decitabine works in treating metastatic PTC or FTC patients who have stopped responding to radioiodine. This result demonstrated after decitabine administration presented restoration of radioiodine uptake in metastatic lesions (NCT00085293). Particularly, a phase I clinical trial designed to assess the efficacy of azacitidine to restore thyroid function in persistent or metastatic thyroid cancer patients. However, the results of this trial, whether azacitidine has the ability to restore iodine uptake enabling detection and treatment with radioiodine in patients or the efficacy of azacitidine plus radioiodine in this patient population, are not posted (NCT00004062). Although combined demethylation drugs and radioiodine has promising results, the side effects cannot be ignored and more clinical studies are urgently needed to avoid adverse effects.
Conclusion
Discoveries of the last decade have completely changed our view on genetics and epigenetic landscape of human thyroid cancers. High BRAF mutation expression, tumor suppressor genes, and thyroid-specific gene hypermethylation have been detected in aggressive thyroid tumor, particularly in advanced thyroid cancer. A majority of studies have demonstrated methylations and BRAF mutation has vital effects on thyroid cancer progression. Furthermore, there have been reported the alterations of epigenetic and genetic associated with thyroid cancer outcomes; increased BRAF mutation may result in local recurrence, metastasis, and invasion. Notably, BRAF mutation combines with gene methylation which may be considered as prognostic factors and novel therapeutic strategies.
Therefore, the pursuit for efficacious therapies to combat malignant thyroid cancer, especially in advanced, metastatic stage, is guaranteed to reduce mortality. Although the efficacy of the conventional treatments is limited in progressive patients, combining thyroidectomy, residual ablation, and TSH suppressive therapy together is still an avenue for improving the survival outcomes in indolent thyroid cancer patients.
In this review, we discussed the BRAF mutation and gene methylations in progressive thyroid cancer and then provided novel ideas for treating refractory thyroid cancer. In fact, because of these molecular findings, large numbers of drugs are being used clinically or under preclinical assessment, such as selective BRAF inhibitors and DMNT inhibitors.
In summary, using targeted therapies in preclinical trials against lethal thyroid cancer has shown to be a promising path for treatment in aggressive TC patients. Continuing studies that will be crucial to make deep genomic and epigenomic analyses as well as optimize combinatorial targeted therapy approaches in patients with aggressive TC will help to develop a precise medicine and decrease the currently dismal mortality rates.
References
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics. CA Cancer J Clin 63(1):11–30
Sipos J, Mazzaferri EL (2010) Thyroid cancer epidemiology and prognostic variables. Clin Oncol (R Coll Radiol) 22(6):395–404
Torre LA T, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65(2):87–108. https://doi.org/10.3322/caac.21262
Hundahl SA, Cady B, Cunningham MP, Mazzaferri E, McKee RF, Rosai J, Shah JP, Fremgen AM, Stewart AK, Hölzer S (2000) Initial results from a prospective cohort study of 5583 cases of thyroid carcinoma treated in the United States during 1996. US and German Thyroid Cancer Study Group. An American College of Surgeons Commission on Cancer Patient Care Evaluation study. Cancer 89(1):202–217
Cho BY, Choi HS, Park YJ (2013) Changes in the clinicopathological characteristics and outcomes of thyroid cancer in Korea over the past four decades. Thyroid 23(7):797–804
Pishkari S, Paryan M, Hashemi M, Baldini E, Mohammadi-Yeganeh S (2018) The role of microRNAs in different types of thyroid carcinoma: a comprehensive analysis to find new miRNA supplementary therapies. J Endocrinol Invest 41(3):269–283
Vu-Phan D, Koenig RJ (2014) Genetics and epigenetics of sporadic thyroid cancer. Mol Cell Endocrinol 386(1–2):55–66
Xing M (2005) BRAF mutation in thyroid cancer. Endocr Relat Cancer 12(2):245–262
Santos JC, Bastos AU, Cerutti JM et al (2013) Correlation of MLH1 and MGMT expression and promoter methylation with genomic instability in patients with thyroid carcinoma. BMC Cancer 13:79
Guan H, Ji M, Hou P et al (2008) Hypermethylation of the DNA mismatch repair Gene hMLH1 and its association with lymph node metastasis and T1799A BRAF mutation in patients with papillary thyroid cancer. Cancer 113(2):247–255
Zane M, Agostini M, Enzo MV et al (2013) Circulating cell-free DNA, SLC5A8 and SLC26A4 hypermethylation, BRAFV600E: a non-invasive tool panel for early detection of thyroid cancer. Biomed Pharmacother 67(8):723–730
Hu S, Liu D, Tufano RP et al (2006) Association of aberrant methylation of tumor suppressor genes with tumor aggressiveness and BRAF mutation in papillary thyroid cancer. Int J Cancer 119(10):2322–2329
Jones PA, Baylin SB (2002) The fundamental role of epigenetic events in cancer. Nat Rev Genet 3(6):415–428
Davis CD, Uthus EO (2004) DNA methylation, cancer susceptibility, and nutrient interactions. Exp Biol Med (Maywood) 229(10):988–995
Sun B, Hu L, Luo ZY et al (2016) DNA methylation perspectives in the pathogenesis of autoimmune diseases. Clin Immunol 164:21–27
Xing M (2007) Gene methylation in thyroid tumorigenesis. Endocrinology 148(3):948–953
Tang J, Xiong Y, Zhou HH, Chen XP (2014) DNA methylation and personalized medicine. J Clin Pharm Ther 39(6):621–627
Lv JF, Hu L, Zhuo W (2016) Epigenetic alternations and cancer chemotherapy response. Cancer Chemother Pharmacol 77(4):673–684
Ai S, Shen L, Guo J et al (2012) DNA methylation as a biomarker for neuropsychiatric diseases. Int J Neurosci 122(4):165–176
Liu MZ, McLeod HL, He FZ (2014) Epigenetic perspectives on cancer chemotherapy response. Pharmacogenomics 15(5):699–715
Stephen JK, Chen KM, Merritt J et al (2015) Methylation markers for early detection and differentiation of follicular thyroid cancer subtypes. Cancer Clin Oncol 4(2):1–12
Schagdarsurengin U, Gimm O, Hoang Vu et al (2002) Frequent epigenetic silencing of the CpG island promoter of RASSF1A in thyroid carcinoma. Cancer Res 62(13):3698–3701
Kunstman JW, Korah R, Healy JM (2013) Quantitative assessment of RASSF1A methylation as a putative molecular marker in papillary thyroid carcinoma. Surgery 154(6):1255–1261 (discussion 1261-2)
Stephen JK, Chen KM, Merritt J et al (2018) Methylation markers differentiate thyroid cancer from benign nodules. J Endocrinol Invest 41(2):163–170
Anania MC, Sensi M, Radaelli E et al (2011) TIMP3 regulates migration, invasion and in vivo tumorigenicity of thyroid tumor cells. Oncogene 30(27):3011–3023
Adamczewski Z, Makarewicz J, Mikosiński S et al (2006) Application of 13-cis-retinoic acid in patients with 131I scintigraphically negative metastases of differentiated thyroid carcinoma. Endokrynol Pol 57(4):403–406
Xing M (2010) Genetic alterations in the phosphatidylinositol-3Kinase/Akt pathway in thyroid cancer. Thyroid 20(7):697–706
Erol A (2012) Death-associated proliferation kinetic in normal and transformed cells. Cell Cycle 11(8):1512–1516
Hoque MO, Rosenbaum E, Westra WH et al (2005) Quantitative assessment of promoter methylation profiles in thyroid neoplasms. J Clin Endocrinol Metab 90(7):40118
Mohammadias J, Larijani B, Khorgami Z (2010) Qualitative and quantitative promoter hypermethylation patterns of the P16, TSHR, RASSF1A and RARb2 genes in papillary thyroid carcinoma. Med Oncol 28(4):1123–1128
Li H, Myeroff L, Smiraglia D et al (2003) SLC5A8, a sodium transporter, is a tumor suppressor gene silenced by methylation in human colon aberrant crypt foci and cancers. Proc Natl Acad Sci USA 100(14):8412–8417
Porra V, Ferraro-Peyret C, Durand C et al (2005) Silencing of the tumor suppressor gene SLC5A8 is associated with BRAF mutations in classical papillary thyroid carcinomas. J Clin Endocrinol Metab 90(5):3028–3035
Xing M, Usadel H, Cohen Y et al (2003) Methylation of the thyroid-stimulating hormone receptor gene in epithelial thyroid tumors: a marker of malignancy and a cause of gene silencing. Cancer Res 63(9):2316–2321
Neumann S, Schuchardt K, Reske A et al (2004) Lack of correlation for sodium iodide symporter mRNA and protein expression and analysis of sodium iodide symporter promoter methylation in benign cold thyroid nodules. Thyroid 14(2):99–111
Galrão AL, Sodré AK, Camargo RY et al (2013) Methylation levels of sodium–iodide symporter (NIS) promoter in benign and malignant thyroid tumors with reduced NIS expression. Endocrine 43:225–229
Galrão AL, Camargo RY, Friguglietti CU et al (2014) Hypermethylation of a new distal sodium/iodide symporter (NIS) enhancer (NDE) is associated with reduced nis expression in thyroid tumors. J Clin Endocrinol Metab 99(6):E944–E952
Mancikova V, Buj R, Castelblanco E et al (2014) DNA methylation profiling of well-differentiated thyroid cancer uncovers markers of recurrence free survival. Int J Cancer 135(3):598–610
Cai LL, Liu GY, Tzeng CM (2016) Genome-wide DNA methylation profiling and its involved molecular pathways from one individual with thyroid malignant/benign tumor and hyperplasia. Medicine (Baltimore) 95(35):e4695
Kimura ET, Nikiforova MN, Zhu Z et al (2003) High prevalence of BRAF mutations in thyroid cancer: genetic evidence for constitutive activation of the RET/PTC-RAS-BRAF signaling pathway in papillary thyroid carcinoma. Cancer Res 63:1454–1457
Ciampi R, Nikiforov YE (2005) Alterations of the BRAF gene in thyroid tumors. Endocr Pathol 16:163–172
Xing M, Westra WH, Tufano RP et al (2005) BRAF mutation predicts a poorer clinical prognosis for papillary thyroid cancer. J Clin Endocrinol Metab 90(12):6373–6379
Xing M, Alzahrani AS, Carson KA et al (2015) Association between BRAF V600E mutation and recurrence of papillary thyroid cancer. J Clin Oncol 33(1):42–50
Galuppini F, Pennelli G, Vianello F et al (2016) BRAF analysis before surgery for papillary thyroid carcinoma: correlation with clinico-pathological features and prognosis in a single-institution prospective experience. Clin Chem Lab Med 54(9):1531–1539
Durante C, Puxeddu E, Ferretti E et al (2007) BRAF mutations in papillary thyroid carcinomas inhibit genes involved in iodine metabolism. J Clin Endocrinol Metab 92(7):2840–2843
Xing M, Cohen Y, Mambo E et al (2004) Early occurrence of RASSF1A hypermethylation and its mutual exclusion with BRAF mutation in thyroid tumorigenesis. Cancer Res 64(5):1664–1668
Hu S, Liu D, Tufano RP et al (2006) Association of aberrant methylation of tumor suppressor genes with tumor aggressiveness and BRAF mutation in papillary thyroid cancer. Int J Cancer 119(10):2322–2329
Hou P, Liu D, Xing M (2011) Genome-wide alterations in gene methylation by the BRAF V600E mutation in papillary thyroid cancer cells. Endocr Relat Cancer 18(6):687–697
Khan MS, Pandith AA, Masoodi SR et al (2014) Epigenetic silencing of TSHR gene in thyroid cancer patients in relation to their BRAF V600E mutation status. Endocrine 47(2):449–455
Liu D, Hu S, Hou P et al (2007) Suppression of BRAF/MEK/MAP kinase pathway restores expression of iodide-metabolizing genes in thyroid cells expressing the V600E BRAF mutant. Clin Cancer Res 13(4):1341–1349
Choi YW, Kim HJ, Kim YH et al (2014) B-RafV600E inhibits sodium iodide symporter expression via regulation of DNA methyltransferase1. Exp Mol Med 46:e120
Schlumberger M, Sherman SI (2012) Approach to the patient with advanced differentiated thyroid cancer. Eur J Endocrinol 166(1):5–11
Hoftijzer H, Heemstra KA, Morreau H et al (2009) Beneficial effects of sorafenib on tumor progression, but not on radioiodine uptake, in patients with differentiated thyroid carcinoma. Eur J Endocrinol 161:923–931
Thomas L, Lai SY, Dong W et al (2014) Sorafenib in metastatic thyroid cancer: a systematic review. Oncologist 19(3):251–258
Ott PA, Hamilton A, Min C et al (2010) A phase II trial of sorafenib in metastatic melanoma with tissue correlates. PLoS One 5(12):e15588
Sosman JA, Kim KB, Schuchter L et al (2012) Survival in BRAF V600-mutant advanced melanoma treated with vemurafenib. N Engl J Med 366(8):707–714
Hauschild A, Grob JJ, Demidov LV et al (2012) Dabrafenib in BRAF-mutated metastatic melanoma: a multicentre, open-label, phase 3 randomised controlled trial. Lancet 380(9839):358–365
Flaherty KT, Puzanov I, Kim KB et al (2010) Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med 363(9):809–819
Kim KB, Cabanillas ME, Lazar AJ et al (2013) Clinical responses to vemurafenib in patients with metastatic papillary thyroid cancer harboring BRAF(V600E) mutation. Thyroid 23(10):1277–1283
Brose MS, Cabanillas ME, Cohen EE et al (2016) Vemurafenib in patients with BRAFV600E-positive metastatic or unresectable papillary thyroid cancer refractory to radioactive iodine: a non-randomised, multicentre, open-label, phase 2 trial. Lancet Oncol 17(9):1272–1282
Dadu R, Shah K, Busaidy NL et al (2015) Efficacy and tolerability of vemurafenib in patients with BRAF(V600E)-positive papillary thyroid cancer: M.D. Anderson Cancer Center off label experience. J Clin Endocrinol Metab 100(1):E77–E81
Fujiwara Y, Yamazaki N, Kiyohara Y et al (2018) Safety, tolerability, and pharmacokinetic profile of dabrafenib in Japanese patients with BRAF (V600) mutation-positive solid tumors: a phase 1 study. Invest New Drugs 36(2):259–268
Linnekamp JF, Butter R, Spijker R et al (2017) Clinical and biological effects of demethylating agents on solid tumours—a systematic review. Cancer Treat Rev 54:10–23
Provenzano MJ, Fitzgerald MP, Krager K et al (2007) Increased iodine uptake in thyroid carcinoma after treatment with sodium butyrate and decitabine (5-Aza-dC). Otolaryngol Head Neck Surg 137(5):722–728
Choi YW, Kim HJ, Kim YH et al (2014) B-RafV600E inhibits sodium iodide symporter expression via regulation of DNA methyltransferase 1. Exp Mol Med 46:e120
Gunda V, Cogdill AP, Bernasconi MJ et al (2013) Potential role of 5-aza-2-deoxycytidine induced MAGE-A4 expression in immunotherapy for anaplastic thyroid cancer. Surgery 154(6):1456–1462 (discussion 1462)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This manuscript is a review of the literature and does not contain original research either on animal or on human subjects.
Informed consent
For this type of study, informed consent is not required.
Rights and permissions
About this article
Cite this article
Zhang, K., Li, C., Liu, J. et al. DNA methylation alterations as therapeutic prospects in thyroid cancer. J Endocrinol Invest 42, 363–370 (2019). https://doi.org/10.1007/s40618-018-0922-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-018-0922-0