Abstract
Thyroid carcinoma (TC) is the most frequent malignant neoplasm of the endocrine system. Molecular methods for diagnosis of invasive thyroid disease can be effectively adopted. Epigenetic factors play an important role in the diversity patterns of gene expression and the phenotypic and biological characteristics of TC subtypes. We aimed to review epigenetic changes in the main subtypes of TC, along with a presentation of the methods that have examined these changes, and active clinical trials for the treatment of advanced TCs targeting epigenetic changes. A literature analysis was performed in MEDLINE using PubMed, Elsevier, and Google Scholar for studies published up to 2016, using the keywords: “Epigenetic alterations” OR “Epigenetic changes”, “thyroid cancers”, “papillary thyroid cancer”, “medullary thyroid cancer”, “follicular thyroid cancer”, and “anaplastic thyroid cancer”, which resulted in 310 articles in English. All related abstracts were reviewed and studies were included that were published in English, had available full text, and determined the details of the methods and materials associated with the epigenetic patterns of TC and its subtypes (100 articles). Analysis of epigenetic alterations in TC subtypes helps to identify pathogenesis and can play an important role in the classification and diagnosis of tumors. Epigenetic mechanisms, especially aberrant methylation of DNA and microRNAs (miRs), are likely to play an important role in thyroid tumorigenesis. Further studies are required to elucidate the role of histone modification mechanisms in TC development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Disorders in mitogen-activated protein kinase (MAPK) and phosphatidylinositol-3-kinase (PI3K-AKT) signaling pathways via DNA methylation and miRs regulation are the most common epigenetic modifications in well-differentiated thyroid carcinomas (TCs) [papillary TC and follicular TC]. |
Genome-wide analysis of DNA methylation patterns leads to the recognition of genes related to tumors with distinct subtypes and mutational status. |
Aberrant promoter hypomethylation occurs in undifferentiated subtypes (poorly differentiated TC [PDTC] and anaplastic TC) more than hypermethylation. |
Histone acetylation levels can change in thyroid cells by neoplastic transformation and hormonal stimulation. |
Deregulation of some miRs causes progression of PDTC and in medullary TC is probably an early event in C cell carcinogenesis. |
1 Introduction
Although thyroid carcinoma (TC) is quite a rare cancer, its incidence is increasing [1] and it is the most common endocrine malignancy, with about 1–5% of women and less than 2% of men affected worldwide. Thyroid cancers arising from follicular epithelial cells, which comprise about 95% of all thyroid tumors, have been categorized as (1) well-differentiated TC (WDTC), including both papillary TC (PTC; 80%) and follicular TC (FTC; 10–15%); (2) poorly differentiated TCs (PDTC; 0.5–7%); and (3) anaplastic TC (ATC; 1–2%) [2]. Medullary TC (MTC), a less common tumor among TCs, arises from parafollicular calcitonin-producing cells.
Generally, cancer as a genetic disease is caused by specific changes in genes that control cell function, especially their growth and division. Some common genetic alterations in TC and its subtypes consist of gene point mutations, copy-number changes, and translocations which dominantly occur in protein-coding genes involved in classical signaling pathways of cell proliferation and survival [3]. These pathways include mitogen-activated protein kinases (MAPK)/extracellular signal-regulated kinases (ERK), phosphatidylinositol-3-kinase (PI3K-AKT), nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), Ras association domain family member 1 (RASSF1)-macrophage stimulating 1 (MST1)-forkhead box O3 (FOXO3), WNT-β-catenin signaling pathway, hypoxia-inducible factor 1-α (HIF1a) pathway, and the thyroid-stimulating hormone receptor (TSHR) signaling pathway [3]; among these, two main pathways, the MAPK/ERK and the PI3K-AKT, play a remarkable role in TC pathogenesis [4]. The most effective molecular variations which disturb the aforementioned pathways have been identified and four of the well-known ones are in the R ET, BRAF, RAS, and paired box 8 (PAX8) genes [5]. The RET rearrangement is found in approximately 28.6% of TCs; BRAF mutation is found in 32.4% of PTC cases [6]; and the point mutation in RAS as a component of MAPK/ERK signaling pathway is frequently seen in cases of PDTC or ATC. RAS mutations occur in 20–50% of follicular cancers. Another chromosomal translocation including fusion of the promoter region of the PAX8 gene and the coding region of the peroxisome proliferator-activated receptor-γ (PPARγ) gene occurs in 35% of FTC cases [7].
Along with genetic variations, environmental factors are reported as a powerful determinant for cancer incidence, and mortality, lifestyle (diet and physical inactivity), and chemical exposure are the most important factors based on the literature [8]. Environmental factors have no effect on gene sequences and they exert their effects through rearrangement of gene expression. These alterations are known as epigenetic changes; different types of epigenetic alterations in TCs have been identified and their important role in the diversity patterns of gene expression and phenotypic and biological characteristics of TCs have been confirmed; understanding each of these changes could be vital before starting any therapeutic approach. In this review, we discuss briefly the mechanism of epigenetic modifications and their role in the pathogenesis of TC and its main subtypes along with a presentation of the methods that have been used to examine these changes. We also introduce some active clinical trials for the treatment of advanced TCs using epigenetic changes. Lastly, we deliberate on and clarify whether there is any difference in epigenetic mechanisms in TC subtypes or not?
2 Methods
2.1 Data Sources
A literature analysis was performed in MEDLINE using PubMed, Elsevier, and Google Scholar to search for studies published up to 2016, using the keywords: “Epigenetic alterations” OR “Epigenetic changes”, “thyroid cancers”, “papillary thyroid cancer”, “medullary thyroid cancer”, “follicular thyroid cancer”, and “anaplastic thyroid cancer”.
2.2 Study Selection
Using the keywords mentioned, 310 articles in English were obtained. All related abstracts were reviewed and studies were included that were published in English, had available full text, and determined the details of the methods and materials associated with the epigenetic patterns of TC and its subtypes (100 articles).
3 Results
3.1 Epigenetics of Thyroid Cancer Subtypes
3.1.1 Papillary Thyroid Carcinoma
PTC accounts for over 85–90% of thyroid malignancies [9]. With the advent of diagnostic techniques and molecular methods of detecting aggressive disease, the nature of PTC has been better elucidated in the last decade [10].
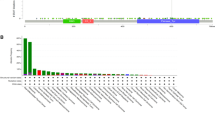
Recently, numerous investigations of epigenetic modifications in PTC have mainly focused on candidate tumor suppressor genes and genes known for their role in thyroid function. Numerous studies have assessed the DNA methylation status of several tumor suppressor genes (RAPβ2 [22%], SLC5A8 [33%], DAPK [34%], TIMP3 [53%], DKK3 [38.8%], DACT2 [64.6%], Mig-6 [79%], XAF1 [35.7%]) in the tissues from PTC patients and in the PTC cell lines [11,12,13,14,15,16]. Other studies results showed that ADAMTS8, HOXB4, ZIC1, KISS1R, INSL4, DPPA2, TCL1B, and NOTCH4 genes were frequently regulated by aberrant methylation in PTC and FTC [17]. Some investigations also showed that RASSF1 was methylated in 80, 78, 70, and 62% of MTC, undifferentiated TC (UDTC), FTC, and PTC, respectively [18], and p16 INK4A was methylated in 33, 44, 50, 75, 85, and 13% of follicular adenoma (FA), PTC, FTC, PDTC, UDTC, and non-tumorous tissue, respectively [19]. SLC26A4 was methylated in 44, 46, 71, 71, and 100% of BA, FTC, PTC, ATC, and cell lines, respectively, using DNA sequencing assays [20]. Moreover, Rap1GAP promoter region was methylated in 9–45% of PTCs [16] (Table 1). Mancikova et al. [21] performed a genome-wide DNA methylation profile in a large WDTC series including 83 tumor samples and eight normal adjacent tissues. They observed 89 hypermethylated CpGs (83 genes) in FA, 460 (416 genes) in FTC, and 39 (31 genes) in PTC, and found that follicular tumors had higher levels of methylation, which seemed to accumulate in a progressive manner along the tumorigenic process from adenomas to carcinomas [21]. In a study by Lee et al. [22], DNA methylation of MAPK signal-inhibiting genes was investigated. The results revealed that the Serpin family A member 5 (SERPINA5) promoter was methylated in 82.9% of PTC samples (n = 76). The methylation level was positively correlated with the presence of a BRAF mutation [22]. One of the most important translational contributions has been presented in the field of PTC in The Cancer Genome Atlas (TCGA) research project is the BRAF-like and RAS-like phenotypes. BRAF-like PTCs are mostly shown in classical structure of tumors such as classic and tall cell variants and mainly in PTCs with solid progress such as the RET/PTC-driven solid variant, while RAS-like PTCs are revealed in follicular-variant PTCs (FVPTCs) [23, 24]. In a large cohort of almost 496 PTCs, the PTC samples were subdivided into BRAF-like and RAS-like groups depending on the exome and RNA sequencing, proteomic profiles, and epigenetic changes in the analysis of the TCGA. Based on the DNA methylation levels, the investigators defined four groups, two of them improved by a H/K/N RAS-mutated FVPTC and two developed by BRAF-mutated classical and tall cell PTC. The TCGA classical/tall cell PTC-enriched cluster was distinct by the low levels of methylation in CpG normally methylated outside of islands by BRAF-mutated tumors. The authors indicated that BRAF-like PTCs specially activate the MAPK pathway, while RAS-like PTCs signal through MAPK in addition to the PI3K pathway [24]. In another study, Smith et al. [25] investigated DNA methylation using locus-specific non-quantitative methods in PTC samples including E-cadherin (ECAD), TSHR, BRAF, solute carrier family 5 member 8 (SLC5A8), R ASSFI, tissue inhibitor of metalloproteinases 3 (TIMP3), sodium/iodide symporter (NIS), death-associated protein kinase (DAPK), ataxia telangiectasia mutated (ATM), retinoid acid receptor β2 (RARβ2), apical iodide transporter (AIT), and MAPK signal-inhibiting genes. The results revealed promoter hypermethylation of TSHR, RARβ2, N IS-L, ATM, and ECAD in 34–59, 22, 22, 50, and 56% of patients with PTC, respectively [25]. Ellis et al. conducted a study of genome-wide methylation patterns in 51 PTC patients based on histological subtype and tumor genotype using advanced genome-wide methylation bead chips. They analyzed altered methylation patterns by stage, recurrence, histological subtype of tumor, and tumor genotype and demonstrated that PTC was globally hypomethylated compared with the normal thyroid, with 2837 differentially methylated CpG sites [26]. Ishida et al. [27] surveyed 39 lesions of PTC using quantitative methylation-specific polymerase chain reaction (qMSP) to assess hypermethylation in multiple genes implicated in regulatory processes such as p16 INK4a and p14 ARF, generated by the cyclin-dependent kinase inhibitor 2A (CDKN2A) gene; they suggested that hypermethylation in p16 INK4a may be linked to tumor growth but not to tumor development, while alterations in p14 ARF may contribute to the induction of chronic inflammation-related PTCs.
Studies of histone modifications associated with PTC are very limited. Recently, Brest et al. [28] reported that two inhibitors of histone deacetylation, trichostatin A and vorinostat, induced overexpression of miR-129-5p, histone acetylation, and apoptosis in cancer cell lines and primary cultures of ATC and PTC. The chromobox 7 (CBX7) gene encodes a protein of 28.4 kDa the level of which progressively decreased in proportion to the malignant grade and neoplasias stage [29]. To elucidate the function of CBX7 in thyroid carcinogenesis, Federico et al. [30] investigated the correlation between CBX7 protein and histone deacetylase 2 (HDAC2) using a proteomic analysis. They confirmed that CBX7 interacts with the HDAC2 protein and is able to inhibit its activity. Moreover, they indicated that both these proteins bind to the ECAD promoter and that CBX7 upregulates ECAD expression; they showed that the expression of CBX7 increased the acetylation status of the histones H3 and H4 on the ECAD promoter [30]. Histone acetylation increased at the NIS promoter in human thyroid cancer cells harboring a homozygous BRAF V600E mutation and suggesting that BRAF V600E normally maintains histone in a deacetylated state at the NIS promoter [31] (Table 2).
Many studies have been conducted to identify the regulation of miRs in PTC and their target genes; it was shown that miR-221 and -222 reduced the P27 expression in the protein levels, miR-146a decreased PKCɛ expression and increased apoptosis, downregulation of miR-181b caused the upregulation of cylindromatosis (CYLD) at the protein levels, and miR-195 directly regulated ZNF367 expression and regulated cellular invasion [32,33,34,35] (Table 3). Cahill et al. [36] investigated the effect of BRAF V600E mutation on transcription and post-transcriptional regulation in PTC by measuring the expression levels of 160 miRs in a set of cell lines using Stem-looped TaqMan™ reverse transcription PCR (RT-PCR). They indicated that 15 miRs were detected to be upregulated and 23 miRs were downregulated. Of these, miR-200a, -200b, and -141 were upregulated and miR-127, -130a, and -144 were downregulated. Moreover, miR-323 and -302b in the BRAF-mutated cell line were downregulated [36]. Song et al. [37] investigated the biological role of miR-96 in PTC cell lines K1 and two pore segment channel 1 (TPC1) and found miR-96 to be upregulated in PTC specimens in comparison to normal tissues by miRs microarray and quantitative RT-PCR analysis. In addition, forkhead box O1 (FOXO1), which plays a role in myogenic growth and differentiation, may be a potential target of miR-96. The expression of FOXO1 had an inverse correlation with expression of miR-96 in PTC specimens, suggesting that miR-96 could promote proliferation and inhibit apoptosis in PTC cell lines and thus may play an oncogenic role in PTC [37]. Dual specificity phosphatase 6 (DUSP6) negatively regulates members of the MAPK superfamily (MAPK/ERK, stress-activated protein kinases/c-Jun N-terminal protein kinases (SAPKs/JNKs), p38). In their study, Gu et al. [38] examined the expression of miR-145 in human PTC and its potential function and found that the overexpression of miR-145 inhibited TPC1 cellular growth by targeting DUSP6 [38]. In another study, with the aim of identifying a subset of differentially expressed miRs between aggressive and non-aggressive PTC, Yip et al. [39] used the miRs array to report that miR-146b, -221, -222, -155, and -31 were upregulated and miR-1, -34b, -130b, and -138 were downregulated [39]. Cahill et al. [40], using microarray analysis in ten pairs of PTC specimens, revealed a group of genes differentially expressed between normal thyroid cell lines and those harboring a RET/PTC1 rearrangement; they showed that 21 miRs overexpressed and 14 underexpressed in these cell lines when compared to the normal thyroid. Microarray analysis of PTC showed that several genes were directly or indirectly regulated by the miR-221 and the use of a bioluminescence imaging system confirmed downregulation of homeobox B5 (HOXB5) by endogenous or exogenous miR-221 [41]. Pallante et al. [42], using significance analysis of microarrays (SAM), reported that miR-221, -222, and -146b were overexpressed and led to their target tyrosine-protein kinase kit (KIT) gene being downregulated; this gene encodes the human homolog of the proto-oncogene c-kit and is a type 3 transmembrane receptor for mast cell growth factor (MGF) [42]. Similarly, other lines of evidence have also identified the roles of miR-221, -222, and -181b overexpression in thyroid cell transformation and the contribution of miR-146b to tumor aggressiveness in PTC. MiR-221, -222, and -146 have high transcriptional regulation in PTC compared to normal tissues [43]. With the upregulation of these miRs, transcription of the KIT gene, which plays a role in the pathogenesis of TC, was decreased. However, there is a lack of data on the PTC pathogenesis, indicating the need for further studies of miR networks in PTC.
3.1.2 Follicular Thyroid Carcinoma
FTC classically accounts for 10–32% of thyroid malignancies. Traditionally, FTC has been classified as minimally invasive (MI-FTC) and widely invasive (WI-FTC) [44]. In the clinical setting, FTC poses a special diagnostic challenge due to the morphological and molecular similarities to the benign FA. Although different molecular profiles have been proposed to improve preoperative diagnosis, the accurate preoperative diagnosis of FTC, especially MI-FTC, continues to be a challenge.
A group of FTC is associated with the RAS gene mutation, whereas the RAS mutation-negative FTC group often features gene rearrangements of PPARγ, most commonly the PAX8-PPARγ fusion. RAS and PAX-PPARγ together explain up to 80% of FTC cases [45]. The tumor-suppressive RAS effector, RASSF1A, one of the two major isoforms of the putative tumor suppressor gene RASSF1, contain a RAS association domain, and plays a role in the regulation of cell cycle and apoptosis [46]. Stephen et al. [47] examined the promoter methylation status of the Caspase 8 (CASP8), CDKN2A, death associated protein kinase 1 (DAPK1), estrogen receptor 1 (ESR1), NIS, RASSF1, and TIMP3 genes in a cohort of FTCs including 26 Hurthle and 27 Classic subtypes using qMSP; they found that RASSF1 was significantly methylated in classic tumor tissue as compared to Hurthle. Moreover, extra thyroidal extension was found to be associated with DAPK1 and ESR1 methylation, suggesting that the methylation status of RASSF1, DAPK1, and ESR1 might molecularly distinguish the TC subtypes and enhance classification and early detection of TC [47]. Besides, no-expression of a tumor-suppressor gene, phosphatase and tensin homolog (PTEN), a phosphatase that blocks the PI3K/AKT signaling pathway, has also been implicated in the development of FTC. The detection of PTEN promoter hypermethylation in about 50% of PTCs and almost 100% of FTCs suggests that it might be involved in the thyroid tumorigenesis [48]. Moreover, some studies showed that hypermethylation of the TRβ gene was evaluated in 34, 81, 25, and 30% of PTCs, FTCs, follicular thyroid adenomas (FTAs), and thyroid tumor cell lines, respectively. The expression level of the T HRB gene was repressed by hypermethylation of the THRB promoter in TCs. Furthermore, TSHR gene promoter was methylated in 59 and 47% of PTC and FTC, respectively [49,50,51] (Table 1).
In various tumor types, the levels of acetylation at several histone residues are associated with clinical aggressiveness [52, 53]. However, information on histone modification in FTC is quite limited.
Several reports have addressed dysregulated miRs expression in FTC and it has been suggested that miRs analysis might help distinguish FTC from FTA. Colamaio et al. [54] recently assessed the expression of miR-142-3p in a large panel of FTA and FTC and evaluated its effect on thyroid cell proliferation and target expression by qRT-PCR; they observed that miR-142-3p is downregulated in FTAs, FTCs, and FVPTC. Moreover, this miR was able to downregulate the expression of absent, small, or homeotic-like (ASH1L) and mixed-lineage leukemia 1 (MLL1) genes by direct and indirect mechanisms, respectively. It has been demonstrated that downregulation of miR-142-3p has a role in thyroid tumorigenesis by regulating ASH1L and MLL1 [54]. In 2006, Weber et al. [55] investigated expression of miRs and their target genes. Four miRs (miR-192, -197, -328, and -346) were overexpressed in FTCs compared to FAs (Table 3). Nikiforova et al. [56] compared miRs expression profiles in 60 surgically removed thyroid neoplastic and non-neoplastic samples and in 62 fine-needle aspiration (FNA) samples by RT-PCR using the TaqMan™ MicroRNA Panel. They found a distinctive expression pattern associated with FTC: miR-155, -187, -221, -222, and -224 resulted in being highly overexpressed in conventional FTCs, while miR-183, -187, -197, -221, -222, and -339 were overexpressed in the FTC oncocytic variants [56]. Wojtas et al. [57] conducted a miR-microarray study to identify miRs differentially expressed between FTCs and their surrounding tissues, and revealed that miR-146b, -183, and -221 were upregulated, whereas miR-199b was downregulated in FTCs. They also studied the influence of these miRs on cell proliferation, cell cycle, apoptosis, and migration in some FTC cell lines, and functional characterization suggested an impact of miR-183 and -146b in FTC development. Furthermore, overexpression of miR-183 significantly repressed apoptosis. MiR-199b and -221 had no significant effects on proliferation, cell cycle, apoptosis, or migration in cell lines. It seemed that miR-146b and -183 might influence FTC development through the induction inhibition of migration and apoptosis [57]. Jikuzono et al. [58] conducted another study on 34 patients with MI-FTC through an extensive analysis of miR expression, and results indicated that miR-221/222, -10b, and -92a profiles in MI-FTC significantly increased metastasis. Despite much progress over recent years, there is still a need for clarification of the molecular and biological relationship of the different benign thyroid neoplasias to each other and to TCs, in particular FTC.
3.1.3 Poorly Differentiated Thyroid Carcinoma
The prevalence of PDTC is about 0.5–7% of all TCs and the mean age of diagnosis is around 60.6 years [59]. PDTC shows intermediate aggressive clinical features between WDTC and ATC [60, 61]. With the advent of genetic/epigenetic analysis, epigenome data on PDTCs are lacking. Further, some dysregulated gene expressions associated with epigenetic modifications are grouped based on their implicated roles in the overall dedifferentiation process in PDTCs [62, 63]. Currently, treatment for PDTC is still challenging and surgery is a current therapeutic choice.
Ogasawara et al. [64] investigated the methylation status of the promoter region of SERPINB5 (serine [or cysteine] proteinase inhibitor, clade B [Ovalbumin], member 5), a mammary serine protease inhibitor (Maspin), in six human ATC cell lines, 17 PDTCs, and 13 ATCs [64]. They found promoter hypomethylation in 41% of PDTCs and 62% of ATCs. Moreover, some investigations indicated the RASSF1 and p16 INK4A methylation status in PDTC [18, 19], which is presented in Table 1.
Studies on histone methyltransferases (HMTs) in PDTCs are very limited; however, recent transcriptome analysis showed that expression of HMTs (lysine methyltransferase 2A (KMT2A), KMT2C, KMT2D, and SET domain containing 2 (SETD2)) was increased more in ATC than in PDTC [65].
Although numerous dysregulated miRs and their target genes have been identified in TCs, very few were found in PDTCs. To date, some miRs such as miR-23, -26a, -125b, -130b, -139-5p, -150, -193a-5p, -219-5p, -451, -455-3p, -886-3p, let7c have been found to be downregulated and others such as miR-15a-3p, -125a-5p, -129, -146b, -182, -183, -187, -221, -222, -339 upregulated in PDTC [56, 66,67,68,69,70].
3.1.4 Anaplastic Thyroid Carcinoma
Compared to other TCs, ATC is the least common but the most aggressive cancer with a median survival rate of 3–5 months. It is thought to develop from existing PTC and FTC, has an extremely high proliferative rate, and can quickly invade neck structures and metastasize to other organs; more importantly, it is resistant to radioiodine treatment [71].
The gene expression patterns of ATC are more complex and not very distinct. There have been a multitude of genetic alterations associated with ATC, very often causing dysfunction in the ERK1/2-MEK1/2 and PI3K-AKT signaling pathways [72]. Keller et al. [73] investigated whether the methylation status of the galectin-3 gene is a candidate molecular marker for thyroid malignancy; to do this they examined the methylation state of a large genomic region encompassing the galectin-3 transcriptional start site in 50 patients, including five normal thyroid, three goiter, 39 PTC, and three ATC cases utilizing high-resolution melt (HRM) analyses. Results showed that five CpGs were differentially methylated among the samples, suggesting that the average methylation state of the five CpGs clearly distinguished cancer from the non-neoplastic thyroid tissues [73]. Hou et al. [74] examined PTEN methylation and its relationship with genetic alterations in the PI3K/AKT pathway in various types of thyroid tumors using q MSP. They found that PTEN methylation was progressively higher from benign thyroid adenoma to FTC and to aggressive ATC, which harbored activating genetic alterations in the PI3K/AKT pathway corresponding to a progressively higher prevalence. The association of PTEN methylation was seen with phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA) alterations and RAS mutations in the PI3K/AKT pathway, within each of the three types of thyroid tumors; in contrast, they found no such a relationship for the tumor suppressor gene RASSF1A [74]. Genome-wide promoter methylation status indicated that hypomethylated genes (280 in ATC and 393 in MTC) were more than aberrantly hypermethylated genes (86 in ATC and 131 in MTC) [17]. It seems that thyroid transcription factor-1 (TTF-1) is a homeodomain containing transcriptional factor identified in thyroid, and DNA methylation of this gene was shown in 60% of the undifferentiated carcinomas (UCs) and 50% of the cell lines [75] (Table 1).
Studies on the associations between histone modifications and ATC are very limited; however, Borbone et al. [76] showed that EZH2 directly contributed to transcriptional silencing of the PAX8 gene and differentiation in ATC tissues. Moreover, in another study, they found that HDACs 1 and 2 overexpressed in ATCs compared with normal cells or benign tumors [77]. Smith et al. [78] found that histone methylation was increased to alter the expression of p16 INK4A, DAPK, ubiquitin C-terminal hydrolase L1 (UCHL1), O-6-methylguanine-DNA methyltransferase (MGMT), TSHR, PTEN, and melanoma antigen gene (MAGE) family member A4 (MAGE-A4) genes in ATC cell lines [78]. Kondo et al. [75] demonstrated that acetylation of H3-lys9 was positively correlated with TTF-1 expression in TC cells. A study on the protein levels of HDACs 1, 2, and 3 showed that HDACs 1 and 2 upregulated in ATCs compared to benign tumors and HDAC inhibitors induced apoptosis [75]. Moreover, another study indicated that an acetylated level of H3K9–K14ac was significantly higher in FA, PTC, FTC, and UC than in normal tissues and the level of H4K12 acetylation was higher in thyroid adenoma than in TCs [79]. Also, oncoproteins RET/PTC, RAS, and BRAF increased levels of H3K9–K14 and H3K18 acetylation [75] (Table 2).
In addition, miRs also can alter the gene expression of ATC cells by targeting expression of essential genes. Investigations have indicated that miR-20a significantly inhibited TC cell proliferation and invasion and targeted the LIMK1 gene. MiR-618 inhibited ATC by suppressing the XIAP gene in ATC cells. Moreover, overexpression of miR-145 inhibited the PI3K/AKT pathway and directly targeted AKT3 [80,81,82,83] (Table 3). Recently, Fuziwara et al. [84] showed that a new group of miRs, such as miR-146b, -221, and -222, were upregulated in ATC and also in PTC and FTC, indicating that the overexpression of these miRs was essential in maintaining tumorigenesis. On the other hand, they mentioned that some specific miRs, such as those of the miR-200 and -30 families, were downregulated in ATC; these are important negative regulators of cell migration, invasion, and epithelial-to-mesenchymal transition (EMT), processes that are over-activated in ATC [84]. Esposito et al. [85] reported that miR-30d is significantly downregulated in human ATC, and this is believed to be an important event in thyroid cell transformation. Additionally, Zhang et al. [86] demonstrated that miR-30d has a critical role in modulating the sensitivity of ATC cells to cisplatin; they also showed that miR-30d could negatively regulate the expression of beclin 1 (BECN1) and lead to suppression of the cisplatin-activated autophagic response that protects ATC cells from apoptosis, suggesting that miR-30d might be exploited as a potential target for therapeutic intervention in the treatment of ATC [86].
3.1.5 Medullary Thyroid Carcinoma
MTC, which arising from parafollicular C cells, encompasses about 3–10% of all TCs, and occurs in both familial and sporadic forms. Approximately 20% of patients develop distant metastases, which makes MTC an incurable disease, responsible for up to 13.4% of all TC mortality [87]. The RAS–RAF–MEK–MAPK–ERK and PI3K–AKT–mTOR (mammalian target of rapamycin) pathways are the most important signaling pathways in MTC and play a crucial role in vital cell processes such as cell survival, growth, proliferation, and differentiation [88, 89]. Through these pathways the product of the RET oncogene plays an essential role in cell survival, proliferation, and apoptosis. Thus, mutations in RET are considered to be an important factors in the diagnosis and treatment of MTC. Mutations of the RET gene can be inherited and are observed in virtually all patients who develop MTC; in addition, somatic mutations have been detected in sporadic cases of the disease [90,91,92,93,94,95].
Schagdarsurengin et al. [96] evaluated the DNA methylation pattern of 17 tumor-related genes in TC cell lines, primary tumors (PTC, FTC, UTC, and MTC), FA, and goiters using MSP and validated by expression analysis. Their results showed that three of these genes, RASSF1A (83%), TSHR (33%), and ERβ (20%), were methylated in MTC [96].
Although histone modifications have been described in various malignancies, there are not enough data on the pattern of expression of epigenetic regulators in MTCs and their relationship with the genotype and phenotype of the tumors. Sponziello et al. [97] revealed the expression profile of more aggressive disease with increased levels of Enhancer of zeste 2 polycomb repressive complex 2 subunit (EZH2) and SET and myeloid, Nervy, and deformed epidermal autoregulatory factor-1 (MYND) domain containing 3 (SMYD3) gene expression, which did not correlate with the mutational status of RET or RAS genes. Thus, messenger RNA (mRNA) expression of HMT EZH2 and SMYD3 may demonstrate useful prognostic biomarkers, modifying the most appropriate follow-up and timing of therapeutic approaches in MTC [97].
Recently published data provide important information on miRs regulation in MTC and on their target genes; NCOR2 and MDM4 were validated as direct targets of miR-10a/b and YAP1 and SLC16a2 were downregulated by miR-375 in MTC compared with non-tumor thyroid tissues [98] (Table 3). Pallante et al. [67] summarized the main alterations in miRs expression that have been identified in thyroid neoplasias, and reported that miR-323, -370, -129, -137, -10a, -124a, -224, -127, -9, -154, -183, -375, and -21 were upregulated and, conversely, miR-9 was downregulated in MTC [67]. Mian et al. [99] investigated dysregulation of miRs in heredity and sporadic MTC patients to determine the relationship between miR profiles and outcomes in MTC; they found significant overexpression of several miRs, including miR-127, -154, -224, -323, -370, -183, -375, and -9, in MTC samples. Furthermore, recently, Duan et al. [100] suggested an important role of non-coding RNAs in related to the incidence of MTC. They showed that miR-129-5p reduced cell growth, induced apoptosis, and inhibited cell migration ability in MTC, by reducing the phosphorylation of AKT. Downregulation of these molecules has been observed in MTC [100].
3.2 Utility of Epigenetics in Thyroid Cancer
Most therapies target specific genes, proteins, or the tissues that contribute to cancer growth and survival, and act selectively on cancer cells with a particular genetic dysfunction. These potential treatments are under assessment for clinical application in aggressive TC [101]. In addition, researchers are looking for new combinations of chemotherapy and other treatments.
Epigenetic therapy is being studied in order to stimulate genes irregularly silenced in cancer by epigenetic mechanisms and to reverse epigenetic alterations, and as such it may soon emerge for clinical use in patients with advanced TCs. Epigenetic drugs mainly target two mechanisms of epigenetic modifications, acetylation and DNA methylation, which control transformed cells’ differentiation and proliferation. The role of HDAC inhibitors has been assessed in numerous hematologic malignancies and solid tumors involving TC in clinical trials sponsored by the National Cancer Institute (NCI) [102] (Table 4). Some of these agents exert their effect via activation of proapoptopic signaling, while others, such as radioactive iodine (I-131), are being used in combination with conventional chemotherapy drugs [103]. Studies have shown that deacetylation inhibitors and demethylating agents are suitable in the treatment of TCs; some of these drugs have been examined in metastatic radioiodine-refractory advanced TC and the lists of these drugs have been reported [104, 105]. Numerous clinical trials using drugs with an epigenetic mode of action, including romidepsin, belinostat, vorinostat, panobinostat, valproic acid, and decitabine, have been completed (http://www.clinicaltrials.gov) (Table 4).
Romidepsin (depsipeptide) is currently used to treat cutaneous T cell lymphoma (CTCL) in subjects who have been treated with at least one other medication. It is a cyclic peptide that inhibits HDAC activity. There are currently two clinical studies ongoing at the NCI: the first is a phase I trial of romidepsin in patients with the thyroid neoplasms and other advanced cancers, testing safety and tolerability; the second is a phase II trial in radioiodine-refractory metastatic non-medullary TCs (stage IV FTC and PTC, recurrent TC, and Hurthle cell variants) to determine the anti-tumor activity of the drug.
Belinostat is used to treat peripheral T cell lymphoma that has not improved or has returned after treatment with other medications. There are currently two phase I clinical trials underway at the NCI, one is looking at advanced solid tumors and the other one solid tumors and lymphoma.
Vorinostat (suberoylanilide hydroxamic (SAHA)) is a hydroxamic acid that binds directly to the HDAC catalytic site and inhibits deacetylase enzymatic activity. A phase II study was completed in patients with insular TC, recurrence TC, stage II/IV FTC and PTC, and MTC. As a result of no complete or partial responses in these patients, vorinostat was not approved for treatment of advanced TCs [106].
Panobinostat (LBH589), which is used to treat multiple myeloma, is a hydroxamic acid with potent inhibitory activity. In vitro treatment of three ATC cell lines (BHT-101, CAL-62, and 8305C) with panobinostat resulted in impairment of cell viability, inhibition of colony formation, cell cycle arrest, and apoptosis induction [107]. A phase II trial of panobinostat was completed in patients with metastatic MTC and radioactive iodine-resistant DTC. There are currently no reported results for this trial.
Valproic acid is a short-chain fatty acid with anticonvulsant properties that is used in the treatment of epilepsy. The mechanism of its therapeutic activity is not well understood, although it may act by increasing the γ-aminobutyric acid level in the brain or by altering the properties of voltage-dependent sodium channels [108]. However, deacetylase inhibitors (DCI) activity, anti-proliferation, and pro-differentiation in various solid tumors has been reported [109, 110]. Two trials using valproic acid have been completed. A phase II study in patients with advanced TCs of follicular origin were treated with liothyronine sodium agent, however, according to the response evaluation criteria in solid tumors (RECIST), no partial or complete response was shown and valproic acid had an effect on radioiodine uptake in these patients [111]. Another phase II in patients was conducted in thyroglobulin positive/radioiodine unresponsive patients with advanced TCs of follicular origin; currently, no data are available on the results of this trial.
Decitabine, or 5-aza-2′-deoxycytidine, is a cytidine antimetabolite analog with potential antineoplastic activity. Decitabine acts as a nucleic acid synthesis inhibitor and inhibits DNA methyltransferase, causing hypomethylation of DNA and intra-S-phase arrest of DNA replication [112]. A phase II trial of decitabine has been completed in patients with metastatic PTC or FTC (stages IVA, IVB, and IVC) who are unresponsive to radioiodine, but no results of this trial are available to date.
Research on epigenetic modifications in TCs must continue, but hopefully once the final results of these trials become available, we may have more effective treatments for these tumors. On the other hand, using miRs for treatment of cancers, as both a target and a tool, could be a new interesting and promising therapy; however, although several preclinical studies underline this possibility, no clinical trial has yet been undertaken.
4 Discussion
During the two last decades, the incidence of TC and its subtypes has increased, which is attributed to the genetic and environmental changes that create epigenetic modifications. Based on the evidence presented in this review considerable epigenetic changes in TC subtypes have been identified and more are being studied. Of these, most of have focused on follicular cell-derived carcinomas of the thyroid gland and WDTCs because of their prevalence and the availability of samples. Based on the studies’ results, epigenetic mechanisms, especially aberrant DNA methylation and regulation of miRs, are suggested to play an important role in thyroid tumorigenesis [113, 114]. It seems that a general analysis of epigenetic alterations in TC subtypes is critical to understanding the relationship between these changes and gene regulation, and how this will contribute to, and inform, diagnosis, prognosis, and also the development of new therapeutic strategies.
The molecular basis for disease progression from WDTC to PDTC and/or ATC is debatable. WDTCs commonly demonstrate disturbed action of the MAPK and PI3K-AKT signaling pathways, or a compounding of the two [3]. These alterations occur via direct genomic/epigenomic mutations or indirectly via epigenetic deregulation. The overlap of dysregulated signaling pathways among these objects may support a concatenation of PDTC and ATC from WDTC [115]. Similarly, between WDTCs and PDTC/ATC there is the observation that the dysfunctions identified in the ERK1/2-MEK1/2 and PI3K-AKT signaling pathways are due to common genetic alterations, such as BRAF V600E [72, 116]. Downregulation of the MAPK signal-inhibiting genes may be regulated by DNA methylation, which was associated with a higher BRAF mutation rate in PTC [36, 117]. BRAF V600E can promote PTC tumorigenesis by altering the methylation, and hence the expression, of numerous important genes [118].
Generally, cell organization can be affected at three levels by epigenetic mechanisms: (1) direct regulation of the gene function (switching it on or off) or modulation of synthesis of specific proteins; (2) regulation of the topographic distribution and functions of proteins; and (3) regulation of cell differentiation by alteration of RNA translation into proteins [119].
DNA methylation may result in downregulation of tumor suppressor genes and overexpression of oncogenes. In the literature, most cases in which DNA methylation was investigated were considered using analysis in the candidate genes promoter region [7, 16, 64]. Genome-wide characterization of DNA methylation patterns of WDTCs shows that tumors with distinct subtypes and mutational status have unique methylation profiles, offering insight into the biology underlying the heterogeneity and differential outcomes of the TCs [21, 26, 61, 118]. The prevalence of DNA methylation is different in TC subtypes; tumor suppressor genes silencing via this mechanism are most common in WDTCs while the frequencies of oncogene overexpression and activation are significantly higher in MTC, ATC, and PDTCs (Table 1). As ATC is the most aggressive subtype of TCs, it seems that the overexpression of oncogenes through their promoter methylation in the thyroid gland has the most adverse effects on thyroid tumorigenesis and this alteration may direct thyrocytes toward undifferentiated subtypes [120]. In addition, it is suggested that TC subtypes present differential promoter methylation signatures, and undifferentiated subtypes are characterized by aberrant promoter hypomethylation rather than hypermethylation [17]. Overall, systematic analysis of global methylation of tumors is likely to identify signaling pathways that lead to the development of cancer. DNA methylation is involved in WDTC development and has led to the identification of novel markers such as etoposide induced 2.4 (EI24) and Wilms Tumor 1 (WT1) which are associated with recurrence-free survival [21].
Most of the studies reviewed here have focused on histone modifications performed on different TC cell lines (Table 2). According to these findings, histone modifications occur in all subtypes of TC. However, due to the low number of studies and their small sample size, the data obtained on histone modifications cannot be generalized to the TC patients and more studies are required to confirm the relationship between these alterations and different TC subtypes. Nevertheless, data showed that treatment with HDAC inhibitors impaired Rap2 activity in both differentiated and anaplastic tumor cell lines [16]. HDAC inhibitors may provide a tractable approach to impair Rap activity in human tumor cells [121]. Neoplastic transformation and hormonal stimulation can modify levels of histone acetylation in thyroid cells.
Gene regulation by miRs is another important epigenetic modification in TC subtypes that has recently drawn researchers’ attention. Study results suggest that the level of miR-222, -221, and -146a were significantly higher in PTC and non-toxic multinodular goiter (NMG) samples, and these molecules have been introduced as recurrence biomarkers in PTC [32, 33, 43]. In the FTC subtype, significant overexpression of miR-197 and -346 in FTC cell lines shows that a combination of FNA results with miR panels will result in an improvement in the discrimination between FTC and FA [55, 56]. Moreover, in PTC, miR-145, a master regulator of TC growth that mediates its effect via the PI3K/AKT pathway, may serve as an adjunct biomarker for PTC diagnosis [38, 82]. Analysis of distinct sets of miRs represents a useful tool to distinguish PDTC from pure PTC [69]. Additionally, the lack of deregulation of some miRs may select a subset of PTC prone to progression to PDTC. Downregulation of miR-20a and -618 shows that these molecules may play an important role as tumor-suppressor miRs in ATC [81, 83]. In addition, miR-10a, -375, and -455 are the most important small-interfering RNAs for tumor development and/or the reflect C cell lineage of MTC (Table 3). Therefore, dysregulation of miRs in MTC is probably an early event in C cell carcinogenesis [67, 98].
Treatment options have been proposed and implemented on the basis of the results obtained from research conducted on epigenetic alterations. Therefore, development of new therapeutic strategies based on targeting epigenetic changes, including inhibition of DNA methyltransferase and inhibition of HDAC, to restore the expression of tumor suppressor miRs or to blunt overexpressed oncogenic miRs may provide a new landscape for treatment of different types of cancers and particularly TCs. With the advent of advanced diagnostic techniques now, endocrine tumors are identified much more frequently than in the past. Preoperative diagnosis of thyroid nodules with molecular testing on FNA is now commonly considered to determine whether these nodules are benign or malignant without the need for diagnostic surgery. Moreover, analysis of epigenetic alterations in TC subtypes helps to identify pathogenesis and can play an important role in the classification and diagnosis of tumors [114]. Further studies are required to elucidate the effect of the histone modification mechanism as a potential issue relating to therapeutic aspects for TCs and also to verify the microarray analysis results (in the regulation of miRs). Given that epigenetic changes can be prevented by controlling the environmental conditions and that these changes are reversible, further studies are recommended in this field. Finding the most imperative environmental factors will be a major step towards the prevention and treatment of TCs.
References
Kilfoy BA, Zheng T, Holford TR, Han X, Ward MH, Sjodin A, et al. International patterns and trends in thyroid cancer incidence, 1973–2002. Cancer Causes Control. 2009;20(5):525–31. doi:10.1007/s10552-008-9260-4.
Fassnacht M, Kreissl MC, Weismann D, Allolio B. New targets and therapeutic approaches for endocrine malignancies. Pharmacol Ther. 2009;123(1):117–41. doi:10.1016/j.pharmthera.2009.03.013.
Xing M. Molecular pathogenesis and mechanisms of thyroid cancer. Nat Rev Cancer. 2013;13(3):184–99.
Hou P, Liu D, Shan Y, Hu S, Studeman K, Condouris S, et al. Genetic alterations and their relationship in the phosphatidylinositol 3-kinase/Akt pathway in thyroid cancer. Clin Cancer Res. 2007;13(4):1161–70.
Zou M, Baitei EY, Alzahrani AS, BinHumaid FS, Alkhafaji D, Al-Rijjal RA, et al. Concomitant RAS, RET/PTC, or BRAF mutations in advanced stage of papillary thyroid carcinoma. Thyroid. 2014;24(8):1256–66.
Şahpaz A, Önal B, Yeşilyurt A, Han Ü, Delibaşı T. BRAFV600E mutation, RET/PTC1 and PAX8-PPAR gamma rearrangements in follicular epithelium derived thyroid lesions-institutional experience and literature review. Balkan Med J. 2015;32(2):156–66.
Nikiforova MN, Lynch RA, Biddinger PW, Alexander EK, Dorn GW, Tallini G, et al. RAS point mutations and PAX8-PPARγ rearrangement in thyroid tumors: evidence for distinct molecular pathways in thyroid follicular carcinoma. J Clin Endocrinol Metab. 2003;88(5):2318–26.
Anand P, Kunnumakara AB, Sundaram C, Harikumar KB, Tharakan ST, Lai OS, et al. Cancer is a preventable disease that requires major lifestyle changes. Pharm Res. 2008;25(9):2097–116.
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277–300.
Hedayati M, Yaghmaei P, Pooyamanesh Z, Zarif Yeganeh M, Hoghooghi Rad L. Leptin: a correlated peptide to papillary thyroid carcinoma? J Thyroid Res. 2011;2011:832163. doi:10.4061/2011/832163.
Hu S, Liu D, Tufano RP, Carson KA, Rosenbaum E, Cohen Y, et al. Association of aberrant methylation of tumor suppressor genes with tumor aggressiveness and BRAF mutation in papillary thyroid cancer. Int J Cancer. 2006;119(10):2322–9.
Yin DT, Wu W, Li M, Wang QE, Li H, Wang Y, et al. DKK3 is a potential tumor suppressor gene in papillary thyroid carcinoma. Endocr Relat Cancer. 2013;20(4):507–14. doi:10.1530/ERC-13-0053.
Zhao Z, Herman JG, Brock MV, Sheng J, Zhang M, Liu B, et al. Methylation of DACT2 promotes papillary thyroid cancer metastasis by activating Wnt signaling. PloS One. 2014. doi:10.1371/journal.pone.0112336.
Lin CI, Du J, Shen WT, Whang EE, Donner DB, Griff N, et al. Mitogen-inducible gene-6 is a multifunctional adaptor protein with tumor suppressor-like activity in papillary thyroid cancer. J Clin Endocrinol Metab. 2011;96(3):E554–65. doi:10.1210/jc.2010-1800.
Yin DT, Chen G, Li HQ, Zheng XY, Wang YF, Zhang Y, et al. Relationship between methylation status of promoter and expression of XAF1 gene in papillary thyroid carcinoma [in Chinese]. Zhonghua Yi Xue Za Zhi. 2012;92(28):1967–70. doi:10.3760/cma.j.issn.0376-2491.2012.28.007.
Zuo H, Gandhi M, Edreira MM, Hochbaum D, Nimgaonkar VL, Zhang P, et al. Downregulation of Rap1GAP through epigenetic silencing and loss of heterozygosity promotes invasion and progression of thyroid tumors. Cancer Res. 2010;70(4):1389–97. doi:10.1158/0008-5472.CAN-09-2812.
Rodriguez-Rodero S, Fernandez AF, Fernandez-Morera JL, Castro-Santos P, Bayon GF, Ferrero C, et al. DNA methylation signatures identify biologically distinct thyroid cancer subtypes. J Clin Endocrinol Metab. 2013;98(7):2811–21. doi:10.1210/jc.2012-3566.
Schagdarsurengin U, Gimm O, Hoang-Vu C, Dralle H, Pfeifer GP, Dammann R. Frequent epigenetic silencing of the CpG island promoter of RASSF1A in thyroid carcinoma. Cancer Res. 2002;62(13):3698–701.
Boltze C, Zack S, Quednow C, Bettge S, Roessner A, Schneider-Stock R. Hypermethylation of the CDKN2/p16INK4A promotor in thyroid carcinogenesis. Pathol Res Pract. 2003;199(6):399–404. doi:10.1078/0344-0338-00436.
Xing M, Tokumaru Y, Wu G, Westra WB, Ladenson PW, Sidransky D. Hypermethylation of the Pendred syndrome gene SLC26A4 is an early event in thyroid tumorigenesis. Cancer Res. 2003;63(9):2312–5.
Mancikova V, Buj R, Castelblanco E, Inglada-Pérez L, Diez A, Cubas AA, et al. DNA methylation profiling of well-differentiated thyroid cancer uncovers markers of recurrence free survival. Int J Cancer. 2014;135(3):598–610.
Lee EK, Chung KW, Yang SK, Park MJ, Min HS, Kim SW, et al. DNA methylation of MAPK signal-inhibiting genes in papillary thyroid carcinoma. Anticancer Res. 2013;33(11):4833–9.
Mete O, Asa SL. Endocrine pathology [with online resource]. Cambridge: Cambridge University Press; 2016.
Cancer Genome Atlas Research Network. Integrated genomic characterization of papillary thyroid carcinoma. Cell. 2014;159(3):676–90. doi:10.1016/j.cell.2014.09.050.
Smith JA, Fan CY, Zou C, Bodenner D, Kokoska MS. Methylation status of genes in papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg. 2007;133(10):1006–11. doi:10.1001/archotol.133.10.1006.
Ellis RJ, Wang Y, Stevenson HS, Boufraqech M, Patel D, Nilubol N, et al. Genome-wide methylation patterns in papillary thyroid cancer are distinct based on histological subtype and tumor genotype. J Clin Endocrinol Metab. 2014;99(2):E329–37.
Ishida E, Nakamura M, Shimada K, Higuchi T, Takatsu K, Yane K, et al. DNA hypermethylation status of multiple genes in papillary thyroid carcinomas. Pathobiology. 2007;74(6):344–52.
Brest P, Lassalle S, Hofman V, Bordone O, Gavric Tanga V, Bonnetaud C, et al. MiR-129-5p is required for histone deacetylase inhibitor-induced cell death in thyroid cancer cells. Endocr Relat Cancer. 2011;18(6):711–9. doi:10.1530/ERC-10-0257.
Pallante P, Federico A, Berlingieri MT, Bianco M, Ferraro A, Forzati F, et al. Loss of the CBX7 gene expression correlates with a highly malignant phenotype in thyroid cancer. Cancer Res. 2008;68(16):6770–8.
Federico A, Pallante P, Bianco M, Ferraro A, Esposito F, Monti M, et al. Chromobox protein homologue 7 protein, with decreased expression in human carcinomas, positively regulates E-cadherin expression by interacting with the histone deacetylase 2 protein. Cancer Res. 2009;69(17):7079–87.
Zhang Z, Liu D, Murugan AK, Liu Z, Xing M. Histone deacetylation of NIS promoter underlies BRAF V600E-promoted NIS silencing in thyroid cancer. Endocr Relat Cancer. 2014;21(2):161–73.
Visone R, Russo L, Pallante P, De Martino I, Ferraro A, Leone V, et al. MicroRNAs (miR)-221 and miR-222, both overexpressed in human thyroid papillary carcinomas, regulate p27Kip1 protein levels and cell cycle. Endocr Relat Cancer. 2007;14(3):791–8. doi:10.1677/ERC-07-0129.
Zhang X, Li D, Li M, Ye M, Ding L, Cai H, et al. MicroRNA-146a targets PRKCE to modulate papillary thyroid tumor development. Int J Cancer. 2014;134(2):257–67. doi:10.1002/ijc.28141.
Li D, Jian W, Wei C, Song H, Gu Y, Luo Y, et al. Down-regulation of miR-181b promotes apoptosis by targeting CYLD in thyroid papillary cancer. Int J Clin Exp Pathol. 2014;7(11):7672–80.
Jain M, Zhang L, Boufraqech M, Liu-Chittenden Y, Bussey K, Demeure MJ, et al. ZNF367 inhibits cancer progression and is targeted by miR-195. PLoS One. 2014;9(7):e101423. doi:10.1371/journal.pone.0101423.
Cahill S, Smyth P, Denning K, Flavin R, Li J, Potratz A, et al. Effect of BRAF V600E mutation on transcription and post-transcriptional regulation in a papillary thyroid carcinoma model. Mol Cancer. 2007;6(1):1.
Song HM, Luo Y, Li DF, Wei CK, Hua KY, Song JL, et al. MicroRNA-96 plays an oncogenic role by targeting FOXO1 and regulating AKT/FOXO1/Bim pathway in papillary thyroid carcinoma cells. Int J Clin Exp Pathol. 2015;8(9):9889–900.
Gu Y, Li D, Luo Q, Wei C, Song H, Hua K, et al. MicroRNA-145 inhibits human papillary cancer TPC1 cell proliferation by targeting DUSP6. Int J Clin Exp Med. 2015;8(6):8590–8.
Yip L, Kelly L, Shuai Y, Armstrong MJ, Nikiforov YE, Carty SE, et al. MicroRNA signature distinguishes the degree of aggressiveness of papillary thyroid carcinoma. Ann Surg Oncol. 2011;18(7):2035–41. doi:10.1245/s10434-011-1733-0.
Cahill S, Smyth P, Finn SP, Denning K, Flavin R, O’Regan EM, et al. Effect of ret/PTC 1 rearrangement on transcription and post-transcriptional regulation in a papillary thyroid carcinoma model. Mol Cancer. 2006;5:70. doi:10.1186/1476-4598-5-70.
Kim HJ, Kim YH, Lee DS, Chung JK, Kim S. In vivo imaging of functional targeting of miR-221 in papillary thyroid carcinoma. J Nucl Med. 2008;49(10):1686–93. doi:10.2967/jnumed.108.052894.
Pallante P, Visone R, Ferracin M, Ferraro A, Berlingieri MT, Troncone G, et al. MicroRNA deregulation in human thyroid papillary carcinomas. Endocr Relat Cancer. 2006;13(2):497–508. doi:10.1677/erc.1.01209.
He H, Jazdzewski K, Li W, Liyanarachchi S, Nagy R, Volinia S, et al. The role of microRNA genes in papillary thyroid carcinoma. Proc Natl Acad Sci USA. 2005;102(52):19075–80. doi:10.1073/pnas.0509603102.
Ito Y, Hirokawa M, Higashiyama T, Takamura Y, Miya A, Kobayashi K, et al. Prognosis and prognostic factors of follicular carcinoma in Japan: importance of postoperative pathological examination. World J Surg. 2007;31(7):1417–24. doi:10.1007/s00268-007-9095-2.
Randolph GW. Surgery of the thyroid and parathyroid glands. Expert consult premium edition—enhanced online features. 2nd ed. Philadelphia: Elsevier Health Sciences; 2012.
Donninger H, Vos MD, Clark GJ. The RASSF1A tumor suppressor. J Cell Sci. 2007;120(Pt 18):3163–72. doi:10.1242/jcs.010389.
Stephen JK, Chen KM, Merritt J, Chitale D, Divine G, Worsham MJ. Methylation markers for early detection and differentiation of follicular thyroid cancer subtypes. Cancer Clin Oncol. 2015;4(2):1–12. doi:10.5539/cco.v4n2p1.
Alvarez-Nunez F, Bussaglia E, Mauricio D, Ybarra J, Vilar M, Lerma E, et al. PTEN promoter methylation in sporadic thyroid carcinomas. Thyroid. 2006;16(1):17–23. doi:10.1089/thy.2006.16.17.
Joseph B, Ji M, Liu D, Hou P, Xing MM. Lack of mutations in the thyroid hormone receptor (TR) α and β genes but frequent hypermethylation of the TRβ gene in differentiated thyroid tumors. J Clin Endocrinol Metab. 2007;92(12):4766–70. doi:10.1210/jc.2007-0812.
Kim WG, Zhu X, Kim DW, Zhang L, Kebebew E, Cheng SY. Reactivation of the silenced thyroid hormone receptor β gene expression delays thyroid tumor progression. Endocrinology. 2013;154(1):25–35. doi:10.1210/en.2012-1728.
Xing M, Usadel H, Cohen Y, Tokumaru Y, Guo Z, Westra WB, et al. Methylation of the thyroid-stimulating hormone receptor gene in epithelial thyroid tumors. Cancer Res. 2003;63(9):2316–21.
Seligson DB, Horvath S, Shi T, Yu H. Global histone modification patterns predict risk of prostate cancer recurrence. Nature. 2005;435(7046):1262.
Seligson DB, Horvath S, McBrian MA, Mah V, Yu H, Tze S, et al. Global levels of histone modifications predict prognosis in different cancers. Am J Pathol. 2009;174(5):1619–28.
Colamaio M, Puca F, Ragozzino E, Gemei M, Decaussin-Petrucci M, Aiello C, et al. miR-142-3p down-regulation contributes to thyroid follicular tumorigenesis by targeting ASH1L and MLL1. J Clin Endocrinol Metab. 2015;100(1):E59–69. doi:10.1210/jc.2014-2280.
Weber F, Teresi RE, Broelsch CE, Frilling A, Eng C. A limited set of human microRNA is deregulated in follicular thyroid carcinoma. J Clin Endocrinol Metab. 2006;91(9):3584–91. doi:10.1210/jc.2006-0693.
Nikiforova MN, Tseng GC, Steward D, Diorio D, Nikiforov YE. MicroRNA expression profiling of thyroid tumors: biological significance and diagnostic utility. J Clin Endocrinol Metab. 2008;93(5):1600–8. doi:10.1210/jc.2007-2696.
Wojtas B, Ferraz C, Stokowy T, Hauptmann S, Lange D, Dralle H, et al. Differential miRNA expression defines migration and reduced apoptosis in follicular thyroid carcinomas. Mol Cell Endocrinol. 2014;388(1–2):1–9. doi:10.1016/j.mce.2014.02.011.
Jikuzono T, Kawamoto M, Yoshitake H, Kikuchi K, Akasu H, Ishikawa H, et al. The miR-221/222 cluster, miR-10b and miR-92a are highly upregulated in metastatic minimally invasive follicular thyroid carcinoma. Int J Oncol. 2013;42(6):1858–68. doi:10.3892/ijo.2013.1879.
Asioli S, Erickson LA, Righi A, Jin L, Volante M, Jenkins S, et al. Poorly differentiated carcinoma of the thyroid: validation of the Turin proposal and analysis of IMP3 expression. Mod Pathol. 2010;23(9):1269.
Patel KN, Shaha AR. Poorly differentiated and anaplastic thyroid cancer. Cancer Control. 2006;13(2):119.
Wreesmann VB, Ghossein RA, Patel SG, Harris CP, Schnaser EA, Shaha AR, et al. Genome-wide appraisal of thyroid cancer progression. Am J Pathol. 2002;161(5):1549–56.
Vecchia C, Malvezzi M, Bosetti C, Garavello W, Bertuccio P, Levi F, et al. Thyroid cancer mortality and incidence: a global overview. Int J Cancer. 2015;136(9):2187–95.
Horn-Ross PL, Lichtensztajn DY, Clarke CA, Dosiou C, Oakley-Girvan I, Reynolds P, et al. Continued rapid increase in thyroid cancer incidence in california: trends by patient, tumor, and neighborhood characteristics. Cancer Epidemiol Biomark Prev. 2014;23(6):1067–79.
Ogasawara S, Maesawa C, Yamamoto M, Akiyama Y, Wada K, Fujisawa K, et al. Disruption of cell-type-specific methylation at the Maspin gene promoter is frequently involved in undifferentiated thyroid cancers. Oncogene. 2004;23(5):1117.
Landa I, Ibrahimpasic T, Boucai L, Sinha R, Knauf JA, Shah RH, et al. Genomic and transcriptomic hallmarks of poorly differentiated and anaplastic thyroid cancers. J Clin Invest. 2016;126(3):1052.
Zhang R, Hardin H, Chen J, Guo Z, Lloyd RV. Non-coding RNAs in thyroid cancer. Endocr Pathol. 2016;27(1):12–20.
Pallante P, Battista S, Pierantoni GM, Fusco A. Deregulation of microRNA expression in thyroid neoplasias. Nat Rev Endocrinol. 2014;10(2):88–101. doi:10.1038/nrendo.2013.223.
Boufraqech M, Klubo-Gwiezdzinska J, Kebebew E. MicroRNAs in the thyroid. Best Pract Res Clin Endocrinol Metab. 2016;30(5):603–19.
Schwertheim S, Sheu SY, Worm K, Grabellus F, Schmid KW. Analysis of deregulated miRNAs is helpful to distinguish poorly differentiated thyroid carcinoma from papillary thyroid carcinoma. Horm Metab Res. 2009;41(6):475–81. doi:10.1055/s-0029-1215593.
Dettmer MS, Perren A, Moch H, Komminoth P, Nikiforov YE, Nikiforova MN. MicroRNA profile of poorly differentiated thyroid carcinomas: new diagnostic and prognostic insights. J Mol Endocrinol. 2014;52(2):181–9.
Smallridge RC. Approach to the patient with anaplastic thyroid carcinoma. J Clin Endocrinol Metab. 2012;97(8):2566–72. doi:10.1210/jc.2012-1314.
Liu D, Yang C, Bojdani E, Murugan AK, Xing M. Identification of RASAL1 as a major tumor suppressor gene in thyroid cancer. J Natl Cancer Inst. 2013;105(21):1617–27. doi:10.1093/jnci/djt249.
Keller S, Angrisano T, Florio E, Pero R, Decaussin-Petrucci M, Troncone G, et al. DNA methylation state of the galectin-3 gene represents a potential new marker of thyroid malignancy. Oncol Lett. 2013;6(1):86–90. doi:10.3892/ol.2013.1312.
Hou P, Ji M, Xing M. Association of PTEN gene methylation with genetic alterations in the phosphatidylinositol 3-kinase/AKT signaling pathway in thyroid tumors. Cancer. 2008;113(9):2440–7. doi:10.1002/cncr.23869.
Kondo T, Nakazawa T, Ma D, Niu D, Mochizuki K, Kawasaki T, et al. Epigenetic silencing of TTF-1/NKX2-1 through DNA hypermethylation and histone H3 modulation in thyroid carcinomas. Lab Invest. 2009;89(7):791–9. doi:10.1038/labinvest.2009.50.
Borbone E, Troncone G, Ferraro A, Jasencakova Z, Stojic L, Esposito F, et al. Enhancer of zeste homolog 2 overexpression has a role in the development of anaplastic thyroid carcinomas. J Clin Endocrinol Metab. 2011;96(4):1029–38. doi:10.1210/jc.2010-1784.
Borbone E, Berlingieri MT, De Bellis F, Nebbioso A, Chiappetta G, Mai A, et al. Histone deacetylase inhibitors induce thyroid cancer-specific apoptosis through proteasome-dependent inhibition of TRAIL degradation. Oncogene. 2010;29(1):105–16. doi:10.1038/onc.2009.306.
Smith N, Nucera C. Personalized therapy in patients with anaplastic thyroid cancer: targeting genetic and epigenetic alterations. J Clin Endocrinol Metab. 2014. doi:10.1210/jc.2014-2803.
Puppin C, Passon N, Lavarone E, Di Loreto C, Frasca F, Vella V, et al. Levels of histone acetylation in thyroid tumors. Biochem Biophys Res Commun. 2011;411(4):679–83. doi:10.1016/j.bbrc.2011.06.182.
Xiong Y, Zhang L, Kebebew E. MiR-20a is upregulated in anaplastic thyroid cancer and targets LIMK1. PLoS One. 2014;9(5):e96103. doi:10.1371/journal.pone.0096103.
Cheng Q, Zhang X, Xu X, Lu X. MiR-618 inhibits anaplastic thyroid cancer by repressing XIAP in one ATC cell line. Ann Endocrinol (Paris). 2014;75(4):187–93. doi:10.1016/j.ando.2014.01.002.
Boufraqech M, Zhang L, Jain M, Patel D, Ellis R, Xiong Y, et al. miR-145 suppresses thyroid cancer growth and metastasis and targets AKT3. Endocr Relat Cancer. 2014;21(4):517–31. doi:10.1530/erc-14-0077.
Yi L, Yuan Y. MicroRNA-618 modulates cell growth via targeting PI3K/Akt pathway in human thyroid carcinomas. Indian J Cancer. 2015;52(Suppl 3):E186–9. doi:10.4103/0019-509x.186577.
Fuziwara CS, Kimura ET. MicroRNA deregulation in anaplastic thyroid cancer biology. Int J Endocrinol. 2014;2014:743450. doi:10.1155/2014/743450.
Esposito F, Tornincasa M, Pallante P, Federico A, Borbone E, Pierantoni GM, et al. Down-regulation of the miR-25 and miR-30d contributes to the development of anaplastic thyroid carcinoma targeting the polycomb protein EZH2. J Clin Endocrinol Metab. 2012;97(5):E710–8.
Zhang Y, Yang WQ, Zhu H, Qian YY, Zhou L, Ren YJ, et al. Regulation of autophagy by miR-30d impacts sensitivity of anaplastic thyroid carcinoma to cisplatin. Biochem Pharmacol. 2014;87(4):562–70. doi:10.1016/j.bcp.2013.12.004.
Kloos RT, Eng C, Evans DB, Francis GL, Gagel RF, Gharib H, et al. Medullary thyroid cancer: management guidelines of the American Thyroid Association. Thyroid. 2009;19(6):565–612. doi:10.1089/thy.2008.0403.
Nozhat Z, Hedayati M, Pourhassan H. Signaling pathways in medullary thyroid carcinoma: therapeutic implications. Int J Endocr Oncol. 2016;3(4):299–312.
Nozhat Z, Hedayati M. PI3K/AKT pathway and its mediators in thyroid carcinomas. Mol Diagn Ther. 2016;20(1):13–26.
Hedayati M, Zarif Yeganeh M, Sheikhol Eslami S, Rezghi Barez S, Hoghooghi Rad L, Azizi F. Predominant RET germline mutations in exons 10, 11, and 16 in Iranian patients with hereditary medullary thyroid carcinoma. J Thyroid Res. 2011;2011:264248. doi:10.4061/2011/264248.
Alvandi E, Akrami SM, Chiani M, Hedayati M, Nayer BN, Tehrani MR, et al. Molecular analysis of the RET proto-oncogene key exons in patients with medullary thyroid carcinoma: a comprehensive study of the Iranian population. Thyroid. 2011;21(4):373–82. doi:10.1089/thy.2010.0267.
Hedayati M, Nabipour I, Rezaei-Ghaleh N, Azizi F. Germline RET mutations in exons 10 and 11: an Iranian survey of 57 medullary thyroid carcinoma cases. Med J Malays. 2006;61(5):564–9.
Shirazi HA, Hedayati M, Daneshpour MS, Shafiee A, Azizi F. Analysis of loss of heterozygsity effect on thyroid tumor with oxyphilia cell locus in familial non medullary thyroid carcinoma in Iranian families. Indian J Hum Genet. 2012;18(3):340–3. doi:10.4103/0971-6866.107989.
Hedayati M, Zarif Yeganeh M, Daneshpour M, Delbarpour Ahmadi A, Azizi F. Frequent germ line mutations in RET proto-oncogene exons 10 and 11 in hereditary medullary thyroid carcinomas of Iranian patients. Kowsar Med J. 2010;15(1):17–21.
Yeganeh MZ, Sheikholeslami S, Hedayati M. RET proto oncogene mutation detection and medullary thyroid carcinoma prevention. Asian Pac J Cancer Prev. 2015;16(6):2107–17.
Schagdarsurengin U, Gimm O, Dralle H, Hoang-Vu C, Dammann R. CpG island methylation of tumor-related promoters occurs preferentially in undifferentiated carcinoma. Thyroid. 2006;16(7):633–42.
Sponziello M, Durante C, Boichard A, Dima M, Puppin C, Verrienti A, et al. Epigenetic-related gene expression profile in medullary thyroid cancer revealed the overexpression of the histone methyltransferases EZH2 and SMYD3 in aggressive tumours. Mol Cell Endocrinol. 2014;392(1–2):8–13. doi:10.1016/j.mce.2014.04.016.
Hudson J, Duncavage E, Tamburrino A, Salerno P, Xi L, Raffeld M, et al. Overexpression of miR-10a and miR-375 and downregulation of YAP1 in medullary thyroid carcinoma. Exp Mol Pathol. 2013;95(1):62–7.
Mian C, Pennelli G, Fassan M, Balistreri M, Barollo S, Cavedon E, et al. MicroRNA profiles in familial and sporadic medullary thyroid carcinoma: preliminary relationships with RET status and outcome. Thyroid. 2012;22(9):890–6. doi:10.1089/thy.2012.0045.
Duan L, Hao X, Liu Z, Zhang Y, Zhang G. MiR-129-5p is down-regulated and involved in the growth, apoptosis and migration of medullary thyroid carcinoma cells through targeting RET. FEBS Lett. 2014;588(9):1644–51. doi:10.1016/j.febslet.2014.03.002.
Sherman SI. Targeted therapy of thyroid cancer. Biochem Pharmacol. 2010;80(5):592–601. doi:10.1016/j.bcp.2010.05.003.
Tan J, Cang S, Ma Y, Petrillo RL, Liu D. Novel histone deacetylase inhibitors in clinical trials as anti-cancer agents. J Hematol Oncol. 2010;3(1):5.
Lane AA, Chabner BA. Histone deacetylase inhibitors in cancer therapy. J Clin Oncol. 2009;27(32):5459–68.
Zarkesh M, Taghaddosi M, Azizi F, Zadeh-Vakili A, Hedayati M. Importance of epigenetic changes in the thyroid cancer incidence and their therapeutic applications. Modares J Med Sci Pathobiol. 2014;17(3):1–21.
Catalano MG, Fortunati N, Boccuzzi G. Epigenetics modifications and therapeutic prospects in human thyroid cancer. Front Endocrinol (Lausanne). 2012;3:40. doi:10.3389/fendo.2012.00040.
Woyach JA, Kloos RT, Ringel MD, Arbogast D, Collamore M, Zwiebel JA, et al. Lack of therapeutic effect of the histone deacetylase inhibitor vorinostat in patients with metastatic radioiodine-refractory thyroid carcinoma. J Clin Endocrinol Metab. 2009;94(1):164–70. doi:10.1210/jc.2008-1631.
Catalano MG, Pugliese M, Gargantini E, Grange C, Bussolati B, Asioli S, et al. Cytotoxic activity of the histone deacetylase inhibitor panobinostat (LBH589) in anaplastic thyroid cancer in vitro and in vivo. Int J Cancer. 2012;130(3):694–704.
Greenfield LJ. Molecular mechanisms of antiseizure drug activity at GABAA receptors. Seizure. 2013;22(8):589–600. doi:10.1016/j.seizure.2013.04.015.
Göttlicher M, Minucci S, Zhu P, Krämer OH, Schimpf A, Giavara S, et al. Valproic acid defines a novel class of HDAC inhibitors inducing differentiation of transformed cells. EMBO J. 2001;20(24):6969–78.
Duenas-Gonzalez A, Candelaria M, Perez-Plascencia C, Perez-Cardenas E, de la Cruz-Hernandez E, Herrera LA. Valproic acid as epigenetic cancer drug: preclinical, clinical and transcriptional effects on solid tumors. Cancer Treat Rev. 2008;34(3):206–22.
Nilubol N, Merkel R, Yang L, Patel D, Reynolds JC, Sadowski SM, et al. A phase II trial of valproic acid in patients with advanced, radioiodine-resistant thyroid cancers of follicular cell origin. Clin Endocrinol (Oxf). 2017;86(1):128–33. doi:10.1111/cen.13154.
Yang X, Lay F, Han H, Jones PA. Targeting DNA methylation for epigenetic therapy. Trends Pharmacol Sci. 2010;31(11):536–46.
Stephen JK, Chitale D, Narra V, Chen KM, Sawhney R, Worsham MJ. DNA methylation in thyroid tumorigenesis. Cancers. 2011;3(2):1732–43. doi:10.3390/cancers3021732.
dos Reis MB, Beltrami CM, Kowaslki LP, Rogatto SR. Epigenetic alterations in well-differentiated thyroid cancer. J Clin Epigenet. 2016;1:1. doi:10.21767/2472-1158.100008.
Liu Z, Hou P, Ji M, Guan H, Studeman K, Jensen K, et al. Highly prevalent genetic alterations in receptor tyrosine kinases and phosphatidylinositol 3-kinase/akt and mitogen-activated protein kinase pathways in anaplastic and follicular thyroid cancers. J Clin Endocrinol Metab. 2008;93(8):3106–16.
Wang Y, Hou P, Yu H, Wang W, Ji M, Zhao S, et al. High prevalence and mutual exclusivity of genetic alterations in the phosphatidylinositol-3-kinase/akt pathway in thyroid tumors. J Clin Endocrinol Metab. 2007;92(6):2387–90.
Zhang B, Liu S, Zhang Z, Wei J, Qu Y, Wu K, et al. Analysis of BRAFV600E mutation and DNA methylation improves the diagnostics of thyroid fine needle aspiration biopsies. Diagn Pathol. 2014. doi:10.1186/1746-1596-9-45.
Hou P, Liu D, Xing M. Genome-wide alterations in gene methylation by the BRAF V600E mutation in papillary thyroid cancer cells. Endocr Relat Cancer. 2011;18(6):687–97. doi:10.1530/ERC-11-0212.
Korochkin L. What is epigenetics. Russ J Genet. 2006;42(9):958–65.
Ciampi R, Knauf JA, Kerler R, Gandhi M, Zhu Z, Nikiforova MN, et al. Oncogenic AKAP9-BRAF fusion is a novel mechanism of MAPK pathway activation in thyroid cancer. J Clin Investig. 2005;115(1):94–101.
Dong X, Korch C, Meinkoth JL. Histone deacetylase inhibitors upregulate Rap1GAP and inhibit Rap activity in thyroid tumor cells. Endocr Relat Cancer. 2011;18(3):301–10. doi:10.1530/ERC-10-0320.
Acknowledgements
This work is part of a Ph.D. research thesis by Maryam Zarkesh. The authors wish to acknowledge Ms. Niloofar Shiva for critical editing of English grammar and syntax of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors (MZ, AZV, FA, FF, MMA, and MH) declare no conflicts of interest.
Funding
This work was supported by Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Rights and permissions
About this article
Cite this article
Zarkesh, M., Zadeh-Vakili, A., Azizi, F. et al. Altered Epigenetic Mechanisms in Thyroid Cancer Subtypes. Mol Diagn Ther 22, 41–56 (2018). https://doi.org/10.1007/s40291-017-0303-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-017-0303-y