Abstract
Purpose
In this study, we evaluated the impact of risk factors for gestational diabetes on clinical/biochemical parameters and maternal/fetal outcomes.
Methods
One hundred eighty-three (n 183) women (age 33.8 ± 5.5 years, 59% Caucasians, 41% non-Caucasians) with gestational diabetes were included in the study. Anamnestic information, anthropometric and laboratory parameters, and maternal and fetal outcomes at delivery were collected.
Results
Insulin therapy prevalence was higher in Asians vs Caucasians (p = 0.006), despite lower pre-pregnancy BMI in Asians (p = 0.0001) and in pre-pregnancy overweight vs normal weight patients (p = 0.04). Insulin-treated patients had higher fasting OGTT glucose than patients on diet therapy (p = 0.003). In multivariate analysis, Asian ethnicity, age ≥ 35 years and pre-pregnancy BMI ≥ 25 kg/m2 were independent predictors of insulin therapy. Cesarean section occurred more in women aged ≥ 35 years than < 35 years (p = 0.02). Duration of pregnancy and age showed inverse correlation (r − 0.3 p = 0.013). Week of delivery was lower in patients ≥ 35 years vs patients < 35 years (p = 0.013). Fasting OGTT glucose was higher in overweight than in normal weight patients (p = 0.016). 1-h OGTT glucose was lower in obese vs normal weight (p = 0.03) and overweight patients (p = 0.03). Prevalence of prior gestational diabetes was higher in overweight/obese women (p = 0.002).
Conclusions
Ethnicity, age, and BMI have the heaviest impact on pregnancy outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gestational diabetes mellitus (GDM) is defined as diabetes diagnosed in the second or third trimester of pregnancy that is not clearly either type 1 or type 2 diabetes (T2D) [1].
GDM prevalence is increasing worldwide in parallel with the rise of obesity and T2D [1,2,3,4]. Approximately 7% of all pregnancies are complicated by GDM, resulting in more than 200,000 cases annually. The prevalence may range from 1 to 14% of all pregnancies, depending on the population studied and the diagnostic tests employed [5]. Diagnostic criteria have changed recently and there has been lack of consent about which criteria to use [6]. Well-established risk factors for GDM are pre-pregnancy overweight/obesity, advanced maternal age, and family history of T2D. However, the contribution of these risk factors differs by race/ethnicity. From a public health perspective, overweight/obesity is considered the most important risk factor for GDM, because it is the most modifiable [7,8,9,10]. Obesity seems to be a strong risk factor for GDM in all racial/ethnic groups, but especially among non-Asians [11]. Ethnicity is considered one of the main risk factors for developing GDM. In particular, ethnic groups which are considered at high-risk of GDM include Hispanics, African-Americans, Native Americans, Asians, Pacific Islanders, and Indigenous Australians [12,13,14]. Overall, South and South East Asian women are considered those with the highest risk [2]. The newly proposed International Association of the Diabetes and Pregnancy Study Groups (IADPSG) approach [15] recommends the administration of a 75-g 2 h OGTT (one-step approach), evaluating fasting, 1- and 2-h glucose levels, and considering any single abnormal value as diagnostic of GDM. The IADPSG criteria are the only based on the results of the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study [16], a large-scale (25,000 pregnant women) multinational cohort study that demonstrated associations between glycemic levels and an increased risk of obstetric and perinatal morbidities. In Italy, GDM screening is based on defined risk factors. In particular, a 75-g 2-h OGTT (one-step approach), evaluating fasting, 1- and 2-h glucose levels is performed at 16–18 weeks of gestation (and repeated at 24–28 weeks, if negative) in women with at least one of the following conditions: GDM in a previous pregnancy, pre-pregnancy body mass index (BMI) ≥ 30 kg/m2, plasma glucose prior, or at the beginning of pregnancy between 100 and 125 mg/dl (5.6–6.9 mmol/l). At 24–28 weeks of gestation, the test is performed in women with at least one of the following conditions: age ≥ 35 years, pre-gestational body mass index (BMI) ≥ 25 kg/m2, fetal macrosomia in a previous pregnancy (≥ 4.5 kg), family history of T2D (first degree relative with T2D), and ethnic groups with high diabetes prevalence (South Asia, the Caribbean, Middle East). Diagnosis of GDM is defined by one or more values of plasma glucose above the thresholds (≥ 92 mg/dl at baseline, ≥ 180 mg/dl 1-h post-load, ≥ 153 mg/dl 2-h post-load) [17, 18].
GDM is associated with short-term adverse outcomes for both mother (hypertension, preeclampsia, cesarean, and pre-term delivery) and their offspring (shoulder dystocia, birth trauma, neonatal jaundice, respiratory distress, and neonatal hypoglycemia) [19]. GDM leads to mothers’ long-term complications, such as increased risk of GDM recurrence, T2D, hypertension, and cardiovascular disease (CVD). In addition, diabetes in pregnancy may increase the risk of obesity and T2D in offspring later in life [1].
The aim of this retrospective observational study was to evaluate the impact of the risk factors considered for selective screening on clinical/biochemical parameters and on maternal and fetal outcomes, in pregnancy complicated by GDM.
Methods
One hundred eighty-three (n 183) women with GDM, followed between January 2014 and July 2016 in the outpatient clinics of Policlinico Umberto I “Sapienza” University Hospital of Rome, were included in the study. All patients gave their written informed consent. The protocol was approved by the hospital ethics committee and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Diagnosis of GDM was defined in accordance with current recommendations [17, 18]. The inclusion criteria were: age ≥ 18 years and delivery within July 2016. The exclusion criteria were: type 1 diabetes; pre-gestational T2D; and multiple pregnancy.
The following data were collected: age; ethnicity; parity; smocking habits; alcohol consumption; and information about the presence of risk factors for GDM, suggested by current recommendation; week of gestation and plasma glucose values at OGTT; and information about medical nutrition therapy and physical activity.
Anthropometric/vital (weight, BMI, blood pressure, and pulse) and laboratory parameters were considered: HbA1c at diagnosis and at third trimester, lipid profile at third trimester (total and HDL cholesterol, triglycerides, non-HDL cholesterol, and LDL cholesterol calculated with Friedewald formula). Fetal ultrasound parameters (third trimester) were collected: amniotic fluid index (AFI), crown-rump length (CRL), bi-parietal diameter (BPD), abdominal circumference (AC), head circumference (HC), femur length (FL), humerus length (HL), and estimated fetal weight (EFW).
Information about the results of self-monitoring blood glucose (SMBG) four times daily, therapy for GDM (diet or insulin), and other therapies (antihypertensive, antiplatelet, and other drugs) at the third trimester was also obtained. Fetal and maternal outcomes were considered at delivery: fetal weight and growth (appropriate, small, and large for gestational age), malformations, neonatal hypoglycemia, hypocalcaemia, hyperbilirubinemia, type of delivery (spontaneous vaginal delivery and cesarean section), miscarriage, maternal, and infant mortality.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD) and categorical variables as percentage. Continuous variables were tested for normality with Kolmogorov–Smirnov test. Differences between two groups were evaluated with independent sample t test for normally distributed continuous variables and with Mann–Whitney U test, for not normally distributed continuous variables. The one-way ANOVA was used to compare means of more than two independent groups. The one-way ANCOVA test was used to analyze differences in means between groups, adjusting for covariates. Categorical variables between groups were compared using Chi-squared Test. The Pearson correlation coefficient was obtained to test the association between variables. A p value < 0.05 was considered statistically significant. Variables presenting clinical relevance and statistical significance (p < 0.05) upon univariate analysis were included in the logistic regression model for prediction of insulin therapy requirement. Odds ratios and the probability of insulin requirement were estimated for the variables included in this model. Statistical analysis was performed with IBM SPSS Statistics software version 23 (Chicago, IL, USA).
Results
Clinical and biochemical parameters of patients and maternal and fetal outcomes are reported in Tables 1 and 2.
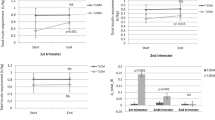
Prevalence of insulin therapy was significantly higher in Asians than in Caucasians (63.6 vs 40.7%, p value = 0.006), despite a significantly lower pre-pregnancy BMI in Asians vs Caucasians (28.2 ± 6.9 vs 23.8 ± 4.6 kg/m2, p = 0.000).
An increased requirement for insulin therapy was observed in patients with pre-pregnancy BMI ≥ 25 kg/m2 vs patients with pre-pregnancy BMI < 25 kg/m2 (61.3 vs 41.3%, p = 0.04).
Patients requiring insulin therapy had higher fasting plasma glucose at OGTT than patients in medical nutrition therapy (93.1 ± 11.3 vs 97.1 ± 11.9 mg/dl, p = 0.003).
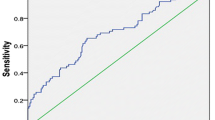
A logistic regression analysis was performed to evaluate the effect of age, ethnicity, pre-pregnancy BMI, and fasting plasma glucose at OGTT on the requirement of insulin therapy. The factors identified as independent predictors of insulin therapy were Asian ethnicity, age ≥ 35 years, and pre-pregnancy BMI ≥ 25 kg/m2 Table 3.
Frequency of cesarean section was higher in women with age ≥ 35 years than in women with age < 35 years (86.6 vs 57.1%, p = 0.02) and a significant negative correlation between duration of pregnancy and maternal age was found (r − 0.3 p = 0.013). Gestational week of delivery was lower in patients with age ≥ 35 years in comparison with patients with age < 35 years (37.7 ± 1.5 vs 38.8 ± 1.6 weeks, p = 0.013). Prevalence of pre-term delivery (< 37 weeks) was 8.1%.
Basal plasma glucose at OGTT was significantly higher in patients with pre-pregnancy BMI ≥ 25 kg/m2 than in normal weight patients (93.7 ± 9.9 vs 87.5 ± 12.8 mg/dl, p = 0.016). Whereas 1-h plasma glucose at OGTT was significantly lower in obese patients compared with normal weight (147.7 ± 31.6 vs 178 ± 27.8 mg/dl, p = 0.03) and overweight patients (147.7 ± 31.6 vs 188.0 ± 27.4 mg/dl, p = 0.03).
Prevalence of GDM in a previous pregnancy was significantly higher in patients with pre-pregnancy BMI ≥ 25 kg/m2, compared with normal weight patients (17 vs 0%, p = 0.002).
No significant differences were found in fetal ultrasound parameters and neonatal outcomes.
Discussion
The aim of this observational study was to evaluate the effect of the risk factors considered for selective screening for GDM on maternal and fetal outcomes.
Asian ethnicity was independently associated with the need for insulin treatment, despite a significantly lower pre-pregnancy BMI. Many studies have found some clinical or biochemical parameters at diagnosis which is associated with the requirement for insulin therapy [20,21,22,23,24,25,26,27,28]. Most of them included pre-pregnancy BMI ≥ 30 kg/m2 and non-European ethnicity [29]. In this study, an increased requirement for insulin therapy was also observed in pre-pregnancy overweight patients, probably due to the effect of insulin resistance: increasing peripheral insulin resistance, which is already physiologically exacerbated during pregnancy, was found to be an important predictor of poor glycemic control in pregnant women with GDM [30]. It is well known that obesity is one of the main risk factors for GDM development and insulin therapy requirement; however, the relative contribution of this risk factor might differ by race/ethnicity. Yet, there is ongoing debate on the definition of overweight and obesity in Asian populations. The WHO and the ADA have recommended the use of lower body mass index (BMI) cut-off points for Asians (< 23 kg/m2 for normal weight) as the lower BMI cutoffs better identify health risks for T2D and cardiovascular disease among Asians [31, 32]. The reasons why Asians have higher risk for GDM and for insulin therapy at a lower BMI might be attributed to a genetic predisposition toward increased insulin resistance in the muscle or increased levels of visceral fat [11]. In this view, the effect of higher values of BMI in predicting the need for insulin treatment might be “masked” by the effect of ethnicity in this study population.
Frequency of cesarean section was found to be higher in patients with age ≥ 35 years. This result was also observed in other studies [33,34,35,36] and it might reflect the picture in the general population, regardless of the presence of GDM. In fact, in developed countries, the relative risk of cesarean section among women with age ≥ 35 years with single pregnancy is increased by 1.39–2.76 times compared to women aged < 35 years [33]. It is well documented that prevalence of cesarean section in pregnancies complicated by GDM is higher than in normal pregnancies, mainly due to high prevalence of macrosomia in uncontrolled GDM. However, Gorgal et al. observed an higher incidence of cesarean section in GDM patients, regardless of fetal weight. Thus, this finding may be due to the higher prevalence of both GDM and cesarean section in women older than 35 years [37]. Moreover, the higher prevalence of cesarean section in older pregnant women with GDM could also reflect an attitude of gynecologists to lower risks of possibly difficult deliveries.
A significant negative correlation between maternal age and duration of gestation was found, although an association between maternal age and pre-term delivery was not observed. In the literature, most studies are observed no association between increased maternal age and pre-term delivery, but there are still conflicting data on this issue [38,39,40]. Thus, further studies are needed to evaluate this aspect, especially in pregnancy complicated by GDM.
Elevated fasting blood glucose level at GDM diagnosis was found to be predictive of insulin therapy in GDM [21,22,23, 25,26,27]. In this study, fasting plasma glucose at OGTT was associated with insulin requirement. However, in multivariate analysis, it was not an independent prediction of insulin therapy. In other studies, 1- and/or 2-h plasma glucose levels at OGTT were significantly higher in insulin-treated group compared with diet group [21, 25, 28]. In this population, 1-h plasma glucose at OGTT was significantly lower in obese patients compared with normal weight and overweight patients, possibly reflecting a higher degree of insulin resistance in the obese group.
Moreover, the previous GDM is a well-established risk factor. It has been demonstrated that recurrence of GDM is strongly associated with pre-pregnancy BMI ≥ 30 kg/m2 [41]. In a recent meta-analysis, pre-pregnancy BMI was also found to be one of the main predictors for GDM recurrence [29]. In accordance with this findings, in this study group, prevalence of the previous GDM was 17% and all patients with recurrent GDM were overweight before pregnancy.
Conclusions
In conclusion, ethnicity, BMI, and age showed to have the heaviest impact on pregnancy outcomes in women with GDM. In this view, it is worth recognizing these risk factors at diagnosis, or at an early stage, to better customize the management of the disease and to prevent adverse outcomes.
References
American Diabetes Association (2017) Standards of medical care in diabetes—2017. Diabetes Care 40(Suppl 1):S1–S2. https://doi.org/10.2337/dc17-S001
Yuen L, Wong VW (2015) Gestational diabetes mellitus: challenges for different ethnic groups. World J Diabetes 6(8):1024–1032. https://doi.org/10.4239/wjd.v6.i8.1024
Albrecht SS, Kuklina EV, Bansil P, Jamieson DJ, Whiteman MK, Kourtis AP et al (2010) Diabetes trends among delivery hospitalizations in the US, 1994–2004. Diabetes Care 33(4):768–773. https://doi.org/10.2337/dc09-1801
Chiefari E, Arcidiacono B, Foti D, Brunetti A (2017) Gestational diabetes mellitus: an updated overview. J Endocrinol Invest. https://doi.org/10.1007/s40618-016-0607-5 (Epub ahead of print)
American Diabetes Association (2004) Gestational diabetes mellitus. Diabetes Care 27(Suppl 1):S88–S90
Coustan DR, Lowe LP, Metzger BE, Dyer AR, International Association of Diabetes and Pregnancy Study Groups (2010) The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study: paving the way for new diagnostic criteria for gestational diabetes mellitus. Am J Obstet Gynecol 202(6):654.e1-6. https://doi.org/10.1016/j.ajog.2010.04.006
Pu J, Zhao B, Wang EJ, Nimbal V, Osmundson S, Kunz L et al (2015) Racial/ethnic differences in gestational diabetes prevalence and contribution of common risk factors. Paediatr Perinat Epidemiol 29(5):436–443. https://doi.org/10.1111/ppe.12209
Triunfo S, Lanzone A, Lindqvist PG (2017) Low maternal circulating levels of vitamin D as potential determinant in the development of gestational diabetes mellitus. J Endocrinol Invest 40(10):1049–1059
Cozzolino M, Serena C, Maggio L, Rambaldi MP, Simeone S, Mello G et al (2017) Analysis of the main risk factors for gestational diabetes diagnosed with International Association of Diabetes and Pregnancy Study Groups (IADPSG) criteria in multiple pregnancies. J Endocrinol Invest 40(9):937–943
Alptekin H, Çizmecioğlu A, Işık H, Cengiz T, Yildiz M, Iyisoy MS (2016) Predicting gestational diabetes mellitus during the first trimester using anthropometric measurements and HOMA-IR. J Endocrinol Invest 39:577–583
Hedderson M, Ehrlich S, Sridhar S, Darbinian J, Moore S, Ferrara A (2012) Racial/ethnic disparities in the prevalence of gestational diabetes mellitus by BMI. Diabetes Care 35(7):1492–1498. https://doi.org/10.2337/dc11-2267
Kjos SL, Buchanan TA (1999) Gestational diabetes mellitus. N Engl J Med 341:1749–1756. https://doi.org/10.1056/NEJM199912023412307
American Diabetes Association (2002) Position Statement. Screening for Diabetes. Diabetes Care 25(supplement 1):S21–S24
Vandorsten JP, Dodson WC, Espeland MA, Grobman WA, Guise JM, Mercer BM et al (2013) NIH consensus development conference: diagnosing gestational diabetes mellitus. NIH Consens State Sci Statements 29(1):1–31
International Association of Diabetes and Pregnancy Study Groups Consensus Panel (2010) International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33:676–682. https://doi.org/10.2337/dc09-1848
Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, HAPO Study Cooperative Research Group et al (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358:1991–2002. https://doi.org/10.1056/NEJMoa0707943
Sistema nazionale per le linee guida dell’Istituto Superiore di Sanità (2010) Linea guida Gravidanza fisiologica. http://www.snlg-iss.it/cms/files/LG_Gravidanza.pdf. Accessed Nov 2010
AMD SID (2016) Standard italiani per la cura del diabete mellito 2016 http://www.standarditaliani.it/skin/www.standarditaliani.it/pdf/STANDARD_2016_June20.pdf. Accessed 20 June 2016
Xiang AH, Li BH, Black MH, Sacks DA, Buchanan TA, Jacobsen SJ et al (2011) Racial and ethnic disparities in diabetes risk after gestational diabetes mellitus. Diabetologia 54(12):3016–3021. https://doi.org/10.1007/s00125-011-2330-2
Pertot T, Molyneaux L, Tan K, Ross GP, Yue DK, Wong J (2011) Can common clinical parameters be used to identify patients who will need insulin treatment in gestational diabetes mellitus? Diabetes Care 34:2214–2216
Wong V, Jalaludin B (2011) Gestational diabetes mellitus: who requires insulin therapy? Aust N Z J Obstet Gynaecol 51:432–436
Akinci B, Celtik A, Yener S, Yesil S (2008) Is fasting glucose during oral glucose tolerance test an indicator of the insulin need in gestational diabetes? Diabetes Res Clin Pract 82:219–225
McFarland MB, Langer O, Conway DL, Berkus MD (1999) Dietary therapy for gestational diabetes: how long is long enough? Obstet Gynecol 93:978–982
Mitra S, Nayak PK, Sahoo J, Mathew A, Padma A, Kamalanathan S et al (2014) Predictors of antenatal insulin requirement in gestational diabetes. Gynecol Endocrinol 30:565–568
Bakiner O, Ozsahin BK, Sariturk C, Ertorer E (2013) Risk factors that can predict antenatal insulin need in gestational diabetes. J Clin Med Res 5:381–388
Barnes RA, Wong T, Ross GP, Jalaludin BB, Wong VW, Smart CE et al (2016) A novel validated model for the prediction of insulin therapy initiation and adverse perinatal outcomes in women with gestational diabetes mellitus. Diabetologia 59:2331–2338
Zhang Y, Shao J, Li F, Xu X (2016) Factors in gestational diabetes mellitus predicting the needs for insulin therapy. Int J Endocrinol 2016:4858976
Watanabe M, Katayama A, Kagawa H, Ogawa D, Wada J (2016) Risk factors for the requirement of antenatal insulin treatment in gestational diabetes mellitus. J Diabetes Res 2016:9648798 (Epub 2016 Nov 23)
Schwartz N, Nachum Z, Green MS (2016) Risk factors of gestational diabetes mellitus recurrence: a meta-analysis. Endocrine 53:662–671
Langer O, Yogev Y, Most O, Xenakis EM (2005) Gestational diabetes: the consequences of not treating. Am J Obstet Gynecol 192(4):989–997
WHO Expert Consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363:157–163
Hsu WC, Araneta MR, Kanaya AM, Chiang JL, Fujimoto W (2015) BMI cut points to identify at-risk Asian Americans for type 2 diabetes screening. Diabetes Care 38:150–158
Bayrampour H, Heaman M (2010) Advanced maternal age and the risk of cesarean birth: a systematic review. Birth 37(3):219–226
Jolly M, Sebire N, Harris J, Robinson S, Regan L (2000) The risks associated with pregnancy in women aged 35 years or older. Hum Reprod 15:2433–2437
Bell JS, Campbell DM, Graham WJ, Penney GC, Ryan M, Hall MH (2001) Can obstetric complications explain the high levels of obstetric interventions and maternity service use among older women? A retrospective analysis of routinely collected data. BJOG 108(9):910–918
O’Leary CM, de Klerk N, Keogh J, Pennell C, de Groot J, York L et al (2007) Trends in mode of delivery during 1984–2003: can they be explained by pregnancy and delivery complications? BJOG 114(7):855–864 (Epub 2007 May 15)
Gorgal R, Gonçalves E, Barros M, Namora G, Magalhães A, Rodrigues T et al (2012) Gestational diabetes mellitus: a risk factor for non-elective cesarean section. J Obstet Gynaecol Res 38(1):154–159
Diet A, Cupisti S, Beckmann MW, Schwab M, Zollner U (2015) Pregnancy and obstetrical outcomes in women over 40 years of age. Geburtshilfe Frauenheilkd 75(8):827–832
Benli AR, Cetin Benli N, Usta AT, Atakul T, Koroglu M (2015) Effect of maternal age on pregnancy outcome and cesarean delivery rate. J Clin Med Res 7(2):97–102
Berkowitz GS, Skovron ML, Lapinski RH, Berkowitz RL (1990) Delayed childbearing and the outcome of pregnancy. N Engl J Med 322:659–664
Major CA, deVeciana M, Weeks J, Morgan MA (1998) Recurrence of gestational diabetes: who is at risk? Am J Obstet Gynecol 179(4):1038–1042
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Filardi, T., Tavaglione, F., Di Stasio, M. et al. Impact of risk factors for gestational diabetes (GDM) on pregnancy outcomes in women with GDM. J Endocrinol Invest 41, 671–676 (2018). https://doi.org/10.1007/s40618-017-0791-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-017-0791-y