Abstract
Most of the current therapies, as well as many of the clinical trials, for multiple sclerosis (MS) target the inflammatory autoimmune processes, but less than 20% of all clinical trials investigate potential therapies for the chronic progressive disease stage of MS. The latter is responsible for the steadily increasing disability in many patients, and there is an urgent need for novel therapies that protect nervous system tissue and enhance axonal growth and/or remyelination. As outlined in this review, solid pre-clinical data suggest neutralization of the neurite outgrowth inhibitor Nogo-A as a potential new way to achieve both axonal and myelin repair. Several phase I clinical studies with anti-Nogo-A antibodies have been conducted in different disease paradigms including MS and spinal cord injury. Data from spinal cord injury and amyotrophic lateral sclerosis (ALS) trials accredit a good safety profile of high doses of anti-Nogo-A antibodies administered intravenously or intrathecally. An antibody against a Nogo receptor subunit, leucine rich repeat and immunoglobulin-like domain-containing protein 1 (LINGO-1), was recently shown to improve outcome in patients with acute optic neuritis in a phase II study. Nogo-A-suppressing antibodies could be novel drug candidates for the relapsing as well as the progressive MS disease stage. In this review, we summarize the available pre-clinical and clinical evidence on Nogo-A and elucidate the potential of Nogo-A-antibodies as a therapy for progressive MS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Solid pre-clinical data suggest Nogo-A neutralization as a potential therapeutic approach for neuro-inflammatory and demyelinating pathology. |
Nogo-A antibodies are now in early clinical development for multiple sclerosis. |
Their potential to boost axonal regeneration and compensatory fiber growth as well as myelin repair makes them an attractive candidate to also treat progressive multiple sclerosis, in which neurodegeneration and chronic demyelination are hallmarks. |
1 Introduction
Multiple sclerosis (MS) is the leading cause of non-traumatic neurological disability in young adults in Europe and America [1]. It is an inflammatory demyelinating disease of the central nervous system (CNS) [2]. The causes of MS are not yet fully understood, but a complex genetic trait and several environmental risk factors have been identified, and the prevailing view suggests an autoimmune etiology [3].
In 85% of cases, the disease begins with a relapsing remitting course (RRMS), during which bouts of inflammatory disease activity, with a transient blood–brain barrier (BBB) opening, are observed. In most patients, RRMS is followed by a progressive phase. This phase is defined by a disappearance of relapses and a gradual increase in disability without remission; finally, many patients become wheelchair bound. This form is referred to as secondary progressive MS. In 10% of cases, patients experience a primary progressive disease course with no superimposed neuro-inflammatory bouts, referred to as primary progressive MS [4]. Thus, approximately 95% of patients are affected by extensive neurodegeneration at some point in the disease course.
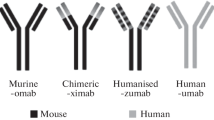
However, no therapies are currently available that simultaneously dampen the inflammatory reactions and also protect the axons from degeneration [5]. Over the last 20 years, several compounds have been well established in the treatment regimen of MS patients: interferon-β, glatiramer acetate, teriflunomide, dimethyl fumarate, natalizumab, fingolimod, alemtuzumab, and mitoxantrone [6]. All of these have mainly immunomodulatory or immunosuppressive properties and are therefore more effective for the treatment of early MS disease stages where acute inflammation is predominant [7, 8]. Although interferon-β and mitoxantrone were investigated in progressive MS, final conclusions about their effectiveness in treating this chronic disease stage are still unclear and the effect is at best moderate [9, 10]. In 2016, another compound, daclizumab was approved as a humanized immunoglobulin G (IgG) against the interleukin-2 receptor-α chain on T cells [11, 12]. Ocrelizumab, a humanized anti-CD20 IgG [13, 14], is at the edge of clinical approval. Ocrelizumab would be the first treatment option for primary progressive MS (reviewed in [15]).
This is a breakthrough, in particular with regard to the disappointing trials during the last 25 years assessing the effectiveness of drug candidates in progressive MS stages [16]. Important reasons for the failure of these trials include that they only targeted the adaptive immune mechanisms. Besides that, the design of these studies was not suited to identify effects in patients with progressive MS [17]. The difficulties in testing potential therapies for progressive MS are reflected by the fact that only a small number of current clinical MS trials investigate interventions for the progressive stage. This is shown by a systematic search on clinicaltrials.gov detecting as few as 17.3% of all studies investigating such interventions (126 of 727 studies, search string: “Multiple Sclerosis OR MS”, last search date: 1 March, 2016). A further complication at the preclinical level is that no proper animal model is available for progressive MS [18]. However, many lessons were learned from preclinical [18] and clinical trials [16]. Additionally, promising new drug candidates are currently in development (reviewed in [19]).
One such candidate, which is in early clinical development for progressive (and relapsing) MS, is an antibody against the protein Nogo-A. In this review, we give a brief overview on this myelin-associated, nerve fiber growth inhibitory protein and its receptors and we summarize its relation to demyelinating, neuro-inflammatory, and neurodegenerative pathology from clinical and preclinical evidence.
2 Multiple Sclerosis Leads to Extensive Neurodegeneration
2.1 Pathogenic Cascade Leading to Neurodegeneration
Axonal and neuronal injuries are common phenomena in acute relapsing MS lesions as shown by histological analysis of MS tissue [20, 21], magnetic resonance imaging [22], and magnetic resonance spectroscopy [23]. The prevailing view is that infiltration of immune cells and subsequent demyelination are responsible for this axonal loss [24].
The early pathological processes trigger a cascade of events, leading to chronic demyelination and neurodegeneration [25], the hallmarks of the secondary progressive disease stage. The chronic inflammation results in microglia and macrophage activation-producing reactive oxygen and nitrogen species (ROS and NOS), which can lead to mitochondrial damage [26, 27] (reviewed in [28]), metabolic stress, protein misfolding, and deceased axonal transport [29, 30]. Accumulating evidence suggests genuine hypoxia as another mechanism contributing to the tissue injury in acute, as well as chronic, MS lesions [31–33].
2.2 Chronic Demyelination Amplifies Neurodegeneration
The demyelinated tissue often fails to successfully repair the myelin, leading to chronically denuded axons [34, 35]. This is in part owing to the failure of oligodendrocyte precursor differentiation and myelination [35]. This chronic demyelination can lead to a lack of support function from the oligodendrocytes/myelin sheaths, which ultimately results in axonal decline [36, 37]. Ion channel redistribution is yet another sequel of chronic demyelination: different neuronal ion channels show redistribution along axons to compensate ionic imbalance, e.g., voltage-gated sodium channels (Nav1.2 and Nav1.6) [38], acid-sensing ion channel 1 (ASIC 1) [39, 40], and transient receptor potential cation channel subfamily M member 4 [41] (reviewed in [42]). This channel redistribution results in ionic imbalance, further perpetuating tissue damage [42].
All these destructive processes can be amplified by pre-existing brain injuries and factors associated with brain aging [25]. Resulting lesions show slow expansion leading to general CNS tissue atrophy [43]. This can result in extensive axonal injury, which can be as high as 70% of axons being destroyed in chronic white matter lesions of severely disabled MS patients [44, 45]. In fact, the progressive neuronal degeneration closely correlates with the progressive neurological decline [46].
2.3 Therapeutic Opportunities
This cascade of pathogenic events culminating in extensive axonal decline offers therapeutic opportunities. One of them is the enhancement of neuronal plasticity and regeneration of neurons and axons. The promotion of remyelination by recruitment of the oligodendrocyte precursor pool is yet another one. Important for therapeutic approaches is that successful remyelination was shown to stop the progressive axonal loss [47, 48].
3 Nogo-A Protein: Its Distribution and Receptors
One of the drug candidates in early clinical development that would be able to induce axonal regeneration and remyelination is an antibody against the neurite outgrowth inhibitory protein Nogo-A [49]. The Nogo-A protein was first characterized as an inhibitory protein for neurite outgrowth in brain and spinal cord myelin in vitro in 1988 [50]; its complementary DNA was cloned in 2000 [51, 52]. It downregulates neuronal growth, stabilizes the CNS wiring, and restricts plasticity in the adult CNS [53]. Nogo-A is a member of the reticulon family and is highly conserved across species. Three isoforms are generated by alternative splicing; A, B, and C, but only Nogo-A has been shown to have inhibitory effects in the CNS. Nogo-A is present in various cell types of the CNS, including oligodendrocytes and neurons [54]. Nogo-A localizes at the cell surface and in the endoplasmic reticulum and can have different membrane topologies with regard to a cytoplasmic vs. extracellular position of the N terminus [55].
Two inhibitory regions have been identified in this 1200-amino acid protein, Nogo-A-Δ20 (amino acids 544–725 in rat Nogo-A) and Nogo-66 (amino acids 1055–1079 in rat Nogo-A, links the two long hydrophobic stretches that span the cell membrane) [49]. The Nogo receptor 1 (NgR1) has been described as a receptor for Nogo-66 [56]. Upon Nogo-A binding, NgR1 associates with the transmembrane proteins leucine rich repeat and Ig-like domain-containing protein 1 (LINGO-1) and p75 or tumor necrosis factor-α receptor superfamily member 19 (TROY) to form a multi-subunit receptor complex [49, 57]. The sphingosine-1-phosphate receptor 2 (S1PR2) is a receptor for Nogo-A-Δ20 [58] (Fig. 1a).
Receptors and downstream signaling of Nogo-A and potential mechanism(s) of Nogo-A antibody therapy in multiple sclerosis (MS). a The myelin-associated protein Nogo-A has two inhibitory regions, Nogo-66 and Nogo-A-Δ20. Nogo-66 binds to Nogo-receptor 1 (NgR1) which forms a complex with leucine rich repeat and Ig-like domain-containing protein 1 (LINGO-1), p75, and/or tumor necrosis factor-α receptor superfamily member 19 (TROY). Sphingosine-1-phosphate receptor 2 (S1PR2) was recently identified as a Nogo-A-Δ20 receptor [58]. b In acute MS lesions, the attack of the myelin sheath by immune cells leads to demyelination. The myelin-associated protein Nogo-A is then present in the myelin debris, potentially limiting axonal/myelin repair in MS plaques. c In acute and chronic MS lesions, neuronal/axonal degeneration can be very prominent. Nogo-A, present in the myelin debris and surrounding myelin sheaths, limits regeneration and compensatory sprouting of these damaged axons. Blocking Nogo-A with antibodies potentially leads to regeneration of axons and restoration of compensatory neuronal circuits. d Signaling cascade upon binding of Nogo-A to its cognate receptors: neuronal S1PR2 as well as the NgR1-LINGO-1-p75/TROY receptor complex activates RhoA and RhoA-associated kinase (ROCK). Different downstream targets including the phosphorylation of collapsin response mediator protein 2 (CRMP-2) [83] lead to a disassembly of the actin and microtubule system with subsequent detrimental collapse of the growth cone. e After demyelination, oligodendrocyte precursor cells are recruited and differentiate into oligodendrocytes to remyelinate the naked axon. As suggested by recent evidence [67], Nogo-A seems to limit the myelinogenic potential of oligodendrocytes: oligodendrocytes from Nogo-A-deficient mice can form an increased amount of myelin internodes. Nogo-A-mediated repulsive interactions would lead to spatial segregation at Ranvier node formation. Remyelinated myelin sheaths are characteristically thinner than original myelin sheaths. MLCII myosin light chain 2
Although Nogo-66 and Nogo-A-Δ20 bind to distinct receptors, it was demonstrated that they modulate the same intracellular signaling pathway: ras homolog gene family member A (RhoA) and rho-associated protein kinase (ROCK) [57] (Fig. 1d). The intracellular changes induced by the signaling cascade include reduced growth of actin filaments, collapse of the growth cone, destabilization of microtubules, and downregulation of growth genes in the neuronal cell body [57, 59]. Paired Ig-like receptor B is an alternative receptor for Nogo-66. This receptor is expressed in many parts of the CNS at low levels but its relevance for signaling might be restricted to neural development or after ischemia [60].
LINGO-1 is a co-receptor for NgR1 upon Nogo-A binding (Fig. 1a). It is expressed exclusively on oligodendrocytes and neurons and it is upregulated upon CNS injury across various animal models and human CNS diseases [61]. Antagonization of LINGO-1 has been shown to be beneficial in various animal models in terms of axonal regeneration and remyelination [61]. However, as LINGO-1 is distributed more widely in the CNS than NgR1 [62], other ligands might exist besides Nogo-A and NgR1. Comparison of the effects of LINGO-1 neutralization to those of Nogo-A neutralization is therefore of great interest (Table 1). Moreover, Nogo-A, like LINGO-1, is largely expressed in the CNS, representing a mostly CNS-specific drug target.
Besides Nogo-A, myelin-associated glycoprotein and oligodendrocyte-myelin glycoprotein are also ligands for NgR1 and reported to have neurite growth inhibitory activity in vitro. Not much is known about their in vivo functions in the context of neurite growth [63]. Nogo-A is by far the best studied, and its extensive characterization suggests an important role during different neurodegenerative disorders [64, 65].
4 Nogo-A is an Inhibitor of Nerve Fiber Growth and Regeneration
In neuronal development, Nogo-A acts as a regulator of axonal growth, branching, and fasciculation [66]. It also regulates the internode length and Ranvier node formation during myelin formation [67]. Nogo-A is involved in the termination of the critical plastic period in several regions of the postnatal CNS [49, 53]. In the adult CNS, Nogo-A takes part in the stabilization of the structure and wiring of the CNS by restricting neurite growth to short distances. However, this growth restricting function of Nogo-A also inhibits regenerative and longer-range plastic events following injury or disease [53]. Suppressing the actions of Nogo-A by different means enhances plasticity and axonal regeneration, e.g., in rodent and monkey models of spinal cord injury and stroke; genetic Nogo-deletion, Nogo-neutralizing antibodies, auto-immunization with Nogo-A, and a blocking Nogo receptor fusion protein or a Nogo receptor blocking peptide have been used in these animal models (reviewed in [53]).
Throughout these studies, Nogo-A neutralization enhanced regrowth and compensatory sprouting of functionally important fiber systems such as the corticospinal tract as well as anatomical plasticity on different levels. At the same time, animals consistently showed significant functional recovery, e.g., in locomotion, skilled stepping over irregular ladders, and balance or fine forepaw movements during grasping [53]. These beneficial effects appeared within 2–4 weeks after the treatment and, at least in spinal cord injury, seemed to be more efficient in acute settings [68]. However, blocking Nogo-A with the NgR1-Fc fusion protein enhanced anatomical and functional recovery also when administered several months after spinal cord trauma [69]. In stroke, even treatment in chronic stages after large ischemic cortical strokes led to improved functional recovery and increased axonal sprouting [70]. Furthermore, the antibody treatment also had positive effects on stroke recovery in aged rats [71].
Of note, transient pharmacogenetic blockade of the newly grown midline-crossing corticospinal fibers after stroke abrogated the recovered grasping function [72]. This shows that newly grown fibers are indeed responsible for improved recovery after anti-Nogo-A antibody treatment. Especially important regarding the future human use of these antibodies are the observations that neurological adverse effects such as enhanced pain, spasticity, or epileptic attacks have never been observed in these studies [73]. Several antibodies with different epitope specificities for the rat and human Nogo-A have been used in preclinical and clinical research. Table 2 summarizes these antibodies, their epitopes, and types.
Another function of Nogo-A, potentially contributing to its ability to enhance recovery from CNS injury, is its involvement in synaptic plasticity. These processes are mainly dependent on neuronal Nogo-A. Dendritic as well as synaptic spine architecture was shown to be influenced by Nogo-A and NgR1 signaling in the hippocampus [74]. Long-term potentiation of hippocampal and cortical synapses was increased when Nogo-A or NgR1 was inactivated [75–77]. Furthermore, genetic deletion of the Nogo receptor family NgR1, NgR2, and NgR3 revealed an important role of Nogo-A as a brake on synapse formation in development [78].
5 Role of Nogo-A in Neuro-Inflammatory and Demyelinating Conditions
In recent years, the idea has been presented that Nogo-A may play a regulatory role in animal models of neuroinflammatory diseases and may thus be considered a potential therapeutic target for MS. Its abundant presence in myelin and myelin debris around acute and chronic MS lesions could restrict axonal regrowth as well as efficient myelin repair (Fig. 1). This hypothesis is supported by a considerable number of studies from different laboratories using different animal models of MS and strategies for Nogo-A neutralization. Moreover, there are supportive data on Nogo-A in MS patients. For a comprehensive molecular review on Nogo-A and MS, see Lee and Petratos [79].
Pioneering work by Karnezis and colleagues showed an important role of Nogo-A in the mouse model of autoimmune inflammatory CNS disease, experimental autoimmune encephalomyelitis (EAE) [80]. They suppressed Nogo-A either by vaccination against Nogo-A or gene deletion. They found lower clinical scores and slower disease progression as well as reduced histological inflammation, demyelination, and axonal damage. The reduced axonal pathology correlated well with the reduction in the severity of clinical disability and EAE progression. At the immunological level, vaccination with Nogo-A induced a shift in the production from proinflammatory T helper-1 to anti-inflammatory T helper-2 cells. However, the latter observation has not been reproduced to date.
The immune response to vaccination of EAE-susceptible mice with Nogo-A peptides, representing different epitopes of the extracellular Nogo-A domain Nogo-66, revealed that some epitopes were encephalitogenic while others ameliorated established EAE [81]. These effects appeared to be mediated by Nogo-66-specific T cells.
Fontoura and colleagues [82] found that intravenous (i.v.) application of anti-Nogo-A IgG after EAE induction with myelin oligodendrocyte glycoprotein (MOG) led to the prevention of disease onset for up to 12 days after the treatment was stopped. Compared with phosphate-buffered saline (PBS) or control IgG injections, the anti-Nogo-A IgG treatment decreased the incidence and severity of EAE and also blocked the progression of the disease.
Blocking Nogo-A by means of neutralizing antibodies has also been shown to enhance recovery in established neuro-inflammation [83]. An improved clinical as well as anatomical outcome, i.e., reduced levels of axonal degeneration shown with the marker P-CRMP-2, was shown after therapeutic administration of anti-Nogo-A antibodies during the course of EAE in mice.
Better clinical outcome in EAE was also observed by using a different method of Nogo-A suppression, namely by genetic knock down with small interfering RNA [84]. In vitro and in vivo, Nogo-A knock down led to higher levels of the growth-associated protein 43 in neurons [85]. This indicates that axonal repair was enhanced by suppressing Nogo-A. Interestingly, using this gene-knock-out approach, the proliferation and cytokine production of myelin-specific T cells were unaltered, suggesting that enhanced axonal regeneration could be the mechanism for the improved clinical recovery. This could be in line with observations in spinal cord injury and stroke models in which Nogo-A-suppression led to enhanced fiber growth and plasticity. Axonal regeneration could, at least in part, be responsible for functional recovery at an early MS disease stage, e.g., in the remission phases [86]. These plastic compensatory strategies of the CNS, e.g., by sprouting of surviving axons, formation of compensatory circuits, or recruitment of reserve pathways, have been shown in animal models of stroke [72], spinal cord injury [87], as well as neuro-inflammatory pathology [88].
Interestingly, Nogo-A mRNA and protein levels were observed to be inversely correlated with those of the axonal growth marker, growth-associated protein 43 at different stages of the course of EAE [89]. This work showed that Nogo-A mRNA expression is reduced at preclinical and acute phases, which is followed by upregulation of mRNA and protein during the chronic EAE stage. In contrast, growth-associated protein 43 was upregulated during acute EAE and downregulated in chronic EAE, often in close spatial proximity to Nogo-A mRNA/protein. The reduction in Nogo-A expression within an active inflammatory lesion therefore could facilitate axonal sprouting, whereas the higher levels of Nogo-A in the chronic lesions could impede neurite growth.
The pre-clinical assessment of potential therapies for progressive MS is hampered by the fact that no animal models are available for mimicking the progressive MS disease course [18]. Most models fail to reproduce the complexity of the processes defining progressive MS, e.g., widespread microglia activation, chronic oxidative injury, subpial demyelination, and cortical pathology at the same time [18]. Moreover, some models that claim to present a progressive phenotype, e.g., immunizing Biozzi antibody high (ABH) mice with spinal cord homogenate and complete Freund’s adjuvant [90], reflect stable disease on a high level of disability rather than true progression.
Chronic demyelination is an important hallmark of progressive MS. Therefore, toxin-induced demyelination models are increasingly used to define therapies aiming at enhancing remyelination, e.g., lysolecithin, ethidium bromide, or cuprizone [91]. Results from such studies suggest that Nogo-A may also be involved in myelin repair in addition to possible immune-modulatory and regeneration-enhancing effects. Studies on myelin development in vitro and in vivo [67] showed that, by acting as a repulsive cue, Nogo-A influences and regulates the periodic non-overlapping arrangement of myelin internodes along axons as well as their number and inter-nodal distances [67]. By genetically deleting Nogo-A in oligodendrocytes, the relevance of this hypothesis was tested in vivo in spinal lysolecithin-induced demyelinating lesions. Interestingly, Nogo-A-deficient mice showed enhanced myelin repair compared with control mice. The amount of myelinating oligodendrocytes was unchanged within the demyelinated lesion. This strongly supports the hypothesis of an increased myelinogenic potential of the Nogo-A-deficient oligodendrocytes, i.e., Nogo-A-deficient oligodendrocytes can form more myelin internodes around axons. Therefore, the neutralization of Nogo-A by antibodies can potentially be exploited to enhance remyelination. The involvement of Nogo-A and its receptors during myelin formation is supported by several other developmental in vitro and in vivo studies [92–94].
In a clinically relevant approach using antibody-mediated Nogo-A-neutralization, subsequent to lysolecithin lesions in adult rat spinal cords, our laboratory obtained evidence for enhanced myelin repair as a consequence of this treatment (unpublished observations). Of note, the antibody-mediated neutralization of LINGO-1, a component of the NgR1-Nogo-A receptor complex, also led to enhanced oligodendrocyte precursor cell differentiation during primary myelination as well as during myelin repair in different in vivo MS animal models [95–97]. In contrast, over-expression of LINGO-1 impeded this precursor differentiation and abolished myelin repair [98]. These (re-)myelination promoting effects are potentially also mediated by RhoA downstream signaling [95], but other signaling cascades were also shown to be involved [98] (Table 1).
The potential of antibodies directed against myelin antigens to promote remyelination has already been shown (reviewed in [99]). Murine as well as human anti-myelin antibodies were able to boost remyelination in rodent MS models. The proposed mechanisms involved either removal of myelin debris after injury or direct effects on oligodendrocyte precursor cells.
6 Role of Nogo-A in Multiple Sclerosis
In addition to these preclinical studies, Nogo-A has also been examined in MS. Nogo-A was found to be upregulated in surviving oligodendrocytes in chronic active demyelinating lesions of MS patients [100]. This is consistent with findings in EAE mice [89]. Elevated serum and cerebrospinal fluid autoantibody levels against the large N-terminal domain of Nogo-A have been found in blood samples from MS patients [101], but anti-Nogo-A antibodies exist also in healthy controls. The levels of these antibodies were increased in RRMS patients compared with chronic-progressive MS patients. Additionally, these anti-Nogo antibodies were more frequent in younger MS patients compared with older MS patients [101]. The role(s) of these Nogo-A antibodies is currently unclear; they could reflect the ongoing auto-inflammatory processes against myelin including Nogo-A. Whether some of these antibodies could participate in reparative functions myelin or axons remains to be determined.
7 Nogo-A Antibodies in Clinical Trials
The experimental data from studies using different MS animal models and the exploratory data from MS patients summarized above suggest Nogo-A antibodies as a potential therapeutic agent for the treatment of RRMS and/or progressive forms of MS. Two phase I studies for Nogo-A antibodies were recently conducted in patients with RRMS (ClinicalTrials.gov, NCT01424423 and NCT01435993). Both studies, with a very limited number of patients, have been terminated, but their results are not fully published yet. In its online clinical study register, GlaxoSmithKline states that the reasons for termination were unrelated to safety issues of the antibody treatment.
Two phase I studies to assess the acute safety, tolerability, and pharmacokinetics of anti-Nogo A antibodies were successfully completed in two other CNS diseases: one after intrathecal administration of anti-Nogo-A antibodies over 30 days in patients with acute spinal cord injury (NCT00406016; Kucher et al., in preparation), and another using very high doses of intravenously infused antibodies in patients with amyotrophic lateral sclerosis (NCT00875446) [102]. Both of these trials showed excellent safety and tolerance of the Nogo-A antibody treatment. A phase II study including more than 300 patients with amyotrophic lateral sclerosis who were randomized to anti-Nogo-A antibodies or placebo further showed that there was no apparent imbalance between treatment groups in adverse events (NCT01753076). Placebo-controlled, multi-centered, phase II proof-of-principle studies are currently in preparation for spinal cord injury.
An antibody against a Nogo-66 receptor-associated component, LINGO-1 (opicinumab), has been tested in phase I and II studies in patients with RRMS/progressive MS or with optic neuritis. High doses of i.v. antibodies were well tolerated [103]. In a phase II study in patients with acute optic neuritis treated with anti-LINGO-1, vision did not improve after 8 months, but the velocity of nerve conduction, as measured by visually evoked potentials, was up to 41% less reduced compared with placebo treatment [104]. As the latency of the visually evoked potentials primarily reflects intact myelin sheaths, these data are interpreted as a sign of preserved myelin sheaths or remyelination. The failure to meet the secondary outcome of attenuation of the loss of retinal nerve fibers by optical coherence tomography indicates that retinal neurons and/or axons were lost despite the anti-LINGO-1 treatment. However, these interpretations are preliminary and await further confirmation.
A very recent press release from a phase II study using monthly i.v. anti-LINGO-1 for relapsing and progressive MS did not meet its primary endpoint, a multicomponent analysis evaluating motor and cognitive function as well as disability (http://media.biogen.com/press-release/investor-relations/biogen-reports-top-line-results-phase-2-study-opicinumab-anti-lingo). The opicinumab infusions were combined with a concurrent interferon-β add-on therapy. A potential reason for this failure despite promising pre-clinical results could be the ambitious and complex trial design. It used a complex multicomponent readout as a primary endpoint including the Timed 25-Foot Walk, the 9-Hole Peg Test, and the Expanded Disability Status Scale. The latter two tests have received criticism for being insensitive outcome measures for progressive MS trials [16]. The Expanded Disability Status Scale is an ordinal scale; therefore, the statistical comparison between contiguous scores is insensitive. Moreover, scores can show high differences between different raters [105]. The 9-Hole Peg Test has floor and ceiling effects, limiting its use for progressive MS trials. The patient collective was also very heterogeneous consisting of RRMS and secondary progressive MS patients, further complicating final interpretations of the preliminary published study results. Full study results including subgroup analysis of RRMS vs. secondary progressive MS patients will be available in the next few months and will bring further clarification.
8 Clinical Aspects of Nogo-A Antibody Therapy
8.1 Requirements for Novel Multiple Sclerosis Therapies
As summarized above, a number of trials to achieve a therapeutic effect in progressive MS are currently ongoing. Experience from previous trials points to different requirements to be fulfilled by new therapies [25]: first, on-going or new inflammatory activity needs to be blocked and, if possible, the compartmentalized intra-CNS chronic activation of microglia should be inhibited as well. Second, neuro- and/or myelin protection should be achieved to inhibit the above-mentioned mechanisms that contribute to neuronal decline in the progressive disease stage. Third, given the presumable intrathecal compartmentalization of inflammation in the progressive stage, a potential drug needs to reach the CNS tissue despite a mostly intact BBB [25, 106], e.g., by intrathecal application [107], or delivery into the CSF space via a shuttle system. Intrathecal application leads to locally maximized drug concentrations with low systemic exposure and can therefore be expected to have minimal systemic side effects [107]. Fourth, besides immunomodulation and neuro-/myelin protection, the regenerative effects of treatments such as anti-Nogo-A should foster repair as much as possible in this phase of disease. Fifth, the different pathogenic mechanisms in the progressive disease may require combinatorial therapies tackling the different targets of the degenerative process as well as various repair processes such as axonal sprouting and myelin repair [16]. Sixth, and critical for testing the effects of such single or combination therapies, the most informative patient subgroups should be identified, and suitable trial designs including imaging readouts and biomarkers for degeneration and repair need to be applied.
Under these assumptions, neutralization of Nogo-A seems a feasible and promising therapeutic strategy for the progressive disease stage of MS. As summarized above, a number of pre-clinical studies, mainly in the rodent EAE and lysolecithin model, and different ways of inhibiting Nogo-A showed functional as well as anatomical recovery in terms of axonal sparing, sprouting, and myelin repair [67, 80, 83, 84]. One study also showed a beneficial immunomodulatory function of Nogo-A inhibition shifting the cytokine profile of T cells from a pro- to an anti-inflammatory one [80]. An anti-Nogo-A therapy could therefore tackle two or even three of the major pathogenic hallmarks of MS (Fig. 1b, c, e). NgR1/Lingo-1 inhibition has also been proposed as an approach to abolish Nogo-A-signaling in MS [79]. Disappointing results of clinical trials investigating growth factors such as brain-derived neurotrophic factor (BDNF), nerve growth factor (NGF), ciliary neurotrophic factor (CNTF), platelet-derived growth factor (PDGF), or glial cell-derived neurotrophic factor (GDNF) suggest that targets should be tissue and cell type specific. None of the other MS drugs, either still in development or already clinically approved, have CNS-specific targets. Therefore, both Nogo-A antibodies and LINGO-1 antibodies are promising agents owing to their high CNS target specificity. In addition, it seems plausible that Nogo-A is present in the myelin debris in MS plaques prior to macrophage clearance, thereby limiting the potential of these plaques for axonal repair. This myelin debris-associated Nogo-A could in fact be an important target of the Nogo-A antibodies to achieve axonal repair in MS. Moreover, the engulfment of myelin debris, potentially ameliorated through opsonization by Nogo-A antibodies, could enhance remyelination [79].
8.2 Pharmacological Aspects of Nogo-A Antibody Therapy
Perhaps the greatest concern of the Nogo-A antibody therapy is its potential limited access to the CNS through the BBB, especially in progressive MS in which the disease process is compartmentalized behind a mainly intact BBB [25].
Preclinical data from a rat stroke model in our laboratory revealed that about 0.1% of a blood infused anti-Nogo-A antibody reached the CSF 7 days after an i.v. bolus infusion (unpublished observations). This is consistent with trials in mouse EAE using IgG [108] and in naive rats using an anti-LINGO-1 IgG [109].
Data from clinical trials support this notion. A study investigating the CSF concentration of rituximab after i.v. application in two MS patients (one with progressive disease) revealed 0.1–0.25% of this antibody being present in the CSF 24 weeks after application [110]. More evidence comes from clinical trials with LINGO-1 IgG [111] and the rHIgM22 antibody [112]. Data from a pharmacokinetic study with rHIgM22 show that it was found in the brain of 14/14 patients after 2 days and in 5/12 patients after 29 days following an i.v. infusion of a single dose. This IgM antibody is five times larger than IgG such as the LINGO-1 or Nogo-A antibody. In the phase I study with i.v. anti-LINGO-1 in 72 healthy volunteers or in 47 patients with either relapsing or progressive MS, doses of ≥10 mg/kg resulted in CSF concentrations of this antibody that were associated with 90% of the maximum remyelination effect in rat remyelination studies [103]. It seems therefore plausible that sufficient amounts of antibodies can cross the BBB when very high i.v. doses are administered.
8.3 Potential ‘Off-Target’ Effects of Nogo-A Antibodies
Both animal models and human observations have linked Nogo-A and NgR1 to schizophrenia (reviewed in [113]). Genetic association studies have identified Nogo-A and NgR as risk polymorphisms for neuropsychiatric disorders such as schizophrenia [114]. Besides this, mice lacking Nogo-A or NgR1 demonstrate behavioral phenotypes reflecting aspects of schizophrenia, e.g., deficits in prepulse inhibition [115, 116]. Neurodevelopmental mechanisms seem to be responsible for this. In line with this, schizophrenic phenotypes have never been observed in rodents [115, 117] or primates [73] during or after therapeutic Nogo-A antibody application.
Nogo-A restricts neuronal plasticity and fiber growth in the adult CNS. Inhibition of this protein by antibodies could therefore potentially lead to aberrant fiber growth and wiring causing, e.g., chronic pain or dyskinesia. These pathologies were, however, not observed in the phase I trials for amyotrophic lateral sclerosis [102] and spinal cord injury (NCT00406016; Kucher et al., in preparation) or in adult spinal cord-injured rats [68] or primates [73] undergoing Nogo-A antibody therapy.
9 Conclusions
Axonal degeneration and chronic demyelination are hallmarks of chronic slowly progressing MS. Preclinical studies in rodent EAE models showed that suppression of the growth inhibitory CNS protein Nogo-A, e.g., by neutralizing anti-Nogo-A antibodies, enhances axonal sprouting and regeneration as well as the formation of new functional circuits. Additionally, myelin repair was enhanced after genetic deletion of Nogo-A in the lysolecithin myelin lesion model. Based on these data, anti-Nogo-A antibodies could be a promising new therapy for relapsing as well as progressive MS. Phase I and II studies with anti-Nogo-A antibodies are currently underway for other neurological indications. The time seems ripe to test these antagonists of the Nogo-A–Nogo receptor pathway as novel therapeutic agents for relapsing and in particular progressive MS.
References
World Health Organization. Multiple Sclerosis International Federation. Atlas: Multiple Sclerosis Resources in the World 2008. Geneva: World Health Organization; 2008. p. 13–7.
Trapp BD, Nave KA. Multiple sclerosis: an immune or neurodegenerative disorder? Annu Rev Neurosci. 2008;31:247–69.
Sawcer S, Hellenthal G, Pirinen M, et al. Genetic risk and a primary role for cell-mediated immune mechanisms in multiple sclerosis. Nature. 2011;476(7359):214–9.
Tallantyre EC, Bo L, Al-Rawashdeh O, et al. Greater loss of axons in primary progressive multiple sclerosis plaques compared to secondary progressive disease. Brain. 2009;132(Pt 5):1190–9.
Fox RJ, Thompson A, Baker D, et al. Setting a research agenda for progressive multiple sclerosis: the International Collaborative on Progressive MS. Mult Scler (Houndmills, Basingstoke, England). 2012;18(11):1534–40.
Torkildsen O, Myhr KM, Bo L. Disease-modifying treatments for multiple sclerosis: a review of approved medications. Eur J Neurol. 2016;23(Suppl. 1):18–27.
Coles AJ, Cox A, Le Page E, et al. The window of therapeutic opportunity in multiple sclerosis: evidence from monoclonal antibody therapy. J Neurol. 2006;253(1):98–108.
Hauser SL, Chan JR, Oksenberg JR. Multiple sclerosis: prospects and promise. Ann Neurol. 2013;74(3):317–27.
Kappos L, Polman C, Pozzilli C, et al. Final analysis of the European multicenter trial on IFNbeta-1b in secondary-progressive MS. Neurology. 2001;57(11):1969–75.
Hartung HP, Gonsette R, Konig N, et al. Mitoxantrone in progressive multiple sclerosis: a placebo-controlled, double-blind, randomised, multicentre trial. Lancet. 2002;360(9350):2018–25.
Kappos L, Wiendl H, Selmaj K, et al. Daclizumab HYP versus interferon beta-1a in relapsing multiple sclerosis. N Engl J Med. 2015;373(15):1418–28.
Gold R, Giovannoni G, Selmaj K, et al. Daclizumab high-yield process in relapsing-remitting multiple sclerosis (SELECT): a randomised, double-blind, placebo-controlled trial. Lancet. 2013;381(9884):2167–75.
Montalban X, Hemmer B, Rammohan K, et al. Efficacy and safety of ocrelizumab in primary progressive multiple sclerosis: results of the phase III double-blind, placebo-controlled ORATORIO study (S49.001). Neurology. 2016;86(16 Suppl.):S49-001.
Hauser S, Comi G, Hartung H-P, et al. Efficacy and safety of ocrelizumab in relapsing multiple sclerosis-results of the interferon-beta-1a-controlled, double-blind, phase III OPERA I and II studies. Mult Scler. 2015;61–2.
McGinley MP, Moss BP, Cohen JA. Safety of monoclonal antibodies for the treatment of multiple sclerosis. Exp Opin Drug Saf. 2017;16(1):89–100.
Ontaneda D, Fox RJ, Chataway J. Clinical trials in progressive multiple sclerosis: lessons learned and future perspectives. Lancet Neurol. 2015;14(2):208–23.
Ransohoff RM, Hafler DA, Lucchinetti CF. Multiple sclerosis: a quiet revolution. Nat Rev Neurol. 2015;11(3):134–42.
Lassmann H, Bradl M. Multiple sclerosis: experimental models and reality. Acta Neuropathol. 2016. doi:10.1007/s00401-016-1631-4.
Shirani A, Okuda DT, Stuve O. Therapeutic advances and future prospects in progressive forms of multiple sclerosis. Neurotherapeutics. 2016;13(1):58–69.
Trapp BD, Peterson J, Ransohoff RM, et al. Axonal transection in the lesions of multiple sclerosis. N Engl J Med. 1998;338(5):278–85.
Stadelmann C. Multiple sclerosis as a neurodegenerative disease: pathology, mechanisms and therapeutic implications. Curr Opin Neurol. 2011;24(3):224–9.
Weinshenker BG. The natural history of multiple sclerosis: update 1998. Semin Neurol. 1998;18(3):301–7.
Filippi M, Rocca MA, De Stefano N, et al. Magnetic resonance techniques in multiple sclerosis: the present and the future. Arch Neurol. 2011;68(12):1514–20.
Criste G, Trapp B, Dutta R. Axonal loss in multiple sclerosis: causes and mechanisms. Handb Clin Neurol. 2014;122:101–13.
Mahad DH, Trapp BD, Lassmann H. Pathological mechanisms in progressive multiple sclerosis. Lancet Neurol. 2015;14(2):183–93.
Fischer MT, Sharma R, Lim JL, et al. NADPH oxidase expression in active multiple sclerosis lesions in relation to oxidative tissue damage and mitochondrial injury. Brain. 2012;135(Pt 3):886–99.
Campbell GR, Kraytsberg Y, Krishnan KJ, et al. Clonally expanded mitochondrial DNA deletions within the choroid plexus in multiple sclerosis. Acta Neuropathol. 2012;124(2):209–20.
Witte ME, Mahad DJ, Lassmann H, van Horssen J. Mitochondrial dysfunction contributes to neurodegeneration in multiple sclerosis. Trends Mol Med. 2014;20(3):179–87.
Dendrou CA, Fugger L, Friese MA. Immunopathology of multiple sclerosis. Nat Rev Immunol. 2015;15(9):545–58.
Sorbara CD, Wagner NE, Ladwig A, et al. Pervasive axonal transport deficits in multiple sclerosis models. Neuron. 2014;84(6):1183–90.
Davies AL, Desai RA, Bloomfield PS, et al. Neurological deficits caused by tissue hypoxia in neuroinflammatory disease. Ann Neurol. 2013;74(6):815–25.
Desai RA, Davies AL, Tachrount M, et al. Cause and prevention of demyelination in a model multiple sclerosis lesion. Ann Neurol. 2016;79(4):591–604.
Lassmann H. Demyelination and neurodegeneration in multiple sclerosis: the role of hypoxia. Ann Neurol. 2016;79(4):520–1.
Patani R, Balaratnam M, Vora A, Reynolds R. Remyelination can be extensive in multiple sclerosis despite a long disease course. Neuropathol Appl Neurobiol. 2007;33(3):277–87.
Franklin RJ, Gallo V. The translational biology of remyelination: past, present, and future. Glia. 2014;62(11):1905–15.
Nave KA. Myelination and support of axonal integrity by glia. Nature. 2010;468(7321):244–52.
Franklin RJ, Ffrench-Constant C, Edgar JM, Smith KJ. Neuroprotection and repair in multiple sclerosis. Nat Rev Neurol. 2012;8(11):624–34.
Craner MJ, Newcombe J, Black JA, et al. Molecular changes in neurons in multiple sclerosis: altered axonal expression of Nav1.2 and Nav1.6 sodium channels and Na+/Ca2+ exchanger. Proc Natl Acad Sci USA. 2004;101(21):8168–73.
Vergo S, Craner MJ, Etzensperger R, et al. Acid-sensing ion channel 1 is involved in both axonal injury and demyelination in multiple sclerosis and its animal model. Brain. 2011;134(Pt 2):571–84.
Friese MA, Craner MJ, Etzensperger R, et al. Acid-sensing ion channel-1 contributes to axonal degeneration in autoimmune inflammation of the central nervous system. Nat Med. 2007;13(12):1483–9.
Schattling B, Steinbach K, Thies E, et al. TRPM4 cation channel mediates axonal and neuronal degeneration in experimental autoimmune encephalomyelitis and multiple sclerosis. Nat Med. 2012;18(12):1805–11.
Friese MA, Schattling B, Fugger L. Mechanisms of neurodegeneration and axonal dysfunction in multiple sclerosis. Nat Rev Neurol. 2014;10(4):225–38.
Frischer JM, Weigand SD, Guo Y, et al. Clinical and pathological insights into the dynamic nature of the white matter multiple sclerosis plaque. Ann Neurol. 2015;78(5):710–21.
Mews I, Bergmann M, Bunkowski S, et al. Oligodendrocyte and axon pathology in clinically silent multiple sclerosis lesions. Mult Scler. 1998;4(2):55–62.
Bjartmar C, Kidd G, Mork S, et al. Neurological disability correlates with spinal cord axonal loss and reduced N-acetyl aspartate in chronic multiple sclerosis patients. Ann Neurol. 2000;48(6):893–901.
Sospedra M, Martin R. Immunology of multiple sclerosis. Ann Rev Immunol. 2005;23:683–747.
Dubois-Dalcq M, Ffrench-Constant C, Franklin RJ. Enhancing central nervous system remyelination in multiple sclerosis. Neuron. 2005;48(1):9–12.
Wootla B, Denic A, Watzlawik JO, et al. Antibody-mediated oligodendrocyte remyelination promotes axon health in progressive demyelinating disease. Mol Neurobiol. 2016;53(8):5217–28.
Schwab ME. Functions of Nogo proteins and their receptors in the nervous system. Nat Rev Neurosci. 2010;11(12):799–811.
Caroni P, Schwab ME. Antibody against myelin-associated inhibitor of neurite growth neutralizes nonpermissive substrate properties of CNS white matter. Neuron. 1988;1(1):85–96.
GrandPre T, Nakamura F, Vartanian T, Strittmatter SM. Identification of the Nogo inhibitor of axon regeneration as a reticulon protein. Nature. 2000;403(6768):439–44.
Chen MS, Huber AB, van der Haar ME, et al. Nogo-A is a myelin-associated neurite outgrowth inhibitor and an antigen for monoclonal antibody IN-1. Nature. 2000;403(6768):434–9.
Schwab ME, Strittmatter SM. Nogo limits neural plasticity and recovery from injury. Curr Opin Neurobiol. 2014;27:53–60.
Huber AB, Weinmann O, Brosamle C, et al. Patterns of Nogo mRNA and protein expression in the developing and adult rat and after CNS lesions. J Neurosci. 2002;22(9):3553–67.
Dodd DA, Niederoest B, Bloechlinger S, et al. Nogo-A, -B, and -C are found on the cell surface and interact together in many different cell types. J Biol Chem. 2005;280(13):12494–502.
Wang KC, Koprivica V, Kim JA, et al. Oligodendrocyte-myelin glycoprotein is a Nogo receptor ligand that inhibits neurite outgrowth. Nature. 2002;417(6892):941–4.
Nash M, Pribiag H, Fournier AE, Jacobson C. Central nervous system regeneration inhibitors and their intracellular substrates. Mol Neurobiol. 2009;40(3):224–35.
Kempf A, Tews B, Arzt ME, et al. The sphingolipid receptor S1PR2 is a receptor for Nogo-a repressing synaptic plasticity. PLoS Biol. 2014;12(1):e1001763.
Montani L, Gerrits B, Gehrig P, et al. Neuronal Nogo-A modulates growth cone motility via Rho-GTP/LIMK1/cofilin in the unlesioned adult nervous system. J Biol Chem. 2009;284(16):10793–807.
Gou X, Zhang Q, Xu N, et al. Spatio-temporal expression of paired immunoglobulin-like receptor-B in the adult mouse brain after focal cerebral ischaemia. Brain Inj. 2013;27(11):1311–5.
Mi S, Pepinsky RB, Cadavid D. Blocking LINGO-1 as a therapy to promote CNS repair: from concept to the clinic. CNS Drugs. 2013;27(7):493–503.
Barrette B, Vallieres N, Dube M, Lacroix S. Expression profile of receptors for myelin-associated inhibitors of axonal regeneration in the intact and injured mouse central nervous system. Mol Cell Neurosci. 2007;34(4):519–38.
Fujita Y, Yamashita T. Axon growth inhibition by RhoA/ROCK in the central nervous system. Frontiers Neurosci. 2014;8:338.
Teng FY, Tang BL. Why do Nogo/Nogo-66 receptor gene knockouts result in inferior regeneration compared to treatment with neutralizing agents? J Neurochem. 2005;94(4):865–74.
Lee JK, Geoffroy CG, Chan AF, et al. Assessing spinal axon regeneration and sprouting in Nogo-, MAG-, and OMgp-deficient mice. Neuron. 2010;66(5):663–70.
Schmandke A, Schmandke A, Schwab ME. Nogo-A: multiple roles in CNS development, maintenance, and disease. Neuroscientist. 2014;20(4):372–86.
Chong SY, Rosenberg SS, Fancy SP, et al. Neurite outgrowth inhibitor Nogo-A establishes spatial segregation and extent of oligodendrocyte myelination. Proc Natl Acad Sci USA. 2012;109(4):1299–304.
Gonzenbach RR, Zoerner B, Schnell L, et al. Delayed anti-nogo-a antibody application after spinal cord injury shows progressive loss of responsiveness. J Neurotrauma. 2012;29(3):567–78.
Wang X, Duffy P, McGee AW, et al. Recovery from chronic spinal cord contusion after Nogo receptor intervention. Ann Neurol. 2011;70(5):805–21.
Tsai SY, Papadopoulos CM, Schwab ME, Kartje GL. Delayed anti-nogo-a therapy improves function after chronic stroke in adult rats. Stroke. 2011;42(1):186–90.
Markus TM, Tsai SY, Bollnow MR, et al. Recovery and brain reorganization after stroke in adult and aged rats. Ann Neurol. 2005;58(6):950–3.
Wahl AS, Omlor W, Rubio JC, et al. Neuronal repair. Asynchronous therapy restores motor control by rewiring of the rat corticospinal tract after stroke. Science (New York, NY). 2014;344(6189):1250–5.
Freund P, Schmidlin E, Wannier T, et al. Nogo-A-specific antibody treatment enhances sprouting and functional recovery after cervical lesion in adult primates. Nat Med. 2006;12(7):790–2.
Zagrebelsky M, Schweigreiter R, Bandtlow CE, et al. Nogo-A stabilizes the architecture of hippocampal neurons. J Neurosci. 2010;30(40):13220–34.
Delekate A, Zagrebelsky M, Kramer S, et al. NogoA restricts synaptic plasticity in the adult hippocampus on a fast time scale. Proc Natl Acad Sci. 2011;108(6):2569–74.
Mironova YA, Giger RJ. Where no synapses go: gatekeepers of circuit remodeling and synaptic strength. Trends Neurosci. 2013;36(6):363–73.
Zemmar A, Weinmann O, Kellner Y, et al. Neutralization of Nogo-A enhances synaptic plasticity in the rodent motor cortex and improves motor learning in vivo. J Neurosci. 2014;34(26):8685–98.
Wills ZP, Mandel-Brehm C, Mardinly AR, et al. The nogo receptor family restricts synapse number in the developing hippocampus. Neuron. 2012;73(3):466–81.
Lee JY, Petratos S. Multiple sclerosis: does Nogo play a role? Neuroscientist. 2013;19(4):394–408.
Karnezis T, Mandemakers W, McQualter JL, et al. The neurite outgrowth inhibitor Nogo A is involved in autoimmune-mediated demyelination. Nat Neurosci. 2004;7(7):736–44.
Fontoura P, Ho PP, DeVoss J, et al. Immunity to the extracellular domain of Nogo-A modulates experimental autoimmune encephalomyelitis. J Immunol. 2004;173(11):6981–92.
Fontoura P, Steinman L. Nogo in multiple sclerosis: growing roles of a growth inhibitor. Journal of the neurological sciences. J Neurol Sci. 2006;245(1–2):201–10.
Petratos S, Ozturk E, Azari MF, et al. Limiting multiple sclerosis related axonopathy by blocking Nogo receptor and CRMP-2 phosphorylation. Brain. 2012;135(Pt 6):1794–818.
Yang Y, Liu Y, Wei P, et al. Silencing Nogo-A promotes functional recovery in demyelinating disease. Ann Neurol. 2010;67(4):498–507.
Nikic I, Merkler D, Sorbara C, et al. A reversible form of axon damage in experimental autoimmune encephalomyelitis and multiple sclerosis. Nat Med. 2011;17(4):495–9.
Tomassini V, d’Ambrosio A, Petsas N, et al. The effect of inflammation and its reduction on brain plasticity in multiple sclerosis: MRI evidence. Hum Brain Mapp. 2016;37(7):2431–45.
Bareyre FM, Kerschensteiner M, Raineteau O, et al. The injured spinal cord spontaneously forms a new intraspinal circuit in adult rats. Nat Neurosci. 2004;7(3):269–77.
Kerschensteiner M, Bareyre FM, Buddeberg BS, et al. Remodeling of axonal connections contributes to recovery in an animal model of multiple sclerosis. J Exp Med. 2004;200(8):1027–38.
Theotokis P, Lourbopoulos A, Touloumi O, et al. Time course and spatial profile of Nogo-A expression in experimental autoimmune encephalomyelitis in C57BL/6 mice. J Neuropathol Exp Neurol. 2012;71(10):907–20.
Anderson JM, Hampton DW, Patani R, et al. Abnormally phosphorylated tau is associated with neuronal and axonal loss in experimental autoimmune encephalomyelitis and multiple sclerosis. Brain. 2008;131(Pt 7):1736–48.
Denic A, Johnson AJ, Bieber AJ, et al. The relevance of animal models in multiple sclerosis research. Pathophysiology. 2011;18(1):21–9.
Jaillard C, Harrison S, Stankoff B, et al. Edg8/S1P5: an oligodendroglial receptor with dual function on process retraction and cell survival. J Neurosci. 2005;25(6):1459–69.
Pernet V, Joly S, Christ F, et al. Nogo-A and myelin-associated glycoprotein differently regulate oligodendrocyte maturation and myelin formation. J Neurosci. 2008;28(29):7435–44.
Syed YA, Baer AS, Lubec G, et al. Inhibition of oligodendrocyte precursor cell differentiation by myelin-associated proteins. Neurosurg Focus. 2008;24(3–4):E5.
Mi S, Miller RH, Lee X, et al. LINGO-1 negatively regulates myelination by oligodendrocytes. Nat Neurosci. 2005;8(6):745–51.
Mi S, Hu B, Hahm K, et al. LINGO-1 antagonist promotes spinal cord remyelination and axonal integrity in MOG-induced experimental autoimmune encephalomyelitis. Nat Med. 2007;13(10):1228–33.
Mi S, Miller RH, Tang W, et al. Promotion of central nervous system remyelination by induced differentiation of oligodendrocyte precursor cells. Ann Neurol. 2009;65(3):304–15.
Lee X, Yang Z, Shao Z, et al. NGF regulates the expression of axonal LINGO-1 to inhibit oligodendrocyte differentiation and myelination. J Neurosci. 2007;27(1):220–5.
Wootla B, Watzlawik JO, Warrington AE, et al. Naturally occurring monoclonal antibodies and their therapeutic potential for neurologic diseases. JAMA Neurol. 2015;72(11):1346–53.
Satoh J, Onoue H, Arima K, Yamamura T. Nogo-A and nogo receptor expression in demyelinating lesions of multiple sclerosis. J Neuropathol Exp Neurol. 2005;64(2):129–38.
Reindl M, Khantane S, Ehling R, et al. Serum and cerebrospinal fluid antibodies to Nogo-A in patients with multiple sclerosis and acute neurological disorders. J Neuroimmunol. 2003;145(1–2):139–47.
Meininger V, Pradat PF, Corse A, et al. Safety, pharmacokinetic, and functional effects of the nogo-a monoclonal antibody in amyotrophic lateral sclerosis: a randomized, first-in-human clinical trial. PLoS One. 2014;9(5):e97803.
Tran JQ, Rana J, Barkhof F, et al. Randomized phase I trials of the safety/tolerability of anti-LINGO-1 monoclonal antibody BIIB033. Neurol Neuroimmunol Neuroinflamm. 2014;1(2):e18.
Cadavid D, Balcer L, Galetta S, et al. Evidence of remyelination with the anti-LINGO-1 monoclonal antibody BIIB033 after acute optic neuritis. Neurology. 2015; E46.
Noseworthy JH, Vandervoort MK, Wong CJ, Ebers GC. Interrater variability with the Expanded Disability Status Scale (EDSS) and Functional Systems (FS) in a multiple sclerosis clinical trial: the Canadian Cooperation MS Study Group. Neurology. 1990;40(6):971–5.
di Nuzzo L, Orlando R, Nasca C, Nicoletti F. Molecular pharmacodynamics of new oral drugs used in the treatment of multiple sclerosis. Drug Design Develop Ther. 2014;8:555–68.
Bonnan M, Ferrari S, Bertandeau E, et al. Intrathecal rituximab therapy in multiple sclerosis: review of evidence supporting the need for future trials. Curr Drug Targets. 2014;15(13):1205–14.
Bien-Ly N, Boswell CA, Jeet S, et al. Lack of widespread BBB disruption in Alzheimer’s disease models: focus on therapeutic antibodies. Neuron. 2015;88(2):289–97.
Pepinsky RB, Shao Z, Ji B, et al. Exposure levels of anti-LINGO-1 Li81 antibody in the central nervous system and dose-efficacy relationships in rat spinal cord remyelination models after systemic administration. J Pharmacol Exp Ther. 2011;339(2):519–29.
Petereit HF, Rubbert-Roth A. Rituximab levels in cerebrospinal fluid of patients with neurological autoimmune disorders. Mult Scler. 2009;15(2):189–92.
Tran J, Palaparthy R, Zhao J, et al. Safety, tolerability and pharmacokinetics of the anti-LINGO-1 monoclonal antibody BIIB033 in healthy volunteers and subjects with multiple sclerosis. Neurology. 2012;78((Meeting Abstracts 1)):P02.021.
Greenberg BM, Rodriguez M, Kantarci O, et al. Safety and tolerability of the remyelinating therapeutic antibody rHIgM22 in patients with stable multiple sclerosis. Neurology. 2015:E48–E49.
Willi R, Schwab ME. Nogo and Nogo receptor: relevance to schizophrenia? Neurobiol Dis. 2013;54:150–7.
Lewis CM, Levinson DF, Wise LH, et al. Genome scan meta-analysis of schizophrenia and bipolar disorder, part II: schizophrenia. Am J Hum Genet. 2003;73(1):34–48.
Willi R, Weinmann O, Winter C, et al. Constitutive genetic deletion of the growth regulator Nogo-A induces schizophrenia-related endophenotypes. J Neurosci. 2010;30(2):556–67.
Budel S, Padukkavidana T, Liu BP, et al. Genetic variants of Nogo-66 receptor with possible association to schizophrenia block myelin inhibition of axon growth. J Neurosci. 2008;28(49):13161–72.
Craveiro LM, Weinmann O, Roschitzki B, et al. Infusion of anti-Nogo-A antibodies in adult rats increases growth and synapse related proteins in the absence of behavioral alterations. Exp Neurol. 2013;250:52–68.
Oertle T, van der Haar ME, Bandtlow CE, et al. Nogo-A inhibits neurite outgrowth and cell spreading with three discrete regions. J Neurosci. 2003;23(13):5393–406.
Schnell L, Schwab ME. Axonal regeneration in the rat spinal cord produced by an antibody against myelin-associated neurite growth inhibitors. Nature. 1990;343(6255):269–72.
Acknowledgements
We thank Dr. Roman Willi and Miguel Maurer for input and discussion about Nogo-A antibody pharmacology. We are grateful for funding from the Swiss Multiple Sclerosis Society, the Hartmann-Müller Foundation, the Swiss National Science Foundation, the Christopher and Dana Reeve Foundation, and the Desirée-and-Niels-Yde Foundation.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This work was supported by grants of the Swiss National Science Foundation (Grant No. 31003A-149315-1 to MES), the Christopher and Dana Reeve Foundation (to MES), the Swiss Multiple Sclerosis Society, the Hartmann‐Müller Foundation, Zurich, the Desirée‐and‐Niels‐Yde Foundation (to BVI), and an MD‐PhD fellowship of the Swiss National Science Foundation (No. 323530_151488, to BVI). No funding was received specifically for the publication of this article.
Conflict of interest
MES is a founder and board member of the University of Zurich spin-off company NovaGo Therapeutics Inc., seeking to develop Nogo-A antibody-based therapeutics. Benjamin V. Ineichen, Patricia S. Plattner, Nicolas Good, Roland Martin, and Michael Linnebank declare no conflicts of interest.
Additional information
B. V. Ineichen and P. S. Plattner contributed equally and share the first authorship.
Rights and permissions
About this article
Cite this article
Ineichen, B.V., Plattner, P.S., Good, N. et al. Nogo-A Antibodies for Progressive Multiple Sclerosis. CNS Drugs 31, 187–198 (2017). https://doi.org/10.1007/s40263-017-0407-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-017-0407-2