Abstract
Monoclonal antibodies (mAbs) are increasingly used to treat rheumatoid arthritis (RA). At present, anti-tumor necrosis factor-α drugs (infliximab, adalimumab, certolizumab pegol, and golimumab), rituximab, and tocilizumab are approved for RA treatment. This review focuses on the pharmacokinetics and pharmacodynamics of mAbs approved in RA. Being large proteins, mAbs exhibit complex pharmacokinetic and pharmacodynamic properties. In particular, owing to the interactions of mAbs with their antigenic targets, the pharmacokinetics of mAbs depends on target turnover and exhibits non-specific (linear) and target-mediated (often nonlinear) clearances. Their volume of distribution is low (3–4 L) and their elimination half-life usually ranges from 2 to 3 weeks. The inter-individual pharmacokinetic variability of mAbs is usually large and is partly explained by differences in antigenic burden or by anti-drug antibodies, which accelerate mAb elimination. The inter-individual variability of clinical response is large and influenced by the pharmacokinetics. The analysis of mAbs concentration-effect relationship relies more and more often on pharmacokinetic-pharmacodynamic modeling; these models being suitable for dosing optimization. Even if adverse effects of mAbs used in RA are well known, the relationship between mAb concentration and adverse effects is poorly documented, especially for anti-tumor necrosis factor-α mAbs. Overall, RA patients treated with mAbs should benefit from individualized dosing strategies. Because of the complexity of their pharmacokinetics and mechanisms of action, the current dosing strategy of mAbs is not based on sound knowledge. New studies are needed to assess individual dosing regimen, adjusted notably to disease activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Current knowledge on the pharmacokinetic variability of monoclonal antibodies showed that increasing antigenic burden (and therefore disease activity) and the presence of anti-drug antibodies, are associated with decreasing in mAb exposure. |
Studies have identified serum mAb concentrations predictive to clinical efficacy, which are currently used in routine therapeutic drug monitoring, especially for anti-tumor necrosis factor-α biopharmaceuticals. |
Current therapeutic drug monitoring tools may be improved by taking into account disease activity using Bayesian and/or physiological PK-PD models and still need to be confirmed in prospective studies. |
1 Introduction
Rheumatoid arthritis (RA) is a chronic, systemic, and progressive inflammatory disease that affects synovial tissues of joints, often resulting in joint alteration and cartilage destruction. Studies on the pathogenesis of RA revealed a major role of both tumor necrosis factor-α (TNF-α) and interleukin-1 (IL-1) in inflammation and matrix destruction, with elevated TNF-α levels at inflammation sites being responsible for disease pathology. Antibodies that blocked TNF-α effectively in animal models were tested in patients with very positive results [1]. The treatment of RA was profoundly modified by anti-TNF-α drugs [2]. Infliximab, first approved for Crohn’s disease, is an anti-TNF-α chimeric monoclonal antibody (mAb). In the ATTRACT trial, infliximab was shown to improve disease activity significantly [3] and in 1999, it was the first anti-TNF-α mAb to be approved by the US Food and Drug Administration (FDA) for the treatment of RA (Table 1).
Later, a fusion protein, etanercept (Enbrel®, 1999), and a human anti-TNF-α mAb, adalimumab (Humira®, 2003), were approved for RA treatment. More recently, abatacept (Orencia®, 2007), golimumab (Simponi®, 2009), a human mAb, and certolizumab pegol (Cimzia®, 2009), a PEGylated Fab′ fragment, joined the anti-TNF-α family (Table 1). Since 2013, several biosimilars of infliximab (such as Inflectra® or Remsima®) have been approved. Even if all these five drugs target TNF-α, they are not equivalent in terms of pharmacodynamics, notably with differences in mAb-TNF complex formation and TNF-mediated signaling disruption [1, 4, 5]. These differences may explain why non-responders to a given anti-TNF-α biopharmaceutical may respond to another one. Because they have also different pharmacokinetics and routes of administration, characteristics that will be developed in this review, each of these TNF-α biopharmaceuticals is unique in terms of clinical efficacy and tolerance.
Since the 1990s, clinical scores were developed to quantify the influence of treatment on disease activity and to determine thresholds for clinical remission, response, or non-response [6]. These scores include ACR (American College of Rheumatology) [7] and DAS28 (Disease Activity Score in 28 joints) [8]. For instance, DAS28-based remission and low disease activity values (<2.6 and 3.2, respectively) allow the determination of lack of response (i.e., patients with no response achievement) or loss of response (i.e., patients with loss of response over time, referred to as secondary failures) [9].
Although mAbs target their antigen with high specificity, a large inter-individual variability in clinical response is observed. In RA, the ACR scale is a common clinical endpoint [10]. In the ATTRACT study, a 3 mg/kg dose of infliximab every 8 weeks led to a large variability in response in terms of ACR. In addition, large inter-individual variability in infliximab trough concentrations was observed, with the highest concentrations being 100-fold the lowest concentrations and the response rate increasing with infliximab concentrations. Therefore, the pharmacokinetic variability influences the variability of clinical response [11].
Beside anti-TNF-α agents, other mAbs are indicated for RA. Rituximab (MabThera®, Rituxan®) is a chimeric monoclonal antibody that targets CD20, a protein present at the surface of B lymphocytes. After being approved for the treatment of B-cell malignancies, i.e., non-Hodgkin lymphomas (1997) and chronic lymphocytic leukemia, rituximab was shown to be effective in RA patients who did not respond to prior disease-modifying anti-rheumatic drugs and methotrexate [12]. Rituximab was approved for RA treatment in combination with methotrexate in 2006 for patients who had not responded to treatment with at least one TNF-α biopharmaceutical. More recently, tocilizumab (Cimzia®, 2009), an anti-IL-6 receptor antibody, was approved in this indication. IL-6 is a cytokine that regulates the immune system, inflammation, and hematopoiesis. Increased levels of IL-6 were shown to be associated with inflammation and clinical outcomes in RA patients; the use of tocilizumab was shown to reduce RA disease activity (Table 1) [13, 14].
After a brief description of the structure of human immunoglobulins and mAbs, this review focuses on the pharmacokinetics and concentration-response relationships of mAbs that have been approved in the treatment of RA (Table 1).
2 Therapeutic Antibody Structures
The structure of therapeutic mAbs was extensively described elsewhere [15–17] and this section will present the main characteristics of human immunoglobulins of the G isotype (IgG). The IgGs are large molecular weight (150 kDa) hydrophilic proteins. They are made of two identical heavy chains and two identical light chains, each of them including constant and variable domains. Four IgG subclasses were described, numbered from 1 to 4. All mAbs of this review are, or derive from, IgG1 (Fig. 1). The IgG structure can be divided into two identical antigen-binding portions (Fab) and a crystallizable portion (Fc). The hypervariable region, a small region at the top of the variable domain, binds to the target antigen with high affinity and specificity. The Fc portion is involved in two important functions:
Structure of an IgG1 (left) and of a PEGylated Fab′ fragment (right). IgG1 are composed of two identical antigen-binding portions (Fab) and one crystallizable portion (Fc). These portions are composed of constant (C, in white), variable (V, in gray), and hypervariable (in black) domains. IgG1 are composed by both heavy (H) and light (L) chains. Certolizumab pegol is composed of one Fab′ portion and two PEG molecules. CH constant heavy, CL constant light, PEG polyethylene glycol, VH variable heavy, VL variable light
-
1.
it binds to effector systems, including the C1q subunit of complement and the effector cells via Fcγ receptors, e.g., FcγRIIIA, which is expressed at the surface of natural killer cells;
-
2.
it binds to the neonatal Fc receptor (FcRn), which is involved in IgG protection from intracellular catabolism and therefore in the clearance of natural IgGs and mAbs with a Fc portion. The structure and role of FcRn were reviewed elsewhere [18, 19].
The first mAbs developed were murine, e.g., muromonab, an anti-CD3 mAb. These mAbs had low affinity for human FcγR and FcRn, leading to poor recruitment of effector functions and poor FcRn-mediated protection, with a short elimination half-life (t½), between 1 and 2 days [16, 19]. They were also highly immunogenic. However, all other mAbs developed for immuno-inflammatory diseases have human constant domains, and therefore have pharmacokinetic and immunological properties comparable to natural IgGs. These mAbs are either chimeric (i.e., with exogenic variable domains), humanized (i.e., with exogenic hypervariable regions), or human (i.e., with no exogenic domain). Progressive humanization of mAbs has only partly solved the problem of their immunogenicity.
Certolizumab is a Fab′ fragment derived from an anti-TNF-α humanized monoclonal antibody (Fig. 1). Because it has no Fc portion, it cannot bind to FcRn and be protected from intracellular catabolism. In addition, because of their small size (around 50 kDa), Fab′ fragments can be eliminated by renal excretion. However, certolizumab is conjugated to a couple of hydrophylic polyethylene glycol (PEG) chains. Compared with the Fab′ alone, certolizumab pegol has improved pharmacological properties, including increased solubility and bioavailability, and reduced immunogenicity and toxicity [20]. The enhanced molecular size (around 90 kDa) may explain the reduction in renal excretion. The pegylation of Fab and Fab′ fragments increases their t½ from around less than one day to several days [21].
3 Pharmacokinetics of mAbs Used in RA
The pharmacokinetics of mAbs was comprehensively reviewed elsewhere [16, 19, 22–25]. The present review summarizes pharmacokinetic features of mAbs, focusing on mAbs used in RA. The largest part of our information was obtained from the scientific literature, but it was completed using FDA pharmacokinetic reports available online when necessary.
Since the 2000s, population pharmacokinetic analysis is increasingly used, notably for mAbs [16, 25]. Briefly, a population approach allows the description of the inter-individual distribution of parameters of interest by computing simultaneously data from all individuals in a given population. This inter-individual distribution allows the quantification of (i) the “mean” (referred to as “typical”) value of each parameter, (ii) the inter-individual variability (referred to as “inter-individual variance”), and (iii) the influence of individual factors on the inter-individual distribution (referred to as “covariates”) [26, 27]. A large part of this review was given to results obtained using population pharmacokinetic modeling, mainly because this approach integrates the description of all pharmacokinetic phases (absorption, distribution, and elimination) and is based on strict quality standards, and therefore provides sufficiently homogenous results, allowing consistent “between-mAbs” and “between-studies” comparisons.
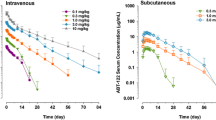
The pharmacokinetics of mAbs administered by the intravenous (IV) route is usually described using two-compartment models in RA patients [16, 19, 22, 23]. Indeed, two compartments were shown to be sufficient to describe mAb pharmacokinetics if the influence of their target antigen is not taken into account. The influence of target antigenic mass is described in Sect. 3.2.2 [28]. More specifically, two-compartment models were used to describe the pharmacokinetics of infliximab [29], rituximab [30], adalimumab [31, 32], golimumab [33], and tocilizumab in RA [34, 35]. The pharmacokinetics of most mAbs administered by the subcutaneous (SC) route was described using one-compartment models [16], as done for adalimumab in RA [36]. Nevertheless, some studies used two-compartment models to describe the pharmacokinetics of mAbs administered by the SC route, as golimumab [37], tocilizumab [38], and certolizumab pegol [39], but these studies benefited from combined IV and SC data. The lack of identification of peripheral compartment parameters may be the result of the rapid distribution phase compared with the absorption phase. For instance, golimumab distribution and absorption half-lives were 2.3 days and 5.3 days, respectively (Table 2).
3.1 Absorption, Distribution, Metabolism, and Excretion of mAbs
3.1.1 Absorption
Initially, mAbs were developed to be administered by the IV route, but more and more of them are being developed to be administered by the SC route. The mechanism of absorption following SC administration is not yet fully understood, but it was suggested that systemic absorption of mAbs occurred by diffusion of IgG across blood vessels and convection through lymphatic vessels [16, 23, 40]. Because the flow through lymphatic vessels is slow, the absorption usually lasts several days, with a large inter-individual variability.
The absorption kinetics of mAbs administered subcutaneously is usually described using a first-order rate constant (k a). In RA patients, k a was estimated between 0.15 and 0.30 day−1, a value similar to values reported for mAbs given in other indications [16]. For certolizumab pegol, the absorption kinetics (k a = 0.26 day−1 [39]) was similar to that of full IgG mAbs. Absolute bioavailability (F) of mAbs is between 50 and 75 %, and around 80 % for certolizumab pegol [41].
3.1.2 Distribution
Central volumes of distribution were similar for all mAbs, including certolizumab pegol, were low, ranging between 3 and 4 L (Table 2). Being large molecular weight (150 kDa) hydrophilic molecules, mAbs should exhibit low tissue penetration and be confined to lymphatic and blood vessels [40]. However, they penetrate into cells via fluid phase endocytosis, notably in endothelial cells, or via receptor-mediated endocytosis via FcγR expressed on the membrane of immunological cells [16, 23, 40]. In addition, FcRn is responsible for the transcytosis of mAbs and may therefore explain their penetration into certain tissues. Therefore, the common interpretation for IgG low volumes of distribution being essentially confined inside blood and interstitial tissues may be abusive. Indeed, a recent study used physiologically based pharmacokinetics and suggested that, central and peripheral compartments of two-compartment models may not be considered as blood and interstitial spaces, respectively, but rather as two distinct groups of tissues, some being kinetically similar to plasma and others not [28]. In addition, non-specific elimination may concern not only unbound antibodies, but also antibody-target complexes. For instance, omalizumab targets circulating IgEs. An increase in total IgE serum levels was shown in patients treated with omalizumab, despite a decrease in unbound IgE serum levels [42]. It may be due to the recycling of omalizumab-IgE complexes via FcRn.
3.1.3 Elimination
Small molecule drugs are eliminated by renal or biliary excretion and/or by metabolism, which mainly occurs in the liver. However, immunoglobulins and most proteins do not follow these elimination pathways. Indeed, the sizes of full IgGs, as well as of PEGylated certolizumab, prevent them for glomerular filtration. The elimination of IgG involves two different pathways, (i) non-specific intracellular elimination and (ii) specific target-mediated elimination. The total clearance of a given mAb is therefore the sum of non-specific (linear) and target-mediated (nonlinear) clearances.
3.1.3.1 Non-Specific Elimination
The mechanisms by which antibodies are cleared from the circulation are not fully understood but it is known that IgG are mainly cleared by intracellular catabolism after cellular uptake. The mechanisms of this uptake include endocytosis and internalization following Fab binding to the antigen at the surface of the target cell or Fc binding to FcγR expressed on immunological cells [16, 23, 43, 44]. If FcRn is present in the cell, cellular uptake is followed by the binding of the Fc portion of the mAb to FcRn at acidic pH (<6.5). Then, the mAb is protected from lysosomal degradation and addressed to the apical or the basolateral membrane. The mAb is released when endosomal pH returns to neutral (7.4), into the circulation for the apical membrane or into the extracellular fluid for the basolateral membrane. The recycling of IgGs by FcRn explains their long t½ (around 21 days) compared with other proteins. FcRn may be saturated when concentrations of IgGs are high, as during polyclonal immunoglobulin therapy [45], but it is not saturated by usual mAbs doses. This allows non-specific elimination to be a linear phenomenon.
3.1.3.2 Specific Elimination
The binding of a given mAb to its target antigen leads to the formation of a mAb-target complex that is eliminated by the immune system by mechanisms that are not fully elucidated. The elimination rate of this complex, which corresponds to target-mediated clearance of mAbs, is different from those of free mAb and target antigen. The joint kinetics of mAbs and their targets is described using target-mediated drug disposition (TMDD) models, which take into account the nonlinear nature of a given drug clearance, when this clearance is dependent on the turnover of its target [46, 47]. TMDD models were shown to be suitable to account for the nonlinear nature of target-mediated mAb clearance [47, 48]. The target-mediated elimination of mAbs depends on several parameters, including target turnover, the saturable and reversible binding of mAbs to their targets, and the elimination rate of the complexes. Target-mediated clearance increases with the target amount. These models, which were initially used to describe antibodies targeting proteins expressed at the cell surface [49], were extended to mAbs targeting circulating molecules such as omalizumab [42]. However, the turnover of the target is often unknown. In this case, TMDD models may be approximated by pharmacokinetic models that include linear and nonlinear (Michaelis–Menten [50]) clearance terms.
In RA patients, clearances of mAbs varied from 0.22 to 0.72 L/day. Elimination half-lives are close to 3 weeks, except for certolizumab pegol and infliximab, which have t½ of 12 and 9 days, respectively (Table 2). Of note, infliximab t½ is around 14–16 days in ankylosing spondylitis [51, 52] and inflammatory bowel disease [53] patients. This inter-disease variability was not explained up to date, but might be due to the turnover of antigenic burden (Sect. 3.2.2.). If the difference between certolizumab pegol t½ and that of other mAbs may be explained by their different structures, the differences in t½ of infliximab between indications is not explained yet. The only mAb used in RA showing a non-linear elimination is tocilizumab. Frey et al. described tocilizumab elimination using linear and Michaelis–Menten terms. [34] The 8-mg/kg dose was associated with a lower total clearance, because of a longer saturation of target-mediated clearance, compared with the 4-mg/kg dose.
3.2 Pharmacokinetic Variability of mAbs
The pharmacokinetics of mAbs is highly variable between patients. [16, 19] In mAbs approved for RA treatment, the inter-individual standard deviation ranged from 12 to 97 % for central volume of distribution and from 17 to 44 % for clearance. Several covariates were found to be associated with the variability of these pharmacokinetic parameters.
3.2.1 Influence of Demographic Factors
Demographic factors, such as body size or sex, are often found to influence the pharmacokinetics of mAbs, body size being often assessed as body weight (BW), and sometimes as body surface area (BSA) (Fig. 2). Generally, volume of distribution and/or clearance of mAbs increase with body size and are higher in men than in women. When BW increases from 50 to 90 kg, the central volume of distribution is doubled for infliximab [29] and golimumab [33]. When BSA increases from 1.4 to 1.9 m2, rituximab central volume of distribution and clearance are increased by 25 and 35 %, respectively [30]. The clearance of adalimumab [36] and rituximab [30] is around 40 % higher in men than in women. The influence of BW or BSA justifies the adjustment of mAb doses to body size. However, no adaptation of dose on sex is recommended.
Dose-concentration-response relationship for anti-tumor necrosis factor-α (TNF-α) monoclonal antibodies (mAbs). Arrows and truncated lines represent stimulation and inhibition relationships respectively between boxes. Increased mAb concentrations decrease TNF-α concentrations. Increased TNF-α concentrations increase disease activity. Because TNF-α burden accelerates mAb elimination, high TNF-α concentrations lead to low mAb concentrations. High mAb concentrations decrease the risk of developing anti-drug antibodies (ADA), which, when they are present, accelerate mAb elimination [67, 72]. Methotrexate inhibits ADA development, probably both by direct immunosuppressive effect and by decreasing TNF-α production and therefore increasing mAb concentrations
3.2.2 Influence of Antigenic Burden
Except for tocilizumab, no nonlinear decay was described for monoclonal antibodies approved in RA. Because the target-mediated clearance is expected to increase with the target amount, the lack of nonlinear elimination may be explained by a continuous saturation of target antigens. For instance, in RA, TNF-α serum levels are around 0.0012 mg/L (70 pmol/L) [54], a value that is 50- to 700-fold lower than residual concentrations of infliximab (around 1.5 mg/L (10 nmol/L) [29]), adalimumab (4.0–8.0 mg/L [27–53 nmol/L] [55]), golimumab (around 0.5 mg/L [3.3 nmol/L] [56]), and certolizumab pegol (around 1.0 mg/L [11 nmol/L] [39]). Although TNF-α serum levels are only part of total TNF-α burden, nonlinear elimination may occur at very low levels of anti-TNF-α mAb and may not be observed with usual therapeutic concentrations. Because the circulating TNF-α level is increased in RA patients compared with healthy subjects, total clearance of anti-TNF-α biopharmaceuticals is higher in RA patients (Fig. 2). This is notably the case for certolizumab pegol, for which apparent clearance is higher in RA patients than in healthy subjects (21 vs. 12 mL/h [41]).
Regarding rituximab, the fact that it induces a rapid and deep B-cell depletion, with a recovery occurring several months after the infusions, does not allow the observation of a potential nonlinear decay [57]. Therefore, as for anti-TNF-α mAbs, nonlinear elimination may not be observed at measurable rituximab concentrations.
Dose-ranging studies of anti-TNF-α mAbs showed an increase in t½ and a decrease in clearance for increasing doses, which was more pronounced in RA patients than in healthy subjects. Golimumab t½ increases slightly with dose in healthy subjects (10.8 days for 50 mg vs. 11.9 days for 100 mg) [58], whereas it increases markedly in RA patients (8 days for 0.1 mg/kg vs 20 days for 10 mg/kg) [33].
The value of mAb t½ reaches a maximum at high mAb doses, probably because of the saturation of target-mediated clearance. Indeed, in RA patients, infliximab t½ seems to reach a stable value for IV doses between 1 and 5 mg/kg [59], whereas adalimumab t½ is stable (with a value of around 18 days) for single IV doses ranging from 0.25 to 5 mg/kg [31].
In RA patients, inflammation was shown to influence infliximab pharmacokinetics: indeed, two studies showed that C-reactive protein (CRP) levels at baseline were inversely correlated with residual infliximab concentrations at steady state [60, 61] and directly correlated with infliximab clearance (Table 2): an increase in CRP levels from 0.1 to 14 mg/L was associated with a shortening of infliximab elimination t½ from 14 to 8 days [29]. Because TNF-α production should precede CRP production [2, 62], serum CRP levels may be considered as a surrogate marker of TNF-α levels in the body. In patients with substantial inflammation, infliximab clearance may be high because of its capture by TNF-α. The fact that systemic inflammation is higher in RA than in ankylosing spondylitis [63] may explain why CRP was not found to influence infliximab clearance in ankylosing spondylitis patients [51]. This influence, expected for other anti-TNF-α biopharmaceuticals, was not reported yet.
For tocilizumab, a dose-ranging study in healthy subjects showed a total clearance decreasing from 1.4 to 0.5 L/day for SC doses increasing from 162 to 648 mg [64]. This marked dose dependence of tocilizumab clearance, which reflects its nonlinear mechanisms of elimination suggests that target-mediated clearance of this mAb is much higher than that of anti-TNF-α biopharmaceuticals.
3.2.3 Influence of Co-Medications
Because mAbs are not eliminated by renal or biliary excretion and/or by metabolism, it may be thought that mAbs pharmacokinetics is not modified by concomitant drugs. However, the pharmacokinetics of infliximab and adalimumab were found to be influenced by methotrexate co-medication, trough concentrations of both infliximab [65] and adalimumab [55] being higher in the presence of methotrexate. Methotrexate was associated with a 30 % decrease in infliximab clearance and an increase in t½ from 9.3 to 13.3 days [29]. Median adalimumab trough concentrations were 4.1 and 7.4 mg/L without and with methotrexate, respectively [55]. Methotrexate, acting as an anti-inflammatory drug, should lead to a significant decrease in TNF-α levels and therefore to a decrease in infliximab target-mediated clearance (Fig. 2). Of note, methotrexate co-treatment did not influence infliximab pharmacokinetics in ankylosing spondylitis patients, probably because antigen burden is lower in this disease than in RA [55]. No sound data reported an influence of other disease-modifying anti-rheumatic drugs (such as azathioprine or prednisolone) on mAbs pharmacokinetics [66].
3.2.4 Influence of Anti-Drug Antibodies
Being exogenous proteins, mAbs can induce an immune response leading to the production of antibodies directed against the biopharmaceutical, often called anti-drug antibodies (ADA). This risk, very high for murine mAbs, is not absent for human antibodies (e.g., adalimumab). The presence of ADA is associated with decreased infliximab [67, 68], adalimumab [69], golimumab [58], and certolizumab pegol [39] concentrations. Being responsible for an underexposure to mAbs [70], the development of ADA is one of the main cause of loss of response to infliximab [71–73] and adalimumab treatment [69, 74]. In approximately 30 % of patients, ADA are only transient, i.e., ADA that can occur at any time during mAb treatment, disappear spontaneously, and are generally of low clinical significance [75, 76]. For rituximab, no immunization was described in patients with B-cell malignancies treated with rituximab, but a few RA patients developed ADA. These ADA were associated with decreased rituximab concentrations, but not with treatment failure [77]. The proportion of patients developing ADA is estimated to range from 8 to 75 % [74], depending on:
-
1.
mAb. Infliximab being notably more immunogenic than adalimumab and rituximab;
-
2.
techniques of ADA detection. Early ADA tests showed interferences with mAbs present in the sample, leading to false-negative results if the mAb concentration was too high (1 or 2 mg/L). New tests detecting ADA to infliximab [78] and adalimumab [79], which are based on acid dissociation of mAbs-ADA complexes and prevention of their reformation, show less interferences. In RA patients, the risk of immunization against adalimumab was initially estimated at 17 % [72] but it is at more than 50 % using these new tests [74].
-
3.
exposure to the mAb. Low trough infliximab concentrations being associated with an increased risk to develop ADA [65, 67]. In addition, infliximab trough concentrations measured 1.5 months after the beginning of the treatment were inversely correlated to ADA titers measured at 6 months [60].
-
4.
co-medication. RA patients treated with infliximab having a lower risk of developing ADA when co-treated with methotrexate [65, 80]. This decreased risk may be explained by both the immunosuppressive activity of methotrexate and the higher infliximab concentrations in co-treated patients.
Even if exposure to mAbs and co-medication were suggested to influence the risk of developing ADA, this influence has not been clearly quantified up to date. In addition, because methotrexate co-treatment influences both anti-TNF-α drug concentrations and ADA development, methotrexate co-treatment may be a confounding factor of influence of ADA on mAb clearance, even if population modeling accounts, even partly, for this confusion. Finally, early ADA tests showed interferences with mAbs present in the sample, leading to false-negative results if the mAb concentration was too high. Indeed, this may lead to biased interpretations of the relationship between mAb exposure and the presence of ADA.
The decrease of mAb concentrations in the presence of ADA can be explained by an increase in mAb clearance (Fig. 2). Indeed, several pharmacokinetic studies showed that infliximab [29, 51–53, 81], golimumab [82], and certolizumab pegol [39] clearances were increased 3- to 4-fold in the presence of ADA. In addition, ADA-mediated clearance is nonlinear: adalimumab pharmacokinetics in the presence of ADA was reported to be similar to TMDD kinetics [83, 84]. The impact of ADA was not assessed for tocilizumab [85] and rituximab [77], although they were detected in these studies.
3.2.5 Influence of Serum Albumin
In chronic bowel disease patients, an inverse relationship was observed between serum albumin levels and infliximab clearance [53] (Fig. 2). Albumin and IgG are both protected from catabolism by FcRn, although they do not compete with each other. Therefore, low albumin levels could reflect a decrease in FcRn activity and therefore a decrease in infliximab recycling [86]. However, the interpretation of albumin as an indicator of FcRn expression is limited by the pathological variations of albumin production.
3.2.6 Influence of Special Patient Populations
3.2.6.1 Age, Renal Failure and Hepatic Failure
Age was rarely associated with alterations of mAbs pharmacokinetics [16], and never for mAbs administered in RA. In addition, because mAbs are not eliminated by renal excretion or by metabolism, the pharmacokinetics of mAbs is not likely to be modified in patients with renal or hepatic impairment, even if an increase in mAbs clearance due to IgG leakage in severe renal impairment cannot be excluded. The elimination of certolizumab pegol depends on the dissociation of the Fab′ portion from PEG molecules, the Fab′ being eliminated in urine [20]. A decrease in elimination of certolizumab pegol in patients with renal failure may therefore be anticipated but this has not been reported yet.
3.2.6.2 Pregnancy
Because FcRn is involved in IgG transplacental transfer, the fetus is exposed to mAbs administered during pregnancy and breast feeding. Indeed, in women treated with infliximab and adalimumab during pregnancy, the cord-to-maternal and fetus-to-maternal mAb concentration ratios were above 100 % for infliximab and adalimumab. These mAbs were detected 6 months after birth in infants’ blood. The exposure-toxicity relationship was not assessed because no serious complication was reported. In addition, the transplacental transfer might decrease maternal mAb exposure, even if this was not reported yet. Low concentrations of infliximab and adalimumab were found in breast milk [87]. Regarding certolizumab pegol, the cord-to-maternal and fetus-to-maternal ratios were below 5 %. The low placental transfer of certolizumab pegol may be owing to the absence of Fc portion and therefore of FcRn binding [87, 88]. The long-term effects of mAbs in infants that were exposed in utero still need to be investigated [89].
4 Concentration-Response Relationships
4.1 Infliximab and Adalimumab: from Dose-response Relationship to Pharmacokinetic-pharmacodynamic Models
In the ATTRACT study, the therapeutic response (ACR) increased with infliximab doses and with infliximab trough concentrations [11]. This result was confirmed by a meta-analysis that showed that a high dose (10 mg/kg) of infliximab was more effective than the standard 3-mg/kg dose, especially in patients with severe disease activity. Indeed, 30–50 % of RA patients needed an increase in infliximab dose because of insufficient response [90, 91]. Even if the presence of ADA was a good predictor of loss of response, half of the non-responder patients had no detectable ADA. Overall, the authors suggested that the dosing regimen should be intensified in patients with high disease activity.
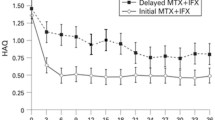
Early studies searched for a relationship between mAbs serum levels and clinical response. In the ATTRACT study, the proportion of patients with ACR50 % and ACR70 % were found to be increased with increasing infliximab trough concentrations [11]; for adalimumab, European League Against Rheumatism (EULAR) response was found to increase with increasing mAb concentrations [69]. This concentration-response relationship for infliximab and adalimumab therefore motivated the analysis of trough concentrations as predictors of clinical response: using receiver operating characteristic analysis, infliximab and adalimumab trough concentrations above 2.5 mg/L [92] and 5 mg/L [55] were shown to be predictive of good clinical response, respectively. Nevertheless, trough mAb concentrations alone cannot predict clinical response but should be interpreted together with disease activity [92], both pieces of information being necessary for the decision to modify the dosing regimen [93]. To quantify the importance of the relationship between mAb concentration and disease activity, a few attempts were made to describe this relationship using pharmacokinetic-pharmacodynamic modeling.
4.2 Pharmacokinetic-Pharmacodynamic Modeling
Pharmacokinetic-pharmacodynamic modeling is increasingly used to design the best dosing regimen during drug development as well as in routine individual dose adjustment. For mAbs used in RA, the first pharmacokinetic-pharmacodynamic models described the relationships between infliximab concentrations and CRP levels on the one hand, and disease activity score in 28 joints (DAS28, a disease activity score for RA) on the other hand, by direct E max models [94]. These models suggested that infliximab concentrations above 5 mg/L led to good biological (CRP) and clinical (DAS28) responses.
The adalimumab concentration-effect relationship was described using a population approach and indirect models for CRP [94, 95] or direct E max models for DAS28 [36]. In the latter study, a large inter-individual variability in patient sensitivity to adalimumab was observed: concentrations leading to 50 % decrease in CRP “input” (C50) and in DAS28 (IC50) were 3.6 and 11.0 mg/L, respectively, with inter-individual standard deviations of 88 and 71 %, respectively. This work suggested that the steady-state adalimumab concentration that should be targeted increases with disease activity. However, because of the long t½ of adalimumab, this target concentration is reached a long time (15–20 weeks) after treatment initiation. Simulations based on the pharmacokinetic-pharmacodynamic model showed that a 160-mg loading dose would allow steady-state concentrations and an optimal efficacy between the first and the second injections [36, 96]. An indirect model was used to describe the relationship between tocilizumab concentrations and DAS28. The concentration leading to a 50 % decrease in DAS28 (EC50) “input” was 3.7 mg/L and varied markedly between patients (inter-individual variability of 170 %). Estimated EC50 for tocilizumab was lower than the estimated IC50 for adalimumab (11.0 mg/L), suggesting that a given effect on DAS28 is obtained with lower concentrations of tocilizumab than of adalimumab. This difference might be explained by differences in antigenic targets, and in mechanisms of action.
Other pharmacokinetic-pharmacodynamic studies attempted to describe ACR in RA patients treated with mAbs. The dichotomous variable ACRn is defined by a decrease of at least n% in the number of tender and swollen joint, plus similar improvement in at least three or five measures specified by the ACR [10]. Using concentration and ACR data from the GO-FORWARD phase III trial [97], two studies described the concentration-ACRn relationship, one of which used ACRn transformed in a continuous nonnegative variable, allowing the use of an indirect response model with inhibition of ACRn “input” [37]. However, this approach was limited by the inability to identify EC50. Because ACRn is dichotomous, it may be more relevant to model the probability to achieve ACRn, an approach that was used to reanalyze the GO-FORWARD trial [37]. The probability of achieving ACRn was therefore described using logistic mixed-effects models with a latent variable accounting for the anti-TNF-α of golimumab [37]. For certolizumab pegol, a Markov mixed-effect model was used to describe the probability of achieving ACR20 [98]. These models appear to be suitable to predict the benefit of dosing regimen modifications: notably, the use of three 400-mg loading doses of certolizumab pegol, allowing a faster response and decreasing the risk of dropouts. However, both logistic and Markov approaches present drawbacks: the logistic approach rests on the assumption that all observations, notably within-patient, are independent, and Markov models may bring difficulties to interpret the model terms.
These pharmacokinetic-pharmacodynamic approaches, if they are useful for predictions of therapeutic response, do not allow the exploration of their mechanisms of action and notably mAb tissue distribution, interactions with their target antigen, and secondary pharmacological pathways. The complexity of subsequent mechanisms may explain the large inter-individual variability in pharmacodynamic parameters. A few studies developed physiologically based pharmacokinetic-pharmacodynamic models for mAbs in RA. A model accounting for infliximab pharmacokinetics, and the turnover of TNF-α, and their interaction inhibiting inflammation, was developed [99] and applied to RA [100]. More recently, a model accounting for the tissue distribution and the interaction of adalimumab and TNF-α into the bloodstream and into joints was developed [101]. However, this model dealt with inflammation as a general variable and did not include a mechanistic description of RA. Up to now, no mechanistic description of the mAb mechanism of action specifically in RA was developed.
5 Concentration-Toxicity Relationships
5.1 Most Common Adverse Effects
The most common adverse effects associated with anti-TNFα mAbs, rituximab, or tocilizumab in humans are infections (viral, bacterial, or fungal) and immunological reactions (infusion-related reactions, injection-site reactions, and hypersensitivity reactions) [41, 56, 102–105]. Serious adverse effects, less frequent but potentially life threatening, including tuberculosis reactivation, opportunistic infections, hepatitis B reactivation, lymphomas and other malignancies, and progressive multifocal leukoencephalopathy, were included in FDA boxed warnings with strict recommendations for monitoring. Other serious adverse effects even less frequent were reported: demyelinating disorders, hepatotoxicity, hematological reactions, heart failure, and other cardiovascular events.
5.2 Dose-Adverse-Effect Relationships
Because clinical trials evaluated different drug dose regimens, a relationship between drug dose and common serious adverse effects was searched in meta-analyses of clinical trials (Table 3). Early evidence of a dose-adverse effect relationship of infliximab and adalimumab in RA was reported in a systematic review and meta-analysis of all randomized placebo-controlled clinical trials [106]. The risk of malignancies was significantly increased in anti-TNF-treated patients and was significantly higher in high-dose infliximab or adalimumab compared with the low dose, with an odds ratio (OR, 95 % confidence interval) of 3.4 (1.4–8.2) [106]. Similarly, the risk of serious infections was significantly increased in anti-TNF-treated patients, and there was a non-significant trend towards an increased risk for high-dose infliximab or adalimumab compared with the low dose, with OR = 1.4 (1.0–2.0) [106]. More recent meta-analyses of clinical trials found no increased overall risk of malignancies with anti-TNF mAbs [107, 108] but confirmed the increased risk of serious infections [108]. A non-significant relationship between dose and serious infection was apparent for golimumab [109], rituximab [110, 111], and tocilizumab [112], but not for certolizumab pegol [113]. A marginally significant lower risk of infusion reactions within 24 h of the first infusion was described for low-dose compared with high-dose rituximab in RA [112]. When considered together, recent evidence does not support dose-dependent malignancies or serious infections with anti-TNF mAbs [108].
5.3 Concentration-Adverse Effect Relationships
In RA patients, the relationship was observed between tocilizumab concentrations and neutrophil and platelet suppression [35]. Indeed, the IL-6 pathway is involved in T-cell activation and stimulation of hematopoiesis: the blockade of IL-6 receptor triggers not only a reduction in systemic inflammation, but also mechanism-related adverse effects, including a decrease in neutrophil and platelet counts. A mechanistic model, which included TMDD and lifespan models [114], showed that the decrease in neutrophil and platelet counts were concentration dependent and was reversible when tocilizumab was withdrawn [35]. To date, no concentration-adverse effect relationship was reported for anti-TNF-α biopharmaceuticals.
6 Discussion
In RA, part of the variability of response to mAbs treatment is due to pharmacokinetic variability, TNF-α inhibition increasing with exposure. The pharmacokinetic variability is explained by several factors, including body size, antigenic burden, and the presence of ADA (Fig. 2). Because of target-mediated elimination, an increased amount of TNF-α leads to increased target-mediated clearance and therefore lower concentrations of the anti-TNF-α mAbs. As a consequence, patients with high disease activity present a lower exposure to anti-TNF-α mAbs. Therefore, RA patients would need higher mAb doses according to disease activity [96], with an increase in doses as soon as underexposure is evidenced [67]. More pharmacokinetic-pharmacodynamic studies are needed to propose rational dosing strategies for anti-TNF-α drugs.
The dosing adjustment of anti-TNF-α mAbs to body size and disease activity is possible for anti-TNF-α administered intravenously, but not for SC forms (e.g., adalimumab, golimumab, and soon tocilizumab), which are mostly developed with a fixed dosing regimen (e.g., adalimumab 40-mg prefilled syringes). Even if the SC route is more convenient for patients and healthcare structures, it may not be adapted to patients with extreme body sizes or inflammation activity, and even more so because absorption adds a source of pharmacokinetic variability.
The development of ADA was largely described for mAbs in RA, especially infliximab and adalimumab. Notably, the risk of developing ADA is lower when immunosuppressive agents are involved and when there is no underexposure to anti-TNF-α. However, there is currently no method to predict the individual risk of immunization before the beginning of treatment. Being able to predict this risk is one of today’s big challenges.
Similarly to most mAbs, adalimumab t½ is around 3 weeks. Because no loading dose is recommended in RA patients, the time to reach steady-state concentrations and maximum effect is delayed (by 15–20 weeks). Therefore, RA patients should benefit from a 160-mg loading dose, as in Crohn’s disease patients, in whom the use of loading doses was shown to increase treatment efficacy and decrease the risk of developing ADA [115, 116]. Of note, omalizumab is to date the only mAb for which SC doses are adjusted to both body size (weight) and antigenic burden (pretreatment serum IgE levels).
The individual adjustment of dose should be particularly useful for mAbs displaying nonlinear elimination: a theoretical work suggested that clinical efficacy of anti-TNF-α and anti-IL-6R is strongly linked to the target occupancy rate [117]. Indeed, the occurrence of a nonlinear elimination for a certain range of mAb concentrations may be interpreted by the fact that targets are no longer saturated, the consequence being an acceleration of mAb elimination. However, an analysis of the non-linearity observed in tocilizumab pharmacokinetic studies showed that antigenic targets are not saturated for some patients treated with the approved dose [34, 35].
To date, several studies showed a potential benefit for therapeutic drug monitoring (TDM) of anti-TNF-α biopharmaceuticals. Notably, trough concentrations above 2.5 mg/L [92] and 5 mg/L [55] were shown to be predictive of good clinical response for infliximab and adalimumab, respectively. The general idea would be to find the optimal scheme for each patient. This optimal scheme, frequently searched empirically, could be calculated using pharmacokinetic modeling and data from the literature, for infliximab [29] as well as for adalimumab [31, 32, 36], taking into account individual factors of pharmacokinetic variability. In addition, using these studies, Bayesian pharmacokinetic models may be developed to estimate individual pharmacokinetic parameters using only a few concentration values [118]. Bayesian models for TDM have been developed for immunosuppressant [119, 120], anticancer [121], and antimicrobial [122, 123] drugs. However, the benefit of anti-TNF-α biopharmaceutical TDM has not been fully established yet. To show this benefit, prospective and randomized studies are needed.
The benefit of dosing adjustment can be assessed by simulations. However, published pharmacokinetic-pharmacodynamic models do not include a sound description of the pathophysiological mechanisms of RA. This may explain the large variability of concentration-effect relationships to erroneous extrapolations. Multi-scale system models, which were previously developed in oncology, may be used to build models including signaling pathways (e.g., the MAPK [124], NF-κB [125], and IL-6 pathways [126]), the expression of genes of interest [127], the regulation of the immune system [126], inflammation [128], and clinical consequences. Multi-scale system biology modeling may allow the connecting of these phenomena and help to (i) optimize the dosing strategy of marketed mAbs, (ii) test and optimize diverse associations of biopharmaceuticals, e.g., adalimumab and tocilizumab, (iii) find new targets of clinical interest, and (iv) find new biomarkers of response to treatment.
Data of dose-dependent adverse effects are still controversial and no definite conclusion can be drawn yet [129]. Overall, toxicological studies in animal models were not able to predict adverse effects observed in humans, notably the risk of malignancy, serious infections, and immunization. Because mAbs are developed against human targets, animal models are insufficient to correctly assess safety [130]. Therefore, adverse effects in humans can only be studied in clinical trials, first before marketing authorization, then in post-marketing trials, registries, or pharmacoepidemiological studies. Notably, studies assessing the relationships between concentration and severe infection and concentration and malignancy are needed. Some results may be obtained rapidly, using cohorts of patients followed in routine, for which mAb concentrations are measured. These studies will be helpful to determine upper limits of mAb concentrations and therefore provide therapeutic ranges that should be targeted using TDM procedures.
7 Conclusion
Several therapeutic strategies based on biopharmaceuticals are available for the treatment of RA. Although the mechanisms of action of mAbs in RA and their use are continuously improving, new studies are needed to develop a rational design of dosing regimens in patients.
References
Tracey D, Klareskog L, Sasso EH, Salfeld JG, Tak PP. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol Ther. 2008;117:244–79.
Elliott MJ, Maini RN. Anti-cytokine therapy in rheumatoid arthritis. Baillieres Clin Rheumatol. 1995;9:633–52.
Maini R, St Clair EW, Breedveld F, Furst D, Kalden J, Weisman M, et al. Infliximab (chimeric anti-tumour necrosis factor alpha monoclonal antibody) versus placebo in rheumatoid arthritis patients receiving concomitant methotrexate: a randomised phase III trial. ATTRACT Study Group. Lancet. 1999;354:1932–9.
Licastro F, Chiappelli M, Ianni M, Porcellini E. Tumor necrosis factor-alpha antagonists: differential clinical effects by different biotechnological molecules. Int J Immunopathol Pharmacol. 2009;22:567–72.
Taylor PC. Pharmacology of TNF blockade in rheumatoid arthritis and other chronic inflammatory diseases. Curr Opin Pharmacol. 2010;10:308–15.
Felson DT, Smolen JS, Wells G, Zhang B, van Tuyl LHD, Funovits J, et al. American College of Rheumatology/European League Against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Arthritis Rheum. 2011;63:573–86.
Anderson J, Caplan L, Yazdany J, Robbins ML, Neogi T, Michaud K, et al. Rheumatoid arthritis disease activity measures: American College of Rheumatology recommendations for use in clinical practice. Arthritis Care Res. (Hoboken). 2012;64:640–7.
van Gestel AM, Prevoo ML, van’t Hof MA, vanRijswijk MH, van de Putte LB, van R P. Development and validation of the European League Against Rheumatism response criteria for rheumatoid arthritis. Comparison with the preliminary American College of Rheumatology and the World Health Organization/International League Against Rheumatism Criteria. Arthritis Rheum. 1996;39:34–40.
Rendas-Baum R, Wallenstein GV, Koncz T, Kosinski M, Yang M, Bradley J, et al. Evaluating the efficacy of sequential biologic therapies for rheumatoid arthritis patients with an inadequate response to tumor necrosis factor-α inhibitors. Arthritis Res Ther. 2011;13:R25.
Olsen NJ, Stein CM. New drugs for rheumatoid arthritis. N Engl J Med. 2004;350:2167–79.
St Clair EW, Wagner CL, Fasanmade AA, Wang B, Schaible T, Kavanaugh A, et al. The relationship of serum infliximab concentrations to clinical improvement in rheumatoid arthritis: results from ATTRACT, a multicenter, randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2002;46:1451–9.
Edwards JCW, Szczepanski L, Szechinski J, Filipowicz-Sosnowska A, Emery P, Close DR, et al. Efficacy of B-cell-targeted therapy with rituximab in patients with rheumatoid arthritis. N Engl J Med. 2004;350:2572–81.
Choy E. Clinical experience with inhibition of interleukin-6. Rheum Dis Clin N Am. 2004;30:405–15.
Nishimoto N, Yoshizaki K, Miyasaka N, Yamamoto K, Kawai S, Takeuchi T, et al. Treatment of rheumatoid arthritis with humanized anti-interleukin-6 receptor antibody: a multicenter, double-blind, placebo-controlled trial. Arthritis Rheum. 2004;50:1761–9.
Breedveld FC. Therapeutic monoclonal antibodies. Lancet. 2000;355:735–40.
Dirks NL, Meibohm B. Population pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49:633–59.
Magdelaine-Beuzelin C, Kaas Q, Wehbi V, Ohresser M, Jefferis R, Lefranc M-P, et al. Structure-function relationships of the variable domains of monoclonal antibodies approved for cancer treatment. Crit Rev Oncol Hematol. 2007;64:210–25.
Junghans RP. Finally! The Brambell receptor (FcRB). Mediator of transmission of immunity and protection from catabolism for IgG. Immunol Res. 1997;16:29–57.
Ternant D, Paintaud G. Pharmacokinetics and concentration-effect relationships of therapeutic monoclonal antibodies and fusion proteins. Expert Opin Biol Ther. 2005;5(Suppl 1):S37–47.
Pasut G. Pegylation of biological molecules and potential benefits: pharmacological properties of certolizumab pegol. BioDrugs. 2014;28(Suppl 1):S15–23.
Jevševar S, Kusterle M, Kenig M. PEGylation of antibody fragments for half-life extension. In: Proetzel G, Ebersbach H, editors. Methods Mol. Biol. vol 901. Totowa: Humana Press; 2012. p. 233–46.
Dostalek M, Gardner I, Gurbaxani BM, Rose RH, Chetty M. Pharmacokinetics, pharmacodynamics and physiologically-based pharmacokinetic modelling of monoclonal antibodies. Clin Pharmacokinet. 2013;52:83–124.
Lobo ED, Hansen RJ, Balthasar JP. Antibody pharmacokinetics and pharmacodynamics. J Pharm Sci. 2004;93:2645–68.
Mould DR, Sweeney KRD. The pharmacokinetics and pharmacodynamics of monoclonal antibodies: mechanistic modeling applied to drug development. Curr Opin Drug Discov Dev. 2007;10:84–96.
Wang W, Wang EQ, Balthasar JP. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84:548–58.
Duffull SB, Wright DFB, Winter HR. Interpreting population pharmacokinetic-pharmacodynamic analyses: a clinical viewpoint. Br J Clin Pharmacol. 2011;71:807–14.
Mould DR, Upton RN. Basic concepts in population modeling, simulation, and model-based drug development-part 2: introduction to pharmacokinetic modeling methods. CPT Pharmacometrics Syst Pharmacol. 2013;2:e38.
Fronton L, Pilari S, Huisinga W. Monoclonal antibody disposition: a simplified PBPK model and its implications for the derivation and interpretation of classical compartment models. J Pharmacokinet Pharmacodyn. 2014;41:87–107.
Ternant D, Ducourau E, Perdriger A, Corondan A, Le Goff B, Devauchelle-Pensec V, et al. Relationship between inflammation and infliximab pharmacokinetics in rheumatoid arthritis. Br J Clin Pharmacol. 2014;78:118–28.
Ng CM, Bruno R, Combs D, Davies B. Population pharmacokinetics of rituximab (anti-CD20 monoclonal antibody) in rheumatoid arthritis patients during a phase II clinical trial. J Clin Pharmacol. 2005;45:792–801.
Weisman MH, Moreland LW, Furst DE, Weinblatt ME, Keystone EC, Paulus HE, et al. Efficacy, pharmacokinetic, and safety assessment of adalimumab, a fully human anti-tumor necrosis factor-alpha monoclonal antibody, in adults with rheumatoid arthritis receiving concomitant methotrexate: a pilot study. Clin Ther. 2003;25:1700–21.
FDA. Adalimumab. Clinical pharmacology biopharmaceutics review(s). http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/ApprovalApplications/TherapeuticBiologicApplications/ucm092770.pdf. Accessed 21 Aug 2014.
Zhou H, Jang H, Fleischmann RM, Bouman-Thio E, Xu Z, Marini JC, et al. Pharmacokinetics and safety of golimumab, a fully human anti-TNF-alpha monoclonal antibody, in subjects with rheumatoid arthritis. J Clin Pharmacol. 2007;47:383–96.
Frey N, Grange S, Woodworth T. Population Pharmacokinetic analysis of tocilizumab in patients with rheumatoid arthritis. J Clin Pharmacol. 2010;50:754–66.
Gibiansky L, Frey N. Linking interleukin-6 receptor blockade with tocilizumab and its hematological effects using a modeling approach. J Pharmacokinet Pharmacodyn. 2012;39:5–16.
Ternant D, Ducourau E, Fuzibet P, Vignault C, Watier H, Lequerré T, et al. Pharmacokinetics and concentration-effect relationship of adalimumab in rheumatoid arthritis. Br J Clin Pharmacol. 2015;79:286–97.
Hu C, Xu Z, Zhang Y, Rahman MU, Davis HM, Zhou H. Population approach for exposure-response modeling of golimumab in patients with rheumatoid arthritis. J Clin Pharmacol. 2011;51:639–48.
Ohta S, Tsuru T, Terao K, Mogi S, Suzaki M, Shono E, et al. Mechanism-based approach using a biomarker response to evaluate tocilizumab subcutaneous injection in patients with rheumatoid arthritis with an inadequate response to synthetic DMARDs (MATSURI study). J Clin Pharmacol. 2014;54:109–19.
FDA. Certolizumab pegol. Clinical pharmacology and biopharmaceutics review(s). http://www.accessdata.fda.gov/drugsatfda_docs/nda/2008/125160s000_ClinPharmR.pdf. Accessed 21 Aug 2014.
Tabrizi M, Bornstein GG, Suria H. Biodistribution mechanisms of therapeutic monoclonal antibodies in health and disease. AAPS J. 2010;12:33–43.
FDA. Certolizumab pegol label information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/125160s000lbl.pdf. Accessed 21 Aug 2014.
Hayashi N, Tsukamoto Y, Sallas WM, Lowe PJ. A mechanism-based binding model for the population pharmacokinetics and pharmacodynamics of omalizumab. Br J Clin Pharmacol. 2007;63:548–61.
Coffey GP, Stefanich E, Palmieri S, Eckert R, Padilla-Eagar J, Fielder PJ, et al. In vitro internalization, intracellular transport, and clearance of an anti-CD11a antibody (Raptiva) by human T-cells. J Pharmacol Exp Ther. 2004;310:896–904.
Tabrizi MA, Tseng C-ML, Roskos LK. Elimination mechanisms of therapeutic monoclonal antibodies. Drug Discov Today. 2006;11:81–8.
Morell A, Terry WD, Waldmann TA. Metabolic properties of IgG subclasses in man. J Clin Invest. 1970;49:673–80.
Levy G. Pharmacologic target-mediated drug disposition. Clin Pharmacol Ther. 1994;56:248–52.
Mager DE, Jusko WJ. General pharmacokinetic model for drugs exhibiting target-mediated drug disposition. J Pharmacokinet Pharmacodyn. 2001;28:507–32.
Gibiansky L, Gibiansky E. Target-mediated drug disposition model: approximations, identifiability of model parameters and applications to the population pharmacokinetic-pharmacodynamic modeling of biologics. Expert Opin Drug Metab Toxicol. 2009;5:803–12.
Ng CM, Stefanich E, Anand BS, Fielder PJ, Vaickus L. Pharmacokinetics/pharmacodynamics of nondepleting anti-CD4 monoclonal antibody (TRX1) in healthy human volunteers. Pharm Res. 2006;23:95–103.
Gibiansky L, Gibiansky E, Kakkar T, Ma P. Approximations of the target-mediated drug disposition model and identifiability of model parameters. J Pharmacokinet Pharmacodyn. 2008;35:573–91.
Ternant D, Mulleman D, Lauféron F, Vignault C, Ducourau E, Wendling D, et al. Influence of methotrexate on infliximab pharmacokinetics and pharmacodynamics in ankylosing spondylitis. Br J Clin Pharmacol. 2012;73:55–65.
Xu Z, Seitz K, Fasanmade A, Ford J, Williamson P, Xu W, et al. Population pharmacokinetics of infliximab in patients with ankylosing spondylitis. J Clin Pharmacol. 2008;48:681–95.
Fasanmade AA, Adedokun OJ, Ford J, Hernandez D, Johanns J, Hu C, et al. Population pharmacokinetic analysis of infliximab in patients with ulcerative colitis. Eur J Clin Pharmacol. 2009;65:1211–28.
Danis VA, Franic GM, Rathjen DA, Laurent RM, Brooks PM. Circulating cytokine levels in patients with rheumatoid arthritis: results of a double blind trial with sulphasalazine. Ann Rheum Dis. 1992;51:946–50.
Pouw MF, Krieckaert CL, Nurmohamed MT, van der Kleij D, Aarden L, Rispens T, et al. Key findings towards optimising adalimumab treatment: the concentration-effect curve. Ann Rheum Dis. 2015;74:513–8.
FDA. Golimumab label information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/125289s0064lbl.pdf. Accessed 21 Aug 2014.
Mélet J, Mulleman D, Goupille P, Ribourtout B, Watier H, Thibault G. Rituximab-induced T cell depletion in patients with rheumatoid arthritis: association with clinical response. Arthritis Rheum. 2013;65:2783–90.
Zhuang Y, Lyn S, Lv Y, Xu Z, Bouman-Thio E, Masterson T, et al. Pharmacokinetics and safety of golimumab in healthy Chinese subjects following a single subcutaneous administration in a randomized phase I trial. Clin Drug Investig. 2013;33:795–800.
FDA. Infliximab. Clinical pharmacology review. http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/ApprovalApplications/TherapeuticBiologicApplications/ucm107704.pdf. Accessed 21 Aug 2014.
Bendtzen K, Geborek P, Svenson M, Larsson L, Kapetanovic MC, Saxne T. Individualized monitoring of drug bioavailability and immunogenicity in rheumatoid arthritis patients treated with the tumor necrosis factor alpha inhibitor infliximab. Arthritis Rheum. 2006;54:3782–9.
Wolbink GJ, Voskuyl AE, Lems WF, de Groot E, Nurmohamed MT, Tak PP, et al. Relationship between serum trough infliximab levels, pretreatment C reactive protein levels, and clinical response to infliximab treatment in patients with rheumatoid arthritis. Ann Rheum Dis. 2005;64:704–7.
Maini RN, Elliott MJ, Brennan FM, Williams RO, Chu CQ, Paleolog E, et al. Monoclonal anti-TNF alpha antibody as a probe of pathogenesis and therapy of rheumatoid disease. Immunol Rev. 1995;144:195–223.
Gratacós J, Collado A, Filella X, Sanmartí R, Cañete J, Llena J, et al. Serum cytokines (IL-6, TNF-alpha, IL-1 beta and IFN-gamma) in ankylosing spondylitis: a close correlation between serum IL-6 and disease activity and severity. Br J Rheumatol. 1994;33:927–31.
Morcos PN, Zhang X, McIntyre C, Bittner B, Rowell L, Hussain Z. Pharmacokinetics and pharmacodynamics of single subcutaneous doses of tocilizumab administered with or without rHuPH20. Int J Clin Pharmacol Ther. 2013;51:537–48.
Maini RN, Breedveld FC, Kalden JR, Smolen JS, Davis D, Macfarlane JD, et al. Therapeutic efficacy of multiple intravenous infusions of anti-tumor necrosis factor alpha monoclonal antibody combined with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis Rheum. 1998;41:1552–63.
Jani M, Barton A, Warren RB, Griffiths CEM, Chinoy H. The role of DMARDs in reducing the immunogenicity of TNF inhibitors in chronic inflammatory diseases. Rheumatology (Oxford). 2014;53:213–22.
Ducourau E, Mulleman D, Paintaud G, Miow Lin DC, Lauféron F, Ternant D, et al. Antibodies toward infliximab are associated with low infliximab concentration at treatment initiation and poor infliximab maintenance in rheumatic diseases. Arthritis Res Ther. 2011;13:R105.
Van den Bemt BJF, den Broeder AA, Wolbink GJ, Hekster YA, van Riel PLCM, Benraad B, et al. Anti-infliximab antibodies are already detectable in most patients with rheumatoid arthritis halfway through an infusion cycle: an open-label pharmacokinetic cohort study. BMC Musculoskelet Disord. 2011;12:12.
Bartelds GM, Wijbrandts CA, Nurmohamed MT, Stapel S, Lems WF, Aarden L, et al. Clinical response to adalimumab: relationship to anti-adalimumab antibodies and serum adalimumab concentrations in rheumatoid arthritis. Ann Rheum Dis. 2007;66:921–6.
Radstake TRDJ, Svenson M, Eijsbouts AM, van den Hoogen FHJ, Enevold C, van Riel PLCM, et al. Formation of antibodies against infliximab and adalimumab strongly correlates with functional drug levels and clinical responses in rheumatoid arthritis. Ann Rheum Dis. 2009;68:1739–45.
Abe T, Takeuchi T, Miyasaka N, Hashimoto H, Kondo H, Ichikawa Y, et al. A multicenter, double-blind, randomized, placebo controlled trial of infliximab combined with low dose methotrexate in Japanese patients with rheumatoid arthritis. J Rheumatol. 2006;33:37–44.
Baert F, Noman M, Vermeire S, Van Assche G, D’ Haens G, Carbonez A, et al. Influence of immunogenicity on the long-term efficacy of infliximab in Crohn’s disease. N Engl J Med. 2003;348:601–8.
Haraoui B, Cameron L, Ouellet M, White B. Anti-infliximab antibodies in patients with rheumatoid arthritis who require higher doses of infliximab to achieve or maintain a clinical response. J Rheumatol. 2006;33:31–6.
Krieckaert CLM, Bartelds GM, Lems WF, Wolbink GJ. The effect of immunomodulators on the immunogenicity of TNF-blocking therapeutic monoclonal antibodies: a review. Arthritis Res Ther. 2010;12:217.
Van Schouwenburg PA, Krieckaert CL, Rispens T, Aarden L, Wolbink GJ, Wouters D. Long-term measurement of anti-adalimumab using pH-shift-anti-idiotype antigen binding test shows predictive value and transient antibody formation. Ann Rheum Dis. 2013;72:1680–6.
Ungar B, Chowers Y, Yavzori M, Picard O, Fudim E, Har-Noy O, et al. The temporal evolution of antidrug antibodies in patients with inflammatory bowel disease treated with infliximab. Gut. 2014;63:1258–64.
Thurlings RM, Teng O, Vos K, Gerlag DM, Aarden L, Stapel SO, et al. Clinical response, pharmacokinetics, development of human anti-chimaeric antibodies, and synovial tissue response to rituximab treatment in patients with rheumatoid arthritis. Ann Rheum Dis. 2009;69:409–12.
Imaeda H, Andoh A, Fujiyama Y. Development of a new immunoassay for the accurate determination of anti-infliximab antibodies in inflammatory bowel disease. J Gastroenterol. 2012;47:136–43.
Van Schouwenburg PA, Bartelds GM, Hart MH, Aarden L, Wolbink GJ, Wouters D. A novel method for the detection of antibodies to adalimumab in the presence of drug reveals “hidden” immunogenicity in rheumatoid arthritis patients. J Immunol Methods. 2010;362:82–8.
Garcês S, Demengeot J, Benito-Garcia E. The immunogenicity of anti-TNF therapy in immune-mediated inflammatory diseases: a systematic review of the literature with a meta-analysis. Ann Rheum Dis. 2013;72:1947–55.
Fasanmade AA, Adedokun OJ, Blank M, Zhou H, Davis HM. Pharmacokinetic properties of infliximab in children and adults with Crohn’s disease: a retrospective analysis of data from 2 phase III clinical trials. Clin Ther. 2011;33:946–64.
Xu ZH, Lee H, Vu T, Hu C, Yan H, Baker D, et al. Population pharmacokinetics of golimumab in patients with ankylosing spondylitis: impact of body weight and immunogenicity. Int J Clin Pharmacol Ther. 2010;48:596–607.
Ng CM, Loyet KM, Iyer S, Fielder PJ, Deng R. Modeling approach to investigate the effect of neonatal Fc receptor binding affinity and anti-therapeutic antibody on the pharmacokinetic of humanized monoclonal anti-tumor necrosis factor-α IgG antibody in cynomolgus monkey. Eur J Pharm Sci. 2014;51:51–8.
Perez Ruixo JJ, Ma P, Chow AT. The utility of modeling and simulation approaches to evaluate immunogenicity effect on the therapeutic protein pharmacokinetics. AAPS J. 2013;15:172–82.
Stubenrauch K, Wessels U, Birnboeck H, Ramirez F, Jahreis A, Schleypen J. Subset analysis of patients experiencing clinical events of a potentially immunogenic nature in the pivotal clinical trials of tocilizumab for rheumatoid arthritis: evaluation of an antidrug antibody ELISA using clinical adverse event-driven immunogenicity testing. Clin Ther. 2010;32:1597–609.
Ordás I, Mould DR, Feagan BG, Sandborn WJ. Anti-TNF monoclonal antibodies in inflammatory bowel disease: pharmacokinetics-based dosing paradigms. Clin Pharmacol Ther. 2012;91:635–46.
Gisbert JP, Chaparro M. Safety of anti-TNF agents during pregnancy and breastfeeding in women with inflammatory bowel disease. Am J Gastroenterol. 2013;108:1426–38.
Mahadevan U, Wolf DC, Dubinsky M, Cortot A, Lee SD, Siegel CA, et al. Placental transfer of anti-tumor necrosis factor agents in pregnant patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2013;11:286–92 (quiz e24).
Hyrich KL, Verstappen SMM. Biologic therapies and pregnancy: the story so far. Rheumatology (Oxford). 2014;53:1377–85.
Berger A. Dose intensification with infliximab in patients with rheumatoid arthritis. Ann Pharmacother. 2005;39:2021–5.
Rahman MU, Strusberg I, Geusens P, Berman A, Yocum D, Baker D, et al. Double-blinded infliximab dose escalation in patients with rheumatoid arthritis. Ann Rheum Dis. 2007;66:1233–8.
Van den Bemt BJF, den Broeder AA, Wolbink G-J, van den Maas A, Hekster YA, van Riel PLCM, et al. The combined use of disease activity and infliximab serum trough concentrations for early prediction of (non-)response to infliximab in rheumatoid arthritis. Br J Clin Pharmacol. 2013;76:939–45.
Mulleman D, Méric J-C, Paintaud G, Ducourau E, Magdelaine-Beuzelin C, Valat J-P, et al. Infliximab concentration monitoring improves the control of disease activity in rheumatoid arthritis. Arthritis Res Ther. 2009;11:R178.
Upton RN, Mould DR. Basic concepts in population modeling, simulation, and model-based drug development: part 3-introduction to pharmacodynamic modeling methods. CPT Pharmacometrics Syst Pharmacol. 2014;3:e88.
Jusko WJ, Ko HC. Physiologic indirect response models characterize diverse types of pharmacodynamic effects. Clin Pharmacol Ther. 1994;56:406–19.
Ducourau E, Ternant D, Lequerre T, Fuzibet P, Le Loet X, Watier H, et al. Towards an individualised target concentration of adalimumab in rheumatoid arthritis. Ann Rheum Dis. 2014;73:1428–9.
Keystone EC, Genovese MC, Klareskog L, Hsia EC, Hall ST, Miranda PC, et al. Golimumab, a human antibody to tumour necrosis factor alpha given by monthly subcutaneous injections, in active rheumatoid arthritis despite methotrexate therapy: the GO-FORWARD Study. Ann Rheum Dis. 2009;68:789–96.
Lacroix BD, Lovern MR, Stockis A, Sargentini-Maier ML, Karlsson MO, Friberg LE. A pharmacodynamic Markov mixed-effects model for determining the effect of exposure to certolizumab pegol on the ACR20 score in patients with rheumatoid arthritis. Clin Pharmacol Ther. 2009;86:387–95.
Furuya Y, Ozeki T, Takayanagi R, Yokoyama H, Okuyama K, Yamada Y. Theory based analysis of anti-inflammatory effect of infliximab on Crohn’s disease. Drug Metab Pharmacokinet. 2007;22:20–5.
Kimura K, Takayanagi R, Yokoyama H, Yamada Y. Theory-based analysis of anti-inflammatory effect of infliximab on Crohn’s disease and rheumatoid arthritis. Rheumatol Int. 2012;32:145–50.
Stepensky D. Local versus systemic anti-tumour necrosis factor-α effects of adalimumab in rheumatoid arthritis. Clin Pharmacokinet. 2012;51:443–55.
FDA. Adalimumab label information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/125057s0215lbl.pdf. Accessed 21 Aug 2014.
FDA. Infliximab label information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/103772s5359lbl.pdf. Accessed 21 Aug 2014.
FDA. Rituximab label information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/103705s5414lbl.pdf. Accessed 21 Aug 2014.
FDA. Tocilizumab label information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/125276s092lbl.pdf. Accessed 21 Aug 2014.
Bongartz T, Sutton AJ, Sweeting MJ, Buchan I, Matteson EL, Montori V. Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA. 2006;295:2275–85.
Lopez-Olivo MA, Tayar JH, Martinez-Lopez JA, Pollono EN, Cueto JP, Gonzales-Crespo MR, et al. Risk of malignancies in patients with rheumatoid arthritis treated with biologic therapy: a meta-analysis. JAMA. 2012;308:898–908.
Michaud TL, Rho YH, Shamliyan T, Kuntz KM, Choi HK. The comparative safety of tumor necrosis factor inhibitors in rheumatoid arthritis: a meta-analysis update of 44 trials. Am J Med. 2014;127:1208–32.
Singh JA, Noorbaloochi S, Singh G. Golimumab for rheumatoid arthritis. Cochrane Database Syst. Rev. 2010;CD008341.
Bredemeier M, de Oliveira FK, Rocha CM. Low- versus high-dose rituximab for rheumatoid arthritis: a systematic review and meta-analysis. Arthritis Care Res. (Hoboken). 2014;66:228–35.
Salliot C, Dougados M, Gossec L. Risk of serious infections during rituximab, abatacept and anakinra treatments for rheumatoid arthritis: meta-analyses of randomised placebo-controlled trials. Ann Rheum Dis. 2008;68:25–32.
Campbell L, Chen C, Bhagat SS, Parker RA, Östör AJK. Risk of adverse events including serious infections in rheumatoid arthritis patients treated with tocilizumab: a systematic literature review and meta-analysis of randomized controlled trials. Rheumatology (Oxford). 2011;50:552–62.
Ruiz Garcia V, Jobanputra P, Burls A, Cabello JB, Gálvez Muñoz JG, Saiz Cuenca ES, et al. Certolizumab pegol (CDP870) for rheumatoid arthritis in adults. Cochrane database Syst. Rev. Chichester: Wiley; 1996. p. CD007649.
Krzyzanski W, Perez Ruixo JJ. Lifespan based indirect response models. J Pharmacokinet Pharmacodyn. 2012;39:109–23.
Hanauer SB, Sandborn WJ, Rutgeerts P, Fedorak RN, Lukas M, MacIntosh D, et al. Human anti-tumor necrosis factor monoclonal antibody (adalimumab) in Crohn’s disease: the CLASSIC-I trial. Gastroenterology. 2006;130:323–33 (quiz 591).
Karmiris K, Paintaud G, Noman M, Magdelaine-Beuzelin C, Ferrante M, Degenne D, et al. Influence of trough serum levels and immunogenicity on long-term outcome of adalimumab therapy in Crohn’s disease. Gastroenterology. 2009;137:1628–40.
Tani K, Takayanagi R, Yokoyama H, Yamada Y. Theoretical analysis of efficacy of biological agent for rheumatoid arthritis based on target molecular binding occupancy. Rheumatol Int. 2013;33:1791–5.
Van der Meer AF, Marcus MAE, Touw DJ, Proost JH, Neef C. Optimal sampling strategy development methodology using maximum a posteriori Bayesian estimation. Ther Drug Monit. 2011;33:133–46.
Andreu F, Colom H, Grinyó JM, Torras J, Cruzado JM, Lloberas N. Development of a population PK model of tacrolimus for adaptive dosage control in stable kidney transplant patients. Ther Drug Monit. 2015;37:246–55.
Staatz CE, Tett SE. Clinical pharmacokinetics and pharmacodynamics of mycophenolate in solid organ transplant recipients. Clin Pharmacokinet. 2007;46:13–58.
Gotta V, Widmer N, Montemurro M, Leyvraz S, Haouala A, Decosterd LA, et al. Therapeutic drug monitoring of imatinib: Bayesian and alternative methods to predict trough levels. Clin Pharmacokinet. 2012;51:187–201.
Nezic L, Derungs A, Bruggisser M, Tschudin-Sutter S, Krähenbühl S, Haschke M. Therapeutic drug monitoring of once daily aminoglycoside dosing: comparison of two methods and investigation of the optimal blood sampling strategy. Eur J Clin Pharmacol. 2014;70:829–37.
Le J, Ngu B, Bradley JS, Murray W, Nguyen A, Nguyen L, et al. Vancomycin monitoring in children using bayesian estimation. Ther Drug Monit. 2014;36:510–8.
Lau KS, Juchheim AM, Cavaliere KR, Philips SR, Lauffenburger DA, Haigis KM. In vivo systems analysis identifies spatial and temporal aspects of the modulation of TNF-α-induced apoptosis and proliferation by MAPKs. Sci Signal. 2011;4:ra16.
Basak S, Behar M, Hoffmann A. Lessons from mathematically modeling the NF-κB pathway. Immunol Rev. 2012;246:221–38.
Lau KS, Cortez-Retamozo V, Philips SR, Pittet MJ, Lauffenburger DA, Haigis KM. Multi-scale in vivo systems analysis reveals the influence of immune cells on TNF-α-induced apoptosis in the intestinal epithelium. PLoS Biol. 2012;10:e1001393.
Hayashi K, Piras V, Tabata S, Tomita M, Selvarajoo K. A systems biology approach to suppress TNF-induced proinflammatory gene expressions. Cell Commun Signal. 2013;11:84.
Lahoz-Beneytez J, Schnizler K, Eissing T. A pharma perspective on the systems medicine and pharmacology of inflammation. Math Biosci. 2015;260:2–5.
Martin PL, Bugelski PJ. Concordance of preclinical and clinical pharmacology and toxicology of monoclonal antibodies and fusion proteins: soluble targets. Br J Pharmacol. 2012;166:806–22.
Loisel S, Ohresser M, Pallardy M, Daydé D, Berthou C, Cartron G, et al. Relevance, advantages and limitations of animal models used in the development of monoclonal antibodies for cancer treatment. Crit Rev Oncol Hematol. 2007;62:34–42.
Acknowledgments
CNRS UMR 7292 participates in the Consortium “Monitoring of monoclonal Antibodies Group in Europe” (MAGE) for inflammatory diseases. The MAGE Consortium is supported by LE STUDIUM Loire Valley Institute for Advanced Studies (http://www.lestudium-ias.com/). CNRS UMR 7292 is also partly supported by the French Higher Education and Research Ministry under the program “Investissements d’avenir” Grant Agreement: LabEx MAbImprove ANR-10-LABX-53-01.
Disclosure
Gilles Paintaud has been a consultant for Laboratoire Français du Fractionnement et des Biotechnologies (LFB) and Pierre Fabre Laboratories. His research team has received grants from Roche Pharma, Chugai, Pfizer, Novartis, and Janssen.
Denis Mulleman has been a consultant and has given lectures on behalf of his institution for Pfizer and MSD. He has been invited to attend international congresses by MSD.
Theodora Bejan-Angoulvant, Christophe Passot, and David Ternant declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ternant, D., Bejan-Angoulvant, T., Passot, C. et al. Clinical Pharmacokinetics and Pharmacodynamics of Monoclonal Antibodies Approved to Treat Rheumatoid Arthritis. Clin Pharmacokinet 54, 1107–1123 (2015). https://doi.org/10.1007/s40262-015-0296-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-015-0296-9