Purpose
TRX1 is a nondepleting anti-CD4 monoclonal IgG1 antibody being developed to induce tolerance by blocking CD4-mediated functions. The purpose of this study is to describe the pharmacokinetics (PK) and pharmacodynamics (PD) of TRX1 and to develop a receptor-mediated PK/PD model that characterizes the relationships between serum TRX1 concentration and total and free CD4 expression in healthy male volunteers.
Methods
Nine subjects from three dosing cohorts in double-blinded, placebo-controlled phase I clinical study was included in the analysis. Serum TRX1 levels were determined using enzyme-linked immunosorbent assay. Blood total and free CD4 receptor levels were determined by using flow cytometric analyses. The receptor-mediated PK/PD model was developed to describe the dynamic interaction of TRX1 binding with CD4 receptors.
Results and Conclusions
TRX1 displayed nonlinear pharmacokinetic behavior and the CD4 receptors on T cells were saturated and down-modulated following treatment with TRX1. Results from in vitro studies using purified human T cells suggested that CD4-mediated internalization may constitute one pathway by which CD4 is down-modulated and TRX1 is cleared in vivo. The developed receptor-mediated PK/PD model adequately described the data. This PK/PD model was used to simulate PK/PD time profiles after different dosing regimens to help guide the dose selection in future clinical studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
CD4+ T cells are key mediators in the initiation and perpetuation of both normal and pathogenic immune responses directed against self-antigens, which can contribute to autoimmune diseases and organ rejection in transplantation. Anti-CD4 antibodies have been consistently shown to induce durable, antigen-specific tolerance to soluble proteins (1,2) and tissue organ transplants (3,4), and to reestablish self-tolerance in rodent model of autoimmune disease (5,6). However, successfully transferring these positive results from rodent models into the clinical setting has met with disappointing results. Over the past several years, several different anti-CD antibodies have been evaluated in clinical studies encompassing a wide range of indication including rheumatoid arthritis (7–9), multiple sclerosis (10–12), psoriasis (13,14), transplant, Crohn’s disease (15,16), and asthma (17). However, the therapeutic effectiveness of these antibodies was modest at best, of short duration, and most likely the consequence of transient immunosuppression. Failure of these anti-CD4 antibodies to produce durable and robust response may be attributed to factors relating to both antibody properties and dose. For example, early clinical studies used murine and chimeric anti-CD4 antibodies that were highly immunogenic, and therefore elicited neutralizing human antimouse antibody and antichimeric antibody response that led to the rapid clearance of these anti-CD4 antibodies (10,17,18). Furthermore, many anti-CD4 antibodies used in previous clinical studies depleted CD4+ T cells, and failed to recognize the advantages of nondepleting anti-CD4 antibodies because the major regulatory T-cell population mediated tolerance is CD4 itself (19,20). In addition, the dose of anti-CD4 antibodies used in most clinical studies, although sufficient to induce varying degrees of immunosuppression, may be too low to induce long-term immunological tolerance because of adverse side effects or the T-cell-depleting nature of these antibodies.
To overcome these potential limitations, a novel humanized anti-CD4 monoclonal IgG1κ antibody was developed to reduce immunogenicity. In addition, one of the amino acid in the Fc region of the heavy chain was modified to reduce FcR interactions and complement binding in order to avert CD4 depletion and infusion reactions. In nonhuman primates, it was demonstrated that a short course of high-dose TRX1 induced a long-term, antigen-specific tolerance to foreign antigens without compromising normal immune function or depleting CD4 lymphocytes (21).
In this report we describe the pharmacokinetic (PK) and pharmacodynamic (PD) profiles of the anti-CD4 antibody TRX1 in normal human volunteers and show that anti-CD4 antibody TRX1 clearance is likely mediated in part by cellular binding and internalization. Furthermore, PK/PD data from the phase I study was used to develop a mechanism-based PK/PD model to describe the receptor-mediated drug disposition of TRX1 and its modulatory effect on CD4 receptors. This model was also utilized to simulate the PK/PD time profiles following different dosing regimens to help guide dose selection for future clinical studies.
Materials and Methods
Antibody
TRX1 is a humanized monoclonal antibody with a molecular weight of 150 kDa, and composed of two identical heavy chains (composed of 44 amino acids each) and two identical light chains (composed of 218 amino acids each), each held together by disulfide bonds. The antibody was formulated for an intravenous infusion at 5.49 mg mL−1 in 20 mM histidine and was supplied in 5-mL glass vials with silicone polymerized butyl rubber stoppers and aluminum crimp seals.
Clinical Study Design
The phase I study was a single-center, double-blind, randomized, placebo-controlled study to investigate the safety, tolerability, PK, and PD of single rising doses of TRX1. The study was conducted at Quintiles Drug Metabolism and Pharmacokinetics Unit in Edinburgh, UK. Four healthy male subjects (per dose group) received a single 2-h intravenous infusion of TRX1 at the dose levels of 1, 5, and 10 mg kg−1. Within each dose group, three subjects were randomized to receive TRX1 and one subject to receive placebo. The study was approved by the institutional review board; all subjects gave written informed consent for their participation in the study. A total of 12 subjects were enrolled in the study. Summary statistics of subject demographic details by treatment are shown in Table I. PK blood samples were collected at day0 preinfusion, 0.5, 1, 2, 3, 5, 6, 8, 12, 24 h (day 1), 48 (day 2) and 72 h (day 3) after commencement of infusion, days 5, 7, 10, 15, 22, and 29, and every 2 weeks thereafter until CD4 levels returned to baseline. PD blood samples (5 mL) were collected from all the patients at the following times to measure total and free CD4 receptors: screening, day 1 (admission), day 0 preinfusion, 3, 12, 24 h (day 2), 48 h (day 3), and 72 h (day 3) after commencement of infusion, days 5, 7, 10, 15, 22, and 29, and thereafter every 2 weeks until TRX1 binding to lymphocytes was no longer detectable.
Analytical Methods
PK Assay
Blood samples were drawn either by direct venipuncture or via an intravenous catheter and collected into plain vacutainers without anticoagulant. Samples were allowed to stand for 60 min to allow the clot to retract, and then centrifuged at 2500 rpm for 10 min at room temperature. The resulting serum was stored at −70°C until further analysis. Serum levels of TRX1 were determined using an enzyme-linked immunosorbent assay (ELISA). The assay was validated over the concentration range of 156–10,000 ng mL−1 TRX1 with precision ranging from 5.98 to 24.2%.
PD Assay
Blood samples were collected into sodium heparin vacutainers and stored at ambient temperatures of 18–22°C. The samples were analyzed by flow cytometry using FACSCalibur 4-color Analyzer (Becton Dickinson, Cowley, UK). One hundred microliters of blood was added to a tube (12×75 mm) containing 1 μg per stain of primary antibodies, i.e., CD8-FITC, CD4-PE, CD3-PerCP, CD45RA. Contents in the tube were mixed well and incubated in the dark at room temperature for 20 min, after which 2 mL of lysis reagent was added. Each tube was vortexed and incubated inthe dark at room temperature for 10 min. The tubes were centrifuged for 5 min at 200 × g and the supernatant removed. The cells were then fixed by adding 0.5 mL of 1% paraformaldehyde and the tubes were stored until analysis (2–4 h) at 4°C.
The saturation of CD4+ lymphocytes and monocytes was monitored by staining blood samples with TRX-1 biotin followed by fluorescein isothiocyanate (FITC)–streptavidin to detect free CD4 sites on cells. T lymphocytes and monocytes were identified by staining with CD3 and CD14, respectively. Coating of CD4 by TRX1 was detected in a separate tube by staining with F(ab′)2 fragment of goat antihuman IgG–biotin, followed by FITC–streptavidin. Data were reported as percent TRX1–biotin stained CD3(+) and CD14(+) cells and percent antihuman IgG stained CD3(+) and CD14(+) cells. Mean channel fluorescence (MCF) was reported for each population as well.
Isolation of Human T Cells
Human T cells were isolated from 100 mL of anonymous whole donor blood using T-cell Negative Isolation Kit (22) (Dynal Biotech, Lake Success, NY, USA). Lymphocytes were separated from whole blood using the Ficoll gradient method (ICN Pharmaceuticals Biochemicals Division, Aurora, OH, USA). The isolated lymphocytes were then suspended in 20 mL of complete media (RPMI 1640, 10% fetal bovine serum, 1% glutamine, 1% penicillin/streptomycin, and 1% sodium pyruvate) in a tissue culture flask and placed in a humidified 37°C tissue incubator for 1 h to allow monocytes and macrophages to attach. Following incubation, the unattached cells were removed from the flasks and resuspended at 107 cells per 200 μl of PBS containing 0.1% bovine serum albumin. Twenty microliters of fetal bovine serum per 107 cells was added, followed by the addition of 20μl of Antibody Mix (Dynal Biotech) for 10 min at 4°C. Excess antibody was washed out, and T cells were negatively separated followed by exposure to a magnetic source. Recovered T cells were greater than 97% in purity, as determined by flow cytometry using FITC-conjugated anti-CD3 monoclonal antibody (data not shown).
Wide-Field Fluorescent Microscopy
Human T cells were incubated with TRX1-488 at a ratio of 106 cells per 1 μg of antibody in 200 μl of PBS for 30 min at 4°C. The cells were washed and then incubated in the same volume with 1 μg of antihuman IgG for an additional 30 min at 4°C. Cells were then washed and incubated at 37°C for a range of time points. At the conclusion of each incubation time point, cells were placed on ice. At the conclusion of all time points, cells were incubated with 5 μM DiI for 5 min at 37°C or 50 nM LysoTracker Red for 30 min at 37°C to label the lysosomes (Molecular Probe, Eugene, OR, USA). In addition, cells were incubated for 5 min with 100 nM Hoechst 33342 (Calbiochem, Bad Soden, Germany) at 37°C to label the nucleus. Labeled cells were then attached to poly[l] lysine-coated plates and assessed for TRX1-488 antibody internalization and subcellular localization using wide-field fluorescent microscopy (22).
Data Analysis
Pharmacokinetic Variables
PK parameters of TRX1 were initially estimated by noncompartmental methods using WinNonlin Pro software, Version 3.1 (Pharsight Corporation, Mountain View, CA, USA). Maximum concentration (C max) and time to C max (T max) were the observed values. Area under the plasma concentration–time curve from zero to last observable time (AUClast) was estimated using the trapezoidal rule. Terminal half-life (t 1/2) was calculated using the terminal linear portion of the log concentration–time curve.
Pharmacodynamic Variables
The pharmacodynamic parameters, free CD4, and total CD4 sites were calculated for each subject at each time point. The PD parameters are represented as a ratio from baseline (using the average of PD estimates at screening, day −1, and day 0 preinfusion).
PK/PD Model
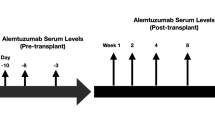
A receptor-mediated pharmacokinetic (PK)/pharmacodynamic (PD) model (23,24) characterizing the relationship between serum TRX1 concentration and total and free CD4 expression was developed (Fig. 1) and simultaneously fitted to both sets of PK/PD data. Drug in the plasma or central compartment was assumed to be eliminated by both nonspecific elimination (K el) and specific receptor-mediated endocytosis. Receptor-mediated endocytosis was modeled as an interaction with free CD4 receptor (R f) to form a drug-receptor complex (X R) via reversible (K on and K off) binding, followed by cellular internalization (K int). A tissue compartment with linear first-order distribution processes (K ct and K tc) was used to account for nonspecific drug binding or distribution.
The differential equations used to describe the PK/PD model (Fig. 1) of TRX1 are as follows:
where X c and X t are the amount of free TRX1 in central and tissue compartment, respectively; R f and X R are the free CD4 and TRX1–CD4 complex concentrations, respectively; K tc and K ct are the first-order distribution rate constants; K el is the first-order nonspecific elimination rate constant from the central compartment; V c is the volume of distribution of TRX1 in the central compartment; K syn and K deg are the zero-order synthesis rate and first-order elimination rate constants of free CD4 receptor, respectively; K on and K off are the association and dissociation rate constants for TRX1–CD4 binding, respectively; and K int is the first-order internalization/degradation rate constant of CD4 receptor complex. SCL is the conversion factor to convert the fluorescent intensity value of free and total CD4 to concentration (nM).
This model was simultaneously fitted to the individual TRX1 concentration data, the total CD4 expression, and the free CD4 receptor sites by use of an iterative two-stage modeling approach (25) implemented in S-ADAPT II program, an augmented version of ADAPT II with population analysis capabilities (26,27). The intersubject variability was assumed to be log normally distributed and was fitted by use of an exponential model. A proportional error model was used to describe the intrasubject variability. With the assumption that the PK/PD system will remain constant after continuous exposure, the final model was then used to simulate the PK/PD profiles of the different multiple dosing regimens. The dose levels of TRX1 simulated were 1, 2, 3, 4, and 5 mg kg−1 i.v. infusion over 2 h on days 0, 4, 9, and 13.
Results
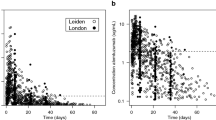
In the study, TRX1 seemed to be well tolerated by the subjects, and first dose side effects, such as fevers, chills, and hypotension, were not observed. The 10 mg kg−1 dose group of TRX1 was associated with pruritic rashes in two out of three subjects. Both subjects were prescribed oral antihistamine. In both cases, the rashes were resolved completely. TRX1 did not deplete the total lymphocyte counts (Fig. 2). The pharmacokinetic parameters of TRX1 profiles (Fig. 3A–C), estimated using noncompartmental analyses, are shown in Table II. Serum TRX1 concentrationsdeclined with a mean apparent terminal half-life of approximately 0.77 to 2.55 days over the dose range of 1–10 mg kg−1. Following a single intravenous infusion of TRX1 administered over 2 h to healthy young subjects, C max increased in a dose-proportional manner. However, the extent of systemic exposure, \(AUC_{{0 - \infty }} \), increased in a greater than dose-proportional manner for TRX1 (i.e., dose-dependent kinetics) over the dose range 1–10 mg kg−1, suggesting the nonlinearity of TRX1 pharmacokinetics. Serum TRX1 concentrations were below the limit of quantification of the assay in the three subjects following 1, 5, and10 mg kg−1 TRX1 by days 5, 15, and 29, respectively.
The CD4 receptor levels were saturated by more than 90% relative to placebo and the duration of maximal effect lasted from 3 h post-TRX1 administration up to 3, 10, and 15 days, following the administration of 1, 5, and 10 mg kg−1 TRX1, respectively (Fig. 3A–C). The levels of total CD4 were reduced by more than 70% relative to placebo, and the duration of maximal effect and the start of the return to baseline levels at each dose level for total CD4 were similar to that of free CD4, with the exception of onset of maximal effect being 12 h post-TRX1 administration. Furthermore, the duration of maximum coating and down-modulation of CD4 receptors increased with increasing dose (Fig. 3A–C).
Wide-field fluorescent microscopy was used to assess the TRX1-induced internalization of CD4 and subcellular localization of T cell internalized TRX1 antibody in isolated human T cells. At time 0, TRX1-488 was localized to the plasma membrane (left panel, Fig. 4A). The internalization of TRX1-488 was observed as early as 15 min, and at 30 min, most of the TRX1-488 located on the plasma membrane was internalized, as there was noticeably less antibody associated with the plasma membrane relative to time 0. Aliquots of these cells incubated in the presence of TRX1-488 for 30 min at 37°C were labeled with LysoTracker Red and Hoechst 33342 to determine whether the internalized antibody is located within the lysosome. Results from this analysis are presented in Fig. 4B. The left panel represents the internalization of TRX1-488 by purified human T cells. The center panel shows the subcellular location of lysosomes in these cells, whereas the right panel shows the merged image of left and center panels, suggesting that the internalized TRX1-488 is located within the lysosomes.
Internalization and subcellular localization of TRX1. Wide-field fluorescent microscopy of purified human T cells incubated with TRX1 antibody conjugated to AlexaFluor 488 (green). (A) Cells were incubated with TRX1-488 and labeled with plasma membrane marker DiI (red) and cytoplasmic marker Hoechst 33342 (blue). The left, center, and right panels represent the internalization of TRX1-488 for 0, 15, and 30 min, respectively. (B) Cells were incubated with TRX1-488 for 30 min and then labeled with lysosome marker LysoTracker Red (red) and Hoechst 33342 (blue). The left panel shows the location of TRX1-488, the center panel shows the location of LysoTracker Red, and the right panel is the merged image of left and center panels.
A fully integrated mechanism-based PK/PD model was developed to describe the serum TRX1 and free and total CD 4 receptor time profiles in human subjects (Fig. 1). The nonlinear pharmacokinetic behavior of TRX1 was assumed to be primarily due to binding of the drug to the CD4 receptors. Figure 3A–C represents the model fitted TRX1 serum concentration, free CD4 sites, and the total CD4 expression data from phase I for subjects 3, 4, and 9, respectively. As shown in Fig. 3A–C, the model fitted the data reasonably well and helped explain the receptor-mediated drug disposition for TRX1 and its effect on CD4 receptors in humans. The residuals were well distributed and there was no systematic bias identified in the goodness-of-fit plots (Fig. 5A and B). In addition, the % CV values calculated for the model parameter estimates were relatively low and indicative of a good model fit (Table III). The equilibrium dissociation constant K d, calculated as the ratio of K off and K on, was estimated to be 19.38 nM, which indicates a high affinity of the antibody to the CD4 receptors.
The PK/PD model was utilized to simulate the data for a multiple dose regimen of TRX1 at various dose levels to help guide the dose selection process for future clinical studies. Simulated profiles were obtained for dosing regimens of 1, 2, 3, 4, and 5 mg kg−1 i.v. infused over 2 h on days 0, 4, 9, and 13 (Fig. 6). Figure 6A and B represents the simulated plasma concentration profiles for TRX1 and free CD4 receptor sites, respectively, at different dosing regimens. Based on the analysis of preclinical efficacy model, it is assumed that the reduction in free CD4 receptor levels could be utilized as a possible marker to aid in dose selection for future clinical doses (21). The CD4 levels at the 1 mg kg−1 dose level recovered to greater than 50% of baseline before the second and third doses, and greater than 35% before the fourth dose (Fig. 6B). However, as evident in Fig. 6B, free CD4 receptors were persistently below set target of 20% up to 24, 31, 36, and 40 days at the 2, 3, 4, and 5 mg kg−1 level.
Figure 7 represents the percentage of contribution of receptor-mediated clearance of TRX1 at various dose levels. It is evident that at lower dose levels the clearance mechanism due to receptor-mediated endocytosis contributed more toward the elimination of the drug than at the higher dose levels because of the saturation of the receptor at higher doses. The contribution of the receptor-mediated clearance ranged from 58.5 to 94.4% at various dose levels.
Discussion
TRX1, an anti-CD4 monoclonal IgG1 antibody, is currently being developed to induce tolerance against foreignproteins, biologic therapeutics, allograft-transplanted organs, and ultimately to self-antigens in autoimmune settings by blocking CD4-mediated functions. In this first human trial of TRX1, pharmacokinetics and pharmacodynamics were investigated after a single intravenous infusion (1–10 mg kg−1) in healthy normal volunteers. The convex shape of the serum concentration–time profiles, and greater than dose-proportional increase in systemic exposure (\(\text{AUC}_{0 - \infty }\)) from a dose range 1–10 mg kg−1 suggested that TRX1 pharmacokinetics in humans is nonlinear. Although TRX1 does not affect the number of circulating T cells (Fig.2), it does coat and down-modulate the CD4 receptors in a dose- and concentration-dependent manner. Coating anddown-modulation of the CD4 antigen by TRX1 were evident in all dose groups studied. The duration of maximum coating and down-modulation of CD4 receptors increased with increasing dose from 1 to 10 mg kg−1. Overall, the pharmacokinetic and pharmacodynamic profiles of TRX1 suggested that receptor-mediated clearance of TRX1 may represent one mechanism by which TRX1 is cleared, and CD4 receptor was saturated and down-modulated after TRX1 treatment in human subjects. In general, majority of the antibodies that modulate the cell surface antigen expression do so through a process similar to receptor-mediated endocytosis of the entire immunocomplex, where the antibody and antigen enter common or distinct pathways for recycling and/or degradation (28). A recent study using human T cells as a model to study the cellular uptake and clearance of efalizumab suggested that this anti-CD11a monoclonal IgG1 antibody is internalized by purified T cells. This CD11a-mediated internalization constitutes one important pathway by which efalizumab is cleared in human (22). Therefore, it is possible that the receptor-mediated clearance of TRX1 and CD4 receptor saturation and down-modulation observed in this study may be mediated by cellular internalization of the TRX1–CD4 receptor complex. Using the purified human T-cell model, we showed that TRX1 was internalized in vitro by human T cells. In addition, the internalized TRX1 was found in subcellular organelles that stained positive for LysoTracker, the fluorescent marker for lysosomes. These results suggested that CD4-mediated internalization and lysosomal targeting of TRX1 may be one pathway by which this antibody is cleared in human.
The findings from the in vitro study were then used to develop a mechanism-based PK/PD model that describes the PK/PD behavior of TRX1 after the i.v. infusion of various dose levels in human subjects. The proposed model described the relationship between serum TRX1 concentration and total and free CD4 reasonably well. The final estimated value of V c (41.7 mL kg−1) closely resembles the plasma volume in humans (∼42.8 mL kg−1) (29), as is expected for a high molecular weight protein and was consistent with the values reported for other monoclonal IgG1 antibodies (30,31). The elimination rate constant (K el) is 0.078 days−1, and represents the elimination of TRX1 from the central compartment in the absence of receptor-mediated endocytosis. Therefore, the theoretical β phase elimination half-life in the absence of receptor-mediated endocytosis can be calculated using the following equation:
This value falls within the range of 15–21 days of the β phase half-life of natural IgG in human (32). The TRX1–CD4 dissociation rate constant, K d, calculated as the ratio of the model estimated K off and K on values, is estimated as 19.38 nM. This finding is different than the K d values of 0.6 ± 0.3 nM obtained from in vitro studies (unpublished data; TolerRx, Inc.). One possible reason for the difference is that the K d value estimated from the model reflects the binding affinity in a “real-time” clinical setting (i.e., within an open and dynamic biological system with disposition pathways for free TRX1, free CD4, and TRX1–CD4 complexes), whereas the K d values estimated by in vitro binding studies were performed under closed microsystem with controlled experimental conditions.
The model takes into account the receptor-mediated endocytosis and nonspecific mechanism of elimination as the elimination pathway of TRX1. Therefore, the total systemic clearance of the TRX1 (CLtotal) can be calculated as follows (24):
where R total is the amount of total CD4 receptors. When the TRX1 concentration is very high, DR → R total and CLtotal was reduced to K el V c, which is a clearance due to nonspecific elimination pathways. Likewise, when the TRX1 concentrations is very low compared to amount of total CD4 receptors, DR → 0, and the CLtotal becomes:
Therefore, it is expected that at a very high TRX1 concentration in patients who receive large doses, the receptor-mediated elimination of TRX1 will become less significant, and the elimination of TRX1 is mainly attributable to linear nonspecific elimination pathways. Therefore, the contribution of CD4 receptor-mediated pathways on TRX1 elimination should decrease as the dose increases. This was confirmed by comparing the values of K el V c obtained from the model to the clearance obtained from the noncompartmental analysis of i.v. single-dose data. The contribution of the nonspecific mechanism of elimination, K el, was thus calculated to be 8.6, 27.1, and 41.7% of the clearance values at 1, 5, and 10 mg kg−1 dose levels, respectively; this finding was further supported by using the simulation study. Figure 7 represents the simulated percentage of eliminated drug due to receptor-mediated clearance mechanisms after a single dose administration. The values obtained for the contribution of the nonspecific clearance of TRX1 are similar to the ones obtained as a ratio of K el V c and total clearance. It is evi-dent that K el does not represent a significant mechanism of elimination until higher i.v. doses (5 mg kg−1) are administered. This can be explained by the hypothesis that receptor-mediated elimination pathway is saturated at higher doses and the contribution of receptor-mediated endocytosis decreases as dose increases.
TRX1 is currently in development for induction of tolerance in autoimmune diseases and organ transplants. Results from the preclinical and phase I studies with TRX1 were promising and indicated that the free CD4 levels could be reduced below 20% baseline up to a period of 15 days at the highest dose level. To achieve reduction in free CD4 levels for an extended period of time, a regimen of multiple i.v. infusions could be further administered. However, the determination of the number and optimal schedule of infusions in human population is associated with a financial and time constraint. Therefore a PK/PD model explaining the disposition of drug in relation to the expression of free receptor sites would lend an understanding in the feasibility and design of a rational clinical study. In this study we have developed an integrated PK/PD model to characterize the i.v. dosing of TRX1 at various dose levels in humans. The developed model described the serum TRX1 and free and total CD4 receptor time profiles reasonably well. The developed PK/PD model was used to simulate PK/PD time profiles after different dosing regimens to guide dose selection in future clinical studies.
References
N. L. Gutstein W. E. Seaman J. H. Scott D. Wofsy (1986) ArticleTitleInduction of immune tolerance by administration of monoclonal antibody to L3T4 J. Immunol. 137 1127–1132 Occurrence Handle1:CAS:528:DyaL28XltlWrsrY%3D Occurrence Handle3090139
S. Qin S. Cobbold H. Tighe R. Benjamin H. Waldmann (1987) ArticleTitleCD4 monoclonal antibody pairs for immunosuppression and tolerance induction Eur. J. Immunol. 17 1159–1165 Occurrence Handle1:STN:280:DyaL2szgsVCmtQ%3D%3D Occurrence Handle2441998
S. P. Cobbold G. Martin H. Waldmann (1990) ArticleTitleThe induction of skin graft tolerance in major histocompatibility complex-mismatched or primed recipients: primed T cells can be tolerized in the periphery with anti-CD4 and anti-CD8 antibodies Eur. J. Immunol. 20 2747–2755 Occurrence Handle1:STN:280:DyaK3M%2FpvFChtw%3D%3D Occurrence Handle1980112
S. E. Marshall S. P. Cobbold J. D. Davies G. M. Martin J. M. Phillips H. Waldmann (1996) ArticleTitleTolerance and suppression in a primed immune system Transplantation 62 1614–1621 Occurrence Handle1:STN:280:DyaK2s7isFGnsg%3D%3D Occurrence Handle8970617
P. Hutchings L. O'Reilly N. M. Parish H. Waldmann A. Cooke (1992) ArticleTitleThe use of a non-depleting anti-CD4 monoclonal antibody to re-establish tolerance to beta cells in NOD mice Eur. J. Immunol. 22 1913–1918 Occurrence Handle1:STN:280:DyaK38zisVejug%3D%3D Occurrence Handle1623929
J. M. Phillips S. Z. Harach N. M. Parish Z. Fehervari K. Haskins A. Cooke (2000) ArticleTitleNondepleting anti-CD4 has an immediate action on diabetogenic effector cells, halting their destruction of pancreatic beta cells J. Immunol. 165 1949–1955 Occurrence Handle1:CAS:528:DC%2BD3cXls1Kms7Y%3D Occurrence Handle10925277
C. Herzog C. Walker W. Muller P. Rieber C. Reiter G. Riethmuller P. Wassmer H. Stockinger O. Madic W. J. Pichler (1989) ArticleTitleAnti-CD4 antibody treatment of patients with rheumatoid arthritis. I. Effect on clinical course and circulating T cells J. Autoimmun. 2 627–642 Occurrence Handle1:STN:280:DyaK3c%2Fis1OgsQ%3D%3D Occurrence Handle2572230
G. Horneff G. R. Burmester F. Emmrich J. R. Kalden (1991) ArticleTitleTreatment of rheumatoid arthritis with an anti-CD4 monoclonal antibody Arthritis Rheum. 34 129–140 Occurrence Handle1:STN:280:DyaK3M7js1Kjsg%3D%3D Occurrence Handle1994909
G. Horneff F. Emmrich G. R. Burmester (1993) ArticleTitleAdvances in immunotherapy of rheumatoid arthritis: clinical and immunological findings following treatment with anti-CD4 antibodies Br. J. Rheumatol. 32 IssueIDSuppl 4 39–47 Occurrence Handle8099518
E. Racadot L. Rumbach M. Bataillard J. Galmiche J. L. Henlin M. Truttmann P. Herve J. Wijdenes (1993) ArticleTitleTreatment of multiple sclerosis with anti-CD4 monoclonal antibody. A preliminary report on B-F5 in 21 patients J. Autoimmun. 6 771–786 Occurrence Handle10.1006/jaut.1993.1063 Occurrence Handle1:STN:280:DyaK2c3gs1Chtw%3D%3D Occurrence Handle8155256
B. W. Oosten Particlevan M. Lai F. Barkhof D. H. Miller I. F. Moseley A. J. Thompson S. Hodgkinson C. H. Polman (1996) ArticleTitleA phase II trial of anti-CD4 antibodies in the treatment of multiple sclerosis Mult. Scler. 1 339–342 Occurrence Handle9345413
B. W. Oosten Particlevan M. Lai S. Hodgkinson F. Barkhof D. H. Miller I. F. Moseley A. J. Thompson P. Rudge A. McDougall J. G. McLeod H. J. Ader C. H. Polman (1997) ArticleTitleTreatment ofmultiple sclerosis with the monoclonal anti-CD4 antibody cM-T412: results of a randomized, double-blind, placebo-controlled, MR-monitored phase II trial Neurology 49 351–357 Occurrence Handle9270561
A. B. Gottlieb M. Lebwohl S. Shirin A. Sherr P. Gilleaudeau G. Singer G. Solodkina R. Grossman E. Gisoldi S. Phillips H. M. Neisler J. G. Krueger (2000) ArticleTitleAnti-CD4 monoclonal antibody treatment of moderate to severe psoriasis vulgaris: results of a pilot, multicenter, multiple-dose, placebo-controlled study J. Am. Acad. Dermatol. 43 595–604 Occurrence Handle10.1067/mjd.2000.107945 Occurrence Handle1:STN:280:DC%2BD3M%2FjtFWqtg%3D%3D Occurrence Handle11004613
P. Morel J. P. Revillard J. F. Nicolas J. Wijdenes H. Rizova J. Thivolet (1992) ArticleTitleAnti-CD4 monoclonal antibody therapy in severe psoriasis J. Autoimmun. 5 465–477 Occurrence Handle10.1016/0896-8411(92)90006-C Occurrence Handle1:STN:280:DyaK3s%2FjvFamtA%3D%3D Occurrence Handle1384529
V. Canva-Delcambre S. Jacquot E. Robinet M. Lemann C. Drouet M. Labalette J. P. Dessaint D. Bengoufa C. Rabian R. Modigliani J. Wijdenes J. P. Revillard J. F. Colombel (1996) ArticleTitleTreatment of severe Crohn's disease with anti-CD4 monoclonal antibody Aliment. Pharmacol. Ther. 10 721–727 Occurrence Handle10.1046/j.1365-2036.1996.59201000.x Occurrence Handle1:CAS:528:DyaK28XmslWqu7o%3D Occurrence Handle8899079
A. Stronkhorst S. Radema S. L. Yong H. Bijl I. J. Berge Particleten G. N. Tytgat S. J. Deventer Particlevan (1997) ArticleTitleCD4 antibody treatment in patients with active Crohn's disease: a phase 1 dose finding study Gut 40 320–327 Occurrence Handle1:CAS:528:DyaK2sXivVWru70%3D Occurrence Handle9135519
B. M. Meiser C. Reiter H. Reichenspurner P. Uberfuhr E. Kreuzer E. P. Rieber G. Riethmuller B. Reichart (1994) ArticleTitleChimeric monoclonal CD4 antibody—a novel immunosuppressant for clinical heart transplantation Transplantation 58 419–423 Occurrence Handle1:STN:280:DyaK2czltlCqsw%3D%3D Occurrence Handle7915442 Occurrence Handle10.1097/00007890-199408270-00005
G. Horneff T. Winkler J. R. Kalden F. Emmrich G. R. Burmester (1991) ArticleTitleHuman anti-mouse antibody response induced by anti-CD4 monoclonal antibody therapy in patients with rheumatoid arthritis Clin. Immunol. Immunopathol. 59 89–103 Occurrence Handle10.1016/0090-1229(91)90084-N Occurrence Handle1:STN:280:DyaK3M3gvVOmtw%3D%3D Occurrence Handle2019013
S. X. Qin M. Wise S. P. Cobbold L. Leong Y. C. Kong J. R. Parnes H. Waldmann (1990) ArticleTitleInduction of tolerance in peripheral T cells with monoclonal antibodies Eur. J. Immunol. 20 2737–2745 Occurrence Handle1:CAS:528:DyaK3MXht1Sju7s%3D Occurrence Handle1702726
S. X. Qin S. Cobbold R. Benjamin H. Waldmann (1989) ArticleTitleInduction of classical transplantation tolerance in the adult J. Exp. Med. 169 779–794 Occurrence Handle10.1084/jem.169.3.779 Occurrence Handle1:STN:280:DyaL1M7ns1yltg%3D%3D Occurrence Handle2647894
D. Winsor-Hines C. Merrill M. O'Mahony P. E. Rao S. P. Cobbold H. Waldmann D. J. Ringler P. D. Ponath (2004) ArticleTitleInduction of immunological tolerance/hyporesponsiveness in baboons with a nondepleting CD4 antibody J. Immunol. 173 4715–4723 Occurrence Handle1:CAS:528:DC%2BD2cXnslWmtbk%3D Occurrence Handle15383608
G. P. Coffey E. Stefanich S. Palmieri R. Eckert J. Padilla-Eagar P. J. Fielder S. Pippig (2004) ArticleTitle In vitro internalization, intracellular transport, and clearance of an anti-CD11a antibody (Raptiva) by human T-cells J. Pharmacol. Exp. Ther. 310 896–904 Occurrence Handle10.1124/jpet.104.067611 Occurrence Handle1:CAS:528:DC%2BD2cXnt1eqt7o%3D Occurrence Handle15190122
G. Levy (1994) ArticleTitlePharmacologic target-mediated drug disposition Clin. Pharmacol. Ther. 56 248–252 Occurrence Handle1:STN:280:DyaK2M%2FgvVGqsw%3D%3D Occurrence Handle7924119 Occurrence Handle10.1038/clpt.1994.134
D. E. Mager W. J. Jusko (2001) ArticleTitleGeneral pharmacokinetic model for drugs exhibiting target-mediated drug disposition J. Pharmacokinet. Pharmacodyn. 8 507–532
J. L. Steimer A. Mallet J. L. Golmard J. F. Boisvieux (1984) ArticleTitleAlternative approaches to estimation of population pharmacokinetic parameters: comparison with the nonlinear mixed-effect model Drug Metab. Rev. 15 265–292 Occurrence Handle1:STN:280:DyaL2c3mtFSisA%3D%3D Occurrence Handle6745083
D. D'Argenio and A. Schumitzky. ADAPT II user's guide: pharmacokinetic/pharmacodynamic system analysis software, Biomedical Simulations Resources, Los Angeles, 1997.
R. J. Bauer S. Guzy (2004) Monte Carlo Parametric Expectation Maximization (MC-PEM) method for analyzing population pharmacokinetic/pharmacodynamic (PK/PD) data D. Z. D'Argenio (Eds) Advanced Methods of Pharmacokinetic and Pharmacodynamic System Analysis, Vol.3 Kluwer Academic Publishers Boston 135–163
T. Wileman C. Harding P. Stahl (1985) ArticleTitleReceptor-mediated endocytosis Biochem. J. 232 1–14 Occurrence Handle1:CAS:528:DyaL28Xhs1Gksg%3D%3D Occurrence Handle2867759
B. Davies T. Morris (1993) ArticleTitlePhysiological parameters in laboratory animals and humans Pharm. Res. 10 1093–1095 Occurrence Handle10.1023/A:1018943613122 Occurrence Handle1:STN:280:DyaK3szptFaqsg%3D%3D Occurrence Handle8378254
J. Lu J. Gaudreault W. F. Novotny B. Lum R. Bruno (2004) ArticleTitleA population pharmacokinetic model for Bevacizumab Clin. Pharmacol. Ther. 75 91
K. A. Harris C. B. Washington G. Lieberman J. Lu R. Mass R. Bruno (2002) ArticleTitleA population pharmacokinetic (PK) model for trastuzumab (Herceptin) and implications for clinical dosing Proc. Am. Soc. Clin. Oncol. 21 488a
T. A. Waldmann W. Strober (1969) ArticleTitleMetabolism of immunoglobulins Prog. Allergy 13 1–110 Occurrence Handle1:CAS:528:DyaF1MXlt1WlurY%3D Occurrence Handle4186070
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ng, C.M., Stefanich, E., Anand, B.S. et al. Pharmacokinetics/Pharmacodynamics of Nondepleting Anti-CD4 Monoclonal Antibody (TRX1) in Healthy Human Volunteers. Pharm Res 23, 95–103 (2006). https://doi.org/10.1007/s11095-005-8814-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-005-8814-3