Abstract
With the aging population, the number of women who will undergo surgery for pelvic organ prolapse (POP) is increasing dramatically. Pelvic reconstructive surgeries for genital prolapse have been shown significant improvement in quality of life and prolapse-related symptoms. With improving the surgical techniques and introducing synthetic mesh, more women undergo repairs of POP recently. However, with the increasing use of mesh in pelvic reconstructive surgery, there has been an increase in the number of patients seeking care for mesh-related complications. There has been a recent surge in the literature regarding the use of vaginally placed mesh for pelvic floor disorders largely due to the widely publicized complications associated with its use. The aim of this study is to review the current literature on mesh complications in POP treatment, with specific emphasis on vaginally-placed mesh for POP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) is recognized as having a significant adverse effect on women’s health and quality of life. The lifetime risk for surgery for POP has been estimated to be around 11.1 % [1], and 30 % of these women will undergo at least reoperation for recurrent prolapse [2]. The need for POP surgery increases with age [3], and it has been conservatively estimated that the surgical workload related to POP will increase by 46 % over the next four decades as our population ages [4].
According to the 2010 Census population report, the US female population reached more than 157 million (50.8 %) which puts as many as 9,420,000 US women might be at risk of POP surgery (http://www.census.gov/2010census/). Pelvic reconstructive surgery for genital prolapse, with or without mesh, is accompanied by a significant improvement in quality of life and prolapse-related symptoms [5]. While the use of non-absorbable synthetic mesh reduces the risk of prolapse recurrence, mesh placement for this purpose is not without risk [5]. However, the ease of use of vaginal mesh kits combined with high anatomic success rates led to rapid adoption of these techniques in clinical practice. In the update to the mesh warning released by the United States Federal Drug Administration in 2010, “at least 100,000 POP repairs that used surgical mesh” were performed and “about 75,000 of these were transvaginal procedures” [6]. This statement suggested that at least 225,000 transvaginal mesh (TVM) procedures were done in a 3-year period (2008–2010 timeframe) [7••].
The FDA first formally warned physicians about the complications of the use of TVM for treatment of POP in 2008 [6, 7••]. In spite of this warning, the interest in mesh kits peaked between 2008 and 2010 [7••]. The complications reported to the MAUDE database following the initial warning ultimately led the FDA to issue an updated Public Health Notification in July 2011 and included a significantly stronger warning for transvaginal POP meshes [7••]. In May 2014, the FDA proposed to reclassify surgical mesh for transvaginal POP repair from class II devices to class III, thus requiring increased safety and efficacy data for mesh kits prior to FDA approval [8••]. This reclassification is based on the tentative determination that the previously used mechanism of approval is not sufficient to provide reasonable assurance of safety and effectiveness for this device. In addition, the FDA proposed to reclassify urogynecologic surgical mesh instrumentation (e.g., manual gastroenterology-urology surgical instrument and accessories or manual surgical instrument for general use) from class I to class II. The agency is reclassifying both the surgical mesh for transvaginal repair and the urogynecologic surgical mesh instrumentation on its own initiative based on new information [7••]. A fivefold increase in the number of adverse medical device reports associated with mesh for POP in the years after the initial warning also prompted the FDA to release a safety communication in 2011 [9]. The updated FDA warning stated that TVM was not routinely found to be more effective than native tissue repair and may expose patients to greater risk [6]. Although the FDA communication was written to promote understanding of the risks associated with TVM and encourage informed decision-making by patients and healthcare providers, it resulted in a great deal of confusion, controversy, and concern regarding the role of TVM [9].
Opinion pieces drafted by specialty societies in response to the FDA warning argued that mesh-related complications are in a large part technique-related and a large number of vaginal mesh POP procedures are being done safely with a complication rate of only 0.67 % [7••, 10•]. Nevertheless, they agreed that further study is needed to clarify these concerns and define the optimal role of transvaginally placed mesh. In this article, we will review the current literature on mesh complications in POP treatment, with specific emphasis on vaginally-placed mesh for POP.
Mesh Erosion
One of the more recognized complications related to vaginally placed mesh is mesh erosion. For purposes of this review, mesh erosion is considered to be mesh visualized through the vaginal epithelium. Although standardized terminology now exists to describe complications such as mesh erosion [11], the variability of the use of the term in the literature makes it difficult to identify exact exposure rates.
A review of vaginal mesh complications of POP surgery has shown a mean rate of mesh exposure to be as high as 13.1 % [12–14], compared to only 3 % following open abdominal sacrocolpopexy and 2.5 % following laparoscopic sacrocolpopexy, respectively [15–17]. In a systematic review by Abed et al. in 2008, 110 studies reporting adverse events of vaginal mesh applications revealed overall mesh erosion rate of 10.3 % [18]. Mesh erosion rates vary from 0 to 25 % in different studies [19, 20]. A Cochrane review by Maher et al. [5] suggested that the use of vaginal mesh was associated with 11.4 % rate of mesh erosion and 6.8 % rate of surgical reintervention. A non-significant increase in rates of vaginal mesh exposure and reoperation for vaginal mesh exposure after vaginal mesh surgery in comparison to laparoscopic sacrocolpopexy has also been recognized (13 vs. 2 %, p = 0.07 and 9 vs. 2 %, p = 0.11, respectively) [21]. Symptoms associated with mesh erosion are not insignificant and include pelvic pain, infection, de novo dyspareunia (painful sex for patient or partner), de novo vaginal bleeding, atypical vaginal discharge, and the need for additional corrective surgeries [8••].
A number of risk factors for mesh erosion have been identified. Patient factors such as smoking status and vaginal atrophy can affect both the tissue integrity and surgical site healing, making exposure in these individuals more likely [22, 23]. Kaufman et al. found an association between vaginal mesh erosion and young age, as well as with sexual activity, but it is not clear if age is independently related to exposure or if younger people are simply more likely to be sexually active; alternatively, sexual activity may be a risk factor because exposure is more often recognized in women who are sexually active [24]. Similarly, some studies have recognized older age as a risk factor for exposure, but it is unclear if this association is due strictly to age or to the more advanced vaginal atrophy often seen in older women, especially since a number of studies have not found a difference in erosion rates between younger and older women [24–27].
It was recognized early on in the adoption of vaginal meshes that factors related to the mesh itself were capable of increasing the risk of mesh exposure. The majority of studies in the literature evaluate the effect of mesh type on sling erosion; however, it is reasonable to extrapolate the effects to their use in prolapse mesh kits. These factors are primarily related to pore size and mesh materials. Polypropylene meshes with large pore size (type IV meshes) are associated with a lower exposure rate than many of their predecessors that were designed to be tightly woven or nonporous [22, 28, 29].
Another risk factor for mesh exposure that is now recognized is the depth of the vaginal dissection prior to mesh placement [23]. With traditional colporrhaphies, surgeons were taught to make the dissection of the vaginal epithelium from the underlying fibromuscular tissues very thin in an effort to preserve as much “strong” tissue as possible for the repair. For vaginal mesh placement, the surgical technique must be altered. In this situation, the dissection must be deep to allow the fibromuscular tissue to overly the mesh, thus providing an “extra layer” of protection against exposure. Additionally, larger vaginal incisions are associated with increased risk of vaginal mesh exposure; in fact, many exposures occur along the previous suture line [30••, 31]. Finally, hysterectomy performed concomitantly with mesh-augmented prolapse repair is associated with higher exposure rates. Theories proposed for this include the large cuff incision as well as potential devascularization of the vaginal epithelium [22, 31].
As evidenced by the recognized risk factors for mesh exposure, prevention of exposure is often possible and is the optimal “management” strategy for these (and other) complications. Preventative measures include avoiding the above-mentioned risk factors wherever possible, such as the use of lighter-weight polypropylene materials with larger pore sizes, use of transverse vaginal incisions for vaginal dissection rather than vertical or t-shaped vaginal incisions, avoidance of folding of the mesh, appropriate thickness of dissection, and deferring mesh placement to a time remote from hysterectomy. Optimizing a patient’s tissue integrity through the preoperative use of vaginal estrogens has not been adequately studied as of yet, but may be an important preventive measure, as is smoking cessation preoperatively. Unfortunately, however, even impeccable patient selection and preparation and surgical technique is unlikely to prevent all mesh exposures. For patients presenting after mesh placement with mesh exposure, a number of treatments have been attempted, with varying efficacy.
It is important to acknowledge that not all mesh exposures need intervention. For this reason, the most conservative treatment option is simply observation. However, when a patient has bothersome vaginal bleeding, discharge, or pain due to the exposure, treatment is warranted [32••, 33•, 34••]. Vaginal estrogen creams have been used with marginal success. For small exposures (<0.5 cm) in atrophic women, it is reasonable to give a trial of estrogen cream prior to more invasive therapies [34••]. The patient should be counseled that the many women do not improve with vaginal estrogen use alone and that in over 60 % of exposures, procedural intervention is required [32••, 34••].
Surgical revision and removal of mesh can be challenging. Described techniques include excision of the exposed portion of the mesh with creation of an advancement flap to provide tension-free wound closure after appropriate mesh-free margins are obtained, revision of the vaginal epithelium with primary closure over the mesh, and—more aggressively—near complete removal of the vaginal mesh [23, 32••, 35•]. It is typically not feasible to remove the entire mesh, primarily due to the course of the mesh arms through inaccessible areas, but many surgeons choose to remove as much vaginal mesh as is safe to remove in an effort to prevent future revisions of re-exposed mesh.
Pelvic Pain
Pelvic pain, including dyspareunia, is a widely acknowledged complication of mesh exposure. The incidence of mesh-related pelvic pain is as high as 30 % [36, 37]. Pelvic pain may be groin pain related to the passage of the mesh arms through muscle tissue. Meshes designed to be anchored in the sacrospinous ligament can lead to pudendal and sciatic neuropathies; meshes passing through the obturator space can cause obturator neuropathies [34••, 38]. In our practice, we have seen many patients with pain originating after a mesh procedure develop pelvic floor myalgias, which in turn cause pelvic pain and dyspareunia. A focally painful segment of hardened mesh due to shrinkage of the vaginal mesh implant may lead to primary vaginal pain syndromes and dyspareunia following vaginal mesh use [39]. A recent case series reported high incidence of pain along contracted mesh sites. Severe vaginal pain and focal tenderness are reported which can be reproduced by palpation of the mesh segment [40].
The main clinical features include groin pain, suprapubic pain, dyspareunia, vaginal tightness, severe vaginal pain with movement, and vaginal shortening on vaginal examination [34••]. Over-tensioning of the mesh arms during implantation, collagen deposition and contraction within the mesh pores are reported to be responsible for mesh hardening and nerve fiber entrapment [39]. This complication needs to be more robustly characterized and addressed in all studies reporting outcomes with synthetic TVM augmented prolapse repairs. However, it is difficult to characterize this as the symptoms are often similar to other mesh-related complications or are compounded by chronic pain syndromes or myalgias.
The pain syndromes related to mesh, like other pain syndromes, can be debilitating and have a profound adverse psychosocial effect in patients who suffer from it. Thus, treatment of pain related to mesh is typically multimodal and should be promptly recognized and instituted [23, 36]. Muscle relaxants and analgesics may improve pain in some individuals and are frequently first-line therapies [36]. Physical therapy has been shown to improve some myalgias, as well as some neuropathies, and should be attempted prior to more aggressive intervention [36, 41]. In some situations, the mesh is clearly tight and tender, and the pain can be clinically reproduced by palpation of a tight band of mesh on vaginal examination. In these patients, surgical removal of the mesh may be preferred since the removal often has rates of improvement in pelvic pain and dyspareunia exceeding 70 % [18, 23, 36]. Dyspareunia related to mesh exposure should typically be treated with surgical revision [36].
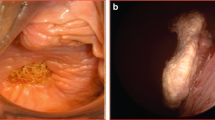
Mesh Extrusion and Perforation
Mesh perforation is defined by the ICS/IUGA Joint Terminology Report as the presence of mesh in a hollow organ or viscus [11]. Extrusion of mesh refers to the passage of the material out of a body or tissue structure [11]. Due to the location of vaginally placed meshes, the most common organs where these complications are identified are the bladder and bowel. Unilateral hydroureteronephrosis and rectovaginal fistula and abscess with rectal expulsion of posterior Prolift have been reported weeks after a mesh procedure [42, 43]. Mesh has been identified in the bladder and urethra when evaluating patients for hematuria and recurrent urinary tract infections, and in the bowel during evaluation for dyschezia and blood in the stool [23, 35•]. Clinical sequelae include pelvic pain, dyspareunia, fistula formation, recurrent urinary tract infections, bladder stones around the foreign body, hematochezia, dyschezia, and the need for additional corrective surgeries (possibly including suprapubic catheter or diverting colostomy) [8••].
The risk factors are not as well studied for mesh extrusion and perforation, but likely involve unrecognized perforation of the viscous with trocars during mesh placement. Careful surgical technique and understanding of pelvic anatomy are critical to preventing this type of complication. Rectal examinations and cystourethroscopy can identify bowel and bladder/urethral injuries intraoperatively, at which time the mesh can be removed and any injury repaired.
Mesh removal remote from placement can be complicated and should involve the appropriate surgeon. The removal of mesh from the rectum may necessitate a colostomy as part of the procedure; for this reason, colorectal surgeons often participate in the mesh removal. Bladder and urethral injuries can involve extensive or difficult dissections into the bladder base, trigone, and urethra and require expertise in repairing these structures, as well as prolonged bladder drainage, often through a suprapubic catheter [23, 35•]. A technique for mesh in the urethra was described by O’Sullivan et al., where otolagaryngological instruments were successfully used to remove mesh from the urethra without the need of a urethrotomy [44]. Further innovations and descriptions of such novel techniques are needed to help improve care of women with these challenging complications.
Infectious Complications
The available evidence suggests infections after prolapse repair using mesh occurs rarely [45]. The incidence of infection may depend on the type of mesh used, underlying comorbidity (e.g., immunosuppression status), the presence of other mesh complication (erosion and extrusion), multifilament or monofilament meshes (multifilament meshes with pore size <10 mm were at higher risk of infection than monofilament mesh with pore size >75 mm) [45]. Mesh-related infections include urinary tract infections (reported rates of 3.5–31 %), vaginal infections (0–18.4 %), wound infections (3–6 %), mesh infections (1 %), and pelvic infections and abscess (1–2 %) [46].
Clinical features include non-specific pelvic pain, persistent vaginal discharge or bleeding, dyspareunia, and urinary or fecal incontinence. Serious complications such as ischiorectal abscess, vesicovaginal fistula, rectovaginal fistula, pelvic abscess in the retropubic space, pararectal abscess, sigmoid bowel-vaginal fistula, enterocutaneous or enteroperineal fistulas can present in severe cases [47].
Treatments of mesh-related infections involve treating the underlying cause. There is some evidence that infection resulting from the mesh itself can be limited by soaking the mesh in an antibiotic solution prior to insertion or with copious irrigation of the surgical site after insertion [23]. Diabetes control must be optimized prior to surgery, and mesh should be avoided where possible in immunosuppressed patients. Infections related to mesh exposure or perforation should be treated with the appropriate antibiotics and the mesh surgically removed.
Conclusions
While treatment of mesh complications can be difficult, the current literature indicates that in most cases treatment is successful. Partial mesh revision/removal for mesh exposure leads to the need for future procedures for mesh exposure in many patients, but when the maximum amount of mesh safely possible to remove is excised, virtually all symptoms of mesh exposure will be resolved [32••, 33•]. Similarly, viscous injuries can successfully be repaired, but there is no data on long-term bladder and bowel function in patients suffering from these injuries. Pelvic pain has high improvement rates, particularly when the pain is reproduced on palpation of the mesh material during examination, but may require prolonged interventions after mesh removal such as physical therapy to achieve resolution [36].
Vaginally placed mesh for POP is associated with a number of complications, ranging from mild to severe in nature. As the literature suggests, the FDA warnings regarding mesh use are not unwarranted. It is important to recognize, as stated in the American Urogynecologic Society’s position statement regarding mesh use, that a complete ban of all POP mesh products should not be employed [10•]. Vaginal mesh does offer durable, effective repair of POP. In some patients, this surgical procedure is the optimal choice for their disorder. Although clearly not without risks, mesh complications can be prevented or successfully treated in many circumstances. Proper patient selection, appropriate surgeon training, and early recognition of complications should minimize these complications and allow for future use in selected individuals.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Olsen AL et al. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6.
Whiteside JL et al. Risk factors for prolapse recurrence after vaginal repair. Am J Obstet Gynecol. 2004;191(5):1533–8.
Smith FJ et al. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–100.
Margulies RU et al. Complications requiring reoperation following vaginal mesh kit procedures for prolapse. Am J Obstet Gynecol. 2008;199(6):678 e1-4.
Maher C et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;30(4), CD004014.
Update on Serious Complications Associated with Transvaginal Placement of Surgical Mesh for Pelvic Organ Prolapse. FDA Saf Commun. 2011.
Miles Murphy, et al. Time to rethink: an evidence-based response from pelvic surgeons to the FDA Safety Communication: “UPDATE on Serious Complications Associated with Transvaginal Placement of Surgical Mesh for Pelvic Organ Prolapse”. Int Urogynecol J. 2012;23:5–9. Highly important paper regarding surgeons’ evidence based perspective on FDA update.
Reclassification of Surgical Mesh for Transvaginal Pelvic Organ Prolapse Repair and Surgical Instrumentation for Urogynecologic Surgical Mesh Procedures; Designation of Special Controls for Urogynecologic Surgical Mesh Instrumentation. Department of Health and Human Services Food and Drug Administration, Thursday, May 1, 2014;79(84):24634–42. Most updated announcement on mesh complications by FDA, Highly important.
Firoozi F, Goldman H. Transvaginal excision of mesh erosion involving the bladder after mesh placement using a prolapse kit: a novel technique. Urology. 2010;75(1):203–6.
American Urogynecologic Society. Position Statement on Restriction of Surgical Options for Pelvic Floor Disorders. 2013. Surgical aspect limitation on POP treatment, Important.
Halylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, Deprest J, Dwyer PL, Fatton B, Kocjancic E, Lee J, Maher C, Rizk DE, Petri E, Sand PK, Schaer GN, Webb R. An International Urogynecological Association (IUGA)/International Continence Society (ICS) Joint Terminology and Classification of the Complications Related Directly to the Insertion of Prostheses (Meshes, Implants, Tapes) & Grafts in Female Pelvic Floor Surgery. 2010.
Altman D et al. Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med. 2011;364(19):1826–36.
Withagen MI et al. Trocar-guided mesh compared with conventional vaginal repair in recurrent prolapse: a randomized controlled trial. Obstet Gynecol. 2011;117(2 Pt 1):242–50.
Vollebregt A et al. Primary surgical repair of anterior vaginal prolapse: a randomised trial comparing anatomical and functional outcome between anterior colporrhaphy and trocar-guided transobturator anterior mesh. BJOG: Int J Obstet Gynaecol. 2011;118(12):1518–27.
Sergent F et al. Transvaginal mesh repair of pelvic organ prolapse by the transobturator-infracoccygeal hammock technique: long-term anatomical and functional outcomes. Neurourol Urodyn. 2011;30(3):384–9.
Maher CM et al. Surgical management of pelvic organ prolapse in women: the updated summary version Cochrane review. Int Urogynecol J. 2011;22(11):1445–57.
Feiner B, Gietelink L, Maher C. Anterior vaginal mesh sacrospinous hysteropexy and posterior fascial plication for anterior compartment dominated uterovaginal prolapse. Int Urogynecol J. 2010;21(2):203–8.
Abed H et al. Incidence and management of graft erosion, wound granulation, and dyspareunia following vaginal prolapse repair with graft materials: a systematic review. Int Urogynecol J. 2011;22(7):789–98.
Rardin CR, Washington BB. New considerations in the use of vaginal mesh for prolapse repair. J Minim Invasive Gynecol. 2009;16:360–4.
Brubaker L, Glazener C, Jacquentin B, Maher C, Melgrem A, Norton P, et al. Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence. 4th International Consultation on Incontinence. Paris, France. Surgery for pelvic Organ Prolapse, Jul 5–9. 2008;1273–320.
Freeman RM et al. A randomised controlled trial of abdominal versus laparoscopic sacrocolpopexy for the treatment of post-hysterectomy vaginal vault prolapse: LAS study. Int Urogynecol J S C Med Assoc. 2011;24(3):377–84.
Cundiff GW et al. Risk factors for mesh/suture erosion following sacral colpopexy. Am J Obstet Gynecol. 2008;199(6):688.e1-5.
Shah HN, Badlani GH. Mesh complications in female pelvic floor reconstructive surgery and their management: a systematic review. Indian J Urol: IJU: J Urol Soc India. 2012;28(2):129–53.
Kaufman Y et al. Age and sexual activity are risk factors for mesh exposure following transvaginal mesh repair. Int Urogynecol J. 2011;22(3):307–13.
Gabriel B et al. Prolapse surgery in women of 80 years and older using the Prolift technique. Int Urogynecol J. 2010;21(12):1463–70.
Ghezzi F et al. Surgical treatment for pelvic floor disorders in women 75 years or older: a single-center experience. Menopause (New York, NY). 2011;18(3):314–8.
Tan YL et al. Comparison of outcomes after vaginal reconstruction surgery between elderly and younger women. Taiwan J Obstet Gynecol. 2014;53(3):348–54.
Lee JK, Agnew G, Dwyer PL. Mesh-related chronic infections in silicone-coated polyester suburethral slings. Int Urogynecol J. 2011;22(1):29–35.
Yamada BS et al. High rate of vaginal erosions associated with the mentor ObTape. J Urol. 2006;176(2):651–4. discussion 654.
Mettu JR, Colaco M, Badlani GH. Evidence-based outcomes for mesh-based surgery for pelvic organ prolapse. Curr Opin Urol. 2014;24(4):370–4. Mesh surgery outcome based on recent evidence, Highly important.
Ganj FA et al. Complications of transvaginal monofilament polypropylene mesh in pelvic organ prolapse repair. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(8):919–25.
Skoczylas LC et al. Managing mesh exposure following vaginal prolapse repair: a decision analysis comparing conservative versus surgical treatment. Int Urogynecol J. 2013;24(1):119–25. Mesh complication management, Highly important.
Cornu JN, Peyrat L, Haab F. Update in management of vaginal mesh erosion. Curr Urol Rep. 2013;14(5):471–5. Mesh complication management update, Important.
Davila G, Jijon A. Managing vaginal mesh exposure/erosions. Curr Opin Obstet Gynecol. 2012;24(5):343–8. Comprehensive mesh complications review, Highly important.
Lee D, Bacsu C, Zimmern PE. Meshology: a fast-growing field involving mesh and/or tape removal procedures and their outcomes. Expert Rev Med Devices. 2014:1–16. Medical device complication, important.
Gyang AN et al. Managing chronic pelvic pain following reconstructive pelvic surgery with transvaginal mesh. Int Urogynecol J. 2014;25(3):313–8.
Sentilhes L et al. Sexual function in women before and after transvaginal mesh repair for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(6):763–72.
Karabulut A, Demitas O, Gok S. A late complication of transobturator tape procedure: Vaginocutaneous fistula formation with vaginal mesh erosion. Int Urogynecol J. 2014;25(4):559–61.
Feiner B, Maher C. Vaginal mesh contraction: definition, clinical presentation, and management. Obstet Gynecol. 2010;115((2 Pt 1)):325–30.
Fatton B et al. Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift technique)—a case series multicentric study. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(7):743–52.
Giamberardino MA et al. Myofascial pain syndromes and their evaluation. Best practice & research. Clin Rheumatol. 2011;25(2):185–98.
Karateke A, Cam C, Ayaz R. Unilateral hydroureteronephrosis after a mesh procedure. J Minim Invasive Gynecol. 2010;17(2):232–4.
Huffaker RK, Shull BL, Thomas JS. A serious complication following placement of posterior Prolift. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(11):1383–5.
O'Sullivan OE et al. Novel endoscopic management of a late complication following TVT insertion for stress urinary incontinence. Am J Case Rep. 2013;14:459–61.
Handa VL et al. Perioperative complications of surgery for genital prolapse: does concomitant antiincontinence surgery increase complications? Urology. 2005;65:483–7.
Falagas ME et al. Mesh-related infections after pelvic organ prolapse repair surgery. Eur J Obstet Gynecol Reprod Biol. 2007;134(2):147–56.
Weidner AC et al. Sacral osteomyelitis: an unusual complication of abdominal sacral colpopexy. Obstet Gynecol. 1997;90:689–91.
Compliance with Ethics Guidelines
Conflict of Interest
Pouya Javadian and Dena O’Leary declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Pelvic Organ Prolapse
Rights and permissions
About this article
Cite this article
Javadian, P., O’Leary, D. Vaginally Placed Meshes: A Review of Their Complications, Risk Factors, and Management. Curr Obstet Gynecol Rep 4, 96–101 (2015). https://doi.org/10.1007/s13669-015-0118-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-015-0118-y