Abstract
Introduction and hypothesis
Treatment of genital prolapse in very elderly women is challenging. Although pessary therapy and colpocleisis are effective, they also have drawbacks. There is only scarce literature about surgical therapy in this age cohort, particularly regarding the use of meshes.
Methods
We aimed to evaluate the feasibility, intraoperative complications, and short-term follow-up results of the Prolift™ technique in 62 women aged over 80 years. Mean follow-up time was 6.2 months.
Results
Prolift™ implantation was well tolerated by patients with regard to surgery and anesthesia, and hospitalization was relatively short (mean, 3.9 days). Intraoperative complications occurred in 1.6%. Early postoperative complications included increased post-void residual volume (25.8%), urinary tract infection (3.2%), and moderate or severe pain (17.7%). Five patients (8.3%) developed prolapse recurrence, and mesh retraction was observed in six patients (10%). There was no mesh erosion at short-term follow-up.
Conclusions
Treatment of advanced prolapse using Prolift™ in very elderly women is a feasible, safe, and effective surgical option, preserving a functional vagina. Thus, this may represent one alternative to colpocleisis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Treatment of pelvic organ prolapse (POP) in women over 80 years of age remains a challenge. According to the World Population Ageing Report of the United Nations, the proportion of those aged 80 years or over will increase almost fourfold over the next 50 years, to reach 4.1% in 2050. By that time, this age group is projected to number almost 379 million worldwide, about 5.5 times as many as in 2000 [1]. Because the life expectancy in these women is greater than their male counterparts, the proportion of women in the older population grows even faster with advancing age [1]. POP is very prevalent in this age cohort and significantly contributes to a decrease in quality of life [2, 3]. Surgical therapy may be hampered by the increased anesthesiological risk due to the frequently present co-morbidities in very elderly patients. Therefore, the use of pessaries can be an effective alternative to surgery. A vaginal pessary can be properly fitted in 74% of women, approximately 50% of whom will continue to use it 1 year later [4, 5]. However, local infection and problems with pessary handling can represent serious shortcomings of this conservative therapy [6].
Traditional surgical techniques include different variations of colpocleisis, which is an effective treatment option [7, 8]. Nevertheless, colpocleisis leads to complete closure of the vaginal channel and, subsequently, eliminates the ability for patients to have vaginal intercourse. Paradoxically, complete closure of the vagina is both the main goal and a potential disadvantage of colpocleisis [9, 10]. In the past few years, there has been a notable decrease in the popularity of colpocleisis with increasing emphasis on the special needs of elderly patients in regards to quality of life, sustained sexual activity, and intercourse. Thus, there is currently more emphasis placed on these issues, and surgical alternatives to colpocleisis are being discussed.
To our knowledge, there are no published data to date that focus on the use of prosthetic material for the surgical treatment of POP in a special cohort of very elderly women. Recently, there has been concern relative to the use of meshes in pelvic floor reconstructive surgery, but reports in this field are rarely objective [11]. The use of meshes in the anterior compartment has been shown to significantly increase the success rates, compared with traditional surgery techniques, with comparable and acceptable complication rates [12, 13].
Meshes could also be of use for women over 80 years of age. First, poor quality and often atrophied pelvic floor tissues restrict the applicability of traditional repair techniques. Secondly, early recurrence or primary failure requiring a secondary intervention should be avoided at all costs in these patients because of the increased anesthesia risk.
Therefore, we aimed to evaluate the feasibility, perioperative and immediate postoperative complications, and short-term follow-up results of total mesh repair using the Prolift™ technique as one alternative for the treatment of advanced symptomatic POP in very elderly patients.
Materials and methods
Patients
Sixty-two patients over the age of 80 years diagnosed with a clinically significant and symptomatic POP between March 2004 and March 2009 were eligible for this retrospective case series. The indication for surgery was a complaint of severe POP with no desire for a pessary or a history of problems with pessaries. All patients underwent staging of POP according to a simplified version of the International Continence Society (ICS) POP-Q staging system [14], which is more applicable to daily clinical practice and based on the ordinal stages of the POP-Q, as described by Swift et al. [15]. A stage II or greater POP was defined as clinically significant.
All pelvic floor reconstructive surgeries were performed in the Department of Gynecological Surgery, Centre Hospitalier Régional Universitaire de Lille, France. The Institutional Review Board approved the investigative protocol (Cos03/2009). All patients had a complete preoperative evaluation including history, physical examination, and urine culture. During preoperative consultation, we also evaluated for clinically evident urinary incontinence, as well as urinary incontinence which was revealed only after reduction of the prolapse. Urodynamic investigation was performed whenever symptoms suggested concomitant stress urinary incontinence (SUI).
Polypropylene mesh implant
The PROLIFT™ pelvic floor repair system (Ethicon Women’s Health and Urology, Somerville, NJ, USA) was used in all patients in this study and is supplied in the form of a mesh kit. The synthetic prosthesis is a pre-cut, nonabsorbable monofilament of polypropylene woven into interlock knitting, extensible in both directions, of low grammage (42.7 g/m2), high global porosity of 66%, with large pores (2.4 mm), and a tensile strength of 7.58 kg/m2. The mesh consists of three distinct parts: The anterior part is inserted between the bladder and the vagina and secured bilaterally by two arms through each obturator foramen. The posterior part is placed between the rectum and the vagina and is secured bilaterally by one arm passing through each ischiorectal fossa and sacrospinous ligament. The intermediate section corresponding to the vaginal apex separates the anterior and posterior parts and was cut if uterine preservation was intended. If the patient had a previous (or concomitant) hysterectomy, the implant was kept in one piece.
Surgical technique
The surgical technique has previously been described in detail [16, 17]. The surgery was performed under regional (epidural) or general anesthesia, while the patient was in a gynecological position with a Foley urinary catheter. In addition, a local tissue infiltration was always used. Preoperative antibiotic prophylaxis with a single shot of a second generation cephalosporine was systematically administered. Fourteen out of 62 patients (22.6%) had a previous hysterectomy, and in the remaining 48 patients with intact uterus, a concomitant vaginal hysterectomy was performed in three cases (6.3%). Of note, when the uterus was preserved, the anterior and posterior mesh was fixed to the uterine isthmus with a single stitch of Prolene suture, to provide efficient support to the uterus. In cases where there was associated SUI, a tension-free TVT-O™ suburethral sling was concomitantly placed.
Data collection
This is a single center case series with data collected retrospectively from the patients’ medical records. The following variables were noted for each patient: age, body mass index (weigh/height2), medical, surgical, gynecological, and obstetrical history, stage of POP and compartments involved, type of prosthesis, post-void residual volume (PVR), eventual urinary and digestive problems, time of surgery, concomitant procedures, and perioperative surgical complications. The degree of postoperative pain was systematically recorded by the nursing staff using a visual analogue scale between 0 and 10. A score below 4 was considered as corresponding to a slight pain level, a score between 4 and 7 to a moderate pain level, and a score above 7 to a severe pain level.
Patients were seen at least once again for a follow-up gynecologic examination 3 months postoperatively. A POP-Q stage of II or greater was defined as POP recurrence.
Data management and statistics
The patients’ pre- and postoperative data were collected and entered into the SPSS V15.0 software package for Windows, which was used for descriptive and statistical analysis (SPSS, Chicago, IL, USA). Correlation between clinical variables and patient characteristics was performed using Pearson’s correlation coefficient and χ 2 tests for categorical variables. Between-group differences for continuous variables were tested with Mann–Whitney U test. A p < 0.05 was considered statistically significant.
Results
Study population
Sixty-two women over 80 years of age, presenting with severe and symptomatic POP between March 2004 and March 2009, underwent pelvic floor reconstructive surgery using prosthetic material. Preoperative patient characteristics are presented in Table 1. Notably, all patients had at least one co-morbidity or chronic illness in our cohort. The most common complaint was the presence of a genital bulge (90%). Approximately 75% of all patients had two or more complaints. A PVR of more than 100 mL with or without voiding dysfunction due to severe POP was preoperatively observed in 22 (35.5%) patients. At least four women (6.5%) had complete urinary retention in their medical history; one patient had acute renal failure, and two had acute pyelonephritis. Eight patients (12.9%) had to manually reduce their POP in order to allow micturation. Three women (4.8%) had vaginal infections, and seven (11.3%) suffered from vaginal or uterine ulcerations due to severe POP or pessary therapy.
Intraoperative characteristics
The mean operative time was 74.4 ± 27.3 (range, 39–204) min. General anesthesia was used in 48 patients (77.4%). We did not perform any associated anterior or posterior fascial repair or myorrhaphy. An intraoperative complication was observed in only one patient (1.6%), who had blood loss (>500 mL) not requiring blood transfusion, but an exceptionally long operative time (204 min) due to a thorough hemostasis. Importantly, complications directly related to the implantation technique, such as bladder or rectal perforation, were not observed.
Early postoperative course
The mean hospital stay was 3.9 ± 0.26 (range, 1–14) days. During the early postoperative (in patient) period, 25 patients (40.3%) developed minor complications (Table 2). In seven of 11 patients, moderate or severe postoperative pain resolved during the duration of the hospital stay. This was in all cases a gluteal pain, two patients complained in addition about thigh pain, and one patient also about pelvic pain. However, four patients (6.5%) had persistent moderate perineal or gluteal pain for a period of 3 to 6 weeks. Of note, moderate and severe postoperative pain was more often observed in patients who were not subjectively cured from urinary incontinence, compared with those who were cured or were significantly improved (33% vs. 7.1%, p = 0.047).
Importantly, major complications requiring the patient to be transferred to the Intensive Care Unit, or the need for surgical revision due to problems with the implanted Prolift™, were not observed during the early postoperative period.
Follow-up
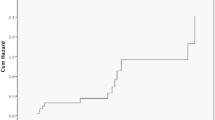
The mean follow-up time was 6.2 ± 1.1 (range, 1.5–36) months. Sixty patients (97%) were available for a follow-up gynecologic examination; and two women had died in the interim, one of them 12 months after surgery due to a colon cancer and the other patient 30 months after surgery due to cardiac disease. Follow-up data are presented in Table 3. Five patients presented with painless mild (n = 4) and moderate (n = 1) mesh retractions, whereas one patient (1.7%) with a mild retraction had moderate and persistent spontaneous perineal pain over a period of several weeks postoperatively. Two of these retractions were observed in the anterior compartment and another two in the posterior one. One patient developed mesh retractions in both compartments, and in another case, the retraction was found at the level of the vaginal cuff after hysterectomy.
There were two (3.3%) reoperations. One patient required reoperation after 2.5 months due to worsening of SUI after total failure of the concomitantly placed suburethral sling. This patient underwent another TVT-O™ sling implantation and was satisfied with the results of the surgery at a 6 months follow-up visit. Another patient had symptomatic POP recurrence 8 months after primary surgery. Subsequently, a laparoscopic sacrocolpopexy was performed, and the short-term (2 months) follow-up examination revealed excellent anatomic results.
Correlations between clinical variables
POP recurrence was associated with the presence of mesh retraction (p = 0.02), postoperative UTI (p < 0.001), and voiding difficulty (p = 0.001).
There was less postoperative PVR > 100 mL and voiding difficulty in patients who had regional compared with general anesthesia (8% and 0% vs. 33% and 18%, respectively), but this was not statistically significant (p = 0.097 and p = 0.105, respectively). Of note, 24 out of 29 concomitant TVT-O™ procedures (86%) were performed under general anesthesia, which might explain the observed differences. Moreover, regional anesthesia was associated with a shorter hospital stay (2.9 vs. 4.2 days, p = 0.012). Postoperative voiding difficulty correlated with early UTI (p < 0.001) and with the length of hospital stay (5.5 days with vs. 3.6 days without voiding difficulty, p = 0.013).
As expected, concomitant surgery was associated with less de novo SUI (0% vs. 23%, p = 0.045), but more de novo urge incontinence (8.6% vs. 0%, p = 0.051), presumably due to the TVT-O™ procedures as the most important part of concomitant surgeries. In line with these findings, concomitant surgery was also associated with a higher number of women being subjectively cured or significantly improved from their urinary incontinence after surgery (86% vs. 37.5%, p = 0.004).
Discussion
The ideal surgical procedure in elderly women with symptomatic POP would allow for an efficient repair and rapid postoperative recovery, and conform to the sexual activity desires of the patient. Amazingly, there is a paucity of data relative to the most optimal therapeutic options for women over 80 years of age, presenting with severe POP [8, 18, 19]. We therefore report on a special cohort of patients over the age of 80, who underwent POP surgery using the Prolift™ technique. More than 95% of women had a preoperative stage III or IV symptomatic POP. We were able to show that this technique is feasible and safe, with an intraoperative complication rate of 1.6%. Specifically, we did not observe any bladder or rectal lesion. However, our sample size was too small, considering that the risk for injury in a younger population accounts for approximately 0.7% (bladder) and 0.15% (rectum) [20].
Minor postoperative complications were observed in 25 patients (40%). This is in line with other published findings, observing that most frequent complications are Dindo classification types 1 to 3 after mesh implantation (13). The most frequently observed complication was a PVR > 100 mL in 26% of patients, but only half (13%) had voiding difficulty during the hospital stay, and none required urinary catheterization at discharge. This is less than in a comparable cohort of 128 patients aged 80 years and older, undergoing conservative POP surgery, in which the authors described a 43% rate of voiding difficulty, and 18% of patients were discharged with a catheter [19]. In addition, our urinary retention rate was lower compared with a study by Alperin et al. [21] who reported 34% of catheterizations at discharge after Prolift™ implantation, although midurethral slings were placed in only 18% of patients. Our rate was in accordance with the data of Fatton et al. [17] who reported an 11.8% urinary retention rate after Prolift™ implantation. The second most common complication in our cohort was moderate-to-severe postoperative pain in approximately 18% of patients. Although this appears to be high, pelvic, buttock, or thigh pain is in fact not uncommon shortly after transgluteal needle passage [21]; only four patients (6.5%) in our cohort complained of persistent moderate perineal or gluteal pain for a period of 3 to 6 weeks. The other seven patients experienced relatively quick resolution of pain. Interestingly, moderate and severe postoperative pain was observed more often in patients who were not cured from urinary incontinence. This finding may have clinical relevance in that patients should be queried about urinary incontinence if there is no other explanation for their pain. Moreover, elderly women may be embarrassed to address this problem directly.
We observed two cases of anal incontinence in the early postoperative course: One patient had preexisting constipation and developed postoperative mild anal incontinence due to a fecaloma, which had resolved by the time of follow-up examination. Another woman who presented with rectal prolapse and preoperative anal incontinence to liquid stool underwent concomitant rectal suspension at the time of surgery; however, this patient did not have postoperative improvement.
One patient who complained about dyspnea postoperatively was diagnosed with a gastric ulcer and treated successfully, but required a longer hospital stay of 14 days overall. The mean hospital stay of 3.9 days in our study was comparable with other studies that reported on younger patient cohorts [17, 22]. The shorter hospital stay of patients after regional anesthesia (2.9 vs. 4.2 days after general anesthesia) could be due to a quicker postoperative mobilization, but might also represent a selection bias. In contrast to this numbers, Schweitzer et al. [19], studying a comparable population of women over 80 years of age treated by traditional surgery techniques, described a median hospital stay of 10 days and a higher complication rate including blood transfusions in 18%. Carey and Leach [23] compared symptomatic anterior wall prolapse repair outcomes in 31 patients 80 years or older to those in 234 younger patients with a 21-month follow-up and showed no difference between the two groups. Another randomized controlled trial demonstrated similar perioperative complication rates and outcomes in women 70 years or older undergoing abdominal sacrocolpopexy compared with those in a younger age group [24].
We avoided concomitant “preventative” hysterectomy in cases of absent uterine pathology because of the increased risk of complications, particularly mesh erosion [20, 25]; hence, our hysterectomy rate was only 6.3%. There was no difference with regard to peri- and postoperative morbidity when comparing the group with uterus preservation to the group of patients with previous hysterectomy. Importantly, there were no erosions seen in our patient cohort at the follow-up examination. Comparison with other studies reveals erosion rates of 4.6% to 11.3% with an average of 7% [13, 17, 20]. Consequently, we should have observed at least two to four mesh erosions from a statistical point of view. However, this could be due to the small number of patients (n = 62) in our cohort group and the short follow-up time. Conversely, if elderly patients are significantly more prone to the risk of mesh erosion, this should have been detected in our cohort of 62 patients.
Our mesh retraction rate at 10% (n = 6) is in accordance with other studies showing retraction rates ranging from 4% to 17% [17, 20]. These six cases were detected at 2-, 3-, 19-, 28-, and 36-month (n = 2) follow-up periods. At first glance, it appears that the longer the follow-up time, the greater the chance of diagnosing a mesh retraction. Nevertheless, those retractions detected at 19, 28, and 36 months of follow-up might have occurred a long time before they were detected in fact, and according to our clinical experience, this is even more probable. However, when a follow-up time of only 3 months is considered, four out of six mesh retractions (67%) would be missed. From a clinical point of view, most retractions (five out of six) were asymptomatic, and only one patient with a slight mesh retraction suffered from moderate pain over several weeks in our study. Tunn et al. [26] reported on retractions of up to 50% of the original mesh length at 6 weeks postoperatively on ultrasonography. Therefore, the actual “dark figure” might be higher. We must also consider critically that there was no standardized classification system for mesh complications at that time, and therefore, we were not able to codify our clinical findings accordingly.
In our study, five patients (8%) succumbed to early POP recurrence, bringing our anatomical success rate to 92%. Importantly, three of these recurrences were in women operated in the first year (between March and November 2004), which points to the surgeon’s learning curve. Our success rate is in accordance with previous studies, ranging between 87% and 95% [13, 17, 20]. The five recurrences were detected at 2, 5, 9, 19, and 36 months of follow-up. Again, if only a 3-month postoperative period is considered, four out of five recurrences would be missed. Therefore, a postoperative follow-up period of at least 3 to 6 months is fully justified. Only one patient in our cohort had a symptomatic recurrent stage III POP and was subsequently reoperated. Another patient with a stage III recurrence was not bothered by her symptoms. The remaining three patients were quasi “downstaged” from stage IV to stage II POP, and all were asymptomatic. This raises the question of what can be defined as success in prolapse surgery [27]. As others have done, we chose the “satisfactory anatomic outcome” (POP stage 0 or I) of the NIH Standardization Workshop as the definition of success. However, data suggest that almost 40% of women presenting for annual gynecologic exams without symptoms of POP would not meet these criteria and that symptom-based definitions better reflect patient’s assessment of treatment success and overall improvement [27]. The clinical relevance of stage II recurrent POP that is asymptomatic is still unclear. If a high proportion progress over time and require reoperation, and if this is not true for stage I recurrent POP, this would indeed have a greater clinical relevance.
Interestingly, we were able to detect a significant correlation between mesh retraction and POP recurrence, and this is in accordance with previous observations [20]. Perhaps, it is the prosthetic retraction that favors relapse because it creates non-reinforced zones [26]. The contribution of inflammatory processes remains to be elucidated, and interestingly, the presence of postoperative voiding difficulty and UTI were also significantly associated with POP recurrence.
In our study, we noted a high rate of preoperative SUI, which was cured in 80% of patients by concomitant suburethral sling implantation, and this was not associated with an increased rate of urinary retention compared with other studies. Conversely, de novo SUI occurred in 10% with no case in the group of patients with a concomitant TVT-O™ implantation. The overall de novo urge rate was 5% (8.6% in patients with a concomitant TVT-O™ implantation), which is in accordance with the literature [17, 20, 28]. The rate of de novo urinary incontinence after colpocleisis is estimated to be even higher [29] and more difficult to treat by suburethral slings due to introital narrowing.
The limitations of our study include the non-randomized nature, retrospective design, relatively small sample size, and short-term follow-up; however, we felt it was important to report these results in view of the very scarce data on the use of meshes in patients over 80 years of age. In fact, older women have been excluded from many of the trials that have examined the outcomes of pelvic floor surgery [30].
In summary, women over 80 years of age undergoing POP reconstructive surgery using the Prolift™ technique do not seem to be predisposed to more mesh-specific complications compared with younger patients, as might be expected due to vaginal atrophy and advanced age. Moreover, the complication rate was not higher compared with traditional surgical techniques.
The operative morbidity and mortality seems to be more influenced by the patients’ co-morbidities than by age itself. Therefore, we believe that age alone should not be an exclusion criterion for any surgical procedure in elderly patients. Prolift™ implantation can represent one reasonable alternative when discussing surgical treatment options in very elderly patients with advanced POP. Further studies are warranted to prospectively evaluate this technique in comparison with traditional surgeries in this age group.
References
Demographic profile of the older population. In: World Population Ageing Report 1950–2050. Population Division, DESA, United Nations. http://www.un.org/esa/population/
Luber KM, Boero S, Choe JY (2001) The demographics of pelvic floor disorders: current observations and future projections. Am J Obstet Gynecol 184:1496–1503
Barber MD, Kuchibhatla MN, Pieper CF, Bump RC (2001) Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol 185:1388–1395
Wu V, Farrell S, Baskett TF, Flowerdew G (1997) A simplified protocol for pessary management. Obstet Gynecol 90:990–994
Sulak PJ, Kuehl TJ, Shull BL (1993) Vaginal pessaries and their use in pelvic relaxation. J Reprod Med 38:919–923
Arias BE, Ridgeway B, Barber MD (2008) Complications of neglected vaginal pessaries: case presentation and literature review. Int Urogynecol J 19:1173–1178
DeLancey JO, Morley GW (1997) Total colpocleisis for vaginal eversion. Am J Obstet Gynecol 176:1228
van Huisseling JCM (2009) A modification of Labhardt’s high perineoplasty for treatment of pelvic organ prolapse in the very old. Int Urogynecol J 20:185–191
Carberry CL, Hampton BS, Aguilar VC (2007) Pyometra necessitating hysterectomy after colpocleisis in an extremely elderly patient. Int Urogynecol J 18:1109–1111
Roth TM (2007) Pyometra and recurrent prolapse after Le Fort colpocleisis. Int Urogynecol J 18:687–688
Jacquetin B, Cosson M (2009) Complications of vaginal mesh: our experience. Int Urogynecol J 20:893–896
Jia X, Glazener C, Mowatt G, MacLennan G et al (2008) Efficacy and safety of using mesh or grafts in surgery for anterior and/or posterior vaginal wall prolapse: systematic review and meta-analysis. BJOG 115:1350–1361
Feiner B, Jelovsek JE, Maher C (2009) Efficacy and safety of transvaginal mesh kits in the treatment of prolapse of the vaginal apex: a systematic review. BJOG 116:15–24
Bump RC, Mattiasson A, Bo K, Brubaker LP et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Swift S, Morris S, McKinnie V, Freeman R et al (2006) Validation of a simplified technique for using the POPQ pelvic organ prolapse classification system. Int Urogynecol J 17:615–620
Debodinance P, Berrocal J, Clavé H, Cosson M et al (2004) Changing attitudes on the surgical treatment of urogenital prolapse: birth of the tension-free vaginal mesh. J Gynécol Obstét Biol Reprod 33:577–588
Fatton B, Amblard J, Debodinance P, Cosson M et al (2007) Transvaginal repair of genital prolapse:preliminary results of a new tension-free vaginal mesh (Prolift™ technique)—a case series multicentric study. Int Urogynecol J 18:743–752
Nieminen K, Heinonen PK (2001) Sacrospinous ligament fixation for massive genital prolapse in women aged over 80 years. BJOG 108:817–821
Schweitzer KJ, Vierhout ME, Milani AL (2005) Surgery for pelvic organ prolapse in women of 80 years of age and older. Acta Obstet Gynecol Scand 84:286–289
Caquant F, Collinet P, Debodinance P, Berrocal J et al (2008) Safety of trans vaginal mesh procedure: retrospective study of 684 patients. J Obstet Gynaecol Res 34:449–456
Alperin M, Sutkin G, Ellison ML et al (2008) Perioperative outcomes of the Prolift™ pelvic floor repair systems following introduction to a urogynecology teaching service. Int Urogynecol J 19:1617–1622
Milani A, Withagen M, Vierhout ME (2009) Trocar-guided total tension-free vaginal mesh repair of post-hysterectomy vaginal vault prolapse. Int Urogynecol J 20:1203–1211
Carey JM, Leach GE (2003) Transvaginal surgery in the octogenarian using cadaveric fascia for pelvic prolapse and stress incontinence: minimal one-year results compared to younger patients. Urology 63:665
Richter HE, Goode PS, Kenton K, Brown MB et al (2007) The effect of age on short-term outcomes after abdominal surgery for pelvic organ prolapse. J Am Geriatr Soc 55:857
Belot F, Collinet P, Debodinance P, Ha Duc E et al (2005) Risk factors for prosthesis exposure in treatment of genital prolapse via the vaginal approach. Gynécol Obstét Fertil 33:970–974
Tunn R, Picot A, Marschke J, Gauruder-Burmester A (2007) Sonomorphological evaluation of polypropylene mesh implants after vaginal mesh repair in women with cystocele or rectocele. Ultrasound Obstet Gynecol 29:449–452
Barber MD, Brubaker L, Nygaard I, Wheller T et al (2009) Defining success after surgery for pelvic organ prolapse. Obstet Gynecol 114:600–609
Sung VW, Schleinitz MD, Rardin CR, Ward RM et al (2007) Comparison of retropubic vs transobturator approach to midurethral slings: a systematic review and meta-analysis. Am J Obstet Gynecol 197:3–11
FitzGerald MP, Brubaker L (2003) Colpocleisis and urinary incontinence. Am J Obstet Gynecol 189:1241–1244
Morse AN, Labin LC, Young SB, Aronson MP et al (2004) Exclusion of elderly women from published randomized trials of stress incontinence surgery. Obstet Gynecol 104:498–503
Conflicts of interest
BG was awarded an International Fellowship grant by the International Urogynecological Association (IUGA) in 2009, which partly funded this research project. BG also received a grant for basic research from the Ministry of Health of the Czech Republic (No. 9299-3/2007). The authors announce an unconditional financial support of basic research by ETHICON Women’s Health & Urology.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Gabriel, B., Rubod, C., Córdova, L.G. et al. Prolapse surgery in women of 80 years and older using the Prolift™ technique. Int Urogynecol J 21, 1463–1470 (2010). https://doi.org/10.1007/s00192-010-1217-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-010-1217-y