Abstract
A 32-year-old female with Crohn's disease experienced a rectovaginal fistula and abscess with rectal expulsion of posterior Prolift. She underwent diagnostic laparoscopy, transanal incision and drainage of abscess, transanal excision of mesh, and laparotomy with loop ileostomy. Weeks later, she underwent colectomy, near-total proctectomy, end ileostomy, and fistula repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Case
A 32-year-old para 2 white female with a 21-year history of Crohn's disease presented to the emergency department with worsening abdominal pain, nausea, vomiting, and diarrhea. She was diagnosed with a rectovaginal fistula 8 months prior and was being treated with biologic therapy including infliximab for Crohn's disease and fistula during the months prior to this admission. She was admitted and placed on ciprofloxacin and metronidazole.
At the time of this admission, her white blood cell count was within normal limits. Her abdominal exam was benign. Computed tomography (CT) scan showed only mild thickening of the bowel wall in the rectosigmoid without distention. Enteric contrast and air were seen in the vagina, suggesting persistent rectovaginal fistula.
Rectal examination was notable for an anterior rectal mucosa defect proximal to the anal sphincter. Flexible sigmoidoscopy revealed an area of dark, granular, and necrotic-appearing tissue. Chronic ulcerations and mucosal granularity suggested inflammation. With rectal insufflation, air and blood oozed from the vagina.
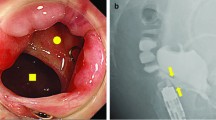
Digital rectal examination under anesthesia revealed an anterior 1.5-cm firm region with an obvious depression correlating with endoscopy. Anoscopy revealed a 1- to 2-cm area of black, possibly necrotic tissue with a piece of mesh having two long tails well entrenched into and through the rectovaginal septum. No obvious vaginal communication was noted. Purulent and feculent fluid was noted in the vagina.
Due to difficulty in extracting the mesh transanally and concern for possible adherence to intraperitoneal structures, a diagnostic laparoscopy was performed. No mesh or abnormality was seen intraperitoneally. Urogynecology was consulted. The mesh appeared consistent with a posterior Prolift mesh. Intraoperatively, the office of the gynecologist who performed the mesh repair was contacted. It was confirmed that she had undergone a laparoscopic supracervical hysterectomy and placement of Prolift mesh in the posterior compartment 2 years earlier. The extruded mesh was sharply dissected free in its entirety (Figs. 1 and 2). There was no evidence of intraperitoneal or obvious retroperitoneal bleeding. The defect in the rectal mucosa was left open due to obvious infection. Anal sphincter musculature was dilated but intact. The abscess around the mesh tract had been drained. The wound was packed. Postoperatively, the patient's hemoglobin dropped to 7.1 g/dl. She received 2 U of packed red blood cells with appropriate increase in hemoglobin.
Postoperatively, it was hoped that the combination of mesh extraction and medical treatment (including infliximab) would allow healing or at least improvement in the Crohn's severity. Six days later, due to intolerable fistula output and perineal pain, the patient underwent a diverting loop ileostomy by mini-laparotomy. Ciprofloxacin and metronidazole were continued. She was discharged 8 days later. Antibiotics and oral pain medications were continued. Vaginal drainage persisted. Nine days after discharge, her postoperative exam was remarkable for persistent rectal mucosa defect, persistent rectovaginal fistula, and ileostomy.
Eleven days later, she was diagnosed with a 6.5 × 6.5 × 10-cm presacral abscess. She was admitted and placed on piperacillin sodium/tazobactam, antiemetics, and pain medications. Interventional radiology drained only 8 mL of old blood. The culture was ultimately negative. Follow-up CT scan showed a smaller presacral fluid collection. She was discharged 2 days later with prescriptions for amoxicillin/clavulanate, an antiemetic and analgesic.
A week later, colonoscopy revealed severe colitis in addition to the rectovaginal fistula. A central line was inserted and total parenteral nutrition was started. Eight days later, she underwent total abdominal colectomy with near-complete proctectomy, end ileostomy, and rectovaginal fistula repair. Pathology report was consistent with Crohn's disease. She was discharged on postoperative day 10. Other than difficulty with pain management, she did well prior to discharge. She continues to experience significant psychosocial difficulties 3 months later.
Discussion
Treatment of pelvic organ prolapse with transvaginally introduced synthetic mesh is controversial. Reported complications include mesh exposure, pain, and rectal erosion [1, 2]. The recent United States of America Food and Drug Administration warning regarding transvaginal placement of surgical mesh provides information on reported adverse events. Guidelines on vaginal graft use have been published by the Society of Gynecologic Surgeons.
This patient's 21-year history of inflammatory bowel disease prior to the placement of the vaginal mesh was complicated by multiple factors. First, ulcerative colitis was initially diagnosed, and she was successfully managed on medical therapy for many years. Subsequently, with the appearance of the rectovaginal fistula, Crohn's disease was suspected and therapy was changed. The patient also lost insurance, which limited her access to care for a period of time.
Crohn's disease is known to affect the anorectum in as many as 60–80% of patients with the diagnosis, and this can manifest itself as ulceration, fistula, abscess, stricture, or carcinoma [3]. Part of an effective management plan for perianal disease, including fistula, involves examination under anesthesia and drainage of any septic foci and stabilization of the infectious component and medical management. Infliximab therapy can promote fistula closure in 55% of patients compared with 13% closure in the placebo group [4]. Combination medical and surgical treatment is also being used with reports of examination under anesthesia and subsequent infliximab therapy accelerating healing, with infliximab treatment followed by definitive surgery showing an additive effect in the treatment regimen for fistulas arising in those with active proctitis [5]. Despite these promising results, women with complicated anovaginal or rectovaginal fistula in the presence of severe proctitis may still require proctectomy for definitive management.
The decision to use a synthetic mesh kit in a 30-year-old woman with a history of inflammatory bowel disease may have been better approached with caution and with the consultation of a multidisciplinary team including gastroenterology, colon and rectal surgery, and urogyneclogy in order to optimize outcomes. Her subsequent morbidity and prolonged recovery period were likely exacerbated by the use of the mesh kit. If a posterior compartment repair was needed, native tissue would have been a less risky option.
References
Dwyer PL, O'Reilly BA (2004) Transvaginal repair of anterior and posterior compartment prolapse with Atrium polypropylene mesh. BJOG 111(8):831–836
Hurtado EA, Appell RA (2008) Management of complications arising from transvaginal mesh kit procedures: a tertiary referral center's experience. Int Urogynecol J Pelvic Floor Dysfunct. doi:10.1007/s00192-008-0721-9
Singh B, McMortensen NJ, Jewell DP, George B (2004) Perianal Crohn's disease. Br J Surg 91:801–814
Present DH, Rutgeerts P, Targan S et al (1999) Infliximab for the treatment of fistulas in patients with Crohn's disease. N Engl J Med 340(18):1398–1405
van der Hagen SJ, Baeten CG, Soeters PB et al (2005) Anti-TNF-alpha (infliximab) used as induction treatment in case of active proctitis in a multistep strategy followed by definitive surgery of complex anal fistulas in Crohn's disease: a preliminary report. Dis Colon Rectum 48:758–767
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huffaker, R.K., Shull, B.L. & Thomas, J.S. A serious complication following placement of posterior Prolift. Int Urogynecol J 20, 1383–1385 (2009). https://doi.org/10.1007/s00192-009-0873-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-0873-2