Abstract
The treatment role of Total Mesorectal Excision (TME) in proximal rectal cancers (PRC) is still debated. Partial Mesorectal Excision (PME) can reduce morbidity in PRC patients. The purpose of this study was to compare short-term clinical and long-term oncological outcomes between the two groups. A total of 157 PRC patients were enrolled in this study (114 performed with PME and 43 with TME). The two groups were compared in terms of perioperative and long-term oncological outcomes. The overall postoperative complications rate was higher in TME group (18.4% vs. 32.5%, p < 0.05). The incidence of diverting ileostomy was also significantly higher in TME group (86.0% vs. 2.6%, p < 0.001). Overall survival rates for 3, 5, and 7 years in PME and TME group accordingly were: 94.6%, 89.3%, 81.5% and 93.2%, 87.6%, 78.4% (p = 0.324). Disease-free survival rates for 3, 5, and 7 years in PME and TME group were: 90.2%, 84.5%, 78.6% and 88.7%, 81.2%, 75.3% (p = 0.297), respectively. Local recurrence rates for 3, 5, and 7 years in PME and TME group were: 2.6%, 6.1%, 8.8% and 4.6%, 9.3%, 11.2% (p = 0.061), respectively. PME is feasible and can be safely performed in PRC patients with favorable oncological outcomes. TME is associated with increasing risk of surgical complications and requires a two-step surgery for stoma takedown.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Total mesorectal excision (TME) has emerged as the gold standard surgical technique for oncologically driven rectal resections in patients with rectal cancer [1]. The development of new surgical techniques, along with the implementation of neoadjuvant chemoradiotherapy (NCRT) protocols, has significantly reduced both local and distant metastasis rates, improving sphincter preservation as well as functional outcomes [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17]. Nevertheless, some studies suggested that proximal rectal cancers (PRC) exhibit distinct oncological behaviors compared to low rectal cancers, raising the question of the necessity of TME for PRC in certain circumstances [18,19,20]. Interestingly, some studies have revealed that, contrary to mid-low rectal cancers, the omission of NCRT does not significantly alter survival rates in patients with PRC [21,22,23,24,25].
Debates persist regarding the necessity of TME for tumors located in the proximal rectum. A recently published meta-analysis revealed that partial mesorectal excision (PME) and TME for PRC are associated with similar circumferential margin (CRM) positivity, local recurrence rates, and urinary function [26]. Interestingly, patients in the PME group showed lower rates of anastomotic leaks and better anorectal functional outcomes compared to the TME group [26]. Consequently, a tumor-specific rectal resection, also known as PME, has been developed as a variation of TME, aiming for a more conservative yet radical resection. However, there is still a paucity of literature on PME for PRC, especially concerning long-term oncological outcomes.
This study aims to compare the postoperative and long-term oncological outcomes between TME and PME for PRC.
Methods
Study population
This retrospective study evaluated a consecutive series of patients with PRC undergoing TME or PME performed by a single surgeon between January 2005 and December 2019. Data were extracted from a prospectively maintained surgical database. Informed consent was obtained from each patient.
The primary aim was to report the short-term outcomes, and the secondary aim was to compare the long-term oncological outcomes between the two groups.
Inclusion criteria were (Fig. 1): (1) rectal adenocarcinoma; (2) proximal location (10–15 cm from the anal verge, AV); (3) clinical TNM stage I-III; (4) no evidence of synchronous tumors and distant metastases; (5) sphincter-saving TME or PME; (6) elective surgery; (7) patients with a follow-up period > 36 months.
Exclusion criteria were: (1) mid-low RC (10 cm from the AV); (2) left colon or sigmoid colon resections; (3) local excision of the rectum; (4) abdominoperineal resections (APR) or Hartmann’s resection; (5) metastatic disease; (6) palliative surgery; (7) patients with a follow-up period of less than 36 months.
The AV was defined as the junction between the perineal skin and anal mucosa. Distance between caudal edge of the tumor and AV was assessed via digital rectal examination, flexible sigmoidoscopy, and rectal magnetic resonance imaging (MRI).
Preoperative protocol
Preoperative staging included chest X-ray, carcinoembryonic antigen (CEA) levels, total colonic examination with flexible or virtual colonoscopy, thoraco-abdominal computed tomography (CT), pelvic-phased array MRI.
NCRT protocols were as follows: (1) long-course neoadjuvant chemoradiotherapy, 50 Gy administered in 25 fractions over 5 weeks, with concomitant chemotherapy using capecitabine (1600 mg/m2 per day of radiotherapy). Surgery was performed 4–8 weeks after completion of neoadjuvant therapy; (2) short-course neoadjuvant radiotherapy, 25 Gy delivered in five fractions over 5–7 days. Surgery was performed in 1–4 weeks after completion of neoadjuvant therapy. Short-course radiotherapy was preferred in patients without any risk of lateral margin positivity.
All patients underwent oral mechanical bowel preparation without oral antibiotics. A single dose of intravenous ciprofloxacin (400 mg) was given 1 h before surgical incision.
Surgical technique
All surgeries were performed by a single surgeon (OA), with more than 20 years of experience in oncological colorectal surgery, at three centers: (1) Istanbul University Faculty of Medicine, Department of General Surgery, Istanbul, Turkey; (2) Liv Hospital, Department of General Surgery, Istanbul, Turkey; (3) Maslak Acibadem Hospital, Istanbul, Turkey. The surgical approach was discussed with each patient and decided according to surgeon’s indication, patient’s opinion, and surgical cost. All patients received extensive explanations of the advantages and disadvantages of each approach and techniques (PME, TME, open, laparoscopic, or robotic). TME was preferred mostly for advanced tumors with invasion of adjacent organs (cT4).
The surgical techniques performed (open, laparoscopic, robotic) were previously described by the authors [8, 14]. Robotic surgeries performed with the Da Vinci Si® or Xi® (Intuitive Surgical, Inc., Sunnyvale, CA, USA) platform was 6 and 4, respectively. Briefly, standard surgical technique included mobilization of the splenic flexure and the descending colon, division of the inferior mesenteric vein below the pancreas, high division of the mesenteric artery 1–2 cm from its origin, and systematic division of the left colic vessels. Rectal mobilization was accomplished under direct vision in the mesorectal plane. Mobilization was completed to allow a perpendicular division of the rectum 5 cm below the tumor, avoiding a cone effect. Then, the rectum was transected at the same level as the mesorectum. Direct colorectal anastomosis was performed with a double stapling technique in all patients. A diverting ileostomy was created in all patients with a NCRT or in case of surgeon’s discretion. The pelvis was routinely drained with a suction drain in the presacral space.
Conversion was defined as any unplanned laparotomy at any time during surgery, regardless of incision length.
Pathological report
Pathological staging was modified according to American Joint Committee on Cancer (AJCC) 8th edition staging system during data review [27]. All pathology specimens were examined to determine tumor size, number of lymph nodes harvested, distal resection margin (DRM), circumferential resection margin (CRM), and mesorectum integrity. Quality of mesorectum was assessed according to Quirke et al. [28]. Positive CRM was defined as direct tumor extension within 1 mm of the radial, non-peritonealized surface of the resected specimen [29].
Postoperative outcomes and follow-up
Postoperative complications, defined as adverse events occurring within 30 days from surgery, were assessed through Clavien-Dindo’s classification [30]. Anastomotic leak diagnosis and treatment followed the International Study Group of Rectal Cancer [31]. Adjuvant chemotherapy (5-FU, capecitabine, and oxaliplatin) was given to patients with pathological stage III cancers. Long-term oncological outcomes were compared between PME and TME groups. Follow-up included control of oncological markers (CEA, carbohydrate antigen 19–9) every three months, evaluation with thoraco-abdominal CT annually, and colonoscopy on the first, third, fifth, and tenth year from surgery.
Overall survival (OS) was measured from date of surgery to that of death/last follow-up, disease-free survival (DFS) to that of tumor recurrence. Recurrence was diagnosed through radiological detection of enlarging lesions or by histological confirmation.
This study followed the STROBE statement for cohort studies [32].
Statistical analysis
Patient characteristics were summarized using basic descriptive statistics. Continuous variables were presented as median (interquartile range, IQR) or mean ± standard deviation accordingly, and compared using the Mann–Whitney U test. Categorical variables were expressed as proportions and analyzed using the Chi-squared or Fisher’s exact test. Statistical analysis was performed using the STATA software package version 9.0 (StataCorp, College Station, TX, USA). Survival and recurrence rates were estimated through the Kaplan–Meier model and compared by the log-rank test. P values < 0.05 were considered statistically significant.
Results
Clinical outcomes
A total of 157 consecutive cases of PRCs were included in the study and divided into two groups: PME (n = 114, 72.6%) and TME (n = 43, 27.4%) group (Fig. 1). Patients’ characteristics are listed in Table 1. The groups were comparable in demographics, body mass index (BMI), American Association of Anesthesiologists (ASA) score, clinical T and N stage, and clinical CRM status.
Mean age was 56.8 ± 4.6 and 57.1 ± 3.8 years (p = 0.711) for PME and TME group of patients, respectively. Mean tumor distance from AV for PME and TME were 12.5 ± 2.6 cm and 10.2 ± 3.3 cm (p = 0.083), respectively. Locally advanced tumor (stage III) rates were 45.6% and 55.8% (p = 0.064) in PME and TME group, respectively.
NCRT consisted of preoperative long course in 14.9% (n = 17) and 13.9% (n = 6) patients in the PME and TME group, respectively. Short-course radiotherapy was applied to 0.9% (n = 1) and 4.6% (n = 2) patients in the PME and TME group, respectively.
Perioperative outcomes
Perioperative outcomes are presented in Table 2. The incidence of minimally invasive approaches in PME group was higher than TME group (92.1 vs. 81.4%, p = 0.46). Diverting ileostomy creation was significantly different between groups (2.6 vs. 86.0%, p < 0.001). No conversion to open surgery was reported in either group. Median operation time was longer in the TME group, but with no statistical significance (106.8 ± 36.5 min vs. 85.6 ± 18.5 min, p = 0.082). Estimated blood loss was also higher in the TME group but with no statistical significance (135.5 ± 110.2 ml vs. 105.0 ± 90.5 ml, p = 0.106). There were no significant differences in terms of days to first flatus and postoperative stay.
Postoperative complications
Overall complication rate was significantly higher in the TME group (18.4 vs. 32.5%, p < 0.05) (Table 2). Complication’s grade was significantly different regarding Clavien–Dindo’s classification with a greater rate of class III-IV occurring in the TME group (11.6 vs. 6.1%, p < 0.05). A total of 8 (7.0%) patients in the PME group and 6 (14.0%) patients in the TME group suffered clinical anastomotic leak (AL) (p = 0.038). In both groups, the patients with AL received NCRT. The TME group of patients with AL had all a protective ileostomy, subsequently they were treated conservatively by maintaining pelvic drainage, until the existing infection was resolved clinically, and postponing the ileostomy closure time. Regarding the PME group, three out of eight patients with AL had an ileostomy and were treated as for the TME group with AL. From the remaining five patients three of them underwent a diverting colostomy which was closed after the complete healing of AL. The other two patients were treated conservatively by postponing the drain removal. There were no 30-days postoperative mortality in both groups.
Histopathological outcomes
Histopathological findings are listed in Table 3. Mean tumor size was 42 ± 11.7 mm in the PME group and 55 ± 14.2 mm in the TME group (p = 0.062).
ypTNM pathological stages for PME and TME group were I (n = 19, 16.7%/n = 4, 9.3%), II (n = 45, 39.5%/n = 12, 27.9%), and III (n = 50, 43.8%/n = 27, 62.8%). CRM involvement was present in six (5.3%) and two (4.6%) patients (p = 0.127), respectively in PME and TME group. DRM length for PME and TME group was 21 ± 1.5 mm and 29 ± 1.8 mm (p = 0.096), respectively. There were no statistically significant differences between PME and TME groups in terms of harvested lymph nodes (20.5 ± 3.1 vs. 23.4 ± 4.6, p = 0.142). Tumor differentiation status did not differ between groups.
Oncological outcomes
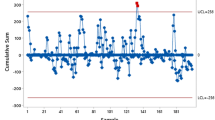
OS rates for 3,5, and 7 years in PME and TME group were: 94.6%, 89.3%, 81.5% and 93.2%, 87.6%, 78.4% (p = 0.324) (Fig. 3). DFS rates for 3,5, and 7 years in PME and TME group were: 90.2%, 84.5%, 78.6% and 88.7%, 81.2%, 75.3% (p = 0.297), respectively (Fig. 2, 3).
Local recurrence (LR) rates for 3, 5, and 7 years in PME and TME group were: 2.6%, 6.1%, 8.8% and 4.6%, 9.3%, 11.2% (p = 0.061), respectively. Distal site LR (intraluminal) for PME and TME group of patients were: 4 (3.5%) and 1 (2.3%), respectively. LR occurring in the remaining PME (n = 6, 5.3%) and TME (n = 4, 9.3%) patients were extraluminally, at the boundaries of the pelvic cavity.
Distant metastasis (DM) rates for 3, 5, and 7 years in PME and TME group were: 7.2%, 9.4%, 12.6% and 6.7%, 9.5%, 13.5% (p = 0.232), respectively. Site of DM in PME group of patients were liver (n = 7, 6.1%), lung (n = 2, 1.7%), bone (n = 2, 1.7%) and peritoneal surface (n = 3, 2.6%). DM site in TME group of patients: liver (n = 3, 7.0%), lung (n = 1, 2.3%), peritoneal surface (n = 1, 2.3%) and brain (n = 1, 2.3%).
Discussion
This study compared two different resection techniques (PME vs. TME) in patients with PRC with respect to postoperative and long-term oncological outcomes. In all cases sphincter-preserving procedures were successfully achieved. Although, the TME procedures presented prolonged surgical time (85.6 ± 18.5 min vs. 106.8 ± 36.5 min; p = 0.082) and increased estimated blood loss (105.0 ± 90.5 ml vs. 135.5 ± 110.2 ml; p = 0.106) compared with PME group, both not reached statistically significance.
The frequency of performed minimally invasive techniques in PME group (92.1%) was numerically higher than the TME group (81.4%). One reason might be that TME patients are presented with more advanced tumors and adjacent organ invasion, which could lead to challenges for minimally invasive surgery. In both groups, conversion rates were null. The rate of diverting ileostomy was significantly higher in TME group of patients (2.6% vs. 86.0%; p < 0.001). This fact makes TME a two-step surgery compared to PME.
Even though nearly half of the patients in PME (45.6%) and TME (55.8%) group presented with an advanced tumor stage, the NCRT frequency rates were low in both groups (15.8% vs. 18.5%). As described previously, administration of NCRT can downsize and downstage the tumor, block tumor dissemination, increase the tumor resection rate and anus preservation rate, and reduce the LR rate [2,3,4]. Recent advances in NCRT protocols allow to obtain high rates of cCR (complete clinical response) in patients with locally advanced rectal cancers [33, 34]. However, most studies regarding NCRT on management of rectal cancer focused on mid-low rectal tumors, and treatment modalities for PRC is still debated.
Anastomotic leakage was also significantly higher in the TME group (7.0 vs. 14.0%; p = 0.038). Significantly lower anastomotic leakage rates in the PME group were also revealed in a recently published meta-analysis (6.9% vs. 10.9%; p <0.001) [26].
The abovementioned results show that PME can be performed with acceptable morbidity compared to TME, further highlighting a perioperative benefit in performing a more conservative technique for patients with PRC without affecting the oncological outcomes. These results were confirmed by a more extensive prospective study conducted by Law et al. (n = 622 patients) which revealed significantly lower anastomotic leakage rates in the PME compared with TME group (1.3 vs. 8.1%; < 0.001). In the same study, TME and diverting stoma (73.5 vs. 8.1%) were found to be independent risk factors for anastomotic leak. Nevertheless, the authors included many rectosigmoid and distal rectal cancer cases in the study. Kanso et al. revealed a 7.6% rate of leakage in their study which only consisted of PME patients, however they included also mid rectal cancers [20]. In the present study, only tumors located 10-15 cm from the AV were included and analyzed. The significantly higher rate of postoperative complications according to Clavien–Dindo’s classification (I-IV) in the TME group (p < 0.05) emphasizes that this technique may be more challenging and cause more morbidity than PME.
Obtaining an adequate CRM and DRM are important pathological parameters which determine LR rate and survival after rectal cancer surgery [35, 36]. The CRM involvement rate (5.3 vs. 4.6%; p = 0.127) was lower in the TME group with no statistical difference. The DRM was also longer in TME (29 ± 1.8 vs. 21 ± 1.5 mm; p = 0.096). The TME group of patients presented with a larger tumor size (55 ± 14.2 vs. 42 ± 11.7 mm; p = 0.062) and more frequently at advanced tumor stage (stage III), 62.8 vs. 43.8%; p = 0.104) but with no statistical differences. The amount of harvested lymph node was also similar in both groups.
Regarding oncological outcomes, our study showed that PME and TME provided similar results with respect to long-term follow-up.
The present study showed that the liver was the most frequent organ metastasis site in both groups (6.1% vs. 7.0%). Pulmonary metastasis rates for PME and TME were 1.7% and 2.3%, respectively. These findings again prove that liver metastasis rates are higher in proximally located rectal tumors compared to distal ones.
The current study revealed that the TME group tended to develop more LR, however without statistical significance. LR at 3,5,7-years in PME and TME group were: 2.6%, 6.1%, 8.8% and 4.6%, 9.3%, 11.2% (p = 0.061), respectively.
The results of the present study are similar to those of previously reported studies. Kanso et al. also reported favorable oncologic outcomes (5-year LR 5.3%, DFS 79.7%, OS 93.2%) on 172 PRC patients who underwent PME [20]. Lopez-Kostner et al. compared outcomes of PRC (n = 229) with sigmoid colon (n = 225) and mid-low rectal cancers (n = 437). All PRCs and sigmoid colon cancers were treated with the same surgical technique (PME). The five-year LR rate of PRC was 4.7%, like sigmoid colon cancers (3.9%), whereas the mid-low rectal cancers were 12.9% [18]. A multicenter randomized controlled trial conducted by Kaser et al. reported that PRC (n = 142, DFS 68%, OS 79%) present similar oncological behavior with sigmoid colon tumors (n = 378, DFS 69%, OS 77%), significantly lower than the respective rates of mid-low rectal cancers (n = 205, DFS 54%, OS 64%). Interestingly, none of the patients received neoadjuvant or adjuvant radiotherapy or TME [37].
Contrary to these reports, several studies in the literature state that TME provides better oncological control when compared with PME in patients with PRC. Bondeven et al. found reduced rates of 3-year LR in PRC patients following TME compared with PME (3.0% vs. 14%; p = 0.032) [23]. Syk et al. reported that despite the wide use of preoperative RT, a significantly high 9% rate of LR occurred in PRC patients treated with PME [38].
The strengths of this study are: (1) long median follow-up providing high quality oncological outcomes; (2) a standardized single surgeon setting with colorectal expertise (> 2000 colorectal oncological cases); (3) specific focus on PRC, which are poorly reported in the literature.
Limitations were: (1) retrospective nature possibly suffering from patient selection bias; (2) single surgeon setting, so the results may not be generalizable to all institutions; (3) relatively small series (especially for the TME group), therefore future large-scale studies are needed to confirm long-term outcomes; (4) absence of postoperative functional outcomes.
Conclusion
This study revealed that PME is associated with shorter operation time and reduced blood loss when compared to TME in patients with PRC. The PME group exhibited significantly lower postoperative complications, including a decreased incidence of anastomotic leakage. Pathological parameters such as CRM involvement, DRM, and harvested lymph nodes did not show significant differences between the two groups. Long-term oncological outcomes, including DFS, OS, and LR, were similar in both groups. Although a cost analysis was not conducted in the current study, it is evident that PME techniques are likely to be cost-effective due to the streamlined nature of the one-step surgery approach.
Data availability
The datasets used or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1:1479–1482
Author A (1993) Initial report from a Swedish multicentre study examining the role of preoperative irradiation in the treatment of patients with resectable rectal carcinoma. Swedish Rectal Cancer Trial. Br J Surg 80:1333–1336
Kapiteijn E, Kranenbarg EK, Steup WH, Taat CW, Rutten HJ, Wiggers T et al (1999) Total mesorectal excision (TME) with or without preoperative radiotherapy in the treatment of primary rectal cancer. Prospective randomised trial with standard operative and histopathological techniques Dutch ColoRectal Cancer Group. Eur J Surg 165:410–420
Sauer R, Becker H, Hohenberger W, Rodel C, Wittekind C, Fietkau R et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351:1731–1740
Aliyev V, Goksoy B, Goksel S, Guven K, Bakir B, Saglam S et al (2021) Intersphincteric Resection for Low Rectal Cancer: Parameters Affecting Functional Outcomes and Survival Rates. Surg Technol Int 39:166–172
Aliyev V, Piozzi GN, Bulut A, Guven K, Bakir B, Saglam S et al (2022) Robotic vs laparoscopic intersphincteric resection for low rectal cancer: a case matched study reporting a median of 7-year long-term oncological and functional outcomes. Updates Surg 74(6):1851–1860
Aliyev V, Goksel S, Bakir B, Guven K, Asoglu O (2021) Sphincter-Saving Robotic Total Mesorectal Excision Provides Better Mesorectal Specimen and Good Oncological Local Control Compared with Laparoscopic Total Mesorectal Excision in Male Patients with Mid-Low Rectal Cancer. Surg Technol Int 38:160–166
Asoglu O, Tokmak H, Bakir B, Aliyev V, Saglam S, Iscan Y et al (2020) Robotic versus laparoscopic sphincter-saving total mesorectal excision for mid or low rectal cancer in male patients after neoadjuvant chemoradiation therapy: comparison of long-term outcomes. J Robot Surg 14:393–399
Piozzi GN, Baek SJ, Kwak JM, kim J, Kim SH. (2021) Anus-Preserving Surgery in Advanced Low-Lying Rectal Cancer: A Perspective on Oncological Safety of Intersphincteric Resection. Cancers 13:4793
Piozzi GN, Lee TH, Kwak JM, Kim J, Kim SH (2021) Robotic-assisted resection for beyond TME rectal cancer: a novel classification and analysis from a specialized center. Updates Surg 73:1103–1114
Milone M, Manigrasso M, Velotti N, Torino S, Vozza A, Sarnelli G, Aprea G, Maione F, Gennarelli N, Musella M, De Palma GD (2019) Completeness of total mesorectum excision of laparoscopic versus robotic surgery: a review with a meta-analysis. Int J Colorectal Dis 34(6):983–991. https://doi.org/10.1007/s00384-019-03307-0
Milone M, Manigrasso M, Burati M, Velotti N, Milone F, De Palma GD (2018) Surgical resection for rectal cancer. Is laparoscopic surgery as successful as open approach? A systematic review with meta-analysis. PLoS ONE 13(10):e0204887. https://doi.org/10.1371/journal.pone.0204887
Schietroma M, Romano L, Apostol AI, Vada S, Necozione S, Carlei F, Giuliani A (2022) Mid- and low-rectal cancer: laparoscopic vs open treatment-short- and long-term results. Meta-analysis of randomized controlled trials. Int J Colorectal Dis 37(1):71–99. https://doi.org/10.1007/s00384-021-04048-9
Shadmanov N, Aliyev V, Piozzi GN, Bakır B, Goksel S, Asoglu O (2024) Perioperative and long-term oncological outcomes of robotic versus laparoscopic total mesorectal excision: a retrospective study of 672 patients. J Robot Surg 18(1):144. https://doi.org/10.1007/s11701-024-01922-w
Gachabayov M, Lee H, Kajmolli A, Felsenreich DM, Bergamaschi R (2024) Impact of robotic total mesorectal excision upon pathology metrics in overweight males with low rectal cancer: a pooled analysis of 836 cases. Updates Surg. 76(2):505–512. https://doi.org/10.1007/s13304-023-01733-y
Aliyev V, Piozzi GN, Shadmanov N, Guven K, Bakır B, Goksel S, Asoglu O (2023) Robotic and laparoscopic sphincter-saving resections have similar peri-operative, oncological and functional outcomes in female patients with rectal cancer. Updates Surg 75(8):2201–2209. https://doi.org/10.1007/s13304-023-01686-2
Aliyev V, Piozzi GN, Huseynov E, Mustafayev TZ, Kayku V, Goksel S, Asoglu O (2023) Robotic male and laparoscopic female sphincter-preserving total mesorectal excision of mid-low rectal cancer share similar specimen quality, complication rates and long-term oncological outcomes. J Robot Surg 17(4):1637–1644. https://doi.org/10.1007/s11701-023-01558-2
Lopez-Kostner F, Lavery IC, Hool GR, Rybicki LA, Fazio VW (1998) Total mesorectal excision is not necessary for cancers of the upper rectum. Surgery 124:612–618
Law WL, Chu KW (2004) Anterior resection for rectal cancer with mesorectal excision: a prospective evaluation of 622 patients. Ann Surg 240:260–268
Kanso F, Lefevre JH, Svrcek M, Chafai N, Parc Y, Tiret E (2016) Partial mesorectal excision for rectal adenocarcinoma: morbidity and oncological outcome. Clin Colorectal Cancer 15(1):82–90
Marinello FG, Frasson M, Baguena G, Flor-Lorente B, Cervantes A, Rosello S et al (2015) Selective approach for upper rectal cancer treatment: total mesorectal excision and preoperative chemoradiation are seldom necessary. Dis Colon Rectum 58:556–565
Park JS, Sakai Y, Simon NSM, Law WL, Kim HR, Oh JH et al (2016) Long-Term Survival and Local Relapse Following Surgery Without Radiotherapy for Locally Advanced Upper Rectal Cancer: An International MultiInstitutional Study. Medicine (Baltimore) 95:e2990
Bondeven P, Laurberg S, Hagemann-Madsen RH, Ginnerup PB (2015) Suboptimal surgery and omission of neoadjuvant therapy for upper rectal cancer is associated with a high risk of local recurrence. Colorectal Dis 17:216–224
Rosenberg R, Maak M, Schuster T, Becker K, Friess H, Gertler R (2010) Does a rectal cancer of the upper third behave more like a colon or a rectal cancer? Dis Colon Rectum 53:761–770
Wang Y, Wang X, Chen J, Huang S, Huang Y (2024) Comparative analysis of preoperative chemoradiotherapy and upfront surgery in the treatment of upper-half rectal cancer: oncological benefits, surgical outcomes, and cost implications. Updates Surg 76(3):949–962. https://doi.org/10.1007/s13304-023-01744-9
Carbone F, Petz W, Borin S, Bertani E, de Pascale S, Zampino MG, Fumagalli RU (2023) Tumour-specific mesorectal excision for rectal cancer: Systematic review and meta-analysis of oncological and functional outcomes. Eur J Surg Oncol 49(11):107069. https://doi.org/10.1016/j.ejso.2023.107069
Weiser MR (2018) AJCC 8th Edition: Colorectal Cancer. Ann Surg Oncol 25:1454–1455
Quirke P, Dixon MF (1998) The prediction of local recurrence in rectal adenocarcinoma by histopathological examination. Int J Colorectal Dis 3:127–131
Nagtegaal ID, Marijnen CA, Kranenbarg EK et al (2002) Cooperative Clinical Investigators Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: not one millimeter but two millimeters is the limit. J Surg Pathol 26(3):350–357
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A et al (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147:339–351
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP et al (2008) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61:344–349
Asoglu O, Bulut A, Aliyev V, Piozzi GN, Guven K, Bakır B, Goksel S (2022) Chemoradiation and consolidation chemotherapy for rectal cancer provides a high rate of organ preservation with a very good long-term oncological outcome: a single-center cohort series. World J Surg Oncol 20(1):358. https://doi.org/10.1186/s12957-022-02816-7
Asoglu O, Goksoy B, Aliyev V, Mustafayev TZ, Atalar B, Bakir B, Guven K, Demir G, Goksel S (2022) Watch and Wait Strategy for Rectal Cancer: How Long Should We Wait for a Clinical Complete Response? Surg Technol Int 40:130–139. https://doi.org/10.52198/22.STI.40.CR1507
Nagtegaal ID, Van de Velde CJ, van der Worp E et al (2002) Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 20:1729–1734
Kelly SB, Mills SJ, Bradburn DM et al (2011) Effect of the circumferential resection margin on survival following rectal cancer surgery. Br J Surg 98:573–581
Kaser SA, Froelicher J, Li Q, Muller S, Metzger U, Castiglione M et al (2015) Adenocarcinomas of the upper third of the rectum and the rectosigmoid junction seem to have similar prognosis as colon cancers even without radiotherapy, SAKK 40/87. Langenbeck’s Arch Surg 400(6):675–682
Syk E, Torkzad MR, Blomqvist L, Nilsson PJ, Glimelius B (2008) Local recurrence in rectal cancer: anatomic localization and effect on radiation target. Int J Radiat Oncol Biol Phys 72(3):658–664. https://doi.org/10.1016/j.ijrobp.2008.01.063
Acknowledgements
This study has been presented on 3rd International Congress on Innovative Approaches in Medical and Health Sciences (2023/Istanbul, Turkey) as a oral presentation.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: OA and VA; methodology: OA, VA, NS and GNP; formal analysis and investigation: OA, VA, NS and GNP; writing—original draft preparation: VA, NS and GNP; writing—review and editing: OA, NS, GNP, VA, BB, and SG; and supervision: OA. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Ethical approval
Institutional Review Board (IRB) approval was waived following the retrospective nature of the study.
Informed consent
Informed consent was obtained from each patient.
Research involving human participants and/or animals
This study was conducted in compliance with the Principles of the Declaration of Helsinki. The identity information of the patients was anonymized during the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aliyev, V., Shadmanov, N., Piozzi, G.N. et al. Comparing total mesorectal excision with partial mesorectal excision for proximal rectal cancer: evaluating postoperative and long-term oncological outcomes. Updates Surg 76, 1279–1287 (2024). https://doi.org/10.1007/s13304-024-01926-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-024-01926-z