Abstract
Study Objective
To evaluate the resident learning curve, demographic and comparative analysis of total laparoscopic hysterectomy.
Design
This retrospective observational study was conducted in a high-volume resident training setup.
Setting
Tertiary care center is used in the study.
Materials and Methods
Eight hundred and one total laparoscopic hysterectomy patients operated by the residents between July 2013 and June 2019 were evaluated with respect to the learning curve, duplication of the steps, the results in terms of intra- and postoperative complications and the time taken for the surgery. Surgeries were assigned as per the institutional inclusion criteria for the residents. The fellowship program enrolled six residents per year for training period of 1 year. The residents initially performed ten simple cases under the supervision of the director followed by ten cases which were performed independently, and based on their learning curve, they then performed advanced cases independently.
Results
TLH was successfully performed in all women by surgical residents in training. The surgical time was 61–120 min in majority (49.3%). 2.99% had intra-operative complications while 7.61% had postoperative complications which were identified and managed. All women recovered uneventfully.
Conclusion(s)
Dedicated teaching staff, uniform surgical protocols and high-volume centers contribute to the safety of TLH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the common major surgeries performed on women is hysterectomy; ninety percent of these are performed for benign indications [1].
Despite various routes for performing a hysterectomy such as abdominal, laparoscopic, vaginal or robot-assisted approach, controversies with respect to the optimal route of surgery [2] always remain a constant matter of debate [3].
Previously, size and mobility of the uterus, age, patient’s body mass index (BMI), past history of any disease or abdominal surgery and nulliparity decided the route of surgery [4].
Laparoscopic hysterectomy carries an advantage of faster recovery and shorter hospital stay, as demonstrated by studies [5]
When the surgeons are well trained, laparoscopic route has been proved to be safer owing to the fewer complications observed when compared with laparotomy or the vaginal route [6].
Ligation of the major vessels supplying the uterus by electrosurgical desiccation, suture ligature or staples through the laparoscopic route encompasses a laparoscopic hysterectomy (LH) [7].
Laparoscopic hysterectomy is a relatively new procedure which is still seldom performed by many gynecologists [8].
Owing to the intricacies of laparoscopic procedures and conflicting obligations during residency training, most gynecology residents are not comfortable in performing a variety of advanced endoscopic procedures at the completion of their training [9].
We feel that absence of volumes is the main reason and therefore decided to retrospectively analyze our data and evaluate the learning curve for total laparoscopic hysterectomy in a high-volume resident training tertiary care center.
Materials and Methods
Evaluation of the resident learning curve, demographic and comparative analysis of total laparoscopic hysterectomy of patients (n = 801) who underwent TLH during July 2013 to June 2019 at the Galaxy Laparoscopy Institute, Pune, India, was done.
Surgeries were done by residents under the supervision of the director. The training program enrolled six residents per year for a training period of one year.
We identified a novel education program that evaluated the learning curve of the residents by dividing the cases into groups of 10 with active assistance first followed by supervision, and the analysis for complications and operative properties was performed between the “first 10,” “10–20” and “20 + ” cases to demonstrate the effect of cutoff levels on the learning curve for laparoscopic hysterectomy.
Residents were given structured training with identical standardized replicable steps.
They initially performed ten simple cases under the supervision of the director followed by ten cases which were performed independently and based on their learning curve; they performed advanced cases independently.
Parameters analyzed included the learning curve, results in terms of complications, time taken for the surgery, demography, intra-operative blood loss and duration of hospital stay.
Preoperative Workup
Relevant preoperative workup comprising of a written informed consent and counseling of patient was done.
Bowel preparation was done one night before the surgery.
Intravenous antibiotic (1 g ceftriaxone) was administered 30 min before the surgery.
The patient was given modified Lloyd-Davies position which includes a bolster under the buttocks at the level of the anterior superior iliac spine (Fig. 1a) [6].
Leakage of the intra-abdominal carbon dioxide following colpotomy was prevented by a surgical glove packed with a sterile pad introduced into the vagina [1].
Procedure of Surgery
Procedure included introduction of the Veress needle at the Palmer’s point (area in the left upper quadrant 3 cm below the costal margin in the mid-clavicular line).
Following insufflation with carbon dioxide, a 5 mm trocar (Endopath® Xcel™ visiport) was inserted in the left upper quadrant lateral to the Veress needle.
A 5 mm telescope was introduced through this port, and the uterus with adnexa was evaluated.
With the aid of the umbilical tube, the primary 10 mm port insertion was done under vision and was supraumbilical/infra-umbilical based on the uterine size and functioned as a camera port followed by three 5 mm accessory ports as shown (Fig. 1b) [6]
Pelvis and upper abdomen were evaluated following insertion of a 10 mm “0” degree telescope.
Myoma screw was used for uterine manipulation.
Coagulation and cutting of the right round ligament, ovarian ligament and the fallopian tube were done. Anterior “U”-shaped incision was taken through the uterovesical fold after opening the anterior leaf of the broad ligament. Sharp and blunt dissection was done, and the urinary bladder was dissected over the cervix.
The left tube and ligament complex was coagulated and cut with uterine retraction to the right, and the anterior U cut was completed.
At this stage, the posterior peritoneum behind the uterine vessels was kept intact. The cervix was lifted anteriorly and kept away from the sigmoid colon with the aid of the working forceps held in the left hand kept at the level of the uterosacral ligaments. Then, identification, coagulation and cutting of the left uterine vessels were done.
Every clamp was placed medial to the uterine artery and parallel to the cervix.
Identical dissection was carried out on the right side. Coagulation and cutting of the posterior peritoneum and the parametrial tissue lateral to the cervix were done maintaining the uterus under continuous traction always ensuring that the dissection was kept above the level of the uterosacral attachment.
At the vaginal angle, parametrium was separated using coagulation. Colpotomy was done from the right vaginal angle toward the left, always being near the cervix which resembled the circumcision of the cervix off its uppermost vaginal attachment.
Whenever indicated, oophorectomy was performed by coagulation and cutting the infundibulo-pelvic ligaments and retrieved per vaginum [1].
Vagina was sutured with 2–0 Vicryl by ipsilateral continuous locking intra-corporeal suturing technique. Following every surgery, bowel and bladder were checked.
Energy Sources
Most of the cases were performed with bipolar cautery and scissors. For some cases, a combination of bipolar, ligature and the harmonic scalpel was also used. Monopolar current was never used. Technique remained uniform irrespective of the energy source used [1].
Catheter was removed after 6 h and liquids were started few hours after the surgery. Depending upon the postoperative course, patient was discharged during the next 3 days, and follow-up was done after 7 days.
Results
During the study period, 801 women were enrolled in the study. All women underwent TLH successfully (Table 1).
Analysis of the demographic parameters revealed that the average age of women was 45 years and the BMI was normal in 59.92% (n = 480) of women included in the study.
Based on the past surgical history, 20.22% (n = 162) had undergone at least one surgery.
The commonest surgery done in the past included LSCS among 64.20% (n = 104) followed by appendectomy among 29.01% (n = 47). Laparoscopic myomectomy and laparoscopic cystectomy/oophorectomy comprised of 4.32% (n = 7) and 2.47% (n = 4), respectively (Fig. 2).
Uterine size was 6–12 weeks in most(n = 462) and16 weeks was the maximum size of the uterus encountered(n = 38) among women who underwent TLH (Fig. 3).
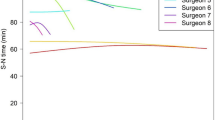
None of them had done a TLH previously. The average operating time and complication rate per resident showed a gradual decline with an increasing number of surgeries. Average surgical time for the first 10 cases was 120 min and 100 min for the next 10 cases. After 20 cases, the surgical time reduced successively and showed a plateau. In a span of 6 years, all 6 residents enrolled for training every year could perform an average of 23 surgeries independently (Fig. 4).
Commonest indication for surgery was uterine fibroid (34.96%) followed by adenomyosis (24.22%). Other indications consisted of endometrial hyperplasia (16.10%), endometrial polyp (8.74%), chronic PID (7.00%), prolapse (5.99%) and risk reduction surgery in 2.99% (Table 2).
Orals were started 6 h post-surgery in 58.30%, on 1st postoperative day in 31.96%, on the 2nd postoperative day in 7.99% and on the 3rd postoperative day in 1.75%. Only 2.75% had a stay for more than 3 days while discharge was given on the first postoperative day in majority (47.94%) of the cases. Blood loss was < 50 ml in 56.8%, 51–100 ml in 38.5%, 101–150 ml in 4.7% patients (Table 3).
Discussion
Attempts to enhance the technique and therefore shorten the learning curve have continued even after 2 decades of the first total laparoscopic hysterectomy by Reich [10]. Laparoscopic hysterectomy is preferred to be the first mode for hysterectomy in many countries as per the present consensus [11].
The resident needed to perform an average of 23 cases to complete the learning curve for total laparoscopic hysterectomy and to perform the surgery independently. Twenty-five cases was the number concluded by Garry et al. required by the surgeons to complete the learning curve [12] and gain adequate experience.
The uniformity of the technique and repetitiveness of the steps over the past 10 years has enabled innumerable residents to duplicate them and understand the surgery in a better manner.
On evaluating the intra-operative complications, serosal ureteral tear was noted in 0.62% (n = 5) in cases with dense ureteral adhesions. Bilateral stenting was done and urinary catheter was kept for a week and discharged uneventfully. Their past surgical history included LSCS in 60% (n = 3) and cystectomy in 40% (n = 2). Indication for TLH was chronic PID. Surgical time was 91–120 and 61–90 min, respectively. Serosal rectal tear was noted in 1.12% (n = 3) among those with rectal adhesions and bladder injury was noted in 1.5% (n = 12) in those with bladder adhesions. Their surgical history included previous LSCS in 73.33% (n = 11) followed by myomectomy in 13.33% (n = 2) and appendectomy in 13.33% (n = 2). Indication for TLH was multiple uterine myomas in 66.67% (n = 10) and adenomyosis in 33.33% (n = 5). Orals were started once flatus had passed, catheter was kept for two weeks, and recovery was uneventful. Evaluation of postoperative complications revealed that urinary tract infection and port site infection were noted in twelve and ten women, respectively, and were treated with antibiotics and alternate day dressing for a week, respectively. Reactionary fever developed in twenty-three women which was treated with antipyretics. Paralytic ileus was noted in six women and urinary retention in five women which were treated conservatively. Pelvic collection was seen in five women and was drained using ultrasonographic guidance with and uneventful recovery. Postoperative hemorrhage was not seen in any patient (Table 4). Operative time for the initial ten surgeries was 120 min. The time reduction with every surgery was directly proportional to the repetitiveness of the procedure. Thus, the average time was less than 100 min after 20 cases for every resident.
Maximum and minimum surgical time in a study by Bettaiah et al. was 20 min and 2 h, respectively [13].
As per the study by Terzi et al., following the first 75 cases, surgical time significantly reduced for junior surgeons [14].
Complication rate was inversely proportional to the number of cases performed by a resident. The complications in our study were seen when the resident had done less than 20 cases. Following 20 cases, there were no major complications.
As per Wattiez et al., an increase in the number of residents performing the surgery did not affect the overall complication rates which was similar to our study [15].
Ascher Walsch et al. concluded that as residents receive more exposure, their ability substantially increases demonstrated by a significant decrease in operating room time [16].
Twinjstra et al. showed that a mentorship program in laparoscopic hysterectomy was of utmost significance for implementation of new surgical techniques with respect to patient safety and suggested that acceleration of the traineeship could be achieved by raising the case volumes via a fellowship for several trainees in one hospital which thus cements the objective of our study [17].
After ten surgeries, residents were able to perform the next ten surgeries independently.
However, this cannot be generalized and is an empiric approach.
All our intra-operative complications namely, ureteric injury (0.62%), serosal bowel injury (0.38%) and bladder injury (1.5%), were recognized and managed intra-operatively.
Re-exploration was not required in any of the cases with intra-operative or postoperative complications.
Supervised mentoring, standardization of steps, disciplined approach and an enthusiastic resident training program were the sole factors which influenced the conversion rate in our study.
Intra-corporeal continuous interlocking technique was employed for all cases for suturing the vaginal cuff.
Following the surgery, none of the patients had vaginal dehiscence probably due to colpotomy using cold scissors, full thickness vaginal vault suturing and all of them being intra-fascial hysterectomies [1].
Different suturing techniques and suture materials did not significantly influence the incidence of vaginal dehiscence as per Smith et al. [18].
Follow-up of residents who had passed out of the institute showed that all of them were now performing laparoscopic gynecological procedures regularly.
The present generation is prepared to accept laparoscopy as the primary choice for gynecological surgery, but there is a mismatch between training and mental acceptance.
This change in attitude in conjunction with better equipment and energy resources leads to early learning.
High-volume centers have the potential to bring out the best from residents. Reasons are standardization of steps and dedicated teaching staff. Thus, surgical outcomes are directly proportional to the volumes.
Uniform preoperative, intra-operative and postoperative surgical protocols, large sample size and retrospective study design were the strengths of our study [1].
This was a single-center study which might not represent the results among other Indian centers [1].
Also, surgical volume or experience of the trainers, senior surgeons is not stated which could cause bias.
Conclusion
Learning curve of TLH in our center was found to be 23 cases.
Dedicated teaching staff, uniform surgical protocols and high-volume centers contribute to the safety of TLH.
Abbreviations
- TLH:
-
Total laparoscopic hysterectomy
- BMI:
-
Body mass index
- LSCS:
-
Lower segment cesarean section
- Fig:
-
Figure
- LH:
-
Laparoscopic hysterectomy
- LAVH:
-
Laparoscopic assisted vaginal hysterectomy
- CO2:
-
Carbon dioxide
- POD:
-
Postoperative day
- LSCH:
-
Laparoscopic-assisted supracervical hysterectomy
- N:
-
Number
- PID:
-
Pelvic inflammatory disease
References
Puntambekar S, Shetty TS, Goel A, et al. Single-centre experience of doing safe total laparoscopic hysterectomy: retrospective analysis of 1200 cases. J Obstet Gynecol India. 2020;70(5):376–83.
Kreuninger JA, Cohen SL, Meurs EAIM, Cox M, et al. Trends in readmission rate by route of hysterectomy—A single-centerexperience. Acta ObstetGynecolScand. 2018;97:285–93.
Pattanaik T, Mishra SP, Das S. Total laparoscopic hysterectomy–a retrospective observational study in a teaching hospital. Ann Int Med Den Res. 2017;3(1):OG10-13.
Wallenstein M, Ananth V, Kim J, et al. Effect of surgical volume on outcomes for laparoscopic hysterectomy for benign indications. Obstet Gynecol. 2012;119:709–16.
David-Montefiore E, Rouzier R, Chapron C, et al. Surgical routes and complications of hysterectomy for benign disorders: a prospective observational study in French university hospitals. Human Reprod. 2007;22(1):260–5.
Puntambekar SP, Wagh GN, Puntambekar SS, et al. A novel technique of total laparoscopic hysterectomy for routine use: evaluation of 140 cases. Int J Biomed Sci. 2008;4(1):38–43.
Sinha R, Sundaram M, Lakhotia S, et al. Total laparoscopic hysterectomy for large uterus. J Gynecol Endosc Surg. 2009;1(1):34–9.
Vree F, Cohen S, Chavan N, et al. The impact of surgeon volume on perioperative outcomes in hysterectomy. JSLS. 2014;18:174–81.
Mikhail E, Scott L, Miladinovic B, et al. Association between fellowship training, surgical volume, and laparoscopic suturing techniques among members of the American association of gynecologic laparoscopists. Minimally Invasive Surg. 2016;2016:1–6.
Nagar O, Sharma A, Shankar V, et al. A comparative study of total laparoscopic hysterectomy and non-descent vaginal hysterectomy for treatment of benign diseases of uterus. Int J Clin Obstetri Gynaecol. 2018;2(4):63–8.
Llarena N, Shah A, Milad M. Bowel injury in gynecologic laparoscopy: a systematic review. Obstetri Gynecol. 2015;125(6):1407–17.
Garry R, Fountain J, Mason S, et al. The eVALuate study: two paralel randomized trials, one comparing laparoscopic with abdominal hysterectomy, the other comparing laparoscopic with vaginal hysterectomy. BMJ. 2004;328:129.
Bettaiah R, Reddy C, Anantha R. Laparoscopic hysterectomies: our 10 years’ experience in a single laparoscopic center. J Obstetri Gynecol India. 2016;66(4):274–81.
Terzi H, Biler A, Demirtas O, et al. Total laparoscopic hysterectomy: analysis of the surgical learning curve in benign conditions. Int J Surg. 2016;35:51–7.
Wattiez A, Soriano D, Cohen SB, et al. The learning curve of total laparoscopic hysterectomy: comparative analysis of 1647 cases. Am Assoc Gynecol Laparosc. 2002;9(3):339–45.
Ascher-Walsh CJ, Capes T. An evaluation of the resident learning curve in performing laparoscopic supracervical hysterectomies as compared with patient outcome: Five-year experience. J Minimally Invasive Gynecol. 2007;14(6):719–23.
Twijnstra AJH, Blikkendaal MD, Kolkman W, Smeets MJGH, et al. Implementation of laparoscopic hysterectomy: maintenance of skills after a mentorship program. Gynecol Obstet Invest. 2010;70:173–8.
Smith K, Caceres A. Vaginal cuff closure in minimally invasive hysterectomy: a review of training, techniques, and materials. Cureus. 2017;9(10):e1766. https://doi.org/10.7759/cureus.1766.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest and nothing to disclose.
Ethical Approval
The study was approved by the Institutional Ethics Committee. Institutional Ethical Clearance taken.
Informed Consent
Informed consent was obtained from all human participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shailesh Puntambekar, Specialist in the Department of Minimal Access Surgery; Theertha Shetty, Fellow in the Department of Minimal Access Surgery (Gynaecology); Seema Puntambekar, Specialist in the Department of Minimal Access Surgery; Arjun Goel, Fellow in the Department of Minimal Access Surgery; Mangesh Panse, Specialist in the Department of Minimal Access Surgery; Ravindra Sathe, Specialist in the Department of Minimal Access Surgery; Swapnil Shelke, Fellow in the Department of Minimal Access Surgery (Gynaecology).
Rights and permissions
About this article
Cite this article
Puntambekar, S., Shetty, T., Puntambekar, S. et al. Learning Curve of Total Laparoscopic Hysterectomy for a Resident in a High-Volume Resident Training Setup. J Obstet Gynecol India 72 (Suppl 1), 267–273 (2022). https://doi.org/10.1007/s13224-021-01540-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-021-01540-8