Abstract
Study Objective
To evaluate the association between outcomes of laparoscopic hysterectomy with respect to clinical factors, intraoperative variants, and post-operative complications.
Design
The study conducted was retrospective (Canadian Task Force Classification II-1).
Setting
The set used in this study was a gynecological laparoscopic centre.
Patients
The present study included 858 women who underwent laparoscopic hysterectomies with or without bilateral/unilateral salpingo-oophorectomy, from December 2004 to May 2014.
Interventions
Eight hundred and sixteen patients underwent total laparoscopic hysterectomy, 14 patients underwent subtotal laparoscopic hysterectomy, 20 patients underwent laparoscopic-assisted vaginal hysterectomy, and 8 patients underwent laparoscopic radical hysterectomy with bilateral pelvic lymph node dissection.
Measurements and Main Results
All surgeries were performed by the same surgeon, using the same surgical technique. The medical records were reviewed, and data were collected with respect to age, indications, type of surgery performed, intraoperative variants, and post-operative complications. Patient average age was 44.9 ± 6.2 years. Most common indication for benign TLH was leiomyoma of 54.4 %. Indications for laparoscopic radical hysterectomy were early stage endometrial cancer (n = 5) and early stage cervical cancer (n = 3). The maximum uterine size operated on was from 20–26 weeks, 4.9 % (n = 42). 9.7 % had previous abdominopelvic surgery. Fifty three % underwent unilateral/bilateral salpingo-oophorectomy. Conversion rate was 0.93 % (n = 8). The minimum and maximum operating time during the total study period was 20 min–2 h. The major complication rates were 0.9 % (n = 8). The hospital stay was not more than 2 days.
Conclusion
In our experience of 858 laparoscopic hysterectomies, 850 were done for benign indications, and 8 done for malignancies. TLH can be performed more safely and under vision, with less blood loss, early post-operative recovery, less post-operative infection, and less complication rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
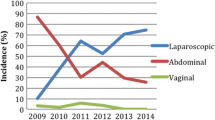
Across the world, the most common gynecologic surgical procedure performed is hysterectomy, the most common being benign indications which contribute to more than 70 % [1] such as myomas, dysfunctional uterine bleeding with or without endometrial hyperplasia, adenomyosis, pre-invasive disease like cervical dysplasia, or for malignant disease such as endometrial cancer or early stage cervical cancer [2]. Nowadays, laparoscopy is being increasingly adopted besides the traditional open access and vaginal access. It has been 20 years since Harvey Reich performed the first total laparoscopic hysterectomy [3]. Later gynecologic surgeons have made many efforts to improve the technique thereby shortening the learning curve and improve outcomes, reducing iatrogenic urinary-tract injuries, intraoperative blood loss [4], hospitalization time, and recovery time [5]. Now with the improvement of surgical skills, it has been considered with a day surgery hospital stay [6–9].
The aim of this study is to evaluate the association between outcomes of laparoscopic hysterectomy with respect to clinical factors, intraoperative variants, post-operative complications in benign, and malignant disease.
Materials and Methods
This is a retrospective study of 858 cases of laparoscopic hysterectomies, between December 2004 and May 2014 performed by the single surgeon using the same surgical technique in a single laparoscopic center. The technique initially involved the use of bipolar and cutting scissors for upper pedicles, uterines, and the Mckenrodts–uterosacral complex, with monopolar being used to open the vault. Later harmonic was used for upper pedicles, Mckenrodts–uterosacral complex, and vault, enseal for uterines. The clinical records of all cases were reviewed, and data were collected with respect to age, major surgical indications, concomitant surgical procedures, and intraoperative variants—single/multiple port, size of uterus, route of morcellation, vault closure, and intra- and post-operative complications.
Surgical Technique
After counseling the patient, informed consent was obtained. Pre-operative preparation mainly involved basic blood counts. Bowel preparation was done the day prior to surgery and kept nil per oral for a minimum of 6 hours.
All surgeries were performed with the patient under general anesthesia and in a modified lithotomy position. Bladder catheterisation was done. The surgeon was always on the left side of the patient.
The veress needle was inserted at the umbilicus for most of the patients. Palmer’s point entry was done in patients with suspected adhesions with previous surgeries or failed umbilicus entry.
After insufflation with carbon dioxide, 10-mm primary trocar was inserted either at umbilicus or supraumbilical depending on the size of the uterus after which Trendelenburg position was given. A 10-mm telescope was introduced, and entry site was inspected for any injury. A maximum of three secondary 5 mm ports were introduced, first on left lateral side, second on right lateral side, and a third port suprapubically in midline. All secondary ports were introduced under vision.
The pelvis and abdomen were inspected to know the nature of disease—adhesions, endometriotic spots, size of uterus, tubal, and ovarian pathology. Adhesions were seen in most of the patients with previous surgeries, which were released either with bipolar and scissors or harmonic. A 5-mm myoma screw was used whenever uterine manipulation was required. Sukhadiya’s vaginal manipulator (Fig. 1) was used for vaginal manipulation.
The technique which was followed was the same. The energy sources used varied from bipolar with scissors, monopolar to harmonic. For patients with removal of ovaries, the infundibulopelvic ligament was cauterized and cut. For women with ovary preservation, the uterine–ovarian ligaments and fallopian tubes were cauterized and cut medial to the ovaries. The anterior and posterior leafs of broad ligament were opened. The bladder dissection was started from left lateral window, the uterovesical fold dissected, and the bladder pushed down. The plane was identified by the loose areolar tissue which is avascular. Following this, bilateral uterines skeletonization was done. The uterines were cauterized just 2 cm lateral to the uterus, and care was taken not to go very laterally to avoid ureteric injury. The vaginal manipulator was pushed to delineate the cervico vaginal junction. A circular incision was given thereby cutting the Mckenrodts and uterosacral complex and opening of vault. Specimen retrieved either by vaginal/laparoscopic morcellation depending on the size of the uterus. Vault was closed vaginally or laparoscopically either with barbed no. 1 suture or vicryl no. 1. Adequate hemostasis was achieved.
Data Analysis
Statistical analysis was performed using SPSS for windows, version 16.0.
Results
In 10 years, 858 laparoscopic hysterectomy procedures were performed. 95.1 % (n = 816) were total laparoscopic hysterectomy, 1.63 % (n = 14) were subtotal laparoscopic hysterectomy, 2.33 % (n = 20) were laparoscopic-assisted vaginal hysterectomy, and 0.9 % (n = 8) were laparoscopic radical hysterectomy with bilateral pelvic lymph node dissection (flow chart). Mean age of the patients who underwent laparoscopic hysterectomies was 44.9 ± 6.2 (minimum 16, maximum 71). The main benign surgical indications were leiomyoma 54.4 %; dysfunctional uterine bleeding refractory to medical management: 17.8 %; adenomyosis: 8.8 %; post-menopausal bleeding: 3.4 %; endometriosis: 3.2 %; endometrial hyperplasia: 2.2 %; and others were chronic pelvic pain, ovarian cyst, and third-degree uterovaginal prolapse (Table 1). The indications for subtotal laparoscopic hysterectomy were endometriosis, huge cervical fibroid, dense bladder, and omental adhesions. Eight laparoscopic radical hysterectomies with bilateral pelvic lymph node dissection were done. Five were early stage endometrial cancer, and three were early stage cervical cancer.
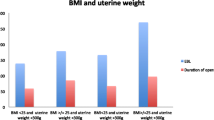
We also observed that among all age groups 31–60 years, the most common indication was leiomyoma followed by dysfunctional uterine bleeding refractory to medical management (Table 2). In >60 years age group, the most common indication was post-menopausal bleeding. 9.7 % (n = 83) of the patients had undergone at least one previous abdominopelvic surgery (Graph 1). Of these, 76 % (n = 63) had previous LSCS, 8.4 % (n = 7) had myomectomy, 6 % (n = 5) had appendicectomy, 7.2 % (n = 6) had cystectomy, 1.2 % (n = 1) had endometriosis, and 1.2 % (n = 1) had umbilical hernia. Maximum size of uterus operated on was 20–26 weeks (n = 42) 4.9 %, and maximum patients had a uterine size of 6–12 weeks (n = 490) 57.6 % (Graph 2). TLH was performed with unilateral or bilateral adnexal surgery in 53 % (n = 455) of the patients, criteria being removal of pathological ovaries only (Graph 3). Laparoscopic morcellation of the uterus was needed in 2.9 % (n = 25) of surgeries, vaginal morcellation in 93.4 % (n = 787) of surgeries, and both routes were used in 3.5 % (n = 30). Eight cases were not included due to conversion to abdominal and vaginal hysterectomy. We observed that vaginal morcellation was more advantageous than laparoscopic morcellation as no sophisticated equipment was required; no extra port was required; it was simple, easy, and faster; no port site post-operative pain; no spillage was observed; and reduced risk of injury to major organs. Vault was closed vaginally in 29.2 % (n = 239), and laparoscopic vault closure was done in 69.7 % (n = 569). Vault was left open in 0.9 % (n = 8) in two patients who underwent laparoscopic radical hysterectomy, one of endometriosis, four of huge fibroids, and one of CIN. This was mainly to facilitate drainage of any collection and also to reduce morbidity in v/o drain insertion. TLH operative time was between 20 min and 2 h. The operating time was reduced with experience. Major intraoperative complications involved two bladder injuries, two ureteric injuries, and one vaginal tear which were corrected intraoperatively. One patient had bradycardia and hypotension which was converted to vaginal hysterectomy. No bowel injuries were noted. Conversion rate was 0.93 %. Four were converted to abdominal hysterectomy, one to mini laparotomy and three to vaginal hysterectomy. Among those who underwent abdominal hysterectomy, one had fibroid uterus with distorted anatomy, one had right ureteric injury and ureteric reanastomosis was done, and two had dense omental and bowel adhesions. One minilaparotomy was done due to impacted broad ligament fibroid. Three were proceeded with vaginal hysterectomy due to dense omental and bowel adhesion, bradycardia, and hypotension.
Concomitant surgical procedures excluding adhesiolysis were performed in 6.5 % (n = 56) of the patients, which included hernia repair in 19, cholecystectomy in 11, appendicectomy in 20, and transobturator tape in 2 (Table 3). Omental adhesions were seen in 79, bladder adhesions in 24, and bowel adhesions in 14, and extensive adhesiolysis was done in 12 (Table 4). Eight laparoscopic radical hysterectomies with pelvic lymph node dissection were done, of which five were endometrial cancers and three were early cervical cancers.
Single-port laparoscopic hysterectomy was done in 20 cases (2.3 %). We compared the size of uterus operated on in single port. The maximum size of uterus was 12–16 weeks (Graph 4).
Post-operative hospital stay was not more than 2 days for most patients, maximum duration of stay being 4 days.
First post-operative follow-up was at 8–10 days. 3–4 % patients presented with bleeding from vault, and one patient had post-operative pancreatic abscess. Two ureterovaginal fistulas were recognized on the fourth and eighth post-operative day and corrected post-operatively. Second post-operative follow-up was at 2–3 months, and menopausal symptoms were the most common complaint. On long-term follow-up, no cases of vault prolapse were observed.
In post-laparoscopic radical hysterectomy, on follow-up, one patient with endometrial cancer had overflow incontinence and one patient with early stage cervical cancer had recurrence.
Discussion
We assessed the outcomes of laparoscopic hysterectomy with respect to clinical factors, intraoperative variants, and post-operative complications.
We observed that TLH is safe and can be performed for various indications including malignancy and even for a larger size uterus.
Initially, laparoscopic hysterectomy was criticized due to its technical difficulty, increased operative time, and increased number of complications particularly ureteric, bladder, and bowel injuries. But then, studies have shown that laparoscopic hysterectomy has been advantageous compared to abdominal hysterectomy which include less operative time and decreased hospital stay [10–13]. Also, laparoscopy allows for easier access to uterine vessels and ureter due to its high-definition imaging and vision magnification.
Most recent studies present TLH as safe, being performed for various indications including malignancy [11, 14–16].
About 9.7 % (n = 83) had undergone at least one previous abdominopelvic surgery. The main surgical indications for hysterectomy in our study were leiomyoma: 54.4 %, dysfunctional uterine bleeding refractory to medical management: 17.8 %, adenomyosis: 8.8 %, post-menopausal bleeding: 3.4 %, endometriosis: 3.2 %, and endometrial hyperplasia: 2.2 %.
Many concomitant procedures were performed, which show the efficacy of the laparoscopic approach for different surgical procedures in gynecology, without the need for conversion to neither a laparotomy nor a second surgical time. The operative time in our study was a minimum of 20 min and maximum of 2 h with a significant decrease over the years.
Mean post-operative stay was 2 days.
In our study, the complication rate was 0.9 %. In various studies conducted, Karaman et al. [15] and Brummer et al. [7] described a major complication rate of 1 and 1.8 %, respectively. In addition, Donnez described his retrospective study with 400 patients who underwent laparoscopic hysterectomy procedure, a major complication rate of 1.5 % [14].
The limitation in our study was that the data were obtained from clinical records and as such was dependent on clear and complete information. In addition, this was a retrospective study, without a control group. Estimations of blood loss were estimations, per se. It is a weakness of this study that blood loss was not measured in a more precise fashion. Precise assessment of patient hospital stays would have required calculation of the hours from the end of surgery to the hour of discharge. Unfortunately, this was not done.
Conclusion
In our experience of 858 laparoscopic hysterectomies, 850 were done for benign indications and 8 done for malignancies. TLH can be performed more safely and under vision, less post-operative infection, less blood loss, and early post-operative recovery. Most common indications for benign TLH were leiomyoma (54.4 %) and DUB refractory to medical management (17.8 %). Average operative time was 20 min–2 h. Most common previous surgeries were LSCS. In the current era of conflicts regarding power morcellation, we observed that vaginal morcellation was observed to be more advantageous than laparoscopic morcellation. Laparoscopic vault closure was found superior to vaginal vault closure as it was done under direct vision including the uterosacral stumps.
References
Whiteman MK, Hillis SD, Jamieson DJ, et al. Inpatient hysterectomy surveillance in the United States, 2000–2004. Am J Obstet Gynecol. 2008;198:1–7.
Hobson DT, Imudia AN, Al-Safi ZA, et al. Comparative analysis of different laparoscopic hysterectomy procedures. Arch Gynecol Obstet. 2012;285(5):1353–61.
Bonilla DJ, Mains L, Rice J, et al. Total laparoscopic hysterectomy: our 5-year experience (1998–2002). Ochsner J. 2010;10:8–12.
Hohl MK, Hauser N. Safe total intrafascial laparoscopic (TAIL) hysterectomy: a prospective cohort study. Gynecol Surg. 2010;7(3):231–9.
O’Hanlan KA, Dibble SL, Garnier AC, et al. Total laparoscopic hysterectomy: technique and complications of 830 cases. JSLS. 2007;11(1):45–53.
Lassen PD, Moeller-Larsen H, De Nully P. Same-day discharge after laparoscopic hysterectomy. Acta Obstet Gynecol Scand. 2012;91(11):1339–41.
Rettenmaier MA, Mendivil AA, Brown JV III, et al. Same-day discharge in clinical stage I endometrial cancer in patients treated with total laparoscopic hysterectomy, bilateral salpingo-oophorectomy and bilateral pelvic lymphadenectomy. Oncology. 2012;82(6):321–6.
Gauta J. Outpatient laparoscopic hysterectomy: evaluation of pain. JSLS. 2011;15(3):346–9.
Nieboer TE, Johnson N, Lethaby A, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009;3–4:CD003677.
Donnez O, Jadoul P, Squifflet J, et al. A series of 3190 laparoscopic hysterectomies for benign disease from 1990 to 2006: evaluation of complications compared with vaginal and abdominal procedures. BJOG. 2009;116:492–500.
Wattiez A, Soriano D, Cohen SB, et al. The learning curve of total laparoscopic hysterectomy: comparative analysis of 1647 cases. J Am Assoc Gynecol Laparosc. 2002;9:339–45.
Kluivers KB, Hendriks JC, Mol BW, et al. Quality of life and surgical outcome after total laparoscopic hysterectomy versus total abdominal hysterectomy for benign disease: a randomized, controlled trial. J Minim Invasive Gynecol. 2007;14:145–52.
Donnez O, Donnez J. A series of 400 laparoscopic hysterectomies for benign disease: a single centre, single surgeon prospective study of complications confirming previous retrospective study. BJOG. 2010;117:752–5.
Karaman Y, Bingol B, Günenç Z. Prevention of complications in laparoscopic hysterectomy: experience with 1120 cases performed by a single surgeon. J Minim Invasive Gynecol. 2007;14:78–84.
Bojahr B, Raatz D, Schonleber G, et al. Perioperative complication rate in 1706 patients after a standardized laparoscopic supracervical hysterectomy technique. J Minim Invasive Gynecol. 2006;13:183–9.
Brummer TH, Seppälä TT, Härkki PS. National learning curve for laparoscopic hysterectomy and trends in hysterectomy in Finland 2000–2005. Hum Reprod. 2008;23:840–5.
Compliance with ethical requirements and Conflict of interest
No ethical approval was needed for this study. Written and informed consents were taken for all patients who underwent the surgery and the authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bettaiah, R., Reddy, C.A.R. Laparoscopic Hysterectomies: Our 10 Years Experience in a Single Laparoscopic Center. J Obstet Gynecol India 66, 274–281 (2016). https://doi.org/10.1007/s13224-014-0665-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-014-0665-6