Abstract
Background
The prognostic implications of ST-segment and T-wave (ST/T) abnormalities in patients undergoing stress SPECT-myocardial perfusion imaging (MPI) are not well defined.
Methods and Results
This was a single-center, retrospective cohort study of consecutive patients who underwent regadenoson stress SPECT-MPI. Patients with baseline electrocardiogram (ECG) abnormalities that impede ST/T analysis or those with known coronary artery disease were excluded. Patients were categorized as having primary ST abnormalities, secondary ST/T abnormalities due to ventricular hypertrophy or right bundle branch block, T-wave abnormalities, or normal ECG. The primary outcome was major adverse cardiovascular events (MACE) defined as the composite of cardiac death or myocardial infarction. Among 6,059 subjects, 1912 (32%) had baseline ST/T abnormalities. During a mean follow-up of 2.3 ± 1.9 years, the incidence of MACE was significantly higher among patients with secondary ST/T abnormalities compared to those with normal ECG (HR 2.05; 95% confidence interval [CI], 1.04-4.05; P = 0.039). No significant difference in MACE was observed among patients with primary ST abnormalities (HR 1.64; CI 0.87-3.06; P = 0.124) or T-wave abnormalities (HR 1.15; CI 0.62-2.16; P = 0.658) compared with patients who had normal ECG. Among patients with secondary ST/T changes, abnormal MPI was not associated with a significant increase in MACE rates compared to normal MPI (HR 1.18; CI 0.31-4.58; P = 0.808). However, abnormal MPI was associated with higher MACE rates among patients with primary ST abnormalities (HR 4.50; CI 1.44-14.10; P = 0.005) and T-wave abnormalities (HR 3.74; CI 1.20-11.68; P = 0.015). Similarly, myocardial ischemia on regadenoson stress SPECT-MPI was not associated with a significant increase in MACE rates in patients with secondary ST/T abnormalities (HR 1.45; CI 0.38-5.61; P = 0.588), while it was associated with a higher incidence of MACE in patients with primary ST abnormalities (HR 3.012; CI 0.95-9.53; P = 0.049) and T-wave abnormalities (HR 5.06; CI 1.60-15.96; P = 0.002).
Conclusion
While patients with secondary ST/T abnormalities had significantly higher MACE risk, abnormal MPI or presence of myocardial ischemia on regadenoson SPECT-MPI in this group does not add prognostic information. Patients with primary ST abnormalities and T-wave abnormalities do not seem to have a significantly higher MACE risk compared to those with normal ECG; however, abnormal MPI or presence of myocardial ischemia, in these groups, correlates with higher MACE rates.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
ST-segment and T-wave abnormalities (ST/T) are frequently encountered in clinical practice 1 and represent a common dilemma in the interpretation of electrocardiograms (ECGs). Such resting ECG abnormalities commonly raise concerns for underlying coronary artery disease (CAD). In addition, these patients frequently have a variety of ischemic equivalent symptoms, and thus often undergo stress imaging studies, such as myocardial perfusion imaging (MPI) with single photon emission computed tomography (SPECT) for diagnostic and prognostic evaluation.2,3 While ST/T abnormalities have been shown to be associated with adverse outcomes in the general population,4,5,6,7,8 the prognostic implications of such abnormalities among patients referred for stress MPI are unclear.9,10,11,12,13,14,15
Some studies have shown that ST/T abnormalities are associated with cardiovascular morbidity and mortality11,15,16 regardless of sex, ethnicity, and comorbidities, while others have found no significant difference.17 This prognostic variability could be due to many factors such as varying inclusion criteria, comorbidities, sample size, and duration of follow-up. Moreover, majority of the studies have not further subcategorized the ST/T abnormalities into primary ST abnormalities, secondary ST/T abnormalities due to ventricular hypertrophy or right bundle branch block, and T-wave abnormalities, to determine cardiovascular outcomes within each subset. Furthermore, limited data exists regarding the prognostic value offered by stress SPECT-MPI in these patients.
The main objective of this study was to determine the prognostic implications of various subsets of ST/T abnormalities in patients undergoing regadenoson stress MPI. We also sought to determine the yield and prognostic value of regadenoson stress SPECT-MPI in patients with various subsets of ST/T abnormalities.
Methods
Study Cohort
We implemented a retrospective cohort study design. Patients who underwent regadenoson stress SPECT-MPI at Rush University Medical Center, Chicago, IL from July 1, 2009, to September 11, 2015, were analyzed. In cases where more than one regadenoson stress MPI was performed, the data from the first study was used for analysis. During the investigation period, 16,506 unique patients underwent their first stress MPI, among whom 5,942 (36%) underwent exercise stress protocol and 10,564 (64%) received regadenoson stress studies. Data on the regadenoson stress MPI studies were collected and analyzed. The detailed methodology used to derive this cohort has been published before.18 Subjects with missing MPI or missing ECG tracings were excluded. Patients with confirmed acute coronary syndromes were excluded, as the prognostic utility of ST-segments and T-wave abnormalities in this setting has been well established.19,20 Patients with conditions that are inherently associated with ST/T abnormalities, namely left bundle branch block, non-specific interventricular conduction delay, and paced ventricular rhythm, were excluded. Patients with baseline atrial flutter, which may impede ST/T analysis were also excluded. Subjects with known CAD, defined as prior myocardial infarction (MI) or coronary revascularization, were also excluded, as ST/T abnormalities may be residua from prior ischemic myocardial insult. Patients with right bundle branch block were not excluded, and the associated ST-segment/T-wave abnormalities were considered secondary.
ECG Criteria
ST/T abnormalities were determined by the interpreting cardiologist at the time of the test, guided by the “Recommendations for the Standardization and Interpretation of the Electrocardiogram” from the American Heart Association, American College of Cardiology, and Heart Rhythm Association consensus statement.21 The observers interpreting the ECGs were unaware of the MPI and outcome data. ST/T abnormalities were defined as any deviation of the ST-segment below the baseline, while T-wave abnormalities were defined as any negative deflection of the T-wave below the baseline. Patients with ST/T abnormalities were further subcategorized into primary ST abnormalities, secondary ST/T abnormalities, and isolated T-wave abnormalities. Secondary ST/T abnormalities were defined as changes in the ST-segment and/or T-wave due to left ventricular hypertrophy, right ventricular hypertrophy, or right bundle branch block. ST-segment abnormalities other than secondary were categorized as primary ST abnormalities. Isolated T-wave changes (without accompanying ST-segment changes), not considered to be secondary, were classified as T-wave abnormalities.
Stress MPI Protocol
Regadenoson stress SPECT-MPI studies were performed according to the American Society of Nuclear Cardiology guidelines.22,23 Patients’ instructions included abstinence of caffeinated foods or beverages for a minimum of 12 hours, and arrival to the nuclear cardiology laboratory in past midnight fasting state. Regadenoson 0.4 mg was given as a single bolus through a peripheral venous catheter followed by a saline flush. Since patients with left bundle branch block and paced ventricular rhythm were excluded from this analysis, all subjects included in this investigation were encouraged to perform a non-standardized low-level leg lifting exercise, as tolerated.24,25 Almost all patients underwent standard one-day rest/regadenoson stress protocol. However, dual-isotope protocol was occasionally used during periods of 99mTc shortage, and two-day protocol with 99mTc-tetrofosmin was used in morbidly obese individuals (body mass index ≥ 40 kg/m2). SPECT-MPI was acquired by dual-head Siemens Ecam® camera (Siemens; Hoffman Estates, IL), without attenuation correction.26,27
MPI scans were quantitatively analyzed by investigators blinded to clinical, ECG, and outcome data, using Corridor4DM software package (INVIA; Ann Arbor, MI). Perfusion abnormalities were quantified using a 17-segment model and the standard 5-point scale (0, normal; 1, mild; 2, moderate; 3, severe; 4, absent radiotracer activity).28 Myocardial perfusion scoring was automatically determined by mapping the normalized segmental photon count intensities to a corresponding perfusion score (0-4).28 The summed stress scores (SSS), summed rest scores (SRS), and summed difference scores (SDS) were determined quantitatively with no investigator over-read. Minimal processing manipulation of perfusion data was allowed in order to correct erroneous software determination of the left ventricular myocardium, base, long access, or apex. Once the perfusion data is reconstructed, perfusion scores were not manipulated or over-read since we intended a fully quantitative perfusion analysis. MPI studies were further classified as normal (SSS 0-3), mildly abnormal (SSS 4-8), moderately abnormal (SSS 9-13), and severely abnormal (SSS ≥ 14).29,30 Similarly, based on SDS, ischemic burden was categorized into no ischemia (SDS 0-1), mild ischemia (SDS 2-4), and moderate to severe ischemia (SDS ≥ 5).29 Transient ischemic dilation (TID) was calculated as the ratio of the stress to rest left ventricular volumes, as measured from the ungated SPECT images.31,32 A TID ratio ≥ 1.31 was considered abnormal, based on published literature.32 Left ventricular ejection fraction (LVEF) was measured quantitatively. LVEF reserve was calculated as post-stress LVEF minus rest LVEF.33
Outcomes
Data was collected on all-cause death, cardiac death, MI, and coronary revascularization. The reviewers who adjudicated outcome events were blinded to the ECG and MPI findings. Outcome status and events dates were determined by conducting a comprehensive chart review of available procedure notes and subsequent clinical encounters in cardiology clinic, primary care visits, emergency room, and hospital admissions. Social Security Death Index search was used to determine the vital status of all patients. Clinical charts (primarily) and death certificates (secondarily) were reviewed to determine the cause of death. Cardiac death was defined as death due to fatal MI, fatal arrhythmias, or heart failure. Cause of death was adjudicated, primarily, by reviewing the electronic health records or, secondarily, from the first listed cause of death in the official death certificate. MI was defined as elevated cardiac biomarkers consistent with acute coronary syndrome, as determined by the managing cardiologist in accordance with the accepted global definition of myocardial infarction guidelines. The primary outcome was major adverse cardiovascular events (MACE), defined as the composite of cardiac death or MI.
Statistical Analysis
Continuous data were expressed as means ± standard deviations, while categorical data were depicted as frequencies and percentages. The Chi-square test was used to compare categorical variables while the two-tailed, independent-samples Student’s t-test was used to compare normally distributed continuous variables. The Mann–Whitney test was used to compare skewed or non-parametric data. Kaplan-Meier plots and the log-rank test were used to compare event-free survivals. Adjusted risks of adverse events were assessed using multivariate Cox regression models and were expressed as hazard ratios (HR) and 95% confidence intervals (CI). Important covariates that were adjusted for included age, gender, hypertension, diabetes mellitus, dyslipidemia, and smoking. Time zero in survival analyses represented the date of stress MPI, and the follow-up time was defined as either a qualifying MACE, last event-free encounter, or a maximum follow-up of 6.5 years, whichever occurred first. Two-tailed P value of < 0.05 was considered statistically significant in all cases. All analyses were performed using SPSS version 23 software package (IBM, Inc.; Armonk, NY). The study was approved by the institutional review board of Rush University Medical Center (Chicago, IL).
Results
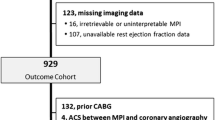
Among 10,564 unique patients who underwent regadenoson stress SPECT-MI, 4,505 were excluded due to missing MPI files (N = 289), missing ECG tracings (N = 41), ventricularly paced rhythm (N = 322), LBBB (N = 295), prior MI or known CAD (N = 3,907), atrial flutter (N = 41), and interventricular conduction delay (N = 231). Table 1 summarizes the baseline characteristics of the 6,059 subjects included in the study. The mean age of the cohort was 60 ± 13 years, 41% were men, 1,912 (32%) had ST/T abnormalities [596 (10%) with primary ST abnormalities, 312 (5%) with secondary ST/T abnormalities, 1,004 (17%) with T-wave abnormalities], and 4,147 (68%) had normal ECG.
Table 2 outlines the MPI findings of the study subjects. Notably, patients with ST/T abnormalities had greater burden of perfusion abnormality (SSS) and myocardial ischemia (SDS), lower LVEF, larger left ventricular end-diastolic volume, and greater left ventricular mass (Table 2). Among the study subjects, 1,118 (18.5%) had abnormal MPI and 1,127 (18.6%) had myocardial ischemia on MPI.
As shown in Figure 1, abnormal MPI was more prevalent among patients with primary ST abnormalities [128/596 (21%)], secondary ST/T abnormalities, [81/312 (26%)], and T-wave abnormalities 223/1004 (22%), compared to those with normal ECG [686/4147 (17%)], (P values < 0.001). Similarly, myocardial ischemia was more prevalent among patients with primary ST abnormalities [126/596 (21%)], secondary ST/T abnormalities [68/312 (22%)], and T-wave abnormalities [207/1004 (21%)], compared to those with normal ECG [726/4147 (18%)], (P values < 0.001). Left ventricular dysfunction was also more prevalent among patients with all subsets of ST/T abnormalities, but also it was more prevalent among those with secondary ST/T abnormalities, compared to those with primary ST abnormalities or T-wave abnormalities (Figure 1). Supplementary Tables 1 and 2 summarize the baseline clinical and imaging characteristics of the study subjects stratified according to subsets of ST/T abnormalities.
Prevalence of MPI abnormalities in study groups. MPI, myocardial perfusion imaging; LV, left ventricular; LVEF, left ventricular ejection fraction. *Prevalence of Abnormal MPI is significantly higher than in Normal ECG group. †Prevalence of Myocardial Ischemia is significantly higher than in Normal ECG group. ‡Prevalence of LV dysfunction is significantly higher than in Normal ECG group
Outcome
During a mean follow-up of 2.3 ± 1.9 years, MACE (composite cardiac death or MI) occurred in 89 (1.5%) patients. The observed MACE rates were significantly different (P = 0.046) among various study groups, as follows: 12/596 (2.0%) in the primary ST abnormalities group, 10/312 (3.2%) in the secondary ST/T abnormalities group, 12/1,004 (1.2%) in T-wave abnormalities group, and 55/4,147 (1.3%) in the normal ECG group (Figure 2). MACE rate was significantly higher among patients with secondary ST/T abnormalities compared with patients who had normal ECG (HR 2.05; 95% CI 1.04-4.05; P = 0.039), even after adjusting for clinical covariates of age, sex, hypertension, diabetes, dyslipidemia, and smoking (HR 2.02; CI 1.02-4.0; R = 0.044). No significant difference in MACE rates was observed among patients with primary ST abnormalities (HR 1.64; 95% CI 0.87-3.06; P = 0.124) or T-wave abnormalities (HR 1.15; 95% CI 0.62-2.16; P = 0.658), compared to those with who had normal ECG.
MACE rates according to baseline ST/T abnormalities. MACE, major adverse cardiac events. P value was derived from a log-rank test comparing MACE-free survival among all four groups. MACE rate was significantly higher among patients with secondary ST abnormalities vs. normal ECG. There was no significant difference in MACE rates between subjects with primary ST abnormalities vs. normal ECG and those with T-wave abnormalities vs. normal ECG
Figures 3 summarizes the annualized event rates in study groups according to MPI abnormalities. As shown in Figure 4, among patients with secondary ST/T abnormalities, abnormal MPI was not associated with a significant increase in MACE rate when compared to patients with a normal MPI (HR 1.18; 95% CI 0.31-4.58; P = 0.808). Conversely, abnormal MPI was associated with higher MACE rates among patients with primary ST abnormalities (HR 4.50; CI 1.44-14.10; P = 0.005) and T-wave abnormalities (HR 3.74; CI 1.20-11.68; P = 0.015). The predictive value of abnormal MPI in patients with primary ST abnormalities and T-wave abnormalities remained significant after adjusting for clinical covariates.
Similar pattern was seen when MACE-free survivals were compared in study groups in relation to myocardial ischemia on regadenoson stress SPECT-MPI (Figure 5). Myocardial ischemia was not associated with a significant increase in MACE rate in patients with secondary ST/T abnormalities when compared to those without myocardial ischemia (HR 1.45; CI 0.38-5.61; P = 0.588). On the other hand, myocardial ischemia was associated with higher MACE rates among patients with primary ST abnormalities (HR 3.012; CI 0.95-9.53; log-rank, P = 0.049) and T-wave abnormalities (HR 5.06; CI 1.60-15.96; P = 0.002). The prognostic value of myocardial ischemia in patients with primary ST abnormalities and T-wave abnormalities was significant after adjusting for clinical covariates.
Discussion
This large cohort study of patients with ST/T abnormalities undergoing regadenoson stress SPECT imaging reports several important clinical findings. First, ST/T abnormalities are common among patients referred for regadenoson stress MPI. Second, there was an independent association of secondary ST/T changes with increased risk of MACE compared to normal ECG, whereas no such association was observed among patients with primary ST abnormalities and isolated T-wave abnormalities. Third, ST/T abnormalities were associated with higher rates of perfusion, functional, and structural abnormalities. Fourth, abnormal MPI or presence of myocardial ischemia on regadenoson SPECT-MPI was not associated with increased risk of MACE in patients with secondary ST/T abnormality. However, abnormal MPI or presence of myocardial ischemia was independently associated with increased MACE rates in patients with primary ST abnormalities or T-wave abnormalities. These results were consistent after adjustment for important clinical covariates. Importantly, the study cohort did not include patients with acute coronary syndrome or known CAD.
With the immense growth in its safety, tolerability, and prognostic data,34,35,36,37,38 regadenoson stress has emerged as the new standard in vasodilator stress MPI. Hage et al. and Katoor et al. demonstrated a step-wise increase in the rates of adverse cardiac events with increasing severity of regadenoson-induced perfusion abnormalities on SPECT-MPI.39,40 Farzaneh-Far et al. established that SSS and SDS derived from regadenoson SPECT-MPI have similar predictive value for MACE as those indices produced by adenosine SPECT-MPI.41 Doukky et al. and Kolkailah et al. confirmed the incremental prognostic value of regadenoson SPECT-MPI in predicting cardiac death or MI in patients with end-stage renal disease, particularly among those undergoing kidney transplantations.30,37,42,43,44,45 More recently, Kassab et al. showed that even subtle perfusion abnormalities (SSS = 1 – 3 or SDS = 1) observed on regadenoson SPECT-MPI are associated with increased prevalence of obstructive CAD and higher rates of coronary revascularization, but no significant difference in hard events of cardiac death or MI.46 Lester et al. showed that abnormal TID in patients with abnormal regadenoson SECT-MPI is associated with increased risk of cardiac events.47 Doukky et al. demonstrated the incremental diagnostic and prognostic value of regadenoson-induced ischemic ST-segment depression, above and beyond MPI.18,48 Aljaroudi et al. and Gomez et al. affirmed the prognostic utility of heart rate response to regadenoson stress in patients with end-stage renal disease.49,50,51 Our study adds to this growing body of evidence, establishing the prognostic utility of regadenoson stress MPI in patients with baselines ST/T abnormalities, a common indication for referral for SPECT-MPI.
In our investigation, secondary ST/T abnormalities have emerged as a high-risk feature with inherent association with poor cardiovascular outcomes regardless of MPI findings. Although the exact explanation for these findings remains unclear, a potential hypothesis could be that the presence of underlying left ventricular functional and structural abnormalities, such as left ventricular dysfunction, left ventricular dilation, and increased left ventricular mass, causing the secondary ECG changes and increased MACE, irrespective of perfusion abnormalities. Underlying comorbidities, such as hypertension, valvular diseases, cardiomyopathies, and pulmonary diseases, can cause secondary ST/T abnormalities (left ventricular hypertrophy, right ventricular hypertrophy, right bindle branch block). Such patients with underlying structural heart disease are inherently at risk of arrhythmias, among other cardiovascular complications that could account for early cardiac death, irrespective of perfusion abnormalities.11 Left ventricular hypertrophy in particular is an independent strong predictor of cardiovascular mortality.52,53,54,55,56,57 Moreover, many patients with LVH have uncontrolled hypertension,58 a known risk factor of atherosclerosis 59,60,61 which could lead to MI60 and other fatal cardiovascular complications. Considering these concerns, patients with secondary ST/T changes should be managed aggressively with a close clinical follow-up, targeting their underlying heart disease. Notably, among patients with secondary ST/T abnormalities, MPI did not provide incremental prognostic information. It is plausible that the outcome of this subset of patients is determined by underlying myocardial pathology and left ventricular function, irrespective of perfusion abnormality. It is also possible, however, that the study sample size was too small to detect a difference in outcome on the basis of perfusion abnormality (type II error).
Previous studies including Kumar et al.11, Davilgus et al.15, and Badheka et al.16 have demonstrated increased cardiovascular mortality with ST/T abnormalities. However, these studies did not perform separate analyses in different subsets of ST/T changes. We found no association of primary ST abnormalities and isolated T-wave abnormalities with increased risk of cardiac death and MI among patients referred for regadenoson stress MPI. Particularly, patients with isolated T-wave abnormalities had the lowest incidence of MACE among all subsets of ST/T abnormalities. These findings suggest that primary ST and T-wave abnormalities are not inherently associated with an increased risk of MACE, in contrast with secondary ST abnormalities which represent a marker for underlying myocardial disease. A plausible explanation for these findings could be the association of minor ST/T abnormalities with benign factors such as anxiety, emotional stress, change in posture, hyperventilation, food ingestion, use of psychotropic drugs, and electrolyte abnormalities,3,7,62,63,64 or may simply be normal variances. However, an abnormal MPI or presence of myocardial ischemia on regadenoson stress SPECT-MPI in patients with primary ST and T-wave abnormalities correlated with an increased risk of MACE. Therefore, it can be concluded that primary ST and isolated T-wave abnormalities alone should not necessarily prompt stress SPECT-MPI unless additional clinical indication is present. Nonetheless, when a clinically indicated stress SPECT-MPI is performed in these patients, MPI findings do provide valuable prognostic information.
We highlight that our cohort is limited to patients who underwent regadenoson stress and did not include patients who received exercise stress MPI. All patients included were encouraged to perform a non-standardized, low-level leg lifting exercise. Compared to patients undergoing exercise stress MPI, those receiving vasodilator stress tend to be older, more obese, and have a higher prevalence of comorbidities such as known CAD, prior MI, congestive heart failure, diabetes, and hypertension.65,66,67 Therefore, patients undergoing vasodilator stress have higher rates of baseline ECG abnormalities than their counterparts referred for exercise stress. In fact, in our cohort, nearly one-third of the study subjects referred for regadenoson stress MPI had baseline ST/T abnormalities. Given their underlying comorbidities and age, patients who undergo vasodilator stress are at greater risk of adverse cardiac events and mortality than those undergoing exercise stress, regardless of MPI findings.66,68,69 Given the high-risk nature of patients undergoing vasodilator stress and given the high prevalence of ST/T abnormalities among these patients, understanding the prognostic implications these baseline ECG abnormalities and the impact of MPI findings on patients outcomes is highly relevant. Our study helps fill-in this knowledge gap. Nonetheless, it is important to examine the prognostic implications of ST/T abnormalities among lower-risk patients undergoing exercise stress MPI.
Limitations
This study has several limitations. First, this was a single-center, observational, retrospective study which may have led to some selection and confounding biases. Second, a single baseline ECG was used for this study, and therefore, any subsequent changes on follow-up were not accounted for. Third, there could be variation in the technique and interpretation of ECG tracings. Fourth, the study was limited to patients undergoing regadenoson stress MPI; and thus, the results may not be generalizable to patients undergoing exercise stress MPI. Lastly, the cause of death in some patients was determined using death certificates which may be inaccurate.
New Knowledge Gained
Our study demonstrated that ST/T abnormalities are common among patients referred for regadenoson stress MPI. Among ST/T abnormalities, only secondary ST/T abnormalities are associated with an increased risk of MACE, regardless of perfusion abnormalities on stress SPECT-MPI. Among patients undergoing regadenoson stress MPI, primary ST abnormalities and isolated T-wave abnormalities are not associated with increased risk of MACE compared to normal ECG. Future studies with larger cohorts, other stress modalities, and multi-center prospective design are warranted to validate prognostication among different subsets of ST/T abnormalities and identify patients who may benefit from additional risk stratification and MPI guided management.
Conclusion
ST/T abnormalities are common among patients referred for regadenoson stress MPI. While secondary ST/T abnormalities are associated with significantly higher incidence of MACE, abnormal MPI or presence of ischemia on regadenoson stress SPECT-MPI does not add prognostic information in this group. Patients with primary ST changes or T-wave abnormalities do not seem to have a higher MACE risk compared with patients with normal ECG. However, abnormal MPI or presence of ischemia in these patients correlates with a higher incidence of MACE.
Abbreviations
- CAD:
-
Coronary Artery Disease
- ST/T:
-
ST-segment and T-wave
- LVEF:
-
Left ventricular ejection fraction
- MACE:
-
Major adverse cardiovascular events
- MPI:
-
Myocardial Perfusion Imaging
- MI:
-
Myocardial Infarction
- SDS:
-
Summed difference scores
- SRS:
-
Summed rest scores
- SSS:
-
Summed stress scores
- TID:
-
Transient ischemic dilation
References
Rose G, Baxter PJ, Reid DD, McCartney P. Prevalence and prognosis of electrocardiographic findings in middle-aged men. Br Heart J 1978;40(6):636-43.
Lee TH, Goldman L. Evaluation of the patient with acute chest pain. N Engl J Med 2000;342(16):1187-95.
Conti A, Mariannini Y, Canuti E, Petrova T, Innocenti F, Zanobetti M, et al. Nuclear scan strategy and outcomes in chest pain patients value of stress testing with dipyridamole or adenosine. World J Nucl Med 2014;13(2):94-101.
Reunanen A, Pyorala K, Punsar S, Aromaa A. Predictive value of ECG findings with respect to coronary heart disease mortality. Adv Cardiol 1978;21:310-2.
Ostor E, Schnohr P, Jensen G, Nyboe J, Hansen AT. Electrocardiographic findings and their association with mortality in the Copenhagen City Heart Study. Eur Heart J 1981;2(4):317-28.
Knutsen R, Knutsen SF, Curb JD, Reed DM, Kautz JA, Yano K. The predictive value of resting electrocardiograms for 12-year incidence of coronary heart disease in the Honolulu Heart Program. J Clin Epidemiol 1988;41(3):293-302.
Cullen K, Stenhouse NS, Wearne KL, Cumpston GN. Electrocardiograms and 13 year cardiovascular mortality in Busselton study. Br Heart J 1982;47(3):209-12.
Bartel A, Heyden S, Tyroler HA, Tabesh E, Cassel JC, Hames CG. Electrocardiographic predictors of coronary heart disease. Arch Intern Med 1971;128(6):929-37.
Ungerleider HE. The prognostic implications of the electrocardiogram. Am J Cardiol 1960;6:35-44.
Prineas RJ, Grandits G, Rautaharju PM, Cohen JD, Zhang ZM, Crow RS. Long-term prognostic significance of isolated minor electrocardiographic T-wave abnormalities in middle-aged men free of clinical cardiovascular disease (The Multiple Risk Factor Intervention Trial [MRFIT]). Am J Cardiol 2002;90(12):1391-5.
Kumar A, Prineas RJ, Arnold AM, Psaty BM, Furberg CD, Robbins J, et al. Prevalence, prognosis, and implications of isolated minor nonspecific ST-segment and T-wave abnormalities in older adults: Cardiovascular Health Study. Circulation 2008;118(25):2790-6.
Kiessling CE, Schaaf RS, Lyle AM. A study of t wave changes in the electrocardiograms of normal individuals. Am J Cardiol 1964;13:598-602.
Harlan WR Jr, Graybiel A, Mitchell RE, Oberman A, Osborne RK. Serial electrocardiograms: their reliability and prognostic validity during a 24-yr. period. J Chronic Dis 1967;20(11):853-67.
Greenland P, Xie X, Liu K, Colangelo L, Liao Y, Daviglus ML, et al. Impact of minor electrocardiographic ST-segment and/or T-wave abnormalities on cardiovascular mortality during long-term follow-up. Am J Cardiol 2003;91(9):1068-74.
Daviglus ML, Liao Y, Greenland P, Dyer AR, Liu K, Xie X, et al. Association of nonspecific minor ST-T abnormalities with cardiovascular mortality: The Chicago Western Electric Study. JAMA 1999;281(6):530-6.
Badheka AO, Rathod A, Marzouka GR, Patel N, Bokhari SS, Moscucci M, et al. Isolated nonspecific ST-segment and T-wave abnormalities in a cross-sectional United States population and Mortality (from NHANES III). Am J Cardiol 2012;110(4):521-5.
Higgins IT, Kannel WB, Dawber TR. The electrocardiogram in epidemiological studies: Reproducibility, validity, and international comparison. Br J Prev Soc Med 1965;19:53-68.
Doukky R, Nigatu A, Khan R, Anokwute C, Fughhi I, Ayoub A, et al. Prognostic significance of ischemic electrocardiographic changes with regadenoson stress myocardial perfusion imaging. J Nucl Cardiol. 2018. https://doi.org/10.1007/s12350-018-1415-4.
Doukky R, Calvin JE. Risk stratification in patients with unstable angina and non-ST segment elevation myocardial infarction: evidence-based review. J Invasive Cardiol 2002;14(4):215-20.
Doukky R, Calvin JE. Part II: risk stratification in patients with unstable angina and non-ST segment elevation myocardial infarction: evidence-based review. J Invasive Cardiol 2002;14(5):254-62.
Rautaharju PM, Surawicz B, Gettes LS, Bailey JJ, Childers R, Deal BJ, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2009;53(11):982-91.
Tilkemeier PL, Bourque J, Doukky R, Sanghani R, Weinberg RL. ASNC imaging guidelines for nuclear cardiology procedures : Standardized reporting of nuclear cardiology procedures. J Nucl Cardiol 2017;24(6):2064-128.
Henzlova MJ, Duvall WL, Einstein AJ, Travin MI, Verberne HJ. ASNC imaging guidelines for SPECT nuclear cardiology procedures: Stress, protocols, and tracers. J Nucl Cardiol 2016;23(3):606-39.
Doukky R, Nigatu A, Khan R, Anokwute C, Fughhi I, Ayoub A, et al. Prognostic significance of ischemic electrocardiographic changes with regadenoson stress myocardial perfusion imaging. J Nucl Cardiol 2018. https://doi.org/10.1007/s12350-014-0047-6.
Iskander F, Iskander M, Gomez J, Doukky R. Prognostic value of regadenoson stress myocardial perfusion imaging in patients with left bundle branch block or ventricular paced rhythm. J Nucl Cardiol. 2019. https://doi.org/10.1007/s12350-019-01762-4.
Chawla D, Rahaby M, Amin AP, Vashistha R, Alyousef T, Martinez HX, et al. Soft tissue attenuation patterns in stress myocardial perfusion SPECT images: A comparison between supine and upright acquisition systems. J Nucl Cardiol 2011;18(2):281-90.
Ballany W, Mansour K, Morales Demori R, Al-Amoodi M, Doukky R. The impact of regimented aminophylline use on extracardiac radioisotope activity in patients undergoing regadenoson stress SPECT myocardial perfusion imaging: A substudy of the ASSUAGE trial. J Nucl Cardiol 2014;21(3):496-502.
Ficaro EP, Lee BC, Kritzman JN, Corbett JR. Corridor4DM: The Michigan method for quantitative nuclear cardiology. J Nucl Cardiol 2007;14(4):455-65.
Doukky R, Hayes K, Frogge N, Balakrishnan G, Dontaraju VS, Rangel MO, et al. Impact of appropriate use on the prognostic value of single-photon emission computed tomography myocardial perfusion imaging. Circulation 2013;128(15):1634-43.
Doukky R, Fughhi I, Campagnoli T, Wassouf M, Ali A. The prognostic value of regadenoson SPECT myocardial perfusion imaging in patients with end-stage renal disease. J Nucl Cardiol 2017;24(1):112-8.
Doukky R, Frogge N, Bayissa YA, Balakrishnan G, Skelton JM, Confer K, et al. The prognostic value of transient ischemic dilatation with otherwise normal SPECT myocardial perfusion imaging: A cautionary note in patients with diabetes and coronary artery disease. J Nucl Cardiol 2013;20(5):774-84.
Golzar Y, Olusanya A, Pe N, Dua SG, Golzar J, Gidea C, et al. The significance of automatically measured transient ischemic dilation in identifying severe and extensive coronary artery disease in regadenoson, single-isotope technetium-99 m myocardial perfusion SPECT. J Nucl Cardiol 2015;22(3):526-34.
Gomez J, Golzar Y, Fughhi I, Olusanya A, Doukky R. The significance of post-stress decrease in left ventricular ejection fraction in patients undergoing regadenoson stress gated SPECT myocardial perfusion imaging. J Nucl Cardiol 2018;25(4):1313-23.
Doukky R, Morales Demori R, Jain S, Kiriakos R, Mwansa V, Calvin JE. Attenuation of the side effect profile of regadenoson: A randomized double-blinded placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging. “The ASSUAGE trial”. J Nucl Cardiol 2012;19(3):448-57.
Doukky R, Rangel MO, Dick R, Wassouf M, Alqaid A, Margeta B. Attenuation of the side effect profile of regadenoson: A randomized double-blind placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging and have severe chronic kidney disease-the ASSUAGE-CKD trial. Int J Cardiovasc Imaging 2013;29(5):1029-37.
Doukky R, Rangel MO, Wassouf M, Dick R, Alqaid A, Morales Demori R. The safety and tolerability of regadenoson in patients with end-stage renal disease: The first prospective evaluation. J Nucl Cardiol 2013;20(2):205-13.
Vij A, Golzar Y, Doukky R. Regadenoson use in chronic kidney disease and end-stage renal disease: A focused review. J Nucl Cardiol 2018;25(1):137-49.
Golzar Y, Doukky R. Regadenoson use in patients with chronic obstructive pulmonary disease: The state of current knowledge. Int J Chron Obstruct Pulmon Dis 2014;9:129-37.
Hage FG, Ghimire G, Lester D, McKay J, Bleich S, El-Hajj S, et al. The prognostic value of regadenoson myocardial perfusion imaging. J Nucl Cardiol 2015;22(6):1214-21.
Kattoor AJ, Kolkailah AA, Iskander F, Iskander M, Diep L, Khan R, et al. The prognostic value of regadenoson SPECT myocardial perfusion imaging: The largest cohort to date. J Nucl Cardiol. 2020. https://doi.org/10.1007/s12350-020-02135-y.
Farzaneh-Far A, Shaw LK, Dunning A, Oldan JD, O’Connor CM, Borges-Neto S. Comparison of the prognostic value of regadenoson and adenosine myocardial perfusion imaging. J Nucl Cardiol 2015;22(4):600-7.
Kolkailah AA, Iskander M, Iskander F, Patel PP, Khan R, Doukky R. The prognostic utility of regadenoson SPECT myocardial perfusion imaging in patients with end-stage renal disease: The largest cohort to date. J Nucl Cardiol. 2020. https://doi.org/10.1007/s12350-020-02259-1.
Doukky R, Fughhi I, Campagnoli T, Wassouf M, Kharouta M, Vij A, et al. Validation of a clinical pathway to assess asymptomatic renal transplant candidates using myocardial perfusion imaging. J Nucl Cardiol 2018;25(6):2058-68.
Golzar Y, Doukky R. Stress SPECT myocardial perfusion imaging in end-stage renal disease. Curr Cardiovasc Imaging Rep 2017;10(5):1-13.
Parikh K, Appis A, Doukky R. Cardiac imaging for the assessment of patients being evaluated for kidney or liver transplantation. J Nucl Cardiol 2015;22(2):282-96.
Kassab K, Hussain K, Torres A, Iskander F, Iskander M, Khan R, et al. The diagnostic and prognostic value of near normal perfusion or borderline ischemia on stress myocardial perfusion imaging. J Nucl Cardiol. 2020. https://doi.org/10.1007/s12350-020-02375-y.
Lester D, El-Hajj S, Farag AA, Bhambhvani P, Tauxe L, Heo J, et al. Prognostic value of transient ischemic dilation with regadenoson myocardial perfusion imaging. J Nucl Cardiol 2016;23(5):1147-55.
Doukky R, Olusanya A, Vashistha R, Saini A, Fughhi I, Mansour K, et al. Diagnostic and prognostic significance of ischemic electrocardiographic changes with regadenoson-stress myocardial perfusion imaging. J Nucl Cardiol 2015;22(4):700-13.
AlJaroudi W, Anokwute C, Fughhi I, Campagnoli T, Wassouf M, Vij A, et al. The prognostic value of heart rate response during vasodilator stress myocardial perfusion imaging in patients with end-stage renal disease undergoing renal transplantation. J Nucl Cardiol 2019;26(3):814-22.
AlJaroudi W, Campagnoli T, Fughhi I, Wassouf M, Ali A, Doukky R. Prognostic value of heart rate response during regadenoson stress myocardial perfusion imaging in patients with end stage renal disease. J Nucl Cardiol 2016;23(3):560-9.
Gomez J, Fughhi I, Campagnoli T, Ali A, Doukky R. Impact of integrating heart rate response with perfusion imaging on the prognostic value of regadenoson SPECT myocardial perfusion imaging in patients with end-stage renal disease. J Nucl Cardiol 2017;24(5):1666-71.
Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Left ventricular mass and incidence of coronary heart disease in an elderly cohort. The Framingham Heart Study. Ann Intern Med 1989;110(2):101-7.
Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med 1990;322(22):1561-6.
Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med 1991;114(5):345-52.
Kannel WB, Dannenberg AL, Levy D. Population implications of electrocardiographic left ventricular hypertrophy. Am J Cardiol 1987;60(17):85i-93i.
Desai CS, Bartz TM, Gottdiener JS, Lloyd-Jones DM, Gardin JM. Usefulness of left ventricular mass and geometry for determining 10-year prediction of cardiovascular disease in adults aged > 65 years (from the Cardiovascular Health Study). Am J Cardiol 2016;118(5):684-90.
Aronow WS. Hypertension and left ventricular hypertrophy. Ann Transl Med 2017;5(15):310.
Drazner MH. The progression of hypertensive heart disease. Circulation 2011;123(3):327-34.
Hollander W. Role of hypertension in atherosclerosis and cardiovascular disease. Am J Cardiol 1976;38(6):786-800.
Frostegård J. Immunity, atherosclerosis and cardiovascular disease. BMC Med 2013;11(1):117.
Alexander RW. Theodore Cooper Memorial Lecture. Hypertension and the pathogenesis of atherosclerosis. Oxidative stress and the mediation of arterial inflammatory response: a new perspective. Hypertension 1995;25(2):155-61.
Taggart P, Carruthers M, Somerville W. Electrocardiogram, plasma catecholamines and lipids, and their modification by oxyprenolol when speaking before an audience. Lancet 1973;2(7825):341-6.
Kemp GL, Ellestad MH. The significance of hyperventilative and orthostatic T-wave changes on the electrocardiogram. Arch Intern Med 1968;121(6):518-23.
Guazzi M, Fiorentini C, Polese A, Magrini F, Olivari MT. Stress-induced and sympathetically-mediated electrocardiographic and circulatory variations in the primary hyperkinetic heart syndrome. Cardiovasc Res 1975;9(3):342-54.
Gonzalez JA, Beller GA. Choosing exercise or pharmacologic stress imaging, or exercise ECG testing alone: How to decide. J Nucl Cardiol 2017;24(2):555-7.
Poulin MF, Alexander S, Doukky R. Prognostic implications of stress modality on mortality risk and cause of death in patients undergoing office-based SPECT myocardial perfusion imaging. J Nucl Cardiol 2016;23(2):202-11.
Kassab K, Kattoor AJ, Doukky R. Ischemia and viability testing in new-onset heart failure. Curr Cardiol Rep 2020;22(8):76.
Navare SM, Mather JF, Shaw LJ, Fowler MS, Heller GV. Comparison of risk stratification with pharmacologic and exercise stress myocardial perfusion imaging: a meta-analysis. J Nucl Cardiol 2004;11(5):551-61.
Hachamovitch R, Kang X, Amanullah AM, Abidov A, Hayes SW, Friedman JD, et al. Prognostic implications of myocardial perfusion single-photon emission computed tomography in the elderly. Circulation 2009;120(22):2197-206.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The study was funded, in part, by Astellas Pharma Global Development (Northbrook, IL). The funding source had no input in the study design, execution, data analysis and interpretation, or manuscript preparation and approval. The authors have no conflicts to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
The authors have also provided an audio summary of the article, which is available to download as ESM, or to listen to via the JNC/ASNC Podcast.
Funding
The study was funded, in part, by Astellas Pharma Global Development (Northbrook, IL). The funding source had no input in the study design, execution, data analysis and interpretation, or manuscript preparation and approval.
Tweet
Baseline ST/T abnormalities have significant prognostic implications. #Regadenoson #MPI provides additional risk stratification. @RamiDoukky @ShahzebKhanMD @CookCtyHealth @RushMedical #CVNuc @JNCjournal @MyASNC.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Khan, M.S., Arif, A.W. & Doukky, R. The prognostic implications of ST-segment and T-wave abnormalities in patients undergoing regadenoson stress SPECT myocardial perfusion imaging. J. Nucl. Cardiol. 29, 810–821 (2022). https://doi.org/10.1007/s12350-020-02382-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-020-02382-z