Abstract
Background
Asynchrony has been reported to be a marker of ischemic-induced left ventricular dysfunction, the magnitude of which correlates with extent of epicardial coronary disease. We wished to determine whether normal-appearing arterial territories with mild degrees of asynchrony have lower 82Rb PET absolute myocardial blood flow (MBF) and/or lower myocardial flow reserve (MFR).
Methods and Results
Data were examined retrospectively for 105 patients evaluated for known/suspected CAD who underwent rest/regadenoson-stress 82Rb PET/CT and quantitative coronary angiography. Rest and stress absolute MBF and MFR were quantified from first-pass 82Rb PET curves. Regional relative myocardial perfusion summed stress score (SSS), summed rest score (SRS), regional phase bandwidth (BW), and regional semi-quantitative asynchrony visual scores of (Asynch) were assessed. We found that in apparently normal arteries (SSS < 4, SRS < 4 and stenosis < 70%), those with abnormally low MFR < 2.0 compared to those with MFR ≥ 2.0 had larger phase BW (186 ± 79° vs 158 ± 67°, P = .02), and more visually apparent Asynch (5.7 ± 4.2 vs 3.9 ± 3.6, P = .02), which was associated with increasing stenosis values (ρ = 0.44, P < .0001).
Conclusion
A subgroup of coronary territories with normal relative perfusion and normal or non-obstructive coronary disease may have reduced MFR, which is signaled physiologically by a mild degree of left ventricular asynchrony.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
PET/CT pharmacologic stress myocardial perfusion imaging is a highly effective technology for diagnosing hemodynamically significant obstructive coronary disease (CAD).1 CAD can be identified by qualitative evaluation of relative tracer uptake or comparison to a known database.2 PET accuracy is improved by using quantified rest and stress absolute myocardial blood flow (MBF) and myocardial flow reserve (MFR = stress MBF/rest MBF).3
In studies of PET accuracy, x-ray contrast arteriography is often the accepted reference standard, defined as per cent luminal stenosis. Coronary arteries are considered abnormal and flow-limited for stenosis ≥ 70%. However, lesser degrees of discrete epicardial stenosis may be associated with abnormal regional flow and wall motion abnormalities,4 due to obstruction at three other anatomic levels: (1) diffuse non-critical epicardial coronary stenoses; (2) microvascular coronary disease, affecting arterioles below the level of angiographic resolution; and (3) endothelial dysfunction in the production of local vasodilators such as nitric oxide and impairment in sympathetic innervation.5 Coronary microvascular disease and endothelial dysfunction may reduce blood flow, manifested by reduced MFR, and produce wall motion abnormalities and ventricular dysfunction.6
An “ischemic cascade” or constellation of sequential cardiac mechanical events has been postulated to occur in response to ischemia resulting from oxygen supply/demand imbalance, including altered diastolic and systolic function, ECG changes, and angina.7 Since oxygen extraction by myocardium is near maximal at rest, metabolic alterations must derive from inadequate coronary blood flow.5 Left ventricular (LV) asynchrony is an additional marker of ischemic-induced LV dysfunction,8 and the magnitude of asynchrony induced by pharmacologic stress correlates directly with extent of epicardial coronary disease.9 Decreasing regional MBF and MFR induces progressively more pronounced asynchrony.10
There has been increased recognition that myocardial perfusion imaging studies with minimal heterogeneity, previously interpreted as normal, may be associated with major adverse acute coronary events during long-term follow-up.11 Events may occur even with summed stress score (SSS) < 4 or low scores for total perfusion deficit.12 Quantitation of flow in such patients may be helpful in elucidating their risk.13
The hypothesis of this investigation is that subtle abnormalities of ventricular function, primarily manifest as abnormal LV synchrony, serve as an early identifier of ischemic LV dysfunction. Asynchrony might be detected even when LV relative perfusion scores are within accepted normal limits, and rigorous anatomic angiographic analysis reveals only subcritical coronary stenosis. We wished to determine whether normal-appearing arterial territories with mild degrees of asynchrony have lower MBF and/or lower MFR.
Materials and Methods
Patients
We conducted a retrospective investigation of an unselected population of patients who were evaluated between 1/1/2010 and 12/31/2016 for known/suspected CAD. Data of 105 patients (age 69 ± 13 years; 42 females; 63 males) were analyzed. All patients had coronary arteriography that was technically adequate for quantitation, and 82Rb rest and regadenoson-stress PET studies with determination of MBF. Mean time difference between PET and angiography was 138 ± 388 days, with no cardiac events (e.g., PCI or MI) between PET and angiography. 39% of patients had a history of PCI, 22% had a history of MI, and 24% had a history of CABG.
The Institutional Review Board approved this retrospective study and the requirement to obtain informed consent was waived. All data were handled in compliance with the Health Insurance Portability and Accountability Act of 1996.
Angiography
Digital cines were reviewed by expert angiographers at a core laboratory (Boston Clinical Research Institute, BCRI, Boston, MA), who quantified stenosis by planimetry using “PlusPlus” software (Sanders Data Systems, Palo Alto, CA). Arteries with at least a 20% stenosis were quantified as to exact percent stenosis. Lesions in vessels < 2.0 mm in diameter were not assessed unless the lesion was in a vascular segment that was the primary conduit of circulation for any myocardial wall/segment, or if the artery segments would be ≥ 2.0 mm in diameter if fully perfused.
For each patient, the three major coronary arterial territories (LAD, LCX, and RCA) were given a score based on the most severe stenosis in the major artery in that territory. In cases in which more than one lesion was identified in a territory, the value of the stenosis of the most severe lesion was recorded. For each territory in which there was no stenosis of ≥ 20% visualized, a value of 0% stenosis was adopted.
PET Data Collection
The PET data acquisition protocol followed standard published guidelines.14 As the pharmacologic testing agent was regadenoson, patient preparation included the standard recommended duration of fasting, abstention from caffeine, and withholding of cardiac medications.15 At rest, 0.94-1.22 GBq (35-45 mCi) of 82Rb was infused from a strontium-rubidium generator over 20-30 seconds. At peak pharmacologic stress 50-60 seconds following initiation of regadenoson injection, a similar activity was injected over approximately 20–30 seconds.16 Blood pressure, heart rate, and cardiac rhythm were monitored and recorded throughout imaging and pharmacologic testing. PET/CT studies were acquired on a GE Discovery VCT 64 PET/CT in 2D mode (N = 74) or on a GE D710 PET/CT 64-slice CT system in 3D mode (N = 31). Data acquired in 3D mode were corrected for prompt gamma rays.17
All data were acquired in gated list mode and reconstructed by OSEM (20 subsets; 2 iterations; z-axis filter = “standard”; post-filter = 2.57 mm FWHM), as recommended by the manufacturer. Attenuation correction of tomograms was performed as part of iterative image reconstruction using CT data. First-pass data subsequently were re-binned as 20 3-second frames, 5 12-second frames, and 7 30-second frames. From the equilibrium phase of the study, myocardial perfusion portions of data were re-binned as gated tomograms at 8 frames/R-R interval, with non-gated equilibrium images formed by summing the gated tomograms.
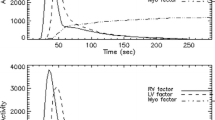
Regional Myocardial Perfusion Computation
Semi-automated software (Emory Cardiac Toolbox, “ECTb,” Emory University, Atlanta, GA) computed MBF from dynamic first-pass data.18 A 1-tissue compartment, 1 rate constant (microsphere analog) model with spillover effects described tracer uptake in myocardial tissue. Algorithms automatically identified blood pool and myocardial tissue voxels. Curves sampled at blood pool locations were corrected for myocardial activity “spill over” caused by LV contraction, respiration, and imperfect spatial resolution. Rest and stress MBF and MFR values were obtained for each of the three main arterial territories. MFR < 2.0 was considered abnormal.19
From equilibrium data, rest and stress LVEF and volumes were calculated using ECTb. These algorithms also applied 82Rb-specific normal limits to equilibrium images to obtain LV relative perfusion scores for perfusion polar maps for three main arterial territories, including SSS, summed rest scores (SRS), and summed difference scores (SDS) generated by an artificial intelligence-driven approach.20
Apparently normal arteries were defined by conventional criteria as those with territorial SRS < 4 and territorial SSS < 4 and stenosis < 70%.
Coronary territories were then assigned to one of the three following classes: (Artery Class1) apparently normal arteries with low relative perfusion scores (SSS and SRS < 4) and insignificant 0%-20% stenosis; (Artery Class2) apparently normal arteries with low relative perfusion scores (SSS and SRS < 4) and with 20%-69% stenosis; (Artery Class3) arteries with significant stenosis: ≥ 70% stenosis.
Regional LV Wall Thickening Computation
ECTb algorithms reported wall thickening (WT) abnormality values ranging from 0 (normal) to 4 (most severe) in each of the 17 segments of LV WT polar maps. WT was quantified for rest and stress for each of the 3 major territories by summing all of the non-zero scores within those territories.
Regional LV Bandwidth Computations
Rest and stress systolic and diastolic phase parameters and visual displays were computed from equilibrium gated tomograms (ECTb SyncTool).21 Phase histograms depicting frequency of occurrence of contractions at each phase of the R-R interval were color coded to polar maps displaying the phase at which maximum contraction occurred (Figures 1A and 1B). Similar phase histograms and polar maps were generated for regional diastolic relaxation (Figures 1C and 1D). SyncTool algorithms reported only global values of phase standard deviation and phase bandwidth (BW), which quantifies the amount of the R-R interval over which 95% of systolic contractions and 95% of diastolic relaxations occur. To obtain territorial values of these parameters, algorithms were written in IDL V 8.2 to analyze polar maps converted to jpg files. Each pixel was scaled from a minimum of 0 to a maximum of 360 to span the range of angles and tabulated in one of 3 arrays to correspond to the locations in the map that corresponded to the 3 main territories, with locations defined in the same way as the indicated boundaries that are routinely displayed on polar maps of relative perfusion and MBF.
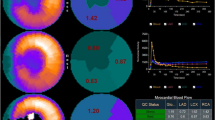
Systolic contraction phase polar maps and phase histograms at rest (A) and stress (B) and diastolic relaxation phase polar maps and phase histograms at rest (C) and stress (D) for a patient with LAD, LCX, and RCA stenosis < 20%, regional SSS of 0, 0, and 0, regional SRS of 0, 0, and 0, regional MFR of 3.8, 3.7, and 3.7, regional visual asynchrony scores of 0, 0, and 0, and regional phase BW values of 79°, 66°, and 66°
Regional LV Visual Asynchrony Analysis
Visual asynchrony scoring of coronary territories was performed using a method previously described by our laboratory.22 A medical imaging physicist and a cardiologist independently graded regional asynchrony on a 5-point scale while viewing rest and stress systolic and diastolic phase histograms and polar maps. The lowest score (0 = “normal”) was assigned to a territory if rest and stress systolic phase histograms were narrow peaks centered near 1/3 R-R, and diastolic phase histograms were narrow peaks centered near 2/3 R-R, along with rest and stress phase maps displaying uniform contraction throughout that territory. The highest score (4 = “markedly asynchronous extensive territory”) was assigned to a territory if phase histograms were broad or scattered and corresponded to a large % of contractions occurring out of phase for a large extent of that territory. For each reader, a composite value of visual regional phase asynchrony (Asynch) was formed, generated by summing all systolic and diastolic rest and stress visual territorial scores, for which the highest possible value was 16 per territory. All scoring was performed by both readers without access to other clinical or computed information. The purpose of defining the semi-quantitative visual Asynch parameter in this way was to quantify observers’ perceptions of unusual-appearing patterns in systolic or diastolic, rest or stress phase relationships while viewing phase polar maps and phase histograms generated by the ECTb algorithms. Examples in which anomalies sometimes are even more striking in diastolic relaxation than in systolic contraction phase maps and phase histograms illustrate the reason that we summed visual scores for all four phase types of systolic, diastolic, rest, and stress visual scores (Figure 2).
Systolic contraction phase polar maps and phase histograms at rest (A) and stress (B) and diastolic relaxation phase polar maps and phase histograms at rest (C) and stress (D) for a patient with LAD, LCX, and RCA stenosis of 48%, 42%, and 0%, regional SSS of 0, 0, and 0, regional SRS of 0, 0, and 0, regional MFR of 1.29, 2.29, and 2.08, regional composite visual asynchrony scores of 10, 9, and 10, and regional composite BW values of 177°, 227°, and 187°
Statistical Analysis
Analyses were performed using “MedCalc” commercially available statistical analysis software.23 Values are reported as means ± one standard deviation. Continuous variables were assessed by the χ2 test to determine normality of distribution. ANOVA assessed whether there were differences among continuous variables by artery class, and assessed whether there were differences among continuous variables, and automatically applied Bonferroni corrections for comparisons among multiple categories. The unpaired or paired t test, as appropriate, compared values between groups for continuous variables that were normally distributed; otherwise, the Mann-Whitney or Wilcoxon test was used. χ2 Analysis of proportions compared ratios. Linear regression determined whether there were significant associations among continuous variables, for which Pearson correlation coefficients (r) were generated. Rank correlation determined strength of association between continuous and discrete variables, for which Spearman’s correlation coefficients (ρ) were generated. Inter-observer agreement for Asynch scores was assessed by the χ2 test for contingency tables. For all tests, probability (P) < .05 was defined as statistically significant, or as adjusted by Bonferroni corrections.
Results
Coronary Artery Classification
315 Coronary arterial territories were assessed for the 105 patients. There were 174 arteries with undetectable stenosis (stenosis < 20%), 72 arteries with 25%-69% stenosis, and 69 arteries with 70%-100% stenosis. Thus, there were 246 arteries with stenosis < 70%. Including relative perfusion considerations (SSS < 4 and SRS < 4), by conventional criteria there were 122 Class1 arteries with low relative perfusion scores and 0%-20% stenosis, 56 Class2 arteries with low relative perfusion scores and stenoses ranging from 25% to 69%, and 69 Class3 arteries with low relative perfusion scores and significant stenoses ranging from 70% to 100%.
Mean QRS duration was 0.11 ± 0.03 seconds, and there were no QRS duration differences among artery classes (P = .13).
Regional Myocardial Perfusion
Rest MBF was higher for apparently normal arteries than abnormal arteries (0.86 ± 0.59 vs 0.77 ± 0.38, P < .001), as was stress MBF (2.03 ± 1.23 vs 1.29 ± 0.84, P < .001), so that regional MFR was higher for apparently normal than abnormal arteries (2.54 ± 1.18 vs 1.79 ± 1.13, P < .001). Nonetheless, 35% (63/178) of apparently normal arteries had territorial MFR below 2.00. Those arteries had a mean MFR value of 1.58 ± 0.27, for which the minimum was 0.98 (Table 1). Despite having normal relative perfusion scores, and similar quantified stenosis values, apparently normal arteries with MFR < 2.00 had lower stress MBF, larger phase BW (186 ± 79° vs 158 ± 67°, P = .02), and a larger Asynch score (5.7 ± 4.2 vs 3.9 ± 3.6, P = .02), compared to apparently normal arteries with MFR ≥ 2.00. WT scores did not differ between the groups (Table 1).
Regional LV Function
Regarding visual Asynch scores, there was good agreement between the two readers (χ2 = 334.8, P < .0001), with contingency coefficient = 0.72 (P < . 001).
In quantifying regional phase parameters, the mean number of pixels sampled per arterial territory was 4,732 ± 847, consistent with 128 transaxial sections having been reconstructed as 128 × 128 matrices, so that the numbers of sampled polar map phase values per territory were on the order of 128 × 128/3. Regional phase standard deviation reflected regional territorial phase BW so closely that only BW values were further analyzed (r = .97).
Table 2 compares apparently normal arteries with stenosis 0%-20% to those with stenosis of 20%-69%. Relative perfusion scores, MFR and WT were similar between the two groups. Regional phase BW was lower in apparently normal arteries with < 20% stenosis compared to 20%-69% stenosis (158 ± 71° vs 182 ± 72°, P = .02), as were visual Asynch scores (3.9 ± 3.7 vs 5.9 ± 4.3, P = .002, Figure 3; Table 2). Regional Asynch scores had significant rank correlation with regional BW (ρ = 0.74, P < .0001). Of all variables tested, Asynch scores correlated most strongly with continuous values of stenosis (ρ = 0.44, P < .0001).
Blood Flow in Apparently Normal Arteries
Considering only apparently normal arteries, ROC analysis of Asynch and BW values to discriminate between arteries with stenosis values ≥ 20% (Figure 2) from those arteries judged to have no recognizable stenosis (Figure 1) yielded threshold values of Asynch > 6 and BW > 165°. Using these as the discrimination thresholds, both resting MBF and stress MBF were significantly higher for Asynch ≤ 6 vs those with Asynch > 6, and for BW ≤ 165° vs BW > 165°, and stenosis was less, despite similar regional MFR (Table 3). Relative perfusion measures were similar for these Asynch and BW categories (Table 3), which was predictable considering that our definitions of apparently normal arteries were those with SRS < 4 and territorial SSS < 4 and stenosis < 70%.
Discussion
The goal of this research was to determine whether pharmacologic stress-induced mild LV dysfunction, manifest as either wall thickening abnormalities or asynchrony, might identify an ischemic response in patients with non-critical coronary stenosis, but who might have diffuse non-obstructive or microvascular CAD. Our findings indicate that in coronary arterial territories with normal relative qualitative perfusion, a previously described index of LV asynchrony22 was significantly increased (greater asynchrony) in coronary artery territories with reduced stress myocardial blood flow and reduced flow reserve. Worsened asynchrony was more likely in arteries with an average stenosis of 20%-69% (mean 47%) than 0%-20%. LV systolic dysfunction, assessed by wall thickening index, did not appear to discriminate between arteries with a lower flow reserve (< 2.0) or between the two levels of subcritical coronary stenosis.
Stress-induced changes in asynchrony have been used increasingly to identify ischemic heart disease and quantify its extent. While pharmacologic stress reduces asynchrony in normal subjects,24 more recently it has been demonstrated that stress-induced asynchrony differentiates ischemic vs non-ischemic cardiomyopathy,8 and that degree of asynchrony correlates with extent of CAD.9 A prior study in patients with normal PET MPI scans showed that systolic asynchrony improved with stress in groups with normal or severely abnormal overall LV function, despite their having a significant prevalence of CAD.25 However, coronary anatomy was not described in that work, and diastolic asynchrony was not evaluated, as in the current study. Other studies have shown that increasing degrees of asynchrony identify multi-vessel CAD on SPECT MPI,9 suggesting that asynchrony should be related to blood flow.13 Our study used stress-induced asynchrony to attempt to distinguish coronaries with modest degrees of non-critical obstruction from those without. Our results indicate that mild degrees of worsening asynchrony may serve as a marker of territories with early ischemia despite normal qualitative perfusion.
MFR reflects total resistance across the coronary vasculature.26 The anatomic level giving rise to pharmacologic stress-induced mild ischemic LV asynchrony in our patients cannot be precisely defined. The fact that asynchrony was associated with MFR < 2.0 and mean coronary stenosis of 47% suggests that it may arise from diffuse non-obstructive CAD, with diffuse luminal narrowing. Base-to-apex perfusion gradients characteristic of non-obstructive arterial narrowing may co-exist with other regions of severe epicardial stenosis.27 Alternatively, mild ischemia may arise in the microvasculature, the coronary pre-arterioles, and arterioles (< 100-400 µm) which provide a large portion of overall coronary resistance.28 These vessels normally auto-regulate to maintain myocardial blood supply. Disease states, such as diabetes and hypertension that may cause arteriolar remodeling, impede autoregulation leading to local myocardial hypoxia. Endothelial dysfunction, through inhibition of vasodilating mediators such as nitric oxide, can reduce local oxygen delivery leading to ischemia. Pathophysiologic changes at any or all of these anatomic levels may cause ischemia and LV asynchrony in the absence of an identifiable “critical stenosis” in the epicardial vasculature.
A scan showing normal relative myocardial perfusion is felt to confer a good long-term prognosis. However, patients with normal scans may have a significant event rate. For PET, an MFR value < 2.0 identifies a group of patients with normal-appearing perfusion imaging who are at increased risk for MACE.29 For SPECT imaging, the REFINE-SPECT study reviewed scans and events (4.5 years of follow-up) in nearly 20,000 patients.12 A normal scan, or a SSS = 0, conferred a 1.3%-2.0% MACE rate. In our study, normal relative perfusion, with mild worsening of asynchrony was associated with MFR < 2.0, and non-obstructive CAD which was more advanced. Whether mild stress-induced asynchrony can help further categorize the risk for events in patients with normal perfusion scans will require further study.
Limitations
Our study is limited by a restricted number of patients, but has the advantage of studying a population selected only on the basis of having technically adequate PET imaging and angiograms. Other investigations that combined PET MPI and angiography included larger populations,30 but relied on qualitative analysis of angiograms, rather than the detailed quantitative analysis used in the present study. It also would have been desirable to relate asynchrony to a physiologic descriptor of coronary stenosis severity, such as fractional flow reserve, but this was beyond the scope of the current study.26
We combined visual systolic and diastolic asynchrony scores into a semi-quantitative parameter designed to achieve the maximal sensitivity for detecting mild degrees of regional asynchrony. Studies on the ischemic cascade suggest that either systolic or diastolic dysfunction may occur early after the initiation of ischemia.7 Our process of assigning scores to quantify visual impressions of asynchrony magnitude is similar to the well-accepted practice of clinicians’ grading of relative myocardial perfusion. Both our quantitative (BW) and semi-quantitative visual asynchrony parameters were limited in that they did not identify whether the preponderance of mild asynchrony was systolic or diastolic in origin. Nevertheless, our semi-quantitative visual approach has been previously validated, and yielded good agreement between observers, supporting the validity of our observations.
Conclusions
Patients with coronary artery disease may have angiography that shows non-obstructed vessels, with normal regional perfusion. The majority of these territories have quantified rest and stress myocardial perfusion and perfusion reserve that are normal, but a sizeable percentage have subnormal MFR. This finding appears to correlate with angiographic anatomy which, though non-obstructive, has a higher percent stenosis than vessels with normal MFR, and with mild abnormalities of overall systolic and/or diastolic LV synchrony. These data suggest that systolic and diastolic asynchrony may help define coronary arterial territories which are apparently normal by relative perfusion criteria, but which have low perfusion reserve and the potential for demonstrating stress-induced ischemia. Consequently, it is advisable to measure regional MBF, MFR, and regional asynchrony for patients with suspected CAD.
New Knowledge Gained
A subgroup of coronary territories with normal relative perfusion and normal or non-obstructive coronary disease may have reduced MBF and/or reduced MFR, which is signaled physiologically by a mild degree of left ventricular asynchrony.
Abbreviations
- Asynch:
-
Asynchrony measure
- BW:
-
Bandwidth
- CAD:
-
Coronary artery disease
- EF:
-
Ejection fraction
- LAD:
-
Left anterior descending
- LCX:
-
Left circumflex
- LV:
-
Left ventricle
- MBF:
-
Myocardial blood flow
- MFR:
-
Myocardial flow reserve
- PET:
-
Positron emission computed tomography
- RCA:
-
Right coronary artery
References
Sampson UK, Dorbala S, Limaye A, Kwong R, Di Carli MF. Diagnostic accuracy of rubidium-82 myocardial perfusion imaging with hybrid positron emission tomography/computed tomography in the detection of coronary artery disease. J Am Coll Cardiol 2007;49:1052-8.
McArdle BA, Dowsley TF, deKemp RA, Wells GA, Beanlands RS. Does rubidium-82 PET have superior accuracy to SPECT perfusion imaging for the diagnosis of obstructive coronary disease? A systematic review and meta-analysis. J Am Coll Cardiol 2012;60:1828-37.
Hajjiri MM, Leavitt MB, Zheng H, Spooner AE, Fischman AJ, Gewirtz H. Comparison of positron emission tomography measurement of adenosine-stimulated absolute myocardial blood flow versus relative myocardial tracer content for physiological assessment of coronary artery stenosis severity and location. JACC Cardiovasc Imaging 2009;2:751-8.
Taqueti VR, Hachamovitch R, Murthy VL, Naya M, Foster CR, Hainer J, et al. Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation 2015;131:19-27.
Di Carli MF, Rory Hachamovitch R. Quantitative coronary flow capacity for risk stratification and clinical decision making: Is it ready for prime time? J Nucl Med 2019;60:407-9.
Schindler TH, Schelbert HR, Quercioli A, Dilsizian V. Cardiac PET imaging for the detection and monitoring of coronary artery disease and microvascular health. Am Coll Cardiol Imaging 2010;3:623-40.
Nesto RW, Kowalchuk GJ. The ischemic cascade: Temporal sequence of hemodynamic, electrocardiographic and symptomatic expressions of ischemia. Am J Cardiol 1987;57:23C-30C.
Igarashi Y, Chikamori T, Hida S, Tanaka H, Shiba C, Usui Y, et al. Usefulness of phase analysis to differentiate ischemic and non-ischemic etiologies of left ventricular systolic dysfunction in patients with heart failure. Circ J 2014;78:141-50.
Huang W-S, Huang C-H, Lee C-L, Chen C-P, Hung G-U, Chen J. Relation of early post-stress left ventricular dyssynchrony and the extent of angiographic coronary artery disease. J Nucl Cardiol 2014;21:1048-56.
Van Tosh A, Votaw JR, Cooke CD, Reichek N, Palestro CJ, Nichols KJ. Relationships between left ventricular asynchrony and myocardial blood flow. J Nucl Cardiol 2017;24:43-52.
Ardestani A, Ahlberg AW, Katten DM, Santilli K, Polk DM, Bateman TM, et al. Risk stratification using line source attenuation correction with rest/stress Tc-99m sestamibi SPECT myocardial perfusion imaging. J Nucl Cardiol 2014;21:118-26.
Otaki Y, Betancur J, Sharir T, Hu LH, Gransar H, Liang JX, et al. 5-Year prognostic value of quantitative versus visual MPI in subtle perfusion defects. Results from REFINE SPECT. JACC Cardiovasc Imaging 2019. https://doi.org/10.1016/j.jcmg.2019.02.028.
Al Jaroudi W. Early post-stress LV dyssynchrony: A new marker for significant CAD. J Nucl Cardiol 2014;21:1057-61.
Dilsizian V, Bacharach SL, Beanlands RS, Bergmann SR, Delbeke D, Dorbala S, et al. ASNC imaging guidelines/SNMMI procedure standard for positron emission tomography (PET) nuclear cardiology procedures. J Nucl Cardiol 2016;23:1187-226.
Bravo PE, Pozios I, Pinheiro A, Merrill J, Tsui BM, Wahl RL, et al. Comparison and effectiveness of regadenoson versus dipyridamole on stress electrocardiographic changes during positron emission tomography evaluation of patients with hypertrophic cardiomyopathy. Am J Cardiol 2012;110:1033-9.
Johnson NP, Gould KL. Regadenoson versus dipyridamole hyperemia for cardiac PET imaging. J Am Coll Cardiol Imaging 2015;8:438-47.
Esteves FP, Nye JA, Khan A, Folks RD, Halkar RK, Garcia EV, et al. Prompt-gamma compensation in Rb-82 myocardial perfusion 3D PET/CT. J Nucl Cardiol 2010;17:247-53.
Votaw JR, Packard RRS. Technical aspects of acquiring and measuring myocardial blood flow: Method, technique, and QA. J Nucl Cardiol 2017. https://doi.org/10.1007/s12350-017-1049-y.
Murthy VL, Bateman TM, Beanlands RS, Berman DS, Borges-Neto S, Chareonthaitawee P, et al. Clinical quantification of myocardial blood flow using PET: Joint position paper of the SNMMI cardiovascular council and the ASNC. J Nucl Cardiol 2018;25:269-97.
Garcia EV, Klein JL, Moncayo V, Cooke CD, Del’Aune C, Folks R, et al. Diagnostic performance of an artificial intelligence-driven cardiac-structured reporting system for myocardial perfusion SPECT imaging. J Nucl Cardiol 2018. https://doi.org/10.1007/s12350-018-1432-3.
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe EL, et al. Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: Development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol 2005;12:68-95.
Van Tosh A, Votaw JR, Cooke CD, Cao J, Palestro CJ, Nichols KJ. Relationship of 82Rb PET territorial myocardial asynchrony to arterial stenosis. J Nucl Cardiol 2020;27:575-88.
“MedCalc” commercially available statistical analysis software, statistical software version 19.1.5. Ostend: MedCalc Software bv.
Cooke CD, Estevez FP, Chen J, Garcia E. Left ventricular mechanical synchrony from stress rest 82Rb PET myocardial perfusion ECG gated studies: Differentiating normal from LBBB patients. J Nucl Cardiol 2011;18:1076-85.
Al Jaroudi W, Chadi A, DiFilippo F, Brunken RC, Cerquiera MD. Effect of stress testing on left ventricular synchrony by phase analysis of gated positron tomography in patients with normal myocardial perfusion. Eur J Nucl Med Mol Imaging 2012;39:665-72.
Motwani M, Motlagh M, Gupta A, Berman DS, Slomka PJ. Reasons and implications of agreements and disagreements between coronary flow reserve, fractional flow reserve, and myocardial perfusion imaging. J Nucl Cardiol 2018;25:104-19.
Gould KL, Nakagawa Y, Nakagawa K, Sdringola S, Hess MJ, Haynie M, et al. Frequency and clinical implications of fluid dynamically significant diffuse coronary artery disease manifest as graded, longitudinal, base-to-apex myocardial perfusion abnormalities by noninvasive positron emission tomography. Circulation 2000;101:1931-9.
Murthy VL, Naya M, Taqueti VR, Foster CR, Gaber M, Hainer J, et al. Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation 2014;129:2518-27.
Ziadi MC, deKemp RA, Williams KA, Guo A, Chow BJ, Renaud JM, et al. Impaired myocardial flow reserve on rubidium-82 positron emission tomography imaging predicts adverse outcomes in patients assessed for myocardial ischemia. J Am Coll Cardiol 2011;58:740-8.
Nakanishi R, Gransar H, Slomka P, Arsanjan R, Shalev A, Thomson LEB, et al. Predictors of high risk coronary disease in subjects with normal SPECT myocardial perfusion. J Nucl Cardiol 2016;23:530-41.
Acknowledgments
We wish to thank J.J. Mathew for his expert assistance in data acquisition and processing of the PET/CT data, and M. Cochet and C. Popma, for their processing of the angiography data at BCRI.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
No other potential conflicts of interest relevant to this article exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Funding
This investigation was supported in part by Grants from Astellas Pharma Global Development, Inc. to St. Francis Hospital and R01HL094438 and R44HL123069 to Emory University. John R. Votaw, C. David Cooke and Kenneth Nichols participate in royalties from Syntermed, Inc.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Van Tosh, A., Votaw, J.R., Cooke, C.D. et al. Early onset of left ventricular regional asynchrony in arteries with sub-clinical stenosis. J. Nucl. Cardiol. 28, 1040–1050 (2021). https://doi.org/10.1007/s12350-020-02251-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-020-02251-9