Abstract
Purpose
There are limited data on whether differences exist in left ventricular (LV) mechanical dyssynchrony indices derived from stress versus rest gated positron emission tomography (PET) in patients with normal myocardial perfusion imaging (MPI).
Methods
Stress/rest 82Rb gated PET was performed in consecutive patients with normal MPI between 2006 and 2010. Patients were divided into two groups: group 1 [LV ejection fraction (EF) ≥ 55% and QRS < 120 ms] and group 2 (LVEF ≤35%). Images were acquired on a dedicated PET scanner prior to and on a hybrid PET/CT system after November 2008. LV dyssynchrony indices [phase standard deviation (SD)° and SD (ms)] were derived from stress and rest gated images.
Results
There were 91 patients in group 1 (age 61 ± 13, LVEF 66 ± 8%, normal QRS) and 126 in group 2 (age 66 ± 12, LVEF 25 ± 7%). The stress derived LVEF were significantly higher than rest for either group (p < 0.0001). Patients with cardiomyopathy had significantly higher dyssynchrony indices compared to those with normal LVEF (rest SD° 49.2 ± 21.5° vs 16.8 ± 7.8° and stress SD° 42.5 ± 19.4° vs 12.4 ± 3.7°, respectively, p < 0.0001 for both). The dyssynchrony indices derived from rest gated images were significantly higher than those derived from stress in both groups (p < 0.001 by unpaired and paired t test) and irrespective of the type of PET scanner utilized. Finally, 20/87 (23%) patients with normal LVEF and 27/66 (41%) of those with cardiomyopathy but without dyssynchrony based on stress indices were recategorized as having significant dyssynchrony given their resting indices.
Conclusion
LV mechanical dyssynchrony indices by phase analysis are smaller when derived from peak stress versus rest gated PET imaging in patients with normal MPI, irrespective of the resting LVEF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Phase analysis of gated myocardial perfusion imaging (MPI) is a newly emerging technique to derive dyssynchrony indices [1–3]. It predicts response to cardiac resynchronization therapy (CRT) [4] and optimizes patient selection [5, 6]. The method depends on extracting count distribution from each slice of the left ventricular (LV) short axis data set and submitting it to a Fourier transform to generate a phase distribution [7]. Most of the studies have been done on gated single photon emission computed tomography (SPECT) studies, and recently limited data have become available with positron emission tomography (PET) [8]. A recent study has shown that the dyssynchrony indices derived from low tracer dose rest SPECT images are significantly higher than those obtained from high tracer dose stress images [9]. However, it is not clear whether this is predominately driven by the difference in counts (i.e., due to higher tracer dose and hyperemic state) or by the physiologic effect of stress on LV synchrony. While comparing high-dose stress and rest gated SPECT images could clarify this point, the 2-day SPECT protocol is rarely performed these days given the high radiation dose to patients. Gated PET images, on the other hand, might prove quite useful. In fact, both rest and stress studies are performed on the same day using identical tracer dose, and stress gated images are acquired within 1–2 min after the tracer infusion, hence representing true peak stress imaging.
The aim of the study was to compare mechanical dyssynchrony indices from gated rest versus stress PET images and determine whether there is a physiologic effect of stress on LV mechanical synchrony in patients with normal MPI.
Materials and methods
Patient selection
We identified consecutive patients who had MPI from the PET clinical database maintained at the Cleveland Clinic and approved by the Institutional Review Board (IRB) between March 2006 and November 2010. Patients were divided into two groups: group 1 included those with normal LV ejection fraction (EF) (LVEF ≥55%) and QRS < 120 ms; group 2 included patients with LVEF ≤35% with no restriction on QRS duration. All patients had a pharmacologic stress/rest 82Rb gated PET with dipyridamole. Patients with hypertrophic cardiomyopathy, end-stage renal disease, congenital heart disease, or abnormal MPI were excluded. Of 832 patients that were identified, 615 were excluded, with 91 patients remaining in group 1 and 126 in group 2 (Fig. 1). Patients’ demographics, comorbidities, and medications were entered prospectively into an IRB approved database at the time of testing and subsequently retrieved for analysis.
Gated PET
Gated PET 82Rb images were acquired on two scanners: (1) prior to 1 November 2008 a dedicated PET scanner (Siemens ECAT HR+) with BGO crystals acquiring in 2-D mode with septa and (2) starting on 1 November 2008 a hybrid PET/CT scanner (Siemens Biograph 40) with LSO crystals acquiring in 3-D mode without septa. The nominal transaxial/axial spatial resolutions were 4.6 mm/4.6 mm for the dedicated PET scanner and 4.4 mm/4.7 mm for the hybrid PET/CT scanner, respectively.
For the dedicated PET scanner, 60 mCi 82RbCl were infused at rest and at stress. The stress test was performed pharmacologically with dipyridamole infusion of 0.56 mg/kg over 4 min and the 82Rb started at 8 min. Data were acquired for 300 s as eight-frame ECG gated sinograms starting 120 s post-infusion. Data for attenuation correction were acquired with 68Ge transmission sources. A single transmission image was shared for both the rest and stress studies. The patient was in the same position for all three scans: rest, transmission, and stress. Data were reconstructed [2-D ordered subset expectation maximization (OSEM) algorithm] as static images (4 iterations, 8 subsets, 8 mm Gaussian filter) and as gated images (2 iterations, 8 subsets, 12 mm Gaussian filter).
For the hybrid PET/CT scanner, 40 mCi 82RbCl were infused at rest and at stress, and dipyridamole was also the pharmacologic stress agent. Data were acquired for 300 s in list mode starting 90 s post-infusion and were histogrammed as static 3-D sinograms and as eight-frame gated 3-D sinograms. If it was later determined that there was unacceptable blood pool activity, then the data were reprocessed with a longer initial delay. Data for attenuation correction were acquired using computed tomography (CT) using a low-dose protocol (120 kVp, 12 mAs, 0.3 mSv dose per scan) with breath-hold at normal end expiration and with metal artifact reduction enabled. A CT scan was acquired immediately before each of the rest and stress PET scans. Data were reconstructed (3-D OSEM algorithm) as static and gated images using the same reconstruction parameters as described above. The estimated total radiation dose delivered to patients was 7.5 mSv and 4.1 mSv using the dedicated and hybrid PET, respectively.
PET images were reoriented along the standard cardiac axes and displayed using the INVIA Corridor4DM software (Ann Arbor, MI, USA). LV volumes and EF were automatically computed by the software for both the rest and stress 82Rb images. The reproducibility of LVEF measurements at our department with gated PET was excellent with less than 3% absolute change in measured LVEF in all patients and 1–2% in those with cardiomyopathy. The MPI and gated PET data were interpreted by board certified nuclear cardiologists or radiologist including WA, WJ, MC, and RB.
LV mechanical dyssynchrony
The dyssynchrony indices were derived from the stress and rest gated images using the time to peak thickening with a single harmonic fit method (Corridor4DM, INVIA, Ann Arbor, MI, USA). The method has been described in detail [10]. Briefly, the maximal myocardial intensity as a function of the gating interval is recorded from a 3-D sampling of the left ventricular myocardium. Each of the time-intensity curves is fitted to a first-order harmonic using Fourier analysis, from which the phase of the first-order harmonic approximates the time from end diastole (typically the start of the cardiac cycle) to the time of the maximum counts for each region, which represents the point of peak contraction. Extracardiac counts were excluded as permissible without reducing cardiac counts during raw image data processing, and proper alignment of the horizontal and vertical axes of the images was performed as needed. Manual corrections to the center, radius, and apex parameters were made only if there was gross visual misalignment of these parameters, and manual base parameter placement was performed to avoid low counts “scatter” from the base of the LV which might contribute to a falsely abnormal phase histogram [11].
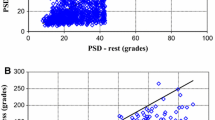
The phase distribution was displayed on a histogram, and the standard deviation (SD) of the phase distribution was generated. The indices were displayed as percentage of the R-R cycle and then converted into degrees by multiplying by 3.6 (360/100) (Fig. 2) and into ms by multiplying by the mean R-R interval length during image acquisition. The mechanical dyssynchrony indices were derived by experienced readers (WA and WJ).
Statistical analysis
A descriptive analysis was performed examining pertinent variables for each group. Continuous variables were expressed as means ± SD and compared using the paired and unpaired Student’s t test or Wilcoxon rank test as appropriate. Categorical variables were expressed as percentages and compared using the Pearson chi-square or Fisher’s exact test as appropriate. The analysis was also stratified according to the type of imaging scanner used (i.e., dedicated PET with 2-D vs hybrid PET/CT with 3-D mode) because of difference in counts statistics and sensitivities. A p value <0.05 was set a priori and considered statistically significant. All statistical analyses were performed using the Statistical Package for the Social Sciences, version 11.5, for Windows (SPSS, Chicago, IL, USA).
Results
Patient characteristics
There were 91 patients with LVEF ≥ 55%, normal MPI and QRS < 120 ms (age 61 ± 13, 56% male) (Ggoup 1) and 126 patients with LVEF ≤35% and normal MPI (age 66 ± 12, 79% male, 15% left bundle branch block) (group 2). Patients in group 2 were older, had more diabetes mellitus, peripheral vascular disease, and atrial fibrillation. The baseline characteristics of the patients are summarized in Table 1.
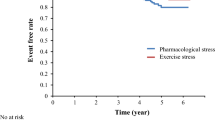
Hemodynamics
The peak heart rates during image acquisition were significantly higher for stress vs rest (85 ± 17 vs 68 ± 12 bpm for group1 and 87 ± 15 vs 77 ± 14 bpm for group 2, respectively, p < 0.001 for both). The stress derived LVEF were significantly higher than rest LVEF for all patients in both groups (p < 0.0001) (Fig. 3). The resting and peak stress blood pressures were not recorded into the stress database prior to November 2010 and were not available for analysis.
LV mechanical dyssynchrony
Patients with cardiomyopathy had significantly higher dyssynchrony indices compared to patients in group 1 (phase SD° 49.2 ± 21.5° vs 16.8 ± 7.8° for rest and 42.5 ± 19.4° vs 12.4 ± 3.7° for stress, respectively, p < 0.0001 for both). Similar values were obtained for phase SD (ms) (Fig. 4). The dyssynchrony indices [phase SD° and SD (ms)] derived from rest gated images were significantly higher than those derived from stress in both groups (p < 0.001 by unpaired and paired t test) (Fig. 4).
Using an SD° cutoff of 20° to define the presence of dyssynchrony as described in a previously published paper[12] (mean + 2*SD of the stress SD° values derived from group 1, cutoff = 12.4 +2*3.7°), 20/87 (23%) patients in group1 with no mechanical dyssynchrony based on stress indices were recategorized as having dyssynchrony if resting indices were used. Similarly, using an SD cutoff value of 43° to define significant mechanical dyssynchrony in patients with cardiomyopathy (group 2) (value extrapolated from the gated SPECT literature [4]), 27/66 (41%) of patients with no dyssynchrony based on stress indices were recategorized as having significant dyssynchrony if resting indices were used.
Effect of imaging scanner on dyssynchrony indices
Two scanners were used to image patients. Prior to November 2008, 61 (67%) and 54 (43%) patients were imaged using a dedicated PET scanner acquiring in 2-D mode (group1 and group 2, respectively), and starting on 1 November 2008, 30 (33%) and 72 (57%) patients were imaged with a hybrid PET/CT scanner acquiring in 3-D mode without septa (group 1 and group 2, respectively). The mean rest LVEF and dyssynchrony indices derived from the first scanner did not differ from those obtained using the second scanner. Similar findings were observed with the stress LVEF and phase SD, for patients in groups 1 and 2. The rest phase SD° and SD (ms) were significantly higher than stress in both groups irrespective of the type of scanner used. Similar changes in LVEF were seen as described previously, also irrespective of the type of PET scanner.
Discussion
This is the first study to evaluate dyssynchrony indices by PET in patients with normal perfusion at rest and peak stress. We also used a cohort of patients with normal LVEF and MPI (group 1) to establish normal values for the population.
Potential factors that may affect dyssynchrony indices when processed from stress rather than rest gated images include: tracer dose, counts, type of stress test (pharmacologic versus exercise), temporal resolution, timing of image acquisition post tracer injection, change in hemodynamics, LVEF, and ischemia. In the current study, both stress and rest gated images were performed with the same tracer dose (60/60 or 40/40 mCi 82Rb); the stress test was performed using dipyridamole infusion for all patients; image acquisition was acquired within a couple of minutes after tracer injection for both stress and rest images, using 8 frames/cycle, per standard protocol; and all patients had normal MPI without any fixed or reversible perfusion defects, hence eliminating many of the potential confounders.
One hypothesis is that the dyssynchrony differences between rest and stress studies may be related to the fact that the stress studies contain more counts due to hyperemia and have better count statistics and image quality. We investigated this indirectly by comparing dyssynchrony indices for studies acquired on the dedicated PET scanner versus the hybrid PET/CT scanner. The PET scanner acquired the 82Rb data in 2-D mode with axial septa, whereas the hybrid PET/CT scanner acquired data in 3-D mode without axial septa. As a result, the PET/CT scanner had much higher sensitivity than the PET scanner, by approximately a factor of 5, and thus produced images with better statistical image quality, even though the tracer dose used with the hybrid scanner was lower than the one used with the dedicated scanner (i.e., 40 vs 60 mCi). Since there was no significant difference in the analysis with regards to the dedicated PET versus PET/CT scanner, this suggests that count statistics were not responsible for the narrower SD at hyperemia for these 82Rb studies. It is important to note that this conclusion does not apply to 99mTc or 201Tl imaged with SPECT, since count statistics and image quality in SPECT differ markedly from 82Rb PET.
The effect of heart rate on dyssynchrony indices was also assessed. This is important since the temporal resolution of the technique is limited (although the effective temporal resolution seems to be much better with the first harmonic mathematical modeling [13]) and might be challenging particularly at fast heart rate. Gating with PET occurs at peak stress and is routinely associated with higher heart rate compared to rest. While phase SD° is a relative index, stress SD (ms) is adjusted for the R-R interval and is indeed consistently lower with stress than rest. Although echocardiographic dyssynchrony indices rely on absolute values of delay timing of opposing wall contraction (ms) [14], most of the literature reports with phase analysis of gated MPI have relied on relative values expressed as % of R-R interval or 360° rather than in ms [7, 15, 16]. Whether one is more accurate or physiologically more significant than the other warrants further investigation.
PET is a potentially attractive alternative to echocardiography in assessing mechanical dyssynchrony. Unlike echocardiography, phase analysis provides a single and uniform dyssynchrony index, is highly reproducible based on automated detection of several hundred data points in three dimensions (which is advantageous in patients with regional wall motion abnormalities and ischemic cardiomyopathy), and is averaged over several hundreds of cardiac cycles (advantageous in patients with atrial fibrillation) [1, 7]. Also, postsystolic shortening, which is often excluded during echocardiographic assessment of mechanical dyssynchrony, is integrated in the mechanical dispersion index or phase SD derived from gated MPI since the phase histogram displays time to peak contraction throughout the cardiac cycle [10].
There was a statistically significant increase in LVEF with stress versus rest in each group. Stress induces improvement in synchrony and contractility that translates into a higher LVEF. Peak stress LVEF is known to be higher than rest LVEF [17]; this difference, also known as LVEF reserve, has been shown using gated PET and carries prognostic information [18]. In our study, the stress LVEF was statistically higher than rest for patients in each group and particularly those with normal LVEF and explains, at least in part, why the stress indices are smaller (i.e., more synchrony) than rest. The absolute difference in LVEF in patients with cardiomyopathy (group 2) [24% (rest) versus 25.5% (stress)], although it reached statistical significance, falls within the reproducibility limits of the technique, hence limiting accurate interpretation and explanation of the change in mechanical dyssynchrony in this group. Other factors such as right ventricular function and hemodynamics could have also affected mechanical synchrony at the time of image gating, but were not available for analysis.
Evaluating mechanical dyssynchrony in patients with cardiomyopathy is important as it has been shown to optimize patient selection for CRT and predict response and outcomes [6]. While most of the literature has been exclusively performed with gated SPECT, there is growing interest in using gated PET [8] which offers better image quality and information on viability among other factors. It is important to decide which gated images to use to derive dyssynchrony indices (stress versus rest), at least in patients with normal MPI. There has been increasing interest in assessing mechanical dyssynchrony from stress echocardiography with promising results [19, 20]. Recent studies have shown that mechanical dyssynchrony indices derived from low-dose dobutamine stress echocardiogram [21] and from bicycle exercise echocardiogram [22] were better predictors of response to CRT than resting echocardiography. The improvement in LV synchronicity, contractility reserve, and mitral regurgitation are some of the potential factors associated with such results. Our study is the first to our knowledge to assess mechanical dyssynchrony from stress gated PET indices. Choosing the rest gated PET rather than stress was associated with recategorization of 41% of patients with low EF as having dyssynchrony. However, this is based on the assumption that the stress indices are the gold standard, which may not be necessarily true, particularly in the absence of outcome data. In fact, there is a difference in the range for defining normalcy in the stress and rest perfusion studies, and perhaps different cutoff values of dyssynchrony indices should be used for each test separately. The current study defines the normal ranges for dyssynchrony indices for stress and rest gated images, and a larger cohort is needed for further validation and to test whether stress derived indices with gated PET are better predictors of outcome, particularly response to CRT.
It would be interesting to define the range of difference in dyssynchrony variables between stress and rest studies, and investigate the significance of a wider difference, and whether it is more clinically relevant than stress or rest variables in isolation. Furthermore, outcome results to clarify the meaning of lower mechanical dyssynchrony from stress gated PET, and whether it is a better predictor of response to CRT, as shown with low-dose dobutamine echocardiography [21], are of great interest. Another potential impact of stress phase analysis in clinical practice is the evaluation of patients with ischemia where LV stunning and worsening of LV dyssynchrony may occur at peak stress, particularly those with left main or severe three-vessel disease who have balanced ischemia; whether mechanical dyssynchrony can increase the sensitivity and specificity of MPI to detect left main or three-vessel severe coronary artery disease needs further evaluation. While a study of a small number of patients with gated SPECT showed that reversible perfusion defect size does not affect the measured dyssynchrony indices (stress vs rest) [23], such findings may not apply to PET which acquires images at peak stress and might exhibit LV myocardial stunning particularly with a large ischemic burden.
Limitations
The study has the limitations of a retrospective study from a single tertiary center with a relatively small number of patients. The study was not designed or powered to assess for clinical outcomes, particularly response to CRT. The 4DM software has not been validated in gated PET studies, but the analysis algorithm was extrapolated from gated SPECT studies. However, a recent paper with a small number of patients showed gated PET images yielded similar dyssynchrony indices to SPECT for patients who had both studies using the same algorithm of the Emory Cardiac Toolbox (ECTb) (R = 0.88) [8], and the 4DM software has also been validated against the ECTb [10]. In addition, there was a lack of an independent and gold standard reference for mechanical dyssynchrony. While phase analysis has been validated against echocardiography [24, 25], the poor reproducibility of echocardiography (particularly tissue Doppler imaging) [26] and the numerous potential indices that could be used have put in question whether echocardiography is truly the gold standard, and if so, which index to use. Phase analysis on the other hand offers a simple, automated, and reproducible method to generate a single dyssynchrony index from a 3-D data set averaged over multiple R-R intervals. Also, the temporal resolution of the technique is low (8 frames/cycle), but the effective temporal resolution seems to approach 15 ms at a heart rate of 60 bpm, at least as shown with the ECTb [13]. However, this needs to be tested and validated separately with 4DM software. The baseline right ventricular function and blood pressure at the time of image acquisition were not available; both of these parameters could potentially affect LV contractility at peak stress and therefore LV synchrony. Also, the actual counts from the stress and rest images were not available since the PET raw data were deleted after image processing. This was evaluated indirectly, and perhaps partially, by stratifying the results based on two scanners with ≈ fivefold differences in sensitivity and count distribution. There was no separate and standard criterion for normalcy in patients with preserved LVEF and normal MPI previously published with PET; we defined normalcy as values up to 2× SD from the mean from our cohort and as described in a previously published study [12]. The cutoff value for SD of 43° has been extrapolated from a single study with SPECT and needs further validation [4]. Finally, the study excluded patients with perfusion defect size in whom mechanical dyssynchrony would have been important to assess, predominately to avoid a potentially confounding effect from stress-induced ischemia on LV synchronicity. Hence, our findings cannot be generalized to all patients with cardiomyopathy, and a separate study is needed to evaluate those with abnormal MPI.
In patients with normal MPI, LV mechanical dyssynchrony indices by phase analysis are smaller and statistically different when derived from stress versus rest gated PET images, irrespective of the LV systolic function and despite using a similar tracer dose. The difference is perhaps partially related to the effect of stress physiology on LV synchrony and improvement of LV function, particularly in those with normal LVEF. Further validation studies are warranted. The clinical implications and predictors of response to CRT of lower mechanical dyssynchrony indices from stress gated PET need to be evaluated in further outcome studies.
References
AlJaroudi W, Chen J, Jaber WA, Lloyd SG, Cerqueira M, Marwick T. Nonechocardiographic imaging in evaluation for cardiac resynchronization therapy. Circ Cardiovasc Imaging 2011;4:334–43.
Chen J, Garcia EV, Bax JJ, Iskandrian AE, Borges-Neto S, Soman P. SPECT myocardial perfusion imaging for the assessment of left ventricular mechanical dyssynchrony. J Nucl Cardiol 2011;18:685–94.
Chen J, Bax JJ, Henneman MM, Boogers MJ, Garcia EV. Is nuclear imaging a viable alternative technique to assess dyssynchrony. Europace 2008;10 Suppl 3:iii101–5.
Henneman MM, Chen J, Dibbets-Schneider P, Stokkel MP, Bleeker GB, Ypenburg C, et al. Can LV dyssynchrony as assessed with phase analysis on gated myocardial perfusion SPECT predict response to CRT? J Nucl Med 2007;48:1104–11.
Boogers MJ, Chen J, van Bommel RJ, Borleffs CJ, Dibbets-Schneider P, van der Hiel B, et al. Optimal left ventricular lead position assessed with phase analysis on gated myocardial perfusion SPECT. Eur J Nucl Med Mol Imaging 2011;38:230–8.
Friehling M, Chen J, Saba S, Bazaz R, Schwartzman D, Adelstein EC, et al. A prospective pilot study to evaluate the relationship between acute change in left ventricular synchrony after cardiac resynchronization therapy and patient outcome using a single-injection gated SPECT protocol. Circ Cardiovasc Imaging 2011;4:532–9.
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe EL, et al. Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol 2005;12:687–95.
Pazhenkottil AP, Buechel RR, Nkoulou R, Ghadri JR, Herzog BA, Husmann L, et al. Left ventricular dyssynchrony assessment by phase analysis from gated PET-FDG scans. J Nucl Cardiol 2011;18:920–5.
AlJaroudi W, Jaber WA, Cerqueira M. Effect of tracer dose on left ventricular mechanical dyssynchrony indices by phase analysis of gated single photon emission computed tomography myocardial perfusion imaging. J Nucl Cardiol 2011 (in press).
AlJaroudi W, Jaber WA, Grimm R, Marwick T, Cerqueira M. Alternative methods for the assessment of mechanical dyssynchrony by phase analysis of gated single photon emission computed tomography myocardial perfusion imaging. Int J Card Imaging 2011 (in press).
Trimble MA, Velazquez EJ, Adams GL, Honeycutt EF, Pagnanelli RA, Barnhart HX, et al. Repeatability and reproducibility of phase analysis of gated single-photon emission computed tomography myocardial perfusion imaging used to quantify cardiac dyssynchrony. Nucl Med Commun 2008;29:374–81.
Pazhenkottil AP, Buechel RR, Husmann L, Nkoulou RN, Wolfrum M, Ghadri JR, et al. Long-term prognostic value of left ventricular dyssynchrony assessment by phase analysis from myocardial perfusion imaging. Heart 2011;97:33–7.
Chen J, Faber TL, Cooke CD, Garcia EV. Temporal resolution of multiharmonic phase analysis of ECG-gated myocardial perfusion SPECT studies. J Nucl Cardiol 2008;15:383–91.
Gorcsan 3rd J. Echocardiographic assessment of ventricular dyssynchrony. Curr Heart Fail Rep 2008;5:31–7.
Trimble MA, Borges-Neto S, Smallheiser S, Chen J, Honeycutt EF, Shaw LK, et al. Evaluation of left ventricular mechanical dyssynchrony as determined by phase analysis of ECG-gated SPECT myocardial perfusion imaging in patients with left ventricular dysfunction and conduction disturbances. J Nucl Cardiol 2007;14:298–307.
Aljaroudi W, Koneru J, Iqbal F, Aggarwal H, Heo J, Iskandrian AE. Left ventricular mechanical dyssynchrony by phase analysis of gated single photon emission computed tomography in end-stage renal disease. Am J Cardiol 2010;106:1042–7.
Aktaş A, Yalcin H, Koyuncu A, Aydinalp A, Müderrisoglu H. The influence of post-exercise cardiac changes on thallium-gated myocardial perfusion scintigraphy findings in normal subjects. Nucl Med Commun 2005;26:109–14.
Dorbala S, Hachamovitch R, Curillova Z, Thomas D, Vangala D, Kwong RY, et al. Incremental prognostic value of gated Rb-82 positron emission tomography myocardial perfusion imaging over clinical variables and rest LVEF. JACC Cardiovasc Imaging 2009;2:846–54.
Moonen M, O’Connor K, Magne J, Lancellotti P, Pierard LA. Stress echocardiography for selecting potential responders to cardiac resynchronisation therapy. Heart 2010;96:1142–6.
Valzania C, Gadler F, Eriksson MJ, Olsson A, Boriani G, Braunschweig F. Electromechanical effects of cardiac resynchronization therapy during rest and stress in patients with heart failure. Eur J Heart Fail 2007;9:644–50.
Altman RK, McCarty D, Chen-Tournoux AA, Tournoux FB, Riedl L, Orencole M, et al. Usefulness of low-dose dobutamine echocardiography to predict response and outcome in patients undergoing cardiac resynchronization therapy. Am J Cardiol 2011;108:252–7.
Rocchi G, Bertini M, Biffi M, Ziacchi M, Biagini E, Gallelli I, et al. Exercise stress echocardiography is superior to rest echocardiography in predicting left ventricular reverse remodelling and functional improvement after cardiac resynchronization therapy. Eur Heart J 2009;30:89–97.
Aljaroudi W, Koneru J, Heo J, Iskandrian AE. Impact of ischemia on left ventricular dyssynchrony by phase analysis of gated single photon emission computed tomography myocardial perfusion imaging. J Nucl Cardiol 2011;18:36–42.
Henneman MM, Chen J, Ypenburg C, Dibbets P, Bleeker GB, Boersma E, et al. Phase analysis of gated myocardial perfusion single-photon emission computed tomography compared with tissue Doppler imaging for the assessment of left ventricular dyssynchrony. J Am Coll Cardiol 2007;49:1708–14.
Marsan NA, Henneman MM, Chen J, Ypenburg C, Dibbets P, Ghio S, et al. Real-time three-dimensional echocardiography as a novel approach to quantify left ventricular dyssynchrony: a comparison study with phase analysis of gated myocardial perfusion single photon emission computed tomography. J Am Soc Echocardiogr 2008;21:801–7.
Chung E, Leon A, Tavazzi L, Sun J, Nihoyannopoulos P, Merlino J, et al. Results of the Predictors of Response to CRT (PROSPECT) trial. Circulation 2008;117:2608–16.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
AlJaroudi, W., Alraies, M.C., DiFilippo, F. et al. Effect of stress testing on left ventricular mechanical synchrony by phase analysis of gated positron emission tomography in patients with normal myocardial perfusion. Eur J Nucl Med Mol Imaging 39, 665–672 (2012). https://doi.org/10.1007/s00259-011-2025-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-011-2025-4