Abstract
Background
Although line source attenuation correction (AC) in SPECT MPI studies improves diagnostic accuracy, its prognostic value is less understood.
Methods
Consecutive patients (n = 6,513) who underwent rest/stress AC ECG-gated SPECT MPI were followed for cardiac death or non-fatal myocardial infarction (MI). A 17-segment model and AC summed stress score (SSS) were used to classify images.
Results
Of the 6,513 patients, cardiac death or non-fatal MI occurred in 267 (4.1%), over 2.0 ± 1.4 years. The AC-SSS in patients with a cardiac event (5.6 ± 7.8) was significantly higher than in those without (1.9 ± 4.6, P < .001). The annualized cardiac event rate in patients with an AC-SSS 1-3 (3.6%) was significantly higher than in those with an AC-SSS = 0 (1.1%, P < .001) but similar to that in those with an AC-SSS 4-8 (2.9%, P = .4). Accordingly, patients were classified to AC-SSS = 0, 1-8, and >8 with annualized cardiac event rates of 1.1%, 3.2%, and 8.5%, respectively (P < .0001). In multivariate analysis, an AC-SSS 1-8 and >8 emerged as independent predictors of cardiac events (P < .02 and P < .0001, respectively).
Conclusion
Rest/stress ECG-gated SPECT MPI with line source AC provides highly effective and incremental risk stratification for future cardiac events.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Attenuation artifact remains a challenge for accurate interpretation and risk stratification of stress nuclear myocardial perfusion imaging (MPI). A recent report by Patel et al1 suggests that the false-positive rate of stress MPI is as high as 60%, resulting in unnecessary catheterizations and lack of confidence in imaging results. Attenuation correction (AC) using either computed tomography (CT) or radionuclide line sources has been documented to improve diagnostic accuracy, especially specificity.2-10 These data have led the American Society of Nuclear Cardiology (ASNC) and the Society of Nuclear Medicine (SNM) in a joint position statement to strongly endorse the routine use of AC with stress radionuclide MPI.11
A continued argument against the implementation of an AC solution has been the lack of outcomes data.12 This is of particular importance in view of concerns that AC devices may underestimate both the presence and severity of perfusion abnormalities and thus coronary artery disease (CAD), potentially resulting in higher cardiac event rates in normal studies after AC. Although several studies have demonstrated a low cardiac event rate in patients with normal stress-only AC results,13 few reports are available in patients undergoing routine rest/stress MPI, including those with abnormal AC results.14,15 Hence, the purpose of this study was to determine the prognostic value of line source AC in consecutive patients with known or suspected CAD referred for rest/stress ECG-gated SPECT MPI.
Methods
Patient Selection
From the Nuclear Cardiology Laboratory clinical database at Hartford Hospital, Hartford, CT, consecutive patients who underwent rest/stress Tc-99m sestamibi SPECT imaging with ECG-gating, between January 2003 and October 2006 were identified. Patients who underwent stress-only Tc-99m sestamibi SPECT imaging or were unable to undergo ECG-gating during image acquisition were excluded. Pretest probability of CAD was calculated using the standard Diamond and Forrester classification.16
Stress Testing and Image Acquisition
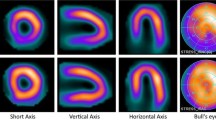
Patients were instructed to fast ≥8 hours prior to testing and to withhold caffeinated products. Patients receiving beta-blockers or oral dipyridamole were instructed not to take those medications at least 8 hours before the test. Patients underwent exercise or pharmacologic stress according to standard techniques.17 For patients undergoing a 1- or 2-day rest/stress protocol, 10-30 mCi of Tc-99m sestamibi was injected for rest and 30-45 mCi for stress imaging. SPECT acquisition was begun 30-60 minutes after stress/rest injection. Images were acquired using either dual-headed Cardio-60 or Cardio-MD cameras (Phillips Medical Systems) equipped with two gadolinium 153 line sources for transmission acquisition18 and VantagePro/ExSPECT II software for AC. Images were acquired over 180° non-circular orbit from 45° right anterior oblique to left posterior oblique, with a 64 × 64 matrix (pixel size of approximately 0.64 cm) for the emission images and a 128 × 128 matrix (pixel size 0.32 cm) for the transmission images. A total of 64 emission, transmission and scatter projections were obtained, 30-35 seconds/projection. Attenuation-corrected transverse images were reconstructed by first prefiltering the emission projections with a fifth-order 0.6 Nyquist Butterworth filter followed by reconstruction via an iterative maximum likelihood expectation maximization algorithm. The motion correction algorithm was implemented on rotating images with motion artifact.
Attenuation maps were reconstructed by the use of a published Bayesian prior approach with Butterworth filter processing at 0.66 critical frequency and an order of 5.19 The attenuation map reconstruction used 12 iterations with a uniform initial estimate. The emission transaxial images were reconstructed by use of a maximum likelihood algorithm with 30 iterations and a uniform initial estimate. The scatter distribution obtained from the scatter window was used to correct both the scatter from the patient into the photopeak window and scatter from the patient into the transmission energy window. All attenuation maps were assessed for adequate counts, field uniformity, and truncation.
Image Interpretation
All images were visually interpreted during daily clinical reading sessions by a consensus of two or more experienced readers using the ASNC 17-segment model and scoring system.20 In visual assessment of perfusion, each segment was scored on a scale of 0-4 (0 = normal, 1 = mild, 2 = moderate, 3 = severe, 4 = absent photon activity). All images were interpreted and scored in sequence, non-AC data first followed by AC data. Both uncorrected and AC corrected images were scored using the same 17-segment scoring system. For each image, a summed stress score (SSS) and a summed rest score (SRS) were calculated for both non-AC and AC data by adding the segment scores at stress and rest, respectively. A summed difference score (SDS) was calculated for both non-AC and AC data by subtracting SRS from SSS.
Definition of Abnormal Perfusion
With non-AC data, cutoffs were determined from previous studies.15 Accordingly, a SSS < 4 was considered normal, 4-8 mildly abnormal, and >8 moderate to severely abnormal perfusion. With AC data, cutoffs chosen were based on those determined by Baghdasarian et al15 Accordingly, an attenuation-corrected SSS (AC-SSS) of 0 was considered normal, 1-3 and 4-8 mildly abnormal, and >8 moderate to severely abnormal perfusion.
Follow-Up
Patient follow-up was obtained by scripted telephone interviews and mailed questionnaires. An investigator unaware of clinical, stress testing and SPECT imaging data confirmed the subsequent occurrence of cardiac-related procedures and/or adverse events by reviewing hospital admission records and death certificates. The primary endpoint for this study was a composite of cardiac death or non-fatal myocardial infarction (MI). Data were censored at the first cardiac event or at the time of last follow-up within a 5-year limit.
Statistical Analysis
Clinical characteristics were expressed as mean ± standard deviation or as proportions. Inter-group comparisons were performed using the χ 2 for categorical variables and t test for continuous variables. Survival curves were generated by the Kaplan-Meier method. Differences between survival curves were compared using the log-rank test. Variables that achieved statistical significance by univariate analysis were entered into Cox proportional hazards regression to identify independent predictors of cardiac events with the AC-SSS entered as a categorical covariate. A forward, stepwise, multi-block procedure was used, with gated SPECT variables entered in the last block to determine incremental value over clinical variables. A P value < .05 was considered significant in all analyses. SAS 9.1.3 was used for statistical analysis.
Results
Clinical Characteristics
Of the 7,312 consecutive patients who underwent 1- or 2-day rest/stress Tc-99m sestamibi SPECT imaging with ECG-gating, follow-up for the subsequent occurrence of cardiac-related procedures and outcomes was available in 92% (n = 6,740) over a mean of 2.0 ± 1.4 years. Patients lost to follow-up (8%) were more often male and younger. Cardiac risk factors were less prevalent. The mean AC-SSS was significantly lower among those who were lost to follow-up (1.7 vs 2.2, P = .01). Patients who underwent either percutaneous coronary intervention or coronary artery bypass grafting ≤60 days after SPECT imaging (n = 227, 3.4%) were excluded. Notably, the mean AC-SDS in patients who underwent early coronary revascularization was significantly higher than in those who did not (5.4 ± 4.9 and 0.9 ± 1.9, respectively, P < .0001). The 6,513 patients who comprised the study cohort for the prognostic analysis had a mean age of 63 ± 13.6 years and 51% were female. Sixty-six percent of the patients were referred for stress nuclear imaging for chest pain evaluation. Other indications for stress imaging were dyspnea, congestive heart failure, arrhythmia, palpitation, dizziness, preoperative cardiac evaluation, and abnormal ECG. The pretest probability for CAD was intermediate in 81% and high in 8% of the study population. Thirty-two percent of the patients had known CAD at the time of SPECT imaging, 31% had diabetes mellitus, and 62% had undergone pharmacologic stress. In addition, 49% were taking aspirin, 35% ACE inhibitors, and 43% beta-blockers (Table 1).
Cardiac Events
In follow-up, 267 (4.1%) patients had an adverse cardiac event, of which 149 (2.3%) suffered cardiac death while 118 (1.8%) sustained a non-fatal MI. Patients with an adverse cardiac event were significantly older than those without and were more likely to have known CAD, diabetes mellitus, hypertension, history of tobacco use, or to have undergone pharmacologic stress. In addition, patients with an adverse cardiac event had a significantly higher SSS, SRS, and SDS either without or with AC than those who were cardiac event-free as well as a significantly lower LVEF on gated SPECT (Table 1).
Impact of Attenuation Correction on Assessment of Myocardial Perfusion
The impact of AC upon assessment of myocardial perfusion was examined (Figure 1). Of 6,513 patients, 35% (n = 2,312) demonstrated completely normal perfusion without AC (SSS = 0) and in all of these patients, AC interpretation was the same (AC-SSS = 0). However, for patients demonstrating a small/mild defect without AC (SSS 1-3), 88% (1,841/2,102) were considered normal with AC (AC-SSS = 0). For patients with a SSS 4-8 without AC, 44% (567/1,299) were considered normal with AC (AC-SSS = 0). For patients demonstrating moderate to severely abnormal perfusion without AC (SSS > 8), only 4% (35/800) were considered normal with AC (AC-SSS = 0) while the vast majority (78% [621/800]) remained in the same SSS category with AC.
Risk Stratification with Attenuation-Corrected Data
The incidence of cardiac death or non-fatal MI in relation to the SSS both without and with AC was examined. As shown in Figure 2, the annualized cardiac event rate in patients with a SSS of 0-3 was low, and accelerated with higher SSS categories. Notably, there were no significant differences in the annualized cardiac event rate for any “traditional” SSS category without or with AC. We then examined the AC outcomes using new cutoffs of normal to be an SSS of 0 and mild to be an SSS of 1-3 (Figure 3). Other SSS categories remained the same. With or without AC, the annualized cardiac event rate in patients with a SSS of 0 was low (0.9% vs 1.1%, respectively, P = NS). When stratified by type of stress test performed, the annualized cardiac event rate was similarly low in exercise stress MPI group with SSS of 0, with or without AC (0.56% vs 0.49%, respectively, P = NS). There was also a similar but higher event rate identified for the pharmacologic stress group (1.58 without AC, 1.2 with AC, P = NS). However, the annualized cardiac event rate in patients with SSS 1-3 was significantly higher with AC compared to that without AC (3.6% vs 1.4%, P = .0001). Conversely, the annualized cardiac event rate with or without AC was similar in patients with a SSS 4-8 or >8. Furthermore, the annualized cardiac event rate was similar in patients with an AC-SSS 1-3 vs 4-8 (3.6% vs 2.9%, respectively, P = .4). Therefore, these two categories were merged introducing the cutoff of AC-SSS 1-8 to represent mildly abnormal perfusion and an AC-SSS > 8 to represent moderately to severely abnormal perfusion in subsequent evaluations (Figure 4).
Cardiac event rates over time in the SSS risk categories of normal, mild, and moderately severe (SSS 0, 1-8, >8, respectively) were examined using Kaplan-Meier analysis (Figure 4). There was a statistically significant difference in 5-year survival free of cardiac death or non-fatal MI between SSS risk categories, with and without AC (P < .0001). Patients with AC-SSS 1-8 or >8 had significantly worse cardiac prognosis compared to those with AC-SSS = 0 and overtime the separation of these survival curves became more profound. Without AC the separation of survival curves of SSS 1-8 and SSS = 0 were less profound (Figure 5). Risk stratification using the same AC risk categories in relation to gender was examined. For both genders, similar findings emerged and an AC-SSS > 8 was associated with the worst outcome (Figure 6).
Independent Predictors of Adverse Cardiac Events
Of the 11 clinical and ECG-gated SPECT variables that were found to be significantly associated with cardiac death or non-fatal MI in univariate analysis (Table 1), 8 emerged as independent predictors of adverse cardiac events in multivariable analysis (5 clinical and 3 ECG-gated SPECT). Notably, LVEF, age, AC-SSS > 8, and pharmacologic stress were the four most powerful predictors of cardiac death or non-fatal MI followed by history of tobacco use, diabetes mellitus, known CAD, and AC-SSS 1-8 (Table 2). The addition of the AC-SSS to the model significantly increased the global χ 2 over clinical variables (314-336, P < .01).
Discussion
To our knowledge, this is the first large study investigating line source AC in a general population who underwent rest/stress ECG-gated stress MPI for clinical indications. In the evaluation of AC, the most important impact was in patients who had mild perfusion abnormalities. After AC, over 88% of studies in this category were considered to be normal (SSS of 0 with AC). The value of this finding was supported by the very low event rate of all patients with SSS of 0 (1% annually). In contrast, those patients whose study remained in the 1-3 SSS category had a significantly higher event rate that also was comparable to the previous risk category of SSS 4-8. There was no significant difference in the event rate of patients in the moderate-severe category (SSS > 8). Thus, our study demonstrates the value of line source AC in successful risk stratification based upon the size and severity of the perfusion abnormality. Of considerable importance was the finding of a low cardiac event rate in patients with completely normal studies after AC, confirming that significant CAD is not missed. In contrast, identification of higher cardiac event rates in patients heretofore considered in the normal category suggests that CAD is associated with even mild attenuation-corrected results. These data give further evidence of the clinical value of AC in SPECT MPI.
The role of stress nuclear MPI in risk stratification is well established21-28 and our current findings are in agreement with these previous observations, demonstrating the highest cardiac risk in patients with moderate to severe perfusion abnormalities and the lowest risk in those with normal studies. From a diagnostic standpoint, however, soft-tissue attenuation artifact affects both accuracy of image interpretations, and ultimately the confidence of the referring physician. AC, using either radionuclide line source or CT methods, has facilitated interpretation of MPI studies by removing most artifacts and resulting in improved specificity and diagnostic accuracy.2-10 These studies have uniformly supported improved diagnostic accuracy. Further, studies have demonstrated that combined ECG-gated SPECT and line source AC have a synergistic impact on improving SPECT diagnostic accuracy.5,18,29-31 Despite the benefits of AC with image interpretation, acceptance of these methods as a routine for SPECT MPI has been slow. While partially due to reimbursement issues, the lack of prognostic data has been a factor.12 Thus, demonstration that attenuation-corrected images present the same risk stratification information, or better could be an important advancement to gain acceptance of these methodologies within the nuclear cardiology community.
Several studies have demonstrated the prognostic value of line source AC and a normal imaging result in low risk patients.2,13,32-34 These data are important to reassure users that there is not a systematic “over-correction” using these methods such that a previously abnormal study without AC that becomes normal with AC does not represent more CAD. The present study extends these data with a very low event rate in patients with completely normal results. Of equal importance is the performance of AC in the daily operation of a laboratory, rather than selected cases. Only two studies have reported on the impact of AC upon outcomes in unselected patients who underwent rest/stress SPECT MPI.14,15 Pazhenkottil et al14 used a CT-based AC while Baghdasarian et al15 used line source AC in consecutive patients in whom ECG-gating was not technically feasible because of arrhythmia. Both of these studies, in a relatively small number of patients, demonstrated that SPECT MPI with AC provides powerful risk stratification when added to clinical variables. Our study extends these earlier observations in a large, clinically referred patient population in which AC was a routine in all patients. Results from this study suggest that line source AC with rest/stress ECG-gated SPECT MPI provides homogenous count distribution and shifts the SSS to a lower value in identifying at-risk patients (≥4 without AC vs ≥1 with AC), likely due to a reduction in the number of false-positive images. An equally important aspect was that both mild and moderate to severe perfusion abnormalities after AC emerged as independent predictors of adverse cardiac events and these risk stratification cutoffs proved effective in both women and men. Importantly, our study confirms that patients with small/mild defects remaining after AC (AC-SSS 1-3) are at increased cardiac risk as compared to those with completely normal results. This finding suggests that any perfusion abnormality remaining after AC is consistent with CAD, not attenuation artifact, and thus consideration should be given to treatment strategies.
One of the clinical concerns with AC is the overcorrection and the potential false negative imaging result which might lead to a higher cardiac event rate in patients with normal AC SPECT perfusion. In our study, approximately 58% of imaging studies with abnormal perfusion normalized after application of AC. Despite a substantially larger number of patients with completely normal perfusion after AC (AC-SSS = 0), a similar low annualized cardiac event rate with or without AC was observed. The ability of AC to identify additional low risk patients on a routine basis should lead to an overall decrease in the cost of patient care through a reduction in referrals for cardiac catheterization and improvement of laboratory utilization.35 A previous concern about AC solutions has included the possibility that use of these devices may underestimate the extent and severity of perfusion abnormalities. An important aspect of our study was a demonstration of similar and significantly higher cardiac event rates in patients with moderate to severe perfusion abnormalities on either non-attenuation-corrected or attenuation-corrected imaging. This finding again reinforces the prognostic value of line source AC in all patients undergoing this procedure.
Study Limitations
Our observations are based on a single-center evaluation. However, our study population was large and diverse. Although data were prospectively collected, this study is retrospective with the possibility of unknown confounders. All images were interpreted in sequence; non-attenuation-corrected data first followed by attenuation-corrected images. Results of both were provided to the referring physician, although the conclusion was based upon the attenuation-corrected images which may have biased the physician with regards to further testing and medication changes.
New Knowledge Gained
The low event rate with a normal attenuation-corrected study provides confidence in the use of the procedure. The higher event rates than in normal studies for patients with mild perfusion abnormalities suggests the presence of CAD, and could impact clinical decisions.
Conclusion
The use of line source AC with ECG-gated rest/stress SPECT MPI provides highly effective and incremental risk stratification for future adverse cardiac events.
References
Patel MR, Peterson ED, Dai D, Brennan JM, Redberg RF, Anderson HV, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med 2010;362:886-95.
Heller GV, Bateman TM, Johnson LL, Cullom SJ, Case JA, Galt JR, et al. Clinical value of attenuation correction in stress-only Tc-99m sestamibi SPECT imaging. J Nucl Cardiol 2004;11:273-81.
Hendel RC, Berman DS, Cullom SJ, Follansbee W, Heller GV, Kiat H, et al. Multicenter clinical trial to evaluate the efficacy of correction for photon attenuation and scatter in SPECT myocardial perfusion imaging. Circulation 1999;99:2742-9.
Kluge R, Sattler B, Seese A, Knapp WH. Attenuation correction by simultaneous emission-transmission myocardial single-photon emission tomography using a technetium-99m-labelled radiotracer: Impact on diagnostic accuracy. Eur J Nucl Med 1997;24:1107-14.
Links JM, DePuey EG, Taillefer R, Becker LC. Attenuation correction and gating synergistically improve the diagnostic accuracy of myocardial perfusion SPECT. J Nucl Cardiol 2002;9:183-7.
Ficaro EP, Fessler JA, Shreve PD, Kritzman JN, Rose PA, Corbett JR. Simultaneous transmission/emission myocardial perfusion tomography. Diagnostic accuracy of attenuation-corrected 99mTc-sestamibi single-photon emission computed tomography. Circulation 1996;93:463-73.
Gallowitsch HJ, Sykora J, Mikosch P, Kresnik E, Unterweger O, Molnar M, et al. Attenuation-corrected thallium-201 single-photon emission tomography using a gadolinium-153 moving line source: Clinical value and the impact of attenuation correction on the extent and severity of perfusion abnormalities. Eur J Nucl Med 1998;25:220-8.
Slart RH, Que TH, van Veldhuisen DJ, Poot L, Blanksma PK, Piers DA, et al. Effect of attenuation correction on the interpretation of 99mTc-sestamibi myocardial perfusion scintigraphy: The impact of 1 year’s experience. Eur J Nucl Med Mol Imaging 2003;30:1505-9.
Masood Y, Liu YH, Depuey G, Taillefer R, Araujo LI, Allen S, et al. Clinical validation of SPECT attenuation correction using x-ray computed tomography-derived attenuation maps: Multicenter clinical trial with angiographic correlation. J Nucl Cardiol 2005;12:676-86.
Utsunomiya D, Tomiguchi S, Shiraishi S, Yamada K, Honda T, Kawanaka K, et al. Initial experience with X-ray CT based attenuation correction in myocardial perfusion SPECT imaging using a combined SPECT/CT system. Ann Nucl Med 2005;19:485-9.
Heller GV, Links J, Bateman TM, Ziffer JA, Ficaro E, Cohen MC, et al. American Society of Nuclear Cardiology and Society of Nuclear Medicine joint position statement: Attenuation correction of myocardial perfusion SPECT scintigraphy. J Nucl Cardiol 2004;11:229-30.
Germano G, Slomka P, Berman DS. Attenuation correction in cardiac SPECT: The boy who cried wolf? J Nucl Cardiol 2007;14:25-35.
Gibson PB, Demus D, Noto R, Hudson W, Johnson LL. Low event rate for stress-only perfusion imaging in patients evaluated for chest pain. J Am Coll Cardiol 2002;39:999-1004.
Pazhenkottil AP, Ghadri JR, Nkoulou RN, Wolfrum M, Buechel RR, Kuest SM, et al. Improved outcome prediction by SPECT myocardial perfusion imaging after CT attenuation correction. J Nucl Med 2011;52:196-200.
Baghdasarian SB, Noble GL, Ahlberg AW, Katten D, Heller GV. Risk stratification with attenuation corrected stress Tc-99m sestamibi SPECT myocardial perfusion imaging in the absence of ECG-gating due to arrhythmias. J Nucl Cardiol 2009;16:533-9.
Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med 1979;300:1350-8.
Henzlova MJ, Cerqueira MD, Mahmarian JJ, Yao SS. Stress protocols and tracers. J Nucl Cardiol 2006;13:e80-90.
Tan P, Bailey DL, Meikle SR, Eberl S, Fulton RR, Hutton BF. A scanning line source for simultaneous emission and transmission measurements in SPECT. J Nucl Med 1993;34:1752-60.
Case JA, Hsu BL, Bateman TM, Cullom SJ. A Bayesian iterative transmission gradient reconstruction algorithm for cardiac SPECT attenuation correction. J Nucl Cardiol 2007;14:324-33.
Hansen CL, Goldstein RA, Berman DS, Churchwell KB, Cooke CD, Corbett JR, et al. Myocardial perfusion and function single photon emission computed tomography. J Nucl Cardiol 2006;13:e97-120.
Berman DS, Hachamovitch R, Kiat H, Cohen I, Cabico JA, Wang FP, et al. Incremental value of prognostic testing in patients with known or suspected ischemic heart disease: A basis for optimal utilization of exercise technetium-99m sestamibi myocardial perfusion single-photon emission computed tomography. J Am Coll Cardiol 1995;26:639-47.
Hachamovitch R, Berman DS, Kiat H, Cohen I, Cabico JA, Friedman J, et al. Exercise myocardial perfusion SPECT in patients without known coronary artery disease: Incremental prognostic value and use in risk stratification. Circulation 1996;93:905-14.
Hachamovitch R, Berman DS, Kiat H, Cohen I, Lewin H, Amanullah A, et al. Incremental prognostic value of adenosine stress myocardial perfusion single-photon emission computed tomography and impact on subsequent management in patients with or suspected of having myocardial ischemia. Am J Cardiol 1997;80:426-33.
Heller GV, Herman SD, Travin MI, Baron JI, Santos-Ocampo C, McClellan JR. Independent prognostic value of intravenous dipyridamole with technetium-99m sestamibi tomographic imaging in predicting cardiac events and cardiac-related hospital admissions. J Am Coll Cardiol 1995;26:1202-8.
Iskandrian AS, Chae SC, Heo J, Stanberry CD, Wasserleben V, Cave V. Independent and incremental prognostic value of exercise single-photon emission computed tomographic (SPECT) thallium imaging in coronary artery disease. J Am Coll Cardiol 1993;22:665-70.
Nallamouthu N, Araujo L, Russell J, Heo J, Iskandrian AE. Prognostic value of simultaneous perfusion and function assessment using technetium-99m sestamibi. Am J Cardiol 1996;78:562-4.
Zanco P, Zampiero A, Favero A, Borsato N, Chierichetti F, Rubello D, et al. Myocardial technetium-99m sestamibi single-photon emission tomography as a prognostic tool in coronary artery disease: Multivariate analysis in a long-term prospective study. Eur J Nucl Med 1995;22:1023-8.
Navare SM, Mather JF, Shaw LJ, Fowler MS, Heller GV. Comparison of risk stratification with pharmacologic and exercise stress myocardial perfusion imaging: A meta-analysis. J Nucl Cardiol 2004;11:551-61.
Thompson RC, Heller GV, Johnson LL, Case JA, Cullom SJ, Garcia EV, et al. Value of attenuation correction on ECG-gated SPECT myocardial perfusion imaging related to body mass index. J Nucl Cardiol 2005;12:195-202.
Links JM, Becker LC, Rigo P, Taillefer R, Hanelin L, Anstett F, et al. Combined corrections for attenuation, depth-dependent blur, and motion in cardiac SPECT: A multicenter trial. J Nucl Cardiol 2000;7:414-25.
Taneja S, Mohan HK, Blake GM, Livieratos L, Clarke SE. Synergistic impact of attenuation correction and gating in routine myocardial SPECT reporting: 2 year follow-up study. Nucl Med Commun 2008;29:390-7.
Chang SM, Nabi F, Xu J, Raza U, Mahmarian JJ. Normal stress-only versus standard stress/rest myocardial perfusion imaging: Similar patient mortality with reduced radiation exposure. J Am Coll Cardiol 2010;55:221-30.
Duvall WL, Wijetunga MN, Klein TM, Razzouk L, Godbold J, Croft LB, et al. The prognosis of a normal stress-only Tc-99m myocardial perfusion imaging study. J Nucl Cardiol 2010;17:370-7.
Mathur S, Heller G, Bateman T, Ruffin R, Yekta A, Katten D, et al. Clinical value of stress-only Tc-99m SPECT imaging: Importance of attenuation correction. J Nucl Cardiol 2013;20:27-37.
Hendel RC. Attenuation correction: Eternal dilemma or real improvement? Q J Nucl Med Mol Imaging 2005;49:30-42.
Disclosures
This study was supported by an investigator-initiated research grant from Philips Medical Systems, Cleveland, OH. The company Philips Medical Systems had no role in the design and conduct of the study collection, management, analysis, and interpretation of the data and preparation, review, or approval of the manuscript. We wish to acknowledge the following financial agreements: G.V. Heller: Grant/honoraria/research support from Philips Medical Systems; T.M. Bateman: Royalty from ExSPECT software for attenuation correction and research support from Philips Medical Systems and GE Healthcare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ardestani, A., Ahlberg, A.W., Katten, D.M. et al. Risk stratification using line source attenuation correction with rest/stress Tc-99m sestamibi SPECT myocardial perfusion imaging. J. Nucl. Cardiol. 21, 118–126 (2014). https://doi.org/10.1007/s12350-013-9816-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-013-9816-x