Abstract
Background
We analysed factors that might influence patients’ and physicians’ decisions against the initiation of guideline adherent adjuvant endocrine therapy (ET).
Methods
In a prospective multi-centre study, including four certified breast cancer centres in Germany, patients with primary breast cancer were included from 2009 to 2012. Patients completed a questionnaire prior to surgery, adjuvant therapy, and 6 months after adjuvant therapy. This questionnaire assessed health-related quality of life (QoL), psychiatric co-morbidity, demographic characteristics, and the intensity of fear for ET. Guideline adherence was classified based on an algorithm derived from international guidelines. The tumour board’s (TB) decisions against or for ET was documented. The TB was blinded regarding the guideline results.
Results
In 666 patients, adjuvant ET was indicated according to the guideline recommendations. The TB decided in 92.3 % (n = 615) of those that adjuvant ET was indicated. TB’s decision against ET was associated with the younger age of patients (OR = 0.5; 95 % CI 0.3–0.9) and poor QoL (OR = 1.7; 95 % CI 1.0–2.8). In 93 patients, ET was not indicated according to the guidelines, and the TB decided in 84 of those not to prescribe ET. The TB decided in 93.4 % of the cases according to the guidelines. Of the patients, where the TB prescribed ET, 5 % (n = 31) decided against ET. This decision was associated with fear of ET (OR = 2.2; 95 % CI 1.0–5.2) and higher age (OR 9; 95 % CI 1.0–48.1). Psychiatric co-morbidity (OR = 1.8; 95 % CI 0.7–4.2), poor QoL (OR = 0.4; 95 % CI 0.2–1.2), and education (OR = 1.2; 95 % CI 0.5–2.6) were not associated with the decision.
Discussion
Guideline adherent implementation of adjuvant ET is high. Physicians’ decision against ET is mainly associated with patients’ younger age and poor quality of life, whereas patients’ decision, once the TB decided to initiate ET and if ET is indicated by guidelines, is associated with higher age and fear of ET.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer among women worldwide and is still associated with remarkable morbidity and mortality. Annual frequency of new cases with invasive breast cancer amounts to 75.000 in Germany [1]. Certainly, despite rising frequency, survival rates have been steadily improved due to ameliorated screening with the earlier detection of invasive cancer and multimodal treatment options [2, 3]. Besides chemo- or targeted therapies, it is widely known that the long-term application of endocrine therapy for patients with hormone receptor positive breast cancer is one of those major treatment components. In addition, randomized breast cancer studies, as well as rising effort for quality assurance in breast cancer treatment by the implementation of certified breast cancer centres, are important features for past and future amendments in breast cancer treatment [4]. Especially, the adherence to current guidelines help to improve the outcome of patients, yet only about 70 % of all patients with breast cancer in Canada undergo guideline adherent therapy [5]. Reasons for guideline adherent treatment deviations are multifarious. Although co-morbidities are considered to be the leading cause for rejections of indicated therapies, there are still several influencing factors on the treatment decision of TB and/or patients that are not fully described and understood. The BRENDA study group reported recently that a relevant part (19 %) of an indicated adjuvant systemic therapy (AST) was not used due to poor QoL or fear for chemotherapy [6].
Following these observations, the objective of this prospective BRENDA II study is to evaluate patient- and physician-related factors that are associated with non-prescription of ET and with non-taking of ET although it was prescribed by the tumour board and indicated according to guidelines in patients with primary breast cancer.
Patients and methods
Patients with primary breast cancer were sampled consecutively over a period of 4 years (01.01.2009–31.12.2012) in four German breast cancer centres, all certified by the German Cancer Society.
Patients were eligible for the study if they were diagnosed with primary, histologically confirmed breast cancer. Exclusion criteria were metastatic disease, recurrent disease, bilateral breast cancer, primary occult disease, phyllodes tumour, or missing informed consent.
Eligible patients were informed about the study by their consultant and then asked to complete a questionnaire prior to surgery (t1), before initiating an adjuvant therapy (t2), and 6 months after the completion of adjuvant therapy (t3). We collected data at the University Medical Centre in Ulm, Kempten Hospital, Memmingen Hospital, and Esslingen Hospital with the help of specially trained breast care nurses. Ethical approval was obtained from the Ethics Committee of the University of Ulm.
Instruments
Demographic data (e.g., age) were provided by the patients, while clinical data were obtained from medical records by trained data managers.
Co-morbid somatic diseases were documented and subsequently coded according to the Charlson co-morbidity index [7]. This index assigns weights to diseases depending on the risk of dying from the disease. A sum score ≥ 3 was considered to be a “severe somatic co-morbidity”.
We evaluated psychiatric co-morbidity using the German version of the Patient Health Questionnaire (PHQ) [8], a self-administered instrument assessing psychiatric syndromes according to the criteria of the ICD-10. The PHQ has been validated using the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders as the gold standard [9].
Quality of life (QoL) was ascertained using the European Organization for Research and Treatment of Cancer Core Instrument (EORTC QLQ-C30) [10]. This is a self-administered questionnaire assessing different dimensions of QoL. Patients were grouped into “poor QoL” (versus “good QoL”) if their global QoL score at t1 exceeded the 75th percentile of the general German population’s age- and sex-specific norms [11].
Fear of ET was measured by asking the patient: “How much are you afraid of endocrine therapy?” (“not at all” to “very much” on a 4-point Likert scale). We also asked whether fears about ET had been evoked by consultations with general practitioners and/or gynaecologists and how often patients had heard about negative experiences with ET from friends or family. Furthermore, we enquired how much the patients associate with ET: weight gain, change of voice, hot flashes, dry vagina, decrease of bone mineral density, pain in the joints, and decrease of libido (“not at all” to “very much” on a 4-point Likert scale).
Wolters et al. demonstrated that guideline recommendations in internationally validated guidelines differ only marginally [12]. For this reason, we used the German national S3-guideline for diagnosis, treatment, and follow-up care in breast cancer (2008 version) [13] to classify ET indication. Risk group classification is based on St. Gallen criteria [14].
Statistical analysis
Statistical analysis included the evaluation of absolute and relative frequencies of treatment decisions regarding ET.
Potential predictors of deviations from guidelines and from treatment decisions were analysed using multivariate logistic regressions. Effect modification was tested using the likelihood ratio tests.
We considered the following variables as potentially relevant predictors: age at study entry (≥45 years vs <45 years), education (≥10 years vs <10 years of schooling), somatic co-morbidity (severe vs no severe), psychiatric co-morbidity (yes vs no), global QoL at t2 (poor vs good QoL), and fear of ET at t1 (high vs low). All variables were entered simultaneously into the model.
As this is an explorative study, we have chosen not to employ the term “statistically significant” or to use a threshold p-value, but rather present p-values to discuss differences that cannot be explained by random variation only.
Results
857 patients of a daily routine collective with primary breast cancer were enrolled in the study; of those, 849 met the inclusion criteria and were contacted for participation. Since 90 patients declined participation or could not be included due to dementia or language problems, 759 patients participated in this study (Fig. 1). The majority of the patients was 45 years of age or older (87 %), and had intermediate risk (75 %). 42 (6 %) patients had severe somatic co-morbidity, all of them being 45 years or older. As none of the patients <45 years suffered from severe somatic co-morbidity, this variable could not be entered in the multivariate regression models later on. Psychiatric co-morbidity was prevalent in 21 % of all patients (Table 1). 134 (17.6 %) patients reported to be very afraid of ET. 30 % of all patients said they had heard about negative experiences with ET from friends or family. Of those who had heard no negative experiences, only 16 % were very afraid of ET, whereas those who heard very often negative experiences, 62 % were afraid of ET (p < 0.001). 39 % of all patients reported that consultations with their general practitioner and/or gynaecologist had evoked anxieties about ET. Of those who said the consultation had provoked no anxieties, 11 % had intense fear of ET, whereas in those who said the consultation had provoked intense anxieties, 79 % were very afraid of ET. The negative side effect most often associated with ET was weight gain (mean 2.8), followed by hot flashes (2.6), decrease of bone mineral density (2.3), and dry vagina (2.3). All negative associations were more frequent in patients with intense fear of ET (all p < 0.001). There was no difference in fear of ET between younger and older patients (p = 0.34).
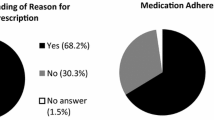
In 81.9 % (n = 622) of patients, the tumour board decided to apply ET, while in 14 % (n = 106), the TB decided not to initiate ET. In 4.1 % (n = 31), no decision on ET by the tumour board is documented. According to the current guidelines, 666 patients should have received an indication for ET, which means that the TB yet voted against ET in 3.3 %. The TB’s decision to avoid ET was more frequent in patients with poor quality of life (OR 1.7; 95 % CI 1.0–2.8) and less frequent in patients with an age ≥45 years (OR 0.5; 95 % CI 0.3–0.9). By contrast, psychological co-morbidity (OR 0.7; 95 % CI 0.4–1.2), fear of ET (OR 0.8; 95 % CI 0.4–1.4), and higher education (OR 0.7; 95 % CI 0.4–1.0) did not play any independent role for the decision-making process of the TB. After TB decision to initiate ET, 5 % (n = 31) patients declined their application. Patients did decline more often when they had intense fear regarding this treatment (OR 2.2; 95 % CI 1.0–5.2) and when they were 45 years or older (OR 9.0; 95 % CI 1.0–84.1). Psychiatric co-morbidity (OR 0.1.8; 95 % CI 0.7–4.2), poor quality of life (OR 0.4; 95 % CI 0.2–1.2), and education (OR 1.2; 95 % CI 0.5–2.6) were not associated with the patients` decision against ET (Table 2).
Discussion
Since the prognosis of patients with breast cancer directly depends on the guideline adherence of treatment decisions, the intention of the BRENDA study group is to estimate frequency of non-adherence and to evaluate underlying factors for deviating from recommendations. There are several studies showing that the disobeyance of guidelines might lead to unfavourable prognosis, and increasing effort should be made to further improve guideline adherent treatment decisions [5, 10, 15–17].
Concerning the application of ET in the adjuvant situation of primary breast cancer, there are several recommendations according to current guidelines [18–20]. Moreover, it is widely known that the application of Tamoxifen for 10 years rather than for 5 years has tremendous effects on the outcome of women with oestrogen receptor positive breast cancer [21, 22]. The compliance of patients is a general basis for the achievements of this long-lasting therapy. Referring to this, several studies addressed the compliance during the application of ET [23, 24]. We analysed factors that might influence patients’ and physicians’ decisions towards the initiation of guideline adherent adjuvant endocrine therapy. Based on our inquiries, TB decision voted against ET in 3.3 %, in those cases, where therapy would have been indicated according to the guidelines. The main factor associated with their decision was younger age of patients and poor quality of life, whereas the patients’ fear of ET or education did not play a role. 5 % of all patients that would have been suitable for ET based on guideline recommendation and TB decision rejected any endocrine therapy. This was mainly related with the patients’ age and fear of therapy. These patients’ risk to have an unfavourable prognosis by rejecting an indicated guideline adherent ET as several studies were able to demonstrate. Interestingly, the rejection of an indicated therapy by the patient was scarcer for ET than for adjuvant chemotherapy [25]. As we reported previously, around 19 % of patients that should have been treated with adjuvant chemotherapy (CT) declined the initiation of therapy. Their decision against CT was associated with poor QoL in elderly patients (≥75 years) and with fear of CT in patients with intermediate risk [6]. Obviously, guideline adherence for adjuvant therapy can be improved to achieve the best possible outcome for patients, even though there is no doubt that 100 % guideline adherence might be difficult to reach. Referring to the kind of adjuvant therapy, physicians will be challenged with information to break down prejudices and fears for adjuvant therapies. In this case, not only the decision for the initiation of ET but also the consequent application over years should be addressed. Indeed, the compliance during therapy might play a superior role with regard to the quantification of decline of the therapy, when compared to the compliance for the initiation of ET. However, to improve both these crucial points, various efforts in the field of patient education and the management of adverse events are required. There are several studies showing that the compliance of patients concerning a long-lasting treatment with ET needs creative, multi-layered approaches [26–28]. Our findings suggest that especially potential fear of ET should be addressed by the doctors, as fears can easier be changed than co-morbid diseases. In general, fear of ET is relatively low in breast cancer patients compared to fear of CT [6]. However, addressing this problem in those with increased anxiety could improve guideline adherence considerable.
There are, of course, several strengths and limitations in the study. A major limitation is that several potential confounders (urban areas/negative experience with medical services) that were not assessed by the questionnaire due to limited capacity or the lack of validated questionnaires. Furthermore, we did not investigate if guideline adherence is associated with improved survival due to the short follow-up of the study and results are restricted to certified centres with TBs. There are also several strengths of the presented study. Improved documentation quality was achieved by specially trained physicians and breast care nurses who interviewed the participants. In addition, the prospective design of the study reduced the likelihood of information bias; physicians were blinded concerning the guideline-based algorithm, and internationally validated instruments were used to measure predictors of treatment decisions and applications.
Conclusion
In summary, guideline adherence concerning recommendations for the initiation of ET in patients with primary breast cancer is high. Patients’ decision to reject an indicated and prescribed ET is related to their age and fear for complications, while physicians more frequently decide against ET if patients have a poor quality of life and when elderly patients are affected. The new insight we obtain from this study is that it is still necessary to improve education of patients and the general population to prevent non-adherence due to anxiety and to steadily improve patients’ outcome.
References
RKI, Breast cancer incidence, Germany. 2014, Robert-Koch-Institute, Tumor Registry.
Fracheboud J, et al. Decreased rates of advanced breast cancer due to mammography screening in The Netherlands. Br J Cancer. 2004;91(5):861–7.
Hanrahan EO, et al. Overall survival and cause-specific mortality of patients with stage T1a, bN0M0 breast carcinoma. J Clin Oncol. 2007;25(31):4952–60.
Kowalski C, et al. Quality of care in breast cancer centers: results of benchmarking by the German Cancer Society and German Society for Breast Diseases. Breast. 2015;24(2):118–23.
Hebert-Croteau N, et al. Compliance with consensus recommendations for systemic therapy is associated with improved survival of women with node-negative breast cancer. J Clin Oncol. 2004;22(18):3685–93.
Schwentner L, Van Ewijk R, Kühn T, Flock F, Felberbaum R, Blettner M, Kreienberg R, Janni W, Wöckel A, Singer S. Exploring patient- and physician-related factors preventing breast cancer patients from guideline-adherent adjuvant chemotherapy-results from the prospective multi-center study BRENDA II. Support Care Cancer. 2016;24(6):2759–66. doi:10.1007/s00520-016-3088-3.
D’Hoore W, Sicotte C, Tilquin C. Risk adjustment in outcome assessment: the Charlson comorbidity index. Methods Inf Med. 1993;32(5):382–7.
Löwe BSR, Zipfel S, Herzog W. PHQ-D Gesundheitsfragebogen für Patienten. Manual. Karlsruhe: Pfizer; 2002.
Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–66.
Wockel A, et al. The impact of adjuvant radiotherapy on the survival of primary breast cancer patients: a retrospective multicenter cohort study of 8935 subjects. Ann Oncol. 2014;25(3):628–32.
Schwarz R, Hinz A. Reference data for the quality of life questionnaire EORTC QLQ-C30 in the general German population. Eur J Cancer. 2001;37(11):1345–51.
Wolters R, et al. A comparison of international breast cancer guidelines—do the national guidelines differ in treatment recommendations? Eur J Cancer. 2012;48(1):1–11.
Kreienberg R, Kopp I, Albert U. Interdisciplinary S3 guideline for diagnosis and therapy of breast cancer in women. German cancer society, 2008.
Goldhirsch A, et al. Progress and promise: highlights of the international expert consensus on the primary therapy of early breast cancer 2007. Ann Oncol. 2007;18(7):1133–44.
Schwentner L, et al. Triple-negative breast cancer: the impact of guideline-adherent adjuvant treatment on survival–a retrospective multi-centre cohort study. Breast Cancer Res Treat. 2012;132(3):1073–80.
Wolters R, et al. Comparing the outcome between multicentric and multifocal breast cancer: what is the impact on survival, and is there a role for guideline-adherent adjuvant therapy? A retrospective multicenter cohort study of 8,935 patients. Breast Cancer Res Treat. 2013;142(3):579–90.
Schwentner L, et al. Survival of patients with bilateral versus unilateral breast cancer and impact of guideline adherent adjuvant treatment: a multi-centre cohort study of 5292 patients. Breast. 2012;21(2):171–7.
Harbeck N, Thomssen C, Gnant M. St. Gallen 2013: brief preliminary summary of the consensus discussion. Breast Care (Basel). 2013;8(2):102–9.
Untch M, et al. 13th st. Gallen international breast cancer conference 2013: primary therapy of early breast cancer evidence, controversies, consensus—opinion of a german team of experts (zurich 2013). Breast Care (Basel). 2013;8(3):221–9.
Curigliano G, et al. Highlights from the 13th St Gallen International Breast Cancer Conference 2013. Access to innovation for patients with breast cancer: how to speed it up? Ecancermedicalscience. 2013;7:299.
Gray R. aTTom: Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years in 6,953 women with early breast cancer. J Clin Oncol. 2013; 31(suppl; abstract 5).
Davies C, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381(9869):805–16.
Fasching PA, et al. Evaluation of therapy management and patient compliance in postmenopausal patients with hormone receptor-positive breast cancer receiving letrozole treatment: the evaluateTM study. Geburtshilfe Frauenheilkd. 2014;74(12):1137–43.
Wuensch P, et al. Discontinuation and non-adherence to endocrine therapy in breast cancer patients: is lack of communication the decisive factor? J Cancer Res Clin Oncol. 2015;141(1):55–60.
Fisher B, et al. Tamoxifen, radiation therapy, or both for prevention of ipsilateral breast tumor recurrence after lumpectomy in women with invasive breast cancers of one centimeter or less. J Clin Oncol. 2002;20(20):4141–9.
Hadji P, et al. The Patient’s Anastrozole Compliance to Therapy (PACT) Program: a randomized, in-practice study on the impact of a standardized information program on persistence and compliance to adjuvant endocrine therapy in postmenopausal women with early breast cancer. Ann Oncol. 2013;24(6):1505–12.
Ziller V, et al. Adherence to adjuvant endocrine therapy in postmenopausal women with breast cancer. Ann Oncol. 2009;20(3):431–6.
Neven P, et al. The impact of educational materials on compliance and persistence rates with adjuvant aromatase inhibitor treatment: first-year results from the compliance of aromatase inhibitors assessment in daily practice through educational approach (CARIATIDE) study. Breast. 2014;23(4):393–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there are no potential conflicts of interest, including financial, personal, or relationship with other people or organizations that could inappropriately influence this work.
Funding source
Parts of this work were supported by the German Federal Ministry of Education and Research (BMBF-Grant-01ZP0505).
Ethical approval
This study and the BRENDA project have been approved by the ethics committee of the University of Ulm.
Additional information
For the BRENDA study group.
About this article
Cite this article
Stüber, T., van Ewijk, R., Diessner, J. et al. Which patient- and physician-related factors are associated with guideline adherent initiation of adjuvant endocrine therapy? Results of the prospective multi-centre cohort study BRENDA II. Breast Cancer 24, 281–287 (2017). https://doi.org/10.1007/s12282-016-0701-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-016-0701-8