Abstract
Mitochondrial dysfunction caused by oxidative stress appears at early stages of aging and age-related diseases. Plasma membrane redox enzymes act in a compensatory manner to decrease oxidative stress and supply reductive capacity to ensure cell survival. Plasma membrane redox enzymes transfer electrons from NAD(P)H to oxidized ubiquinone and α-tocopherol, resulting in inhibition of further oxidative damage. Plasma membrane redox enzymes and their partners are affected by aging, leading to progression of neurodegenerative disease pathogenesis. Up-regulating plasma membrane redox enzymes via calorie restriction and phytochemicals make cells more resistant to oxidative damage under stress conditions by maintaining redox homeostasis and improving mitochondrial function. Investigation into plasma membrane redox enzymes can provide mechanistic details underlying the relationships between plasma membrane redox enzymes and mitochondrial complexes and provide a good therapeutic target for prevention and delay of neurodegenerative disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neurodegenerative disorders such as Alzheimer’s disease (AD) and Parkinson’s disease (PD) are considered age-related diseases since their incidence is correlated with age. During the aging process, cellular and physiological functions in neurons are inevitably attenuated (Miller and Shukitt-Hale 2012; Fernandez del Rio et al. 2016). Deterioration is represented by imbalanced redox homeostasis, impaired energy metabolism, and apoptotic cell death (Braidy et al. 2008; Johannesson et al. 2012; Anandhan et al. 2017). In fact, aging is a stochastic, complex, unavoidable, and irreversible degenerative process (Hayflick 2000). Aging can be explained by several, closely connected theories, including the genetic theory (Le Bourg 2014; Wang et al. 2014), the telomere shortening theory (Tumpel and Rudolph 2012; Zhu et al. 2018), the free radical theory (Liochev 2013; Barja 2014; Koltover 2017), and the mitochondrial dysfunction theory (Kong et al. 2014; Faitg et al. 2017; Grimm and Eckert 2017).
Plasma membrane redox enzymes and their partners
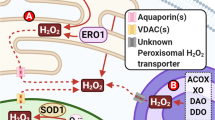
Plasma membrane redox enzymes are NADH-dependent enzymes located on the inner surface of the plasma membrane and require an intracellular electron donor (NAD(P)H) and antioxidant molecules (coenzyme Q (CoQ) and α-tocopherol) for electron transport (Hyun et al. 2006a) (Fig. 1). NAD(P)H is a universal electron donor in the cytosol and is produced by glycolysis and in the mitochondria by the citric acid cycle. CoQ is found in micro-organelles including the plasma membrane and mitochondria and is present in three different forms: oxidized CoQ, a semi-quinone radical (CoQ·−), and reduced CoQ. The reduced form of CoQ (ubiquinol) can scavenge superoxide (O ·−2 ) or lipid radicals alone or in association with α-tocopherol, leading to inhibition of lipid peroxidation propagation and formation of CoQ·− (Crane 2001; Turunen et al. 2004). The semi-quinone radical is converted to ubiquinol by plasma membrane redox enzymes.
Plasma membrane redox enzymes are essentially NADH-dependent enzymes and include cytochrome b5 reductase (b5R) (Marques-da-Silva et al. 2010; Samhan-Arias et al. 2018), NADH-quinone oxidoreductase 1 (NQO1) (Chan et al. 2002; Gray et al. 2011; Ross and Siegel 2017), NADH-ferricyanide reductase (Baker et al. 2004), and NADH-CoQ reductase (Germinario et al. 2000). b5R (EC 1.6.5.5, also called ascorbate free radical reductase) is a 32-kDa FAD-containing monomeric enzyme and is involved in the transfer of one electron from NADH to CoQ in the plasma membrane, forming CoQ·− (Matsuda et al. 2000; Bewley et al. 2001). NQO1 (EC 1.6.99.2, also known as DT-diaphorase) is a 33-kDa homodimeric enzyme with a non-covalently bound FAD (Pey et al. 2016; Ross and Siegel 2017; Chhetri et al. 2018). NQO1 is an important enzyme in the plasma membrane because it does not produce free radicals during electron transport, uses both NADH and NADPH as electron donors, and is induced by oxidative stress. NQO1 is responsible for the transfer of two electrons, resulting in no semi-quinone radicals (Gong et al. 2008; Jaber and Polster 2015). NQO1 is induced through the NF-E2-related factor 2 (Nrf2)-Keap1 pathway (Gan et al. 2013) (Fig. 2). Under normal conditions, Nrf2 is bound to Keap1 and then degraded by the proteasome. However, oxidative stress breaks disulfide bonds in the Nrf2–Keap1 complex, leading to dissociation of Nrf2 (Jaiswal 2000; Nioi and Hayes 2004). Free Nrf2 is translocated into the nucleus and bound to c-Jun. The Nrf2-c-Jun complex can attach to antioxidant response elements and induce detoxifying enzymes, which include NQO1.
Neuroprotective mechanisms induced by PM redox enzymes. Electron flows are shown in red, and neuroprotective roles of CR and phytochemicals are marked with orange arrows. ARE antioxidant response element, b5R cytochrome b5 reductase, CoQH2 reduced form of coenzyme Q, CR calorie restriction, CREB cAMP response element, ETS electron transport system, FOXO3 Forkhead box family of transcription factors, NQO1 NADH-quinone oxidoreductase, Nrf2 NF-E2-related factor 2, PKC protein kinase C
Plasma membrane redox enzymes and their functions
The plasma membrane is a very important micro-organelle since it acts as a front line for regulating cellular physiology, such as hormonal and neuronal signaling. It also plays a key role in protection against external oxidative insults (del Castillo-Olivares et al. 2000; Ly and Lawen 2003; Reddy et al. 2017).
Electrons taken from intracellular NAD(P)H by the plasma membrane redox enzymes are transferred to CoQ, leading to neutralization of extracellular oxidative molecules such as ascorbate free radicals (del Castillo-Olivares et al. 2000; Rodriguez-Aguilera et al. 2000; Ly and Lawen 2003; May et al. 2003; Crane et al. 2013; Ross and Siegel 2017) (Fig. 2). CoQ is a crucial electron shuttle in the plasma membrane (Arroyo et al. 2000). The PM redox enzymes protect the plasma membrane from lipid peroxidation by maintaining levels of reduced forms of CoQ and α-tocopherol (Crane et al. 2013; Ross and Siegel 2017). Ubiquinol, a reduced form of CoQ, can protect the mitochondrial function of platelets stored for transfusion ((Merlo Pich et al. 2002), regulate ceramide signaling of apoptotic cell death (Navas et al. 2002; Navas and Manuel Villalba 2004), and enhance mitochondrial function, which results in slowed senescence in senescence-accelerated mice (Tian et al. 2014).
Free radicals, oxidative damage, and mitochondrial dysfunction
ATP is essential for cell survival. However, free radicals (e.g. O ·−2 ) are generated primarily in the mitochondrial when ATP is being produced by oxidative phosphorylation. Free radicals leaked from the electron transport chain can attack biomolecules, such as DNA, lipids, and proteins, resulting in production of abnormal proteins and impairment of many biochemical and physiological functions (Ahsan 2013; Gebicki 2016; Valko et al. 2016). In particular, the mitochondria are more sensitive to oxidative stress because mitochondrial DNA is less tightly packed, and their DNA repair systems and levels of antioxidant capacity are lower than those in the cytosol (Liu et al. 2009). Decreased glutathione peroxidase and lower level of glutathione are identified in damaged mitochondria (Monteiro et al. 2004; Dannenmann et al. 2015; Hardeland 2017).
In fact, altered mitochondrial function occurs at early stages of neurodegenerative disease pathogenesis, as has been shown through decreased antioxidant defense and increased oxidative damage (Mawrin et al. 2004; Reddy and Reddy 2011; Wen et al. 2011; Moran et al. 2012). Accumulation of mutations in the mitochondrial DNA (Maruszak et al. 2006; (Keogh and Chinnery 2015) can alter mitochondrial complexes, resulting in reduced mitochondrial complex I activity in AD, PD, and amyotrophic lateral sclerosis (ALS) (Ghiasi et al. 2012; Onyango et al. 2017), dysfunctional complex II and IV activity in ALS (Menzies et al. 2002), and defective complex III activity in aged hearts (Lesnefsky et al. 2001). Alterations in mitochondrial activity can induce ATP depletion, secondarily affecting other biochemical processes.
Compensatory mechanisms in response to mitochondrial dysfunction and oxidative damage
Under energy shortage conditions like mitochondrial dysfunction or intense muscle activity, cells can produce more ATP using alternative systems via lactate fermentation coupled to stimulated glycolysis. Interestingly, cells can survive without functional mitochondria when they are cultured in the presence of pyruvate and uridine. Mitochondria-deficient cells, also called ρ0 cells, can survive using enhanced glycolytic ATP production coupled to electron transport in the plasma membrane (Piechota et al. 2006; Schubert et al. 2015). Lower production of reactive oxygen species (ROS) and higher activity of the plasma membrane redox enzymes are shown in ρ0 cells than in the parental cells (Hyun et al. 2007).
Plasma membrane redox enzymes exist in all types of eukaryotic cells (Villalba and Navas 2000; Crane et al. 2013). Plasma membrane redox enzyme activity is also enhanced in human patients with diminished mitochondrial function, which is a representative parameter in insulin-dependent diabetes mellitus (Lenaz et al. 2002). Plasma membrane redox enzymes can protect neuronal cells from oxidative stress-induced apoptosis through maintenance of redox homeostasis when supplemented with ubiquinol (a reduced form of CoQ) in aged and AD brains (Rodriguez-Aguilera et al. 2000; Villalba and Navas 2000). Plasma membrane redox enzymes may be involved in extending the life-span in yeast and mammals by elevating the NAD+/NADH ratio and stimulating mammalian Sir2 (SIRT1) (Merker et al. 2002; Cohen et al. 2004).
Down-regulation of plasma membrane redox enzymes and neurodegeneration
Alterations in plasma membrane redox enzyme activity and other associated components have been identified in aged tissues and neurodegenerative diseases. Levels of lipid peroxidation and protein nitration are elevated in hepatocytes isolated from aged rats (Oberley et al. 2008; Grossini et al. 2015). Plasma membrane fluidity in rats is related to a decrease in the docosahexaenoic acid/arachidonic acid ratio and changes in composition of other phospholipids (Hashimoto et al. 2001; Moghadam et al. 2013). α-Tocopherol contents are reduced in lymphocytes from non-insulin-dependent diabetes mellitus (NIDDM) patients, suggesting that NIDDM progression could be linked to altered electron transfer by plasma membrane redox enzymes (Yanagawa et al. 2001).
These deteriorations are also reported in AD. NQO1 expression in the hippocampal neurons of 3 × transgenic mice harboring presenilin 1 (M146V), a precursor of amyloid protein (Swe), and tau (P301L) transgenes, which lead to amyloid β plaques and neurofibrillary tangles (Oddo et al. 2003), is lower than in age-matched controls (Torres-Lista et al. 2014). SantaCruz et al. had also observed region-specific alterations in NQO1 activity and expression (SantaCruz et al. 2004). In addition, a possible link between NQO1 mutation and AD has been reported. A missense mutation in codon 187 due to a C609T polymorphism in the NQO1 cDNA can reduce level of NQO1 activity in heterozygote populations (Ross et al. 2000; Kiyohara et al. 2005; Kukongviriyapan 2012; Gong et al. 2013; Pey et al. 2016). Higher levels of the C/T and T/T alleles have also been identified in AD patients (Ma et al. 2003), suggesting that low level of the C/C allele may be a risk factor for AD (Bian et al. 2008).
Levels of other plasma membrane components, sphingomyelin and cholesterol, are also altered in the aged and in AD (Cutler et al. 2004). CoQ in the mitochondria from different tissues are decreased by up to 50% in aged patients and people with AD (Mariani et al. 1991; Ernster and Dallner 1995). Total α-tocopherol level in serum is significantly lower in AD patients than in age-matched people (Bourdel-Marchasson et al. 2001; Polidori and Mecocci 2002). Levels of oxidized forms of α-tocopherol are increased in patients with AD and vascular dementia (Tohgi et al. 1994). In addition, impaired plasma membrane redox enzymes and decreased levels of CoQ and α-tocopherol are found in the hippocampus and cortex of 3 × transgenic mice (Hyun et al. 2010).
These studies have demonstrated that impairment of lipids and electron shuttles in the plasma membrane can be biomarkers of aging and neurodegenerative disorders and suggest that their composition can be restored with activated plasma membrane redox enzymes.
Up-regulation of plasma membrane redox enzymes and neuroprotection
The previously described findings suggest that the aging process can be delayed if activity of the plasma membrane redox enzymes is up-regulated. Up-regulated plasma membrane redox enzymes can cause a higher NAD+/NADH ratio (Merker et al. 2002), which is also induced by calorie restriction (Cohen et al. 2004). In fact, calorie restriction is known as the only reliable method for extending life-span in mammalian models (Spindler 2001; Heilbronn and Ravussin 2003; Guarente and Picard 2005). Calorie restriction is involved in mitochondrial biogenesis and regulation of mitochondrial membrane fluidity (Lambert et al. 2004; Lopez-Lluch et al. 2006). Calorie restriction diminishes ROS production in the mitochondria by decreasing free protons and increasing uncoupling protein levels (Agarwal et al. 2005; Bevilacqua et al. 2005; Hagopian et al. 2005). As a result, calorie restriction can reduce oxidative damage and increase antioxidant capacity.
Components in the plasma membrane can also be up-regulated by calorie restriction. Plasma membrane redox enzyme activity was enhanced by calorie restriction, whereas this activity significantly decreased in the livers and brains from ad libitum-fed mice (De Cabo et al. 2004; Hyun et al. 2006b). Plasma membrane lipids are protected from lipid peroxidation by calorie restriction (Hyun et al. 2006b). Overexpressed NQO1 or b5R also made neuronal cells more resistant to oxidative/nitrative stress, but cells with down-regulated redox enzymes were more vulnerable to insults (Hyun et al. 2012; Hyun and Lee 2015). These findings suggest an important role of plasma membrane redox enzymes in maintaining normal brain function.
Plasma membrane redox enzymes, improvement of mitochondrial function, and neuroprotection
Mitochondrial dysfunction causes energy shortage, resulting in alterations in biochemical cascades. As stated earlier, energy shortage problems can be solved, in part, by enhanced glycolysis linked to fermentation and by activated plasma membrane redox enzymes (for example, in ρ0 cells). The possibility of improving mitochondrial function by overexpressing NQO1 or b5R has been reported. Transfected NQO1 or b5R can induce enhanced mitochondrial complex activity with lower ROS production and higher ATP generation, possibly due to more efficient electron transport in mitochondrial complexes (Hyun et al. 2012; Hyun and Lee 2015). Improved mitochondrial function, decreased oxidative damage, and modest life-span extension were also found in transgenic mice overexpressing b5R (Martin-Montalvo et al. 2016). These mice showed reduced levels of liver cancer following treatment with diethylnitrosamine and lower levels of inflammatory parameters.
Similar effects can be induced in cells cultured in the presence of sulforaphane and curcumin, which break disulfide bonds between Nrf2–Keap1, and result in expression of several detoxifying enzymes, including NQO1 and heme oxygenase 1 (HO-1) (Turpaev 2013), (Fig. 2; Table 1). Sulforaphane is an isothiocyanate present in broccoli sprouts and can activate Nrf2, which translocates to the nucleus, binds to an antioxidant response element (ARE), and induces detoxifying enzymes, for instance NQO1 (Yanaka et al. 2005). Retina cells cultured with sulforaphane are more resistant to UV-induced photooxidative damage (Gao and Talalay 2004; Tanito et al. 2005). Curcumin is a phenolic component enriched in curry (Joe et al. 2004), and following dietary supplement containing curcumin, transient ischemic damage was lower in gerbils (Wang et al. 2005). Similarly, a transgenic AD mouse model (APPSw Tg2576) fed curcumin showed reduced amyloid β (Aβ) level, lower oxidative damage, and less inflammation due to protective mechanisms that include HO-1 and p38 MAP kinase (Lim et al. 2001). Moreover, organosulfur compounds found in garlic and onions can protect neurons in several ways. Allium and allicin enhance the level of an uncoupling protein (UCP), leading to protection of hippocampal neurons from Aβ and tunicamycin (Oi et al. 1999). Allicin and other phytochemicals can activate transient receptor potential ion channels in the plasma membrane, resulting in attenuation of stress (Macpherson et al. 2005). Organosulfur products can also induce cellular stress responses through stimulation of the Nrf2-ARE pathway (Chen et al. 2004). Panaxydol, panaxynol, and panaxytriol, which are found in lipid-soluble ginseng extracts, induce NQO1 expression (Lee et al. 2009). Overexpressed NQO1 protected cells from toxic components in lipid-soluble ginseng extracts (Kim et al. 2016). Other neurohormetic phytochemicals can also contribute to protection of cells against a variety of toxic insults via activation of various cell survival mechanisms (Table 1).
Conclusion
By supporting survival mechanisms through increased NAD+/NADH ratios and decreased oxidative stress, plasma membrane redox enzymes can protect neurons during mitochondrial dysfunction due to aging or from a neurodegenerative disorder. Down-regulated plasma membrane redox enzymes are one cause of neurodegenerative disease, which up-regulated plasma membrane redox enzymes can delay. Taken together, these findings indicate that mitochondrial dysfunction should be an early target for aging therapy and could be solved by enhancing plasma membrane enzymes. In addition, plasma membrane redox enzymes may play a central role in maintaining redox homeostasis and energy metabolism through regulation of the SIRT gene in the nucleus and mitochondrial energetics (Fig. 2). Animals overexpressing plasma membrane redox enzymes or phytochemicals that induce plasma membrane redox enzymes may be good model systems for investigating AD pathogenesis. PM redox enzymes may be good therapeutic targets for delaying aging and neurodegenerative disease.
References
Agarwal S, Sharma S, Agrawal V, Roy N (2005) Caloric restriction augments ROS defense in S. cerevisiae, by a Sir2p independent mechanism. Free Radic Res 39:55–62
Ahsan H (2013) 3-Nitrotyrosine: a biomarker of nitrogen free radical species modified proteins in systemic autoimmunogenic conditions. Hum Immunol 74:1392–1399
Anandhan A, Jacome MS, Lei S, Hernandez-Franco P, Pappa A, Panayiotidis MI, Powers R, Franco R (2017) Metabolic dysfunction in parkinson’s disease: bioenergetics, redox homeostasis and central carbon metabolism. Brain Res Bull 133:12–30
Araki T, Sasaki Y, Milbrandt J (2004) Increased nuclear NAD biosynthesis and SIRT1 activation prevent axonal degeneration. Science 305:1010–1013
Arroyo A, Kagan VE, Tyurin VA, Burgess JR, de Cabo R, Navas P, Villalba JM (2000) NADH and NADPH-dependent reduction of coenzyme Q at the plasma membrane. Antioxid Redox Signal 2:251–262
Baker MA, Lane DJ, Ly JD, De Pinto V, Lawen A (2004) VDAC1 is a transplasma membrane NADH-ferricyanide reductase. J Biol Chem 279:4811–4819
Balogun E, Hoque M, Gong P, Killeen E, Green CJ, Foresti R, Alam J, Motterlini R (2003) Curcumin activates the haem oxygenase-1 gene via regulation of Nrf2 and the antioxidant-responsive element. Biochem J 371(Pt 3):887–895
Barja G (2014) The mitochondrial free radical theory of aging. Prog Mol Biol Transl Sci 127:1–27
Bevilacqua L, Ramsey JJ, Hagopian K, Weindruch R, Harper ME (2005) Long-term caloric restriction increases UCP3 content but decreases proton leak and reactive oxygen species production in rat skeletal muscle mitochondria. Am J Physiol Endocrinol Metab 289:E429–E438
Bewley MC, Marohnic CC, Barber MJ (2001) The structure and biochemistry of NADH-dependent cytochrome b5 reductase are now consistent. Biochemistry 40(45):13574–13582
Bian JT, Zhao HL, Zhang ZX, Bi XH, Zhang JW (2008) Association of NAD(P)H:quinone oxidoreductase 1 polymorphism and Alzheimer’s disease in Chinese. J Mol Neurosci 34:235–240
Bourdel-Marchasson I, Delmas-Beauvieux MC, Peuchant E, Richard-Harston S, Decamps A, Reignier B, Emeriau JP, Rainfray M (2001) Antioxidant defences and oxidative stress markers in erythrocytes and plasma from normally nourished elderly Alzheimer patients. Age Ageing 30:235–241
Braidy N, Guillemin G, Grant R (2008) Promotion of cellular NAD(+) anabolism: therapeutic potential for oxidative stress in ageing and Alzheimer’s disease. Neurotox Res 13:173–184
Chan TS, Teng S, Wilson JX, Galati G, Khan S, O’Brien PJ (2002) Coenzyme Q cytoprotective mechanisms for mitochondrial complex I cytopathies involves NAD(P)H: quinone oxidoreductase 1 (NQO1). Free Radic Res 36:421–427
Chen C, Pung D, Leong V, Hebbar V, Shen G, Nair S, Li W, Kong AN (2004) Induction of detoxifying enzymes by garlic organosulfur compounds through transcription factor Nrf2: effect of chemical structure and stress signals. Free Radic Biol Med 37:1578–1590
Chen CY, Jang JH, Li MH, Surh YJ (2005) Resveratrol upregulates heme oxygenase-1 expression via activation of NF-E2-related factor 2 in PC12 cells. Biochem Biophys Res Commun 331:993–1000
Chhetri J, King AE, Gueven N (2018) Alzheimer’s Disease and NQO1: is there a Link? Curr Alzheimer Res 15:56–66
Cohen HY, Miller C, Bitterman KJ, Wall NR, Hekking B, Kessler B, Howitz KT, Gorospe M, de Cabo R, Sinclair DA (2004) Calorie restriction promotes mammalian cell survival by inducing the SIRT1 deacetylase. Science 305:390–392
Crane FL (2001) Biochemical functions of coenzyme Q10. J Am Coll Nutr 20:591–598
Crane FL, Low H, Sun IL (2013) Evidence for a relation between plasma membrane coenzyme Q and autism. Front Biosci (Elite Ed) 5:1011–1016
Cutler RG, Kelly J, Storie K, Pedersen WA, Tammara A, Hatanpaa K, Troncoso JC, Mattson MP (2004) Involvement of oxidative stress-induced abnormalities in ceramide and cholesterol metabolism in brain aging and Alzheimer’s disease. Proc Natl Acad Sci USA 101:2070–2075
Dannenmann B, Lehle S, Hildebrand DG, Kübler A, Grondona P, Schmid V, Holzer K, Fröschl M, Essmann F, Rothfuss O, Schulze-Osthoff K (2015) High glutathione and glutathione peroxidase-2 levels mediate cell-type-specific DNA damage protection in human induced pluripotent stem cells. Stem Cell Rep 4:886–898
Das S, Tosaki A, Bagchi D, Maulik N, Das DK (2006) Potentiation of a survival signal in the ischemic heart by resveratrol through p38 mitogen-activated protein kinase/mitogen- and stress-activated protein kinase 1/cAMP response element-binding protein signaling. J Pharmacol Exp Ther 317:980–988
De Cabo R, Cabello R, Rios M, López-Lluch G, Ingram DK, Lane MA, Navas P (2004) Calorie restriction attenuates age-related alterations in the plasma membrane antioxidant system in rat liver. Exp Gerontol 39:297–304
del Castillo-Olivares A, Nunez de Castro I, Medina MA (2000) Dual role of plasma membrane electron transport systems in defense. Crit Rev Biochem Mol Biol 35:197–220
Ernster L, Dallner G (1995) Biochemical, physiological and medical aspects of ubiquinone function. Biochim Biophys Acta 1271:195–204
Faitg J, Reynaud O, Leduc-Gaudet JP, Gouspillou G (2017) Skeletal muscle aging and mitochondrial dysfunction: an update. Med Sci (Paris) 33:955–962
Fernandez del Rio L, Gutierrez-Casado E, Varela-Lopez A, Villalba JM (2016) Olive oil and the hallmarks of aging. Molecules 21:163
Gan FF, Ling H, Ang X et al (2013) A novel shogaol analog suppresses cancer cell invasion and inflammation, and displays cytoprotective effects through modulation of NF-kappaB and Nrf2-Keap1 signaling pathways. Toxicol Appl Pharmacol 272:852–862
Gao X, Talalay P (2004) Induction of phase 2 genes by sulforaphane protects retinal pigment epithelial cells against photooxidative damage. Proc Natl Acad Sci USA 101:10446–10451
Gebicki JM (2016) Oxidative stress, free radicals and protein peroxides. Arch Biochem Biophys 595:33–39
Germinario RJ, Continelli L, Pratt S (2000) Sugar transport regulation: comparative characterization of the effect of NADH CoQ reductase deficiency in two cell culture systems. Proc Soc Exp Biol Med 225:116–122
Ghiasi P, Hosseinkhani S, Noori A, Nafissi S, Khajeh K (2012) Mitochondrial complex I deficiency and ATP/ADP ratio in lymphocytes of amyotrophic lateral sclerosis patients. Neurol Res 34:297–303
Gong X, Gutala R, Jaiswal AK (2008) Quinone oxidoreductases and vitamin K metabolism. Vitam Horm 78:85–101
Gong M, Yi Q, Wang W (2013) Association between NQO1 C609T polymorphism and bladder cancer susceptibility: a systemic review and meta-analysis. Tumour Biol 34:2551–2556
Gray JP, Eisen T, Cline GW, Smith PJ, Heart E (2011) Plasma membrane electron transport in pancreatic beta-cells is mediated in part by NQO1. Am J Physiol Endocrinol Metab 301:E113–E121
Grimm A, Eckert A (2017) Brain aging and neurodegeneration: from a mitochondrial point of view. J Neurochem 143:418–431
Grossini E, Bellofatto K, Farruggio S, Sigaudo L, Marotta P, Raina G, De Giuli V, Mary D, Pollesello P, Minisini R, Pirisi M, Vacca G (2015) Levosimendan inhibits peroxidation in hepatocytes by modulating apoptosis/autophagy interplay. PLoS ONE 10:e0124742
Guarente L, Picard F (2005) Calorie restriction–the SIR2 connection. Cell 120:473–482
Hagopian K, Harper ME, Ram JJ, Humble SJ, Weindruch R, Ramsey JJ (2005) Long-term calorie restriction reduces proton leak and hydrogen peroxide production in liver mitochondria. Am J Physiol Endocrinol Metab 288:E674–E684
Hardeland R (2017) Melatonin and the electron transport chain. Cell Mol Life Sci 74:3883–3896
Hashimoto M, Shahdat MH, Shimada T, Yamasaki H, Fujii Y, Ishibashi Y, Shido O (2001) Relationship between age-related increases in rat liver lipid peroxidation and bile canalicular plasma membrane fluidity. Exp Gerontol 37:89–97
Hayflick L (2000) The future of ageing. Nature 408(6809):267–269
Heilbronn LK, Ravussin E (2003) Calorie restriction and aging: review of the literature and implications for studies in humans. Am J Clin Nutr 78:361–369
Hyun DH, Lee GH (2015) Cytochrome b5 reductase, a plasma membrane redox enzyme, protects neuronal cells against metabolic and oxidative stress through maintaining redox state and bioenergetics. Age (Dordr) 37:122
Hyun DH, Emerson SS, Jo DG, Mattson MP, de Cabo R (2006a) Calorie restriction up-regulates the plasma membrane redox system in brain cells and suppresses oxidative stress during aging. Proc Natl Acad Sci USA 103:19908–19912
Hyun DH, Hernandez JO, Mattson MP, de Cabo R (2006b) The plasma membrane redox system in aging. Ageing Res Rev 5:209–220
Hyun DH, Hunt ND, Emerson SS, Hernandez JO, Mattson MP, de Cabo R (2007) Up-regulation of plasma membrane-associated redox activities in neuronal cells lacking functional mitochondria. J Neurochem 100:1364–1374
Hyun DH, Mughal MR, Yang H, Lee JH, Ko EJ, Hunt ND, de Cabo R, Mattson MP (2010) The plasma membrane redox system is impaired by amyloid beta-peptide and in the hippocampus and cerebral cortex of 3xTgAD mice. Exp Neurol 225:423–429
Hyun DH, Kim J, Moon C, Lim CJ, de Cabo R, Mattson MP (2012) The plasma membrane redox enzyme NQO1 sustains cellular energetics and protects human neuroblastoma cells against metabolic and proteotoxic stress. Age (Dordr) 34:359–370
Jaber S, Polster BM (2015) Idebenone and neuroprotection: antioxidant, pro-oxidant, or electron carrier? J Bioenerg Biomembr 47(1–2):111–118. https://doi.org/10.1007/s10863-014-9571-y
Jaiswal AK (2000) Regulation of genes encoding NAD(P)H:quinone oxidoreductases. Free Radic Biol Med 29:254–262
Joe B, Vijaykumar M, Lokesh BR (2004) Biological properties of curcumin-cellular and molecular mechanisms of action. Crit Rev Food Sci Nutr 44:97–111
Johannesson T, Kristinsson J, Torsdottir G, Snaedal J (2012) Ceruloplasmin (Cp) and iron in connection with Parkinson’s disease (PD) and Alzheimer’s disease (AD). Laeknabladid 98:531–537
Keogh MJ, Chinnery PF (2015) Mitochondrial DNA mutations in neurodegeneration. Biochim Biophys Acta 1847:1401–1411
Kim MS, Kwon DY, Cho HJ, Lee MS (2006) Protective effects of Korean herbal remedy against oxidative stress in cardiomyocytes. Phytother Res 20:235–236
Kim HK, Son TG, Jo DG, Kim DC, Hyun DH (2016) Cytotoxicity of lipid-soluble ginseng extracts is attenuated by plasma membrane redox enzyme NQO1 through maintaining redox homeostasis and delaying apoptosis in human neuroblastoma cells. Arch Pharm Res 39:1339–1348
Kiyohara C, Yoshimasu K, Takayama K, Nakanishi Y (2005) NQO1, MPO, and the risk of lung cancer: a HuGE review. Genet Med 7:463–478
Kobayashi Y, Furukawa-Hibi Y, Chen C et al (2005) SIRT1 is critical regulator of FOXO-mediated transcription in response to oxidative stress. Int J Mol Med 16:237–243
Koltover VK (2017) Free radical timer of aging: from chemistry of free radicals to systems theory of reliability. Curr Aging Sci 10:12–17
Kong Y, Trabucco SE, Zhang H (2014) Oxidative stress, mitochondrial dysfunction and the mitochondria theory of aging. Interdiscip Top Gerontol 39:86–107
Kraft AD, Johnson DA, Johnson JA (2004) Nuclear factor E2-related factor 2-dependent antioxidant response element activation by tert-butylhydroquinone and sulforaphane occurring preferentially in astrocytes conditions neurons against oxidative insult. J Neurosci 24:1101–1112
Kukongviriyapan V (2012) Genetic polymorphism of drug metabolizing enzymes in association with risk of bile duct cancer. Asian Pac J Cancer Prev 13(Suppl):7–15
Lambert AJ, Wang B, Merry BJ (2004) Exogenous insulin can reverse the effects of caloric restriction on mitochondria. Biochem Biophys Res Commun 316:1196–1201
Le Bourg E (2014) Evolutionary theories of aging can explain why we age. Interdiscip Top Gerontol 39:8–23
Lee LS, Stephenson KK, Fahey JW et al (2009) Induction of chemoprotective phase 2 enzymes by ginseng and its components. Planta Med 75:1129–1133
Lenaz G, Paolucci U, Fato R, D’Aurelio M, Parenti Castelli G, Sgarbi G, Biagini G, Ragni L, Salardi S, Cacciari E (2002) Enhanced activity of the plasma membrane oxidoreductase in circulating lymphocytes from insulin-dependent diabetes mellitus patients. Biochem Biophys Res Commun 290:1589–1592
Lesnefsky EJ, Gudz TI, Moghaddas S, Migita CT, Ikeda-Saito M, Turkaly PJ, Hoppel CL (2001) Aging decreases electron transport complex III activity in heart interfibrillar mitochondria by alteration of the cytochrome c binding site. J Mol Cell Cardiol 33:37–47
Lim GP, Chu T, Yang F, Beech W, Frautschy SA, Cole GM (2001) The curry spice curcumin reduces oxidative damage and amyloid pathology in an Alzheimer transgenic mouse. J Neurosci 21:8370–8377
Liochev SI (2013) Reactive oxygen species and the free radical theory of aging. Free Radic Biol Med 60:1–4
Liu CY, Lee CF, Wei YH (2009) Role of reactive oxygen species-elicited apoptosis in the pathophysiology of mitochondrial and neurodegenerative diseases associated with mitochondrial DNA mutations. J Formos Med Assoc 108:599–611
Lopez-Lluch G, Hunt N, Jones B, Zhu M, Jamieson H, Hilmer S, Cascajo MV, Allard J, Ingram DK, Navas P, de Cabo R (2006) Calorie restriction induces mitochondrial biogenesis and bioenergetic efficiency. Proc Natl Acad Sci USA 103:1768–1773
Ly JD, Lawen A (2003) Transplasma membrane electron transport: enzymes involved and biological function. Redox Rep 8:3–21
Ma QL, Yang JF, Shao M, Dong XM, Chen B (2003) Association between NAD(P)H: quinone oxidoreductase and apolipoprotein E gene polymorphisms in Alzheimer’s disease. Zhonghua Yi Xue Za Zhi 83:2124–2127
Macpherson LJ, Geierstanger BH, Viswanath V, Bandell M, Eid SR, Hwang S, Patapoutian A (2005) The pungency of garlic: activation of TRPA1 and TRPV1 in response to allicin. Curr Biol 15:929–934
Mandel SA, Avramovich-Tirosh Y, Reznichenko L, Zheng H, Weinreb O, Amit T, Youdim MB (2005) Multifunctional activities of green tea catechins in neuroprotection. Modulation of cell survival genes, iron-dependent oxidative stress and PKC signaling pathway. Neurosignals 14:46–60
Mariani C, Bresolin N, Farina E, Moggio M, Ferrante C, Ciafaloni E, Sertorelli S, Ciccone A, Scarlato G (1991) Muscle biopsy in Alzheimer’s disease: morphological and biochemical findings. Clin Neuropathol 10:171–176
Marques-da-Silva D, Samhan-Arias AK, Tiago T, Gutierrez-Merino C (2010) L-type calcium channels and cytochrome b5 reductase are components of protein complexes tightly associated with lipid rafts microdomains of the neuronal plasma membrane. J Proteomics 73:1502–1510
Martin-Montalvo A, Sun Y, Diaz-Ruiz A, Ali A, Gutierrez V, Palacios HH, Curtis J, Siendones E, Ariza J, Abulwerdi GA, Sun X, Wang AX, Pearson KJ, Fishbein KW, Spencer RG, Wang M, Han X, Scheibye-Knudsen M, Baur JA, Shertzer HG, Navas P, Villalba JM, Zou S, Bernier M, de Cabo R (2016) Cytochrome b5 reductase and the control of lipid metabolism and healthspan. NPJ Aging Mech Dis 2:16006
Maruszak A, Gaweda-Walerych K, Soltyszewski I, Zekanowski C (2006) Mitochondrial DNA in pathogenesis of Alzheimer’s and Parkinson’s diseases. Acta Neurobiol Exp (Wars) 66:153–176
Matsuda H, Kimura S, Iyanagi T (2000) One-electron reduction of quinones by the neuronal nitric-oxide synthase reductase domain. Biochim Biophys Acta 1459:106–116
Mawrin C, Kirches E, Krause G, Schneider-Stock R, Bogerts B, Vorwerk CK, Dietzmann K (2004) Region-specific analysis of mitochondrial DNA deletions in neurodegenerative disorders in humans. Neurosci Lett 357:111–114
May JM, Qu ZC, Li X (2003) Ascorbic acid blunts oxidant stress due to menadione in endothelial cells. Arch Biochem Biophys 411:136–144
Menzies FM, Cookson MR, Taylor RW, Turnbull DM, Chrzanowska-Lightowlers ZM, Dong L, Figlewicz DA, Shaw PJ (2002) Mitochondrial dysfunction in a cell culture model of familial amyotrophic lateral sclerosis. Brain 125(Pt 7):1522–1533
Merker MP, Bongard RD, Kettenhofen NJ, Okamoto Y, Dawson CA (2002) Intracellular redox status affects transplasma membrane electron transport in pulmonary arterial endothelial cells. Am J Physiol Lung Cell Mol Physiol 282:L36–L43
Merlo Pich M, Castagnoli A, Biondi A, Bernacchia A, Tazzari PL, D’Aurelio M, Parenti Castelli G, Formiggini G, Conte R, Bovina C, Lenaz G (2002) Ubiquinol and a coenzyme Q reducing system protect platelet mitochondrial function of transfusional buffy coats from oxidative stress. Free Radic Res 36:429–436
Miller MG, Shukitt-Hale B (2012) Berry fruit enhances beneficial signaling in the brain. J Agric Food Chem 60:5709–5715
Moghadam NN, Holmstrup M, Pertoldi C, Loeschcke V (2013) Age-induced perturbation in cell membrane phospholipid fatty acid profile of longevity-selected Drosophila melanogaster and corresponding control lines. Exp Gerontol 48:1362–1368
Monteiro G, Kowaltowski AJ, Barros MH, Netto LE (2004) Glutathione and thioredoxin peroxidases mediate susceptibility of yeast mitochondria to Ca(2+)-induced damage. Arch Biochem Biophys 425:14–24
Moran M, Moreno-Lastres D, Marin-Buera L, Arenas J, Martin MA, Ugalde C (2012) Mitochondrial respiratory chain dysfunction: implications in neurodegeneration. Free Radic Biol Med 53:595–609
Navas P, Manuel Villalba J (2004) Regulation of ceramide signaling by plasma membrane coenzyme Q reductases. Methods Enzymol 378:200–206
Navas P, Fernandez-Ayala DM, Martin SF, Lopez-Lluch G, De Caboa R, Rodriguez-Aguilera JC, Villalba JM (2002) Ceramide-dependent caspase 3 activation is prevented by coenzyme Q from plasma membrane in serum-deprived cells. Free Radic Res 36:369–374
Nioi P, Hayes JD (2004) Contribution of NAD(P)H:quinone oxidoreductase 1 to protection against carcinogenesis, and regulation of its gene by the Nrf2 basic-region leucine zipper and the arylhydrocarbon receptor basic helix-loop-helix transcription factors. Mutat Res 555:149–171
Oberley TD, Swanlund JM, Zhang HJ, Kregel KC (2008) Aging results in increased autophagy of mitochondria and protein nitration in rat hepatocytes following heat stress. J Histochem Cytochem 56:615–627
Oddo S, Caccamo A, Shepherd JD, Murphy MP, Golde TE, Kayed R, Metherate R, Mattson MP, Akbari Y, LaFerla FM (2003) Triple-transgenic model of Alzheimer’s disease with plaques and tangles: intracellular Abeta and synaptic dysfunction. Neuron 39:409–421
Oi Y, Kawada T, Shishido C, Wada K, Kominato Y, Nishimura S, Ariga T, Iwai K (1999) Allyl-containing sulfides in garlic increase uncoupling protein content in brown adipose tissue, and noradrenaline and adrenaline secretion in rats. J Nutr 129:336–342
Onyango IG, Khan SM, Bennett JP Jr (2017) Mitochondria in the pathophysiology of Alzheimer’s and Parkinson’s diseases. Front Biosci (Landmark Ed) 22:854–872
Pey AL, Megarity CF, Medina-Carmona E, Timson DJ (2016) Natural small molecules as stabilizers and activators of cancer-associated NQO1 polymorphisms. Curr Drug Targets 17:1506–1514
Piechota J, Szczesny R, Wolanin K, Chlebowski A, Bartnik E (2006) Nuclear and mitochondrial genome responses in HeLa cells treated with inhibitors of mitochondrial DNA expression. Acta Biochim Pol 53:485–495
Polidori MC, Mecocci P (2002) Plasma susceptibility to free radical-induced antioxidant consumption and lipid peroxidation is increased in very old subjects with Alzheimer disease. J Alzheimers Dis 4:517–522
Reddy PH, Reddy TP (2011) Mitochondria as a therapeutic target for aging and neurodegenerative diseases. Curr Alzheimer Res 8:393–409
Reddy VD, Padmavathi P, Bulle S, Maturu P, Puvvada PK, Nallanchakravarthula V (2017) Association between alcohol-induced oxidative stress and membrane properties in synaptosomes: a protective role of vitamin E. Neurotoxicol Teratol 63:60–65
Rodriguez-Aguilera JC, Lopez-Lluch G, Santos-Ocana C, Villalba JM, Gomez-Diaz C, Navas P (2000) Plasma membrane redox system protects cells against oxidative stress. Redox Rep 5(2–3):148–150
Ross D, Siegel D (2017) Functions of NQO1 in cellular protection and CoQ10 metabolism and its potential role as a redox sensitive molecular switch. Front Physiol 8:595
Ross D, Kepa JK, Winski SL, Beall HD, Anwar A, Siegel D (2000) NAD(P)H:quinone oxidoreductase 1 (NQO1): chemoprotection, bioactivation, gene regulation and genetic polymorphisms. Chem Biol Interact 129:77–97
Samhan-Arias AK, Fortalezas S, Cordas CM, Moura I, Moura JJG, Gutierrez-Merino C (2018) Cytochrome b5 reductase is the component from neuronal synaptic plasma membrane vesicles that generates superoxide anion upon stimulation by cytochrome c. Redox Biol 15:109–114
SantaCruz KS, Yazlovitskaya E, Collins J, Johnson J, DeCarli C (2004) Regional NAD(P)H:quinone oxidoreductase activity in Alzheimer’s disease. Neurobiol Aging 25:63–69
Schubert S, Heller S, Loffler B, Schäfer I, Seibel M, Villani G, Seibel P (2015) Generation of rho zero cells: visualization and quantification of the mtDNA depletion process. Int J Mol Sci 16:9850–9865
Song K, Kim YS, Moon SK, Ko CN, Cho KH, Bae HS, Lee KS (2001) Effects of uwhangchungsimwon on cell viability, proliferation, and gene expression of human neuronal cell line IMR32. Am J Chin Med 29:445–458
Spindler SR (2001) Calorie restriction enhances the expression of key metabolic enzymes associated with protein renewal during aging. Ann N Y Acad Sci 928:296–304
Tanito M, Masutani H, Kim YC, Nishikawa M, Ohira A, Yodoi J (2005) Sulforaphane induces thioredoxin through the antioxidant-responsive element and attenuates retinal light damage in mice. Invest Ophthalmol Vis Sci 46:979–987
Tian G, Sawashita J, Kubo H, Nishio SY, Hashimoto S, Suzuki N, Yoshimura H, Tsuruoka M, Wang Y, Liu Y, Luo H, Xu Z, Mori M, Kitano M, Hosoe K, Takeda T, Usami S, Higuchi K (2014) Ubiquinol-10 supplementation activates mitochondria functions to decelerate senescence in senescence-accelerated mice. Antioxid Redox Signal 20:2606–2620
Tohgi H, Abe T, Nakanishi M, Hamato F, Sasaki K, Takahashi S (1994) Concentrations of alpha-tocopherol and its quinone derivative in cerebrospinal fluid from patients with vascular dementia of the Binswanger type and Alzheimer type dementia. Neurosci Lett 174:73–76
Torres-Lista V, Parrado-Fernandez C, Alvarez-Monton I, Frontiñán-Rubio J, Durán-Prado M, Peinado JR, Johansson B, Alcaín FJ, Giménez-Llort L (2014) Neophobia, NQO1 and SIRT1 as premorbid and prodromal indicators of AD in 3xTg-AD mice. Behav Brain Res 271:140–146
Tumpel S, Rudolph KL (2012) The role of telomere shortening in somatic stem cells and tissue aging: lessons from telomerase model systems. Ann N Y Acad Sci 1266:28–39
Turpaev KT (2013) Keap1-Nrf2 signaling pathway: mechanisms of regulation and role in protection of cells against toxicity caused by xenobiotics and electrophiles. Biochemistry (Mosc) 78:111–126
Turunen M, Olsson J, Dallner G (2004) Metabolism and function of coenzyme Q. Biochim Biophys Acta 1660:171–199
Valko M, Jomova K, Rhodes CJ, Kuca K, Musilek K (2016) Redox- and non-redox-metal-induced formation of free radicals and their role in human disease. Arch Toxicol 90:1–37
Vantieghem A, Xu Y, Assefa Z, Piette J, Vandenheede JR, Merlevede W, De Witte PA, Agostinis P (2002) Phosphorylation of Bcl-2 in G2/M phase-arrested cells following photodynamic therapy with hypericin involves a CDK1-mediated signal and delays the onset of apoptosis. J Biol Chem 277:37718–37731
Villalba JM, Navas P (2000) Plasma membrane redox system in the control of stress-induced apoptosis. Antioxid Redox Signal 2:213–230
Wang Q, Sun AY, Simonyi A, Jensen MD, Shelat PB, Rottinghaus GE, MacDonald RS, Miller DK, Lubahn DE, Weisman GA, Sun GY (2005) Neuroprotective mechanisms of curcumin against cerebral ischemia-induced neuronal apoptosis and behavioral deficits. J Neurosci Res 82:138–148
Wang X, Ma Z, Cheng J, Lv Z (2014) A genetic program theory of aging using an RNA population model. Ageing Res Rev 13:46–54
Wen Y, Li W, Poteet EC, Xie L, Tan C, Yan LJ, Ju X, Liu R, Qian H, Marvin MA, Goldberg MS, She H, Mao Z, Simpkins JW, Yang SH (2011) Alternative mitochondrial electron transfer as a novel strategy for neuroprotection. J Biol Chem 286:16504–16515
Westerheide SD, Bosman JD, Mbadugha BN, Kawahara TL, Matsumoto G, Kim S, Gu W, Devlin JP, Silverman RB, Morimoto RI (2004) Celastrols as inducers of the heat shock response and cytoprotection. J Biol Chem 279:56053–56060
Yanagawa K, Takeda H, Egashira T, Matsumiya T, Shibuya T, Takasaki M (2001) Changes in antioxidative mechanisms in elderly patients with non-insulin-dependent diabetes mellitus. Investigation of the redox dynamics of alpha-tocopherol in erythrocyte membranes. Gerontology 47:150–157
Yanaka A, Zhang S, Tauchi M, Suzuki H, Shibahara T, Matsui H, Nakahara A, Tanaka N, Yamamoto M (2005) Role of the nrf-2 gene in protection and repair of gastric mucosa against oxidative stress. Inflammopharmacology 13:83–90
Zhu Y, Liu X, Ding X, Wang F, Geng X (2018) Telomere and its role in the aging pathways: telomere shortening, cell senescence and mitochondria dysfunction. Biogerontology 20:1–16
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) funded by the Korean Government (GRANT No. NRF-2016R1D1A1B03932759).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author has no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hyun, DH. Plasma membrane redox enzymes: new therapeutic targets for neurodegenerative diseases. Arch. Pharm. Res. 42, 436–445 (2019). https://doi.org/10.1007/s12272-019-01147-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12272-019-01147-8