Abstract
It remains uncertain whether plasma D-dimer level can predict no-reflow in patients with STEMI who had pPCI after 48 h of symptom onset. This study retrospectively enrolled 229 consecutive patients who had pPCI for acute STEMI within 2–7 days of symptom onset between January 2008 and December 2018. Patients were divided into no-reflow group (TIMI flow grade 0–2) and reflow group (TIMI flow grade 3). Predictors of no-reflow were assessed by univariate and multivariate binary logistic regression analyses. Plasma D-dimer level can independently predict no-reflow in patients with STEMI who had pPCI within 2–7 days of symptom onset (OR 2.52 per 1 mg/L increase, 95% CI 1.16–5.47, p = 0.019). This finding indicated that pPCI may be safe and feasible for STEMI patients within 2–7 days of symptom onset with low D-dimer level.

Plasma D-dimer level can independently predict no-reflow in patients with STEMI who had pPCI within 2–7 days of symptom onset. pPCI may be safe and feasible for STEMI patients within 2–7 days of symptom onset with low D-dimer level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary percutaneous coronary intervention (pPCI) is the most effective reperfusion strategy for patients with acute ST-segment elevation myocardial infarction (STEMI) [1], especially when performed within 12 h of symptom onset and, according to the 2017 European Society of Cardiology (ESC) guidelines, up to 48 h [2]. However, approximately one-third of eligible patients do not receive early reperfusion therapy because of late presentation [3], for which optimal strategy remains uncertain [4]. Serious complications especially no-reflow phenomenon occur more likely when PCI was performed at 2–7 days, leading to higher early and late morbidity and mortality [5, 6]. The high incidence of immediate no-reflow after stenting has discouraged PCI during said period [7].
No-reflow is commonly secondary to heavy intra-coronary thrombus burden [8, 9] and impaired microvascular function [10]. An increase in the level of D-dimer, the simplest degradation product of fibrin, reflects ongoing or recent thrombosis [11]. D-dimer level can independently predict no-reflow and major cardiovascular adverse events (MACE) after PCI in early STEMI [12,13,14]; however, it remains to be determined if this also applies to the 2–7-day interval. We hypothesized that, as an indirect estimate of thrombus burden, plasma D-dimer level can also predict no-reflow phenomenon when PCI was performed at 2–7 days of symptom onset.
Methods
Study Population and Design
We retrospectively screened 240 consecutive patients who had pPCI for acute STEMI from 48 h to 7 days after the onset of symptoms between January 2008 and December 2018. Of them, 229 patients whose D-dimer levels were measured on admission were included in this study. The diagnosis of acute STEMI was based on the specific electrocardiography (ECG) criteria laid down in the European Society of Cardiology, American College of Cardiology Foundation, American Heart Association, and World Heart Federation (ESC/ACCF/AHA/WHF) committee [15]. Coronary blood flow was analyzed according to thrombolysis in myocardial infarction (TIMI) flow grade [16]. Angiographic no-reflow was defined as postinterventional TIMI flow grade < 3 without clear evidence of dissection, stenosis, or vasospasm [17]. Patients were divided into no-reflow group (TIMI flow grade 0–2) and reflow group (TIMI flow grade 3). Patients with culprit lesion in the left main coronary artery; left main coronary artery stenosis > 50%; previous coronary artery bypass surgery; major surgeries or severe injuries in the past 6 months; cardiogenic shock; pain to balloon time < 48 h; thrombolysis failure and rescue PCI; active infectious or inflammatory diseases; presence of any chronic inflammatory-autoimmune disease including rheumatologic disorders, hematologic diseases, class IV heart failure, severe respiratory, renal, or hepatic dysfunction or failure; and history of thromboembolic disease, treated cancer, inflammatory process, or pregnancy were excluded from the current study. The study protocol was reviewed and approved by the Ethics Committee of Zhongshan Hospital, Fudan University.
Coronary Angiography and Percutaneous Coronary Intervention
All patients received a 300 mg chewable aspirin and a 300-mg loading dose of clopidogrel or a 180-mg loading dose of ticagrelor on admission, and 100 U/kg intravenous standard heparin during the procedure. Coronary angiography and pPCI were performed by experienced interventional cardiologists. At least one drug-eluting stent was implanted in the culprit lesion of infarct-related artery (IRA). The technical aspects of the procedure, duration and pressure of inflation, and thrombus aspiration or not were at the discretion of individual operators. After the intervention, all patients were prescribed clopidogrel (75 mg once daily for 12 months) or ticagrelor (90 mg twice daily for 12 months) and aspirin (100 mg indefinitely).
Visual assessments for lesion characteristics, thrombus burden, and pre- and post-interventional TIMI flow grade were performed by two interventional cardiologists blinded to patients’ clinical data. TIMI thrombus score was used to evaluate thrombus burden in all patients, and TIMI thrombus score ≥ 4 was defined as high-grade angiographic thrombus burden [18]. TIMI flow grade 3 was defined as complete coronary flow within three cardiac cycles, whereas TIMI flow grade < 3 denoted incomplete perfusion or complete perfusion over three cardiac cycles.
Data Collection
All clinical and sociodemographic characteristics of the patients were extracted from hospital files and computer records. Peripheral venous blood samples for the determination of baseline biochemical parameters including D-dimer, N-terminal pro-B-type natriuretic peptide (NT-pro BNP), cardiac troponin T (cTnT), high-sensitivity C-reactive protein (hs-CRP), creatine kinase, complete blood count, and renal function were obtained on admission in the emergency department and all measurements were performed 15 min after blood collection. Estimated glomerular filtration rate (eGFR) on admission was calculated according to modification of diet in renal disease formula. Blood sampling for D-dimer measurement was made using a commercial D-dimer assay (MDA immunoturbidimetric assay; Sysmex, CA7000). Postprocedural transthoracic echocardiography was performed on all patients during the in-hospital period as recommended [19]. MACEs were defined as in-stent thrombosis, nonfatal myocardial infarction (MI), and in-hospital mortality during the in-hospital follow-up period. In-stent thrombosis was defined as angiographically documented total occlusion. Non-fatal MI was defined as recurrent chest pain and/or development of new ECG changes accompanied by a new increase ≥ 20% in levels of cardiac biomarkers measured after the recurrent event. In-hospital mortality had to be verified as death from MI, cardiac arrest, or other cardiac causes.
Statistical Analysis
Continuous data were expressed as mean (standard deviation) and compared using independent samples t test, while categorical variables were expressed as number (percentage) and were compared using the chi-square tests. A p value of < 0.05 was regarded as statistically significant. Independent predictors of angiographic no-reflow were determined by binary logistic regression analysis with stepwise selection. Odds ratios (ORs), 95% confidence intervals (CIs), and p values were calculated using the IBM SPSS Statistics 19.0 software package (SPSS, Inc., Chicago, IL). To assess the predictive value of D-dimer, receiver operating characteristics (ROC) analysis was conducted with calculations of the area under the ROC curve (AUC), sensitivity, and specificity.
Results
The study population consisted of 229 patients (mean age 63.7 (12.1); 83.0% male) who underwent pPCI for acute STEMI 2–7 days after symptom onset. Postinterventional TIMI flow grade 3 was achieved in most patients (n = 201, 87.8%) and the incidence of angiographic no-reflow was 12.2% (n = 28).
Baseline Characteristics
As summarized in Table 1, baseline and clinical characteristics were balanced between study groups except for higher proportions of smokers, Killip class ≥ 2, TIMI flow grades, and total ischemic time in no-reflow group compared with reflow group.
Laboratory Test Results
As shown in Table 2, angiographic no-reflow group had higher levels of D-dimer (Fig. 1a), log (NT-pro BNP), hs-CRP, white blood cell, and neutrophil counts compared with reflow group.
Box diagram for comparison of D-dimer level in different groups. a Mean D-dimer level was significantly higher in no-reflow group than that in reflow group (*p value < 0.05). b Mean D-dimer level was significantly higher in patients with TIMI thrombus score ≥ 3 compared with those with TIMI thrombus score < 3 (*p value < 0.01)
Angiographic and Echocardiographic Findings
The proportion of patients with TIMI thrombus score ≥ 3 and thrombus aspiration in no-reflow group was significantly higher than that in reflow group. Multivessel disease proportion and postprocedural LVEF were similar between the two groups; however, the proportion of pericardial effusion in the no-reflow group was higher than that in the reflow group (p < 0.05; Table 3).
Independent Predictive Value of D-Dimer for Angiographic No-Reflow
D-dimer level was higher in patients with TIMI thrombus score ≥ 3 compared with those with TIMI thrombus score < 3 (1.9 (1.6) vs. 0.6 (0.6), p < 0.01) (Fig.1b). As shown in Table 4, besides TIMI thrombus score, plasma D-dimer level can independently predict the no-reflow phenomenon after PCI (OR 2.52 per 1 mg/L increase, 95% CI 1.16–5.47, p = 0.019).
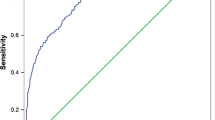
Prognostic Value of D-Dimer Level on No-Reflow Phenomenon
In ROC analysis (Fig. 2), a D-dimer value of 0.53 (mg/L) was identified as an effective cut-off point in prediction of postprocedural no-reflow phenomenon, with 85.7% of sensitivity and 67.7% of specificity (AUC = 0.78; 95% CI, 0.69–0.88, p = 0.049).
In-Hospital Outcomes
There is no significance between the two groups in the in-stent thrombosis or non-fatal MI. The no-reflow group had a higher in-hospital mortality rate than the reflow group (p = 0.014; Table 5).
Discussion
This study, to our knowledge, is the first to demonstrate that plasma D-dimer level on admission can independently predict no-reflow in patients who had pPCI for acute STEMI 2–7 days after symptom onset.
PPCI is not recommended by the guidelines in patients with STEMI if the onset of symptoms came on over 48 h, because it provides little benefit after longstanding myocardial necrosis and is associated with complications, such as myocardial hemorrhage, microembolism, and no-reflow. However, Horie et al. [20] showed that even with late reperfusion, percutaneous transluminal coronary angioplasty (PTCA) had beneficial effects on cardiac events’ occurrence over a 5-year period after MI. Both DECOPI [21] and OAT [22] trials demonstrated no difference in clinical outcomes between patients randomized to PCI versus optimal medical therapy alone with an occluded IRA over 48 h post-MI (25% of PCI was performed within 5 days). The results are consistent with the safety documented in the present study and may be related to thrombus aspiration and extensive use of glycoprotein IIb/IIIa antagonists. However, the incidence of no-reflow in DECOPI, OAT, and the present study is 17.8%, 18%, and 12.23%, respectively, which is higher than that for PCI within 12 h of symptom onset. No-reflow remained a powerful independent predictor of death or myocardial infarction, patients with no-reflow presented more frequently with congestive heart failure and pericardial effusion than patients with normal flow [23], most of which was confirmed in our study. Therefore, it is necessary to assess risk for no-reflow before pPCI for this subpopulation to further improve the safety of intervention.
There are ample evidences for using D-dimer to assess thrombus burden. The coagulation system plays a major role in the development of thrombosis in the setting of AMI [24]. Over 60% of thrombus is fibrin fibers, with the proportion increasing with ischemic time [25], while platelets, erythrocytes, cholesterol crystals, and leukocytes together comprise the remaining 40% [25]. D-dimer is a final product of the specific degradation of fibrin monomer crosslinked by activating factor XIII and hydrolyzed by plasmin. The plasma level of D-dimer increases in subjects with ongoing or recent thrombosis [11], reflecting activation of the fibrinolysis and coagulation systems [26], and serves as an indirect estimation of the size of the thrombotic mass available for fibrinolysis and the severity of the hypercoagulable state [27]. It has been suggested that high D-dimer levels reflect a systemic prothrombotic state and focal vessel wall-related fibrin formation with unstable atherosclerotic plaque activity [6]. Plasma D-dimer levels have been correlated with thrombus burden in cases of acute pulmonary embolism and lower extremity venous thrombosis [28,29,30,31] and acute myocardial infarction [14, 32]. D-dimer levels are significantly higher in patients treated within 12 h of symptom onset and with TIMI thrombus score > 4 vs. ≤ 4 [12].
Thrombus age has impact on D-dimer level [14]. Thrombosis activity and thrombus burden are important contributors to magnitude of D-dimer level increase, with D-dimer level positively correlating with “fresh” thrombus burden. In theory, old thrombosis no longer leads to D-dimer production, and continuously, negative D-dimer would suggest resolution or chronic organization of acute thrombosis [33,34,35,36]. However, in our study, D-dimer level correlated with thrombus burden in STEMI patients with 2–7 days of symptom onset. Patients with TIMI thrombus score ≥ 3 vs. < 3 had significantly higher D-dimer levels, indicating that heavy thrombus burden beyond the initial 2 days window for PCI also increases the risk of distal embolization and no-reflow. Studies in the setting of pulmonary embolism also documented that plasma D-dimer levels reflect thrombus burden over a long period [30, 31, 37]. The finding that D-dimer level predicts no-reflow is consistent with thrombus burden being an important underlying factor of no-reflow [8, 9, 26, 38], which might allow risk assessment of pPCI procedure for the patients who had pPCI within 2–7 days of symptom onset, a thus far controversial PCI time window [39, 40] and not recommended in guidelines. This finding implies that pPCI may be safe and feasible for STEMI patients within 2–7 days with low D-dimer level, while PCI should be delayed for those with high D-dimer level. Large-scale multicenter studies are warranted to further assess the safety and long-term efficacy of pPCI performed within 2–7 days of symptom onset for STEMI and to explore other cardiac biomarkers that could be used to identify patients who would benefit most from pPCI.
Limitations
The study has the limitations inherent to its single center, retrospective design with a relatively small sample size which might introduce selection bias. The pathophysiological process of AMI is very complex, including endothelial integrity destruction, plaque rupture, thrombosis, mechanical effects, reperfusion, stress, and changes in blood composition, among other variables. Therefore, it might be simplistic to expect a single biochemical parameter related to thrombus burden to allow risk stratification of pPCI for STEMI. We only presented in-hospital events in our study; lack of follow-up data may be another limitation for our study.
Conclusion
Plasma D-dimer level on admission can independently predict no-reflow in patients with STEMI who had pPCI within 2–7 days of symptom onset; pPCI may be safe and feasible for these patients with low D-dimer level.
Abbreviations
- cTnT:
-
Cardiac troponin T
- ECG:
-
Electrocardiogram
- eGFR:
-
Estimated glomerular filtration rate
- hs-CRP:
-
High-sensitivity C-reactive protein
- IRA:
-
Infarct-related artery
- MACE:
-
Major cardiovascular adverse events
- MI:
-
Myocardial infarction
- NT-pro BNP:
-
N-terminal pro-B-type natriuretic peptide
- pPCI:
-
Primary percutaneous coronary intervention
- PTCA:
-
Percutaneous transluminal coronary angioplasty
- STEMI:
-
ST-segment elevation myocardial infarction
- TIMI:
-
Thrombolysis in myocardial infarction
References
Ibanez, B., James, S., Agewall, S., et al. (2018). 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (esc). European Heart Journal, 39, 119–177.
Authors/Task Force m, Windecker, S., Kolh, P., et al. (2014). 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). European Heart Journal, 35, 2541–2619.
Eagle, K. A., Goodman, S. G., Avezum, A., et al. (2002). Practice variation and missed opportunities for reperfusion in ST-segment-elevation myocardial infarction: findings from the Global Registry of Acute Coronary Events (GRACE). Lancet, 359, 373–377.
Hochman, J. S., Lamas, G. A., Buller, C. E., et al. (2006). Coronary intervention for persistent occlusion after myocardial infarction. The New England Journal of Medicine, 355, 2395–2407.
Celik, T., Balta, S., Demir, M., et al. (2016). Predictive value of admission red cell distribution width-platelet ratio for no-reflow phenomenon in acute ST segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Cardiology Journal, 23, 84–92.
Ndrepepa, G., Tiroch, K., Fusaro, M., et al. (2010). 5-year prognostic value of no-reflow phenomenon after percutaneous coronary intervention in patients with acute myocardial infarction. Journal of the American College of Cardiology, 55, 2383–2389.
Rezkalla, S. H., & Kloner, R. A. (2008). Coronary no-reflow phenomenon: from the experimental laboratory to the cardiac catheterization laboratory. Catheterization and Cardiovascular Interventions, 72, 950–957.
Napodano, M., Ramondo, A., Tarantini, G., et al. (2009). Predictors and time-related impact of distal embolization during primary angioplasty. European Heart Journal, 30, 305–313.
Izgi, A., Kirma, C., Tanalp, A. C., et al. (2007). Predictors and clinical significance of angiographically detected distal embolization after primary percutaneous coronary interventions. Coronary Artery Disease, 18, 443–449.
Mathew, V., & Gersh, B. J. (2004). To open or not to open: that remains the question. European Heart Journal, 25, 2177–2179.
Hou, H., Ge, Z., Ying, P., et al. (2012). Biomarkers of deep venous thrombosis. Journal of Thrombosis and Thrombolysis, 34, 335–346.
Erkol, A., Oduncu, V., Turan, B., et al. (2014). The value of plasma D-dimer level on admission in predicting no-reflow after primary percutaneous coronary intervention and long-term prognosis in patients with acute ST segment elevation myocardial infarction. Journal of Thrombosis and Thrombolysis, 38, 339–347.
Zhang, H., Qiu, B., Zhang, Y., et al. (2018). The value of pre-infarction angina and plasma D-dimer in predicting no-reflow after primary percutaneous coronary intervention in ST-segment elevation acute myocardial infarction patients. Medical Science Monitor, 24, 4528–4535.
Sarli, B., Akpek, M., Baktir, A. O., et al. (2015). Impact of D-dimer level on postinterventional coronary flow and in-hospital mace in ST-segment elevation myocardial infarction. Herz, 40, 507–513.
Alpert, J. S. (2018). The fourth edition of the universal definition of myocardial infarction. The American Journal of Medicine, 131, 1265–1266.
Gibson, C. M., Murphy, S. A., Rizzo, M. J., et al. (1999). Relationship between TIMI frame count and clinical outcomes after thrombolytic administration. Thrombolysis in myocardial infarction (TIMI) study group. Circulation, 99, 1945–1950.
Rezkalla, S. H., & Kloner, R. A. (2002). No-reflow phenomenon. Circulation, 105, 656–662.
Gibson, C. M., de Lemos, J. A., Murphy, S. A., et al. (2001). Combination therapy with abciximab reduces angiographically evident thrombus in acute myocardial infarction: a timi 14 substudy. Circulation, 103, 2550–2554.
Gottdiener, J. S., Bednarz, J., Devereux, R., et al. (2004). American society of echocardiography recommendations for use of echocardiography in clinical trials. Journal of the American Society of Echocardiography, 17, 1086–1119.
Horie, H., Takahashi, M., Minai, K., et al. (1998). Long-term beneficial effect of late reperfusion for acute anterior myocardial infarction with percutaneous transluminal coronary angioplasty. Circulation, 98, 2377–2382.
Steg, P. G., Thuaire, C., Himbert, D., et al. (2004). Decopi (desobstruction coronaire en post-infarctus): a randomized multi-centre trial of occluded artery angioplasty after acute myocardial infarction. European Heart Journal, 25, 2187–2194.
Hochman, J. S., Lamas, G. A., Knatterud, G. L., et al. (2005). Design and methodology of the occluded artery trial (OAT). American Heart Journal, 150, 627–642.
Ramjane, K., Han, L., & Jin, C. (2008). The diagnosis and treatment of the no-reflow phenomenon in patients with myocardial infarction undergoing percutaneous coronary intervention. Experimental and Clinical Cardiology, 13, 121–128.
Ardissino, D., Merlini, P. A., Bauer, K. A., et al. (2003). Coagulation activation and long-term outcome in acute coronary syndromes. Blood, 102, 2731–2735.
Silvain, J., Collet, J. P., Nagaswami, C., et al. (2011). Composition of coronary thrombus in acute myocardial infarction. Journal of the American College of Cardiology, 57, 1359–1367.
Limbruno, U., De Carlo, M., Pistolesi, S., et al. (2005). Distal embolization during primary angioplasty: histopathologic features and predictability. American Heart Journal, 150, 102–108.
Undas, A., Szuldrzynski, K., Stepien, E., et al. (2008). Reduced clot permeability and susceptibility to lysis in patients with acute coronary syndrome: effects of inflammation and oxidative stress. Atherosclerosis, 196, 551–557.
Becattini, C., Lignani, A., Masotti, L., Forte, M. B., & Agnelli, G. (2012). D-dimer for risk stratification in patients with acute pulmonary embolism. Journal of Thrombosis and Thrombolysis, 33, 48–57.
Hochuli, M., Duewell, S., & Frauchiger, B. (2007). Quantitative D-dimer levels and the extent of venous thromboembolism in CT angiography and lower limb ultrasonography. Vasa, 36, 267–274.
Jeebun, V., Doe, S. J., Singh, L., Worthy, S. A., & Forrest, I. A. (2010). Are clinical parameters and biomarkers predictive of severity of acute pulmonary emboli on CTPA? QJM, 103, 91–97.
Ghanima, W., Abdelnoor, M., Holmen, L. O., et al. (2007). D-dimer level is associated with the extent of pulmonary embolism. Thrombosis Research, 120, 281–288.
Kikkert, W. J., Claessen, B. E., Stone, G. W., et al. (2014). D-dimer levels predict ischemic and hemorrhagic outcomes after acute myocardial infarction: a horizons-ami biomarker substudy. Journal of Thrombosis and Thrombolysis, 37, 155–164.
Pengo, V., Palareti, G., Cosmi, B., et al. (2008). D-dimer testing and recurrent venous thromboembolism after unprovoked pulmonary embolism: a post-hoc analysis of the prolong extension study. Thrombosis and Haemostasis, 100, 718–721.
Verhovsek, M., Douketis, J. D., Yi, Q., et al. (2008). Systematic review: D-dimer to predict recurrent disease after stopping anticoagulant therapy for unprovoked venous thromboembolism. Annals of Internal Medicine, 149(481–490), W494.
Kearon, C., Spencer, F. A., O'Keeffe, D., et al. (2015). D-dimer testing to select patients with a first unprovoked venous thromboembolism who can stop anticoagulant therapy: a cohort study. Annals of Internal Medicine, 162, 27–34.
Palareti, G., Cosmi, B., Legnani, C., et al. (2006). D-dimer testing to determine the duration of anticoagulation therapy. The New England Journal of Medicine, 355, 1780–1789.
Kucher, N., Schroeder, V., & Kohler, H. P. (2003). Role of blood coagulation factor xiii in patients with acute pulmonary embolism. Correlation of factor xiii antigen levels with pulmonary occlusion rate, fibrinogen, D-dimer, and clot firmness. Thrombosis and Haemostasis, 90, 434–438.
Yip, H. K., Chen, M. C., Chang, H. W., et al. (2002). Angiographic morphologic features of infarct-related arteries and timely reperfusion in acute myocardial infarction: predictors of slow-flow and no-reflow phenomenon. Chest, 122, 1322–1332.
Yousef, Z. R., Redwood, S. R., Bucknall, C. A., Sulke, A. N., & Marber, M. S. (2002). Late intervention after anterior myocardial infarction: effects on left ventricular size, function, quality of life, and exercise tolerance: results of the open artery trial (toat study). Journal of the American College of Cardiology, 40, 869–876.
Dzavik, V., Buller, C. E., Lamas, G. A., et al. (2006). Randomized trial of percutaneous coronary intervention for subacute infarct-related coronary artery occlusion to achieve long-term patency and improve ventricular function: the total occlusion study of Canada (TOSCA)-2 trial. Circulation, 114, 2449–2457.
Acknowledgments
The authors would like to thank the research staff for their help.
Funding
This work was supported by the National Key Research and Development Program of China (2016YFC1301200) and the National Natural Science Foundation of China (81200170, 81870269, 81570223).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human Subjects/Informed Consent Statement
No treatment was tested in patients by the authors for this article. Fudan University affiliated Zhongshan Hospital Ethics Committee had approved the work and received all the written informed consent.
Additional information
Associate Editor Craig M. Stolen oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xue Gong and Xiaoting Lei are co-first authors.
Rights and permissions
About this article
Cite this article
Gong, X., Lei, X., Huang, Z. et al. D-Dimer Level Predicts Angiographic No-Reflow Phenomenon After Percutaneous Coronary Intervention Within 2–7 Days of Symptom Onset in Patients with ST-Segment Elevation Myocardial Infarction. J. of Cardiovasc. Trans. Res. 14, 728–734 (2021). https://doi.org/10.1007/s12265-020-09991-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-020-09991-6