Abstract
Objective
Preintervention thrombus burden in the infarct-related artery is an independent predictor of no-reflow and adverse outcomes in coronary artery disease. The role of D-dimers in the acute phase of ST-elevated myocardial infarction (STEMI) during primary percutaneous coronary intervention (PCI) has not been fully elucidated. We aimed to investigate the predictive value of serum D-dimer levels on the outcome of patients with STEMI.
Methods and results
A total of 266 consecutive patients presenting with STEMI within the first 12 h of symptom onset were included in this study. Patients were divided into two groups based on the postinterventional Thrombolysis In Myocardial Infarction (TIMI) flow grade score. Postinterventional TIMI grades of 0, 1, or 2 were defined as no-reflow (group 1) and angiographic success was defined as TIMI 3 flow (group 2). D-dimer levels were significantly higher in patients with postinterventional no-reflow than in patients with postinterventional TIMI grade 3 flow (686 ± 236 μg/ml–418 ± 164 μg/ml, p < 0.001). Multivariate logistic regression analysis showed that D-dimer level was an independent predictor of postinterventional no-reflow (OR: 1.005; 95 % CI: 1.003–1.007; p < 0.001) and in-hospital major adverse cardiovascular events (MACE; OR: 1.002; 95 % CI: 1.000–1.004; p = 0.029). Receiver operator characteristics analysis provided a cut-off value of 549 μg/ml for D-dimer for predicting no-reflow with an 83 % sensitivity and an 81 % specificity, and 544 μg/ml for predicting in-hospital MACE with a 69 % sensitivity and a 67 % specificity.
Conclusion
In conclusion, D-dimer levels measured on admission may be an independent predictor of no-reflow, which is also a predictor of adverse outcomes in patients with STEMI.
Zusammenfassung
Ziel
Die prävinterventionelle Thrombuslast in der vom Infarkt betroffenen Arterie stellt einen unabhängigen Prädiktor des No-Reflow-Phänomens und ungünstiger Ereignisse bei koronarer Herzkrankheit dar. Die Rolle des D-Dimers in der akuten Phase des ST-Strecken-Hebungs-Infarkts (STEMI) bei primärer perkutaner Koronarintervention (PCI) ist noch nicht vollständig geklärt. Ziel der Studie war es, den prädiktiven Wert der D-Dimer-Serumspiegel für den Verlauf bei Patienten mit STEMI zu untersuchen.
Methoden und Ergebnisse
Insgesamt wurden 266 Patienten mit STEMI, die sich innerhalb der ersten 12 h nach Beginn der Symptome vorstellten, konsekutiv in die Studie aufgenommen. Die Patienten wurden gemäß ihrem postinterventionellen Grad des Blutflusses nach TIMI („thrombolysis in myocardial infarction“) in 2 Gruppen aufgeteilt. Ein postinterventioneller TIMI-Grad von 0, 1 oder 2 wurde als No-Reflow-Phänomen (Gruppe 1) und ein angiographischer Erfolg als TIMI-Fluss von 3 definiert (Gruppe 2). Bei Patienten mit postinterventionellem No-Reflow-Phänomen waren die D-Dimer-Werte signifikant höher als bei Patienten mit postinterventionellem Fluss von TIMI-Grad 3 (686 ± 236 μg/ml–418 ± 164 μg/ml; p < 0,001). Die multivariate logistische Regressionsanalyse ergab, dass der D-Dimer-Spiegel ein unabhängiger Prädiktor für ein postinterventionelles No-Reflow-Phänomen (OR: 1,005; 95%-KI: 1,003–1,007; p < 0,001) und für größere unerwünschte kardiovaskuläre Ereignisse („major adverse cardiovascular events“, MACE) während des stationären Aufenthalts (OR: 1,002; 95%-KI: 1,000–1,004; p = 0,029) war. Nach der Receiver-operating-characteristics-Analyse ergab sich ein D-Dimer-Grenzwert von 549 μg/ml, um ein No-Reflow-Phänomen mit einer Sensitivität von 83 % und einer Spezifität von 81 % vorherzusagen, und ein D-Dimer-Grenzwert von 544 μg/ml, um MACE während des stationären Aufenthalts mit einer Sensitivität von 69 % und einer Spezifität von 67 % vorherzusagen.
Schlussfolgerung
Fazit ist, dass der bei Aufnahme bestimmte D-Dimer-Spiegel möglicherweise ein unabhängiger Prädiktor für ein No-Reflow-Phänomen ist, welches auch einen Prädiktor für unerwünschte Ereignisse bei Patienten mit STEMI darstellt.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Since the introduction of catheter-based reperfusion strategies, a great improvement has been achieved in the survival of patients presenting with ST-segment elevation myocardial infarction (STEMI) [1, 2]. Increasing data show that primary percutaneous coronary intervention (PCI) is the most successful and rapid way of reperfusion in STEMI [3]. However, in some of patients with STEMI, primary PCI may fail to restore microvascular and myocardial reperfusion because of distal microembolization known as the no-reflow phenomenon [4].
D-dimer is a specific product of fibrin degradation that results from the activation of thrombin, activated factor XIII, and plasmin [5]. Presence of D-dimer in plasma is indicative of thrombus formation. In patients with STEMI, it has been shown that preinterventional thrombus burden in the infarct-related artery (IRA) is an independent predictor of no-reflow [6, 7, 8].
Since intracoronary thrombosis plays a key role in the pathogenesis of STEMI, measurement of D-dimer, a marker of thrombosis and hypercoagulable state, may provide valuable information in this direction. We considered that the D-dimer value could be related to the amount of fibrin formation [9]. Although the predictive value of D-dimer for cardiovascular mortality in STEMI has been shown previously, the way in which the mortality increases needs to be clarified. Therefore, in this study we aimed to investigate the predictive value of serum D-dimer concentration in predicting postinterventional no-reflow and in-hospital major adverse cardiovascular events (MACE) in patients with STEMI.
Patients and methods
Between September 2012 and July 2013, 294 patients with STEMI presented to the emergency department of Kayseri Education and Research Hospital. A total of 266 consecutive patients (137 male, mean age 64 ± 10 years) presenting with STEMI within the first 12 h of symptom onset were prospectively included in this study and 28 patients were excluded according to exclusion criteria. Inclusion criteria were: (1) presentation within 12 h of symptom onset and ECG findings consistent with acute STEMI (1 mm ST elevation in two contiguous limb leads or 2 mm in precordial leads or new-onset left bundle brunch block); (2) total occlusion of the infarct-related artery at the time of intervention. All enrolled participants were treated with primary PCI. Exclusion criteria were: (1) TIMI 1 or greater flow of the IRA on initial angiography; (2) saphenous vein graft occlusion; (3) presentation with cardiogenic shock or cardiac arrest; (4) patients with normal coronary arteries; (5) patients with coronary anatomy favorable for emergency coronary artery by-pass grafting surgery. Patients with known congestive heart failure, previous deep venous thrombosis or pulmonary emboli history, malignancy, advanced liver and kidney disease, and patients on oral anticoagulants were also excluded. Patients were divided into two groups based on the postinterventional Thrombolysis In Myocardial Infarction (TIMI) flow grade score. Postinterventional TIMI grades 0, 1, or 2 were defined as no-reflow (group 1) [10, 11]. Angiographic success was defined as TIMI 3 flow (group 2). In patients with postinterventional TIMI grade 3 flow, the myocardial blush grade (MBG) was also analyzed. MBG of the infarct region was classified as follows: 0 = no myocardial blush or contrast density; 1 = minimal myocardial blush or contrast density; 2 = myocardial blush or contrast density that exists to a lesser extent and its clearance is reduced compared with noninfarct-related coronary artery; and 3 = normal myocardial blush or contrast density comparable with that obtained during angiography of a contralateral or an ipsilateral noninfarct-related coronary artery. Adequate tissue reperfusion was defined as MBG 2 or 3 after PCI. Patients were then divided into two groups according to MBGs. Patients with MBG 0 and 1 were defined as having poor myocardial blush and patients with MBG 2 and 3 were defined as having good myocardial blush.
Blood samples for D-dimer analysis were obtained during the initial evaluation of patients in the emergency department and all measurements were performed 15 min after blood collection by using a commercial D-dimer assay (MDA immunoturbidimetric assay; Organon Teknika). Blood sampling for D-dimer measurement was made before administration of clopidogrel, heparin, or GP IIb/IIIa inhibitor. Total cholesterol, triglyceride, and low-density lipoprotein (LDL) levels were also measured using an Olympus AU-640 analyzer (Mishima Olympus Co. Ltd, Shizuoka, Japan). All patients received 300 mg aspirin, 600 mg clopidogrel, and 5,000 IU of unfractionated heparin in the catheterization laboratory before intervention. Transthoracic echocardiography was performed on all patients to evaluate left ventricular ejection fraction (LVEF) immediately after primary PCI in the coronary care unit.
Selective coronary angiography and primary PCI were performed using the standard Judkins technique (Siemens Artis Zee Floor, Munich, Germany) by experienced interventional cardiologists who carry out an average of more than 75 PCI/year. Coronary angioplasty was performed via a femoral approach using standard 6- or 7-Fr guiding catheters. After visualizing the left and right coronary arteries, 150 μg nitroglycerine was selectively injected into the IRA to rule out a possible coronary spasm. Only bare-metal stents with or without balloon predilatation were used in this study. Glycoprotein IIb/IIIa inhibitors were used in the coronary care unit as per the operator’s discretion after primary PCI. Digital angiograms were analyzed after procedures for the classification of TIMI flow grade and blush grades by two independent, experienced interventional cardiologists, blinded to the laboratory results. A postinterventional TIMI flow grade of less than 3 was defined as no-reflow. Electrocardiograms were obtained before and after 60 min of PCI to assess ST-segment resolution.
MACE was defined as nonfatal MI, in-stent thrombosis, and in-hospital mortality during hospitalization. Nonfatal MI was defined as a new rise of more than 20 % in cardiac biomarkers accompanied with recurrent chest pain and/or ischemic ECG changes. In-stent thrombosis was defined as angiographically documented total occlusion of the IRA.
All analyses were carried out using SPSS 15.0 for Windows (SPSS Inc., Chicago, Ill., USA). Continuous variables are given as mean ± standard deviation; categorical variables are defined as percentages. The variables were analyzed using the Kolmogorov–Smirnov test to determine whether or not they were normally distributed. An independent-samples t test was used to compare continuous variables between the two groups. Nonparametric values were compared with the Mann–Whitney U test. The chi-square test was used to compare categorical data. The effects of different variables on no-reflow and in-hospital MACE were calculated using univariate analyses for each variable. The variables for which the unadjusted p value was less than 0.10 in logistic regression analysis were identified as potential risk markers and included in the full model. We reduced the model using backward elimination multivariate logistic regression analyses, and we eliminated potential risk markers using likelihood ratio tests. A receiver operator characteristic (ROC) curve was constructed to determine the predictive value of D-dimer on no-reflow and in-hospital MACE. A two-tailed p value of < 0.05 was considered significant.
Results
After primary PCI, TIMI grade 3 flow was achieved in 203 patients (130 male, mean age 63 ± 9 years) and in 63 patients (39 male, mean age 64 ± 10 years) no-reflow (< TIMI grade 3 flow) occurred. Of 203 patients with postinterventional TIMI grade 3 flow, the MBG was 0 in 3 patients, 1 in 29 patients, 2 in 41 patients, and 3 in 162 patients. There were no significant differences between groups in terms of age, gender, history of diabetes, hypertension, and body mass index. Smoking was more frequent in the no-reflow group (41–19 %, p = 0.001, Tab. 1). Hemoglobin, total cholesterol, low-density lipoprotein (LDL) cholesterol, triglyceride levels, and platelet count were also similar in patients with postinterventional TIMI grade 3 flow and no-reflow. Admission LVEF (45 ± 9 % vs. 38 ± 9 %, p < 0.001) was significantly higher in patients with TIMI grade 3 flow than in patients with no reflow. White blood cell (WBC) count (11.9 ± 2.7 × 103/μl–10.3 ± 2.8 × 103/μl, p < 0.001), peak CKMB level (74 ± 17 U/l–51 ± 12 U/l, p < 0.001), and D-dimer levels were significantly higher in patients with no-reflow than in patients with TIMI grade 3 flow (686 ± 236 μg/ml–418 ± 164 μg/ml, p < 0.001, Tab. 1, Fig. 1). In patients with poor postinterventional myocardial blush (MBG 0–1), the D-dimer level was significantly higher than in those with good postinterventional myocardial blush (MBG 2–3; 678 ± 206–430 ± 122 μg/ml, p < 0.001, Fig. 2). The D-dimer level was significantly correlated with time from onset of symptoms to PCI (r = 0.268, p = 0.001), indicating the impact of thrombus age on D-dimer level.
Stent length (21 ± 4–17 ± 3 mm, p < 0.001) and glycoprotein IIb-IIIa inhibitor administration rate (35–15 %, p = 0.001) were significantly higher in patients with no-reflow. In-hospital MACE occurred in 20 (31 %) patients in the no-reflow group and 17 (8 %) patients in the TIMI grade 3 flow group (p < 0.001). The mean luminal diameter of the IRA was 3.23 ± 0.5 for LAD occlusions, 2.91 ± 0.4 for LCX occlusions, and 2.87 ± 0.4 for RCA occlusions.
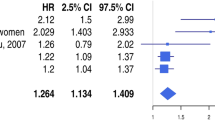
There was a significant inverse correlation between D-dimer level and ST-segment resolution (r = − 0.538, p < 0.001). Multivariate logistic regression analysis showed that WBC count (OR: 1.144; 95 % CI: 1.007–1.300; p = 0.039), D-dimer level (OR: 1.005; 95 % CI: 1.003–1.007; p < 0.001), stent length (OR: 1.259; 95 % CI: 1.139–1.391; p < 0.001), time to intervention (OR: 1.007; 95 % CI: 1.002–1.013; p = 0.009), and current smoking (OR: 2.583; 95 % CI: 1.152–5.789; p = 0.021) were independent predictors of postinterventional no-reflow (Tab. 2). In addition, age (OR: 1.066; 95 % CI: 1.015–1.119; p = 0.011), left anterior descending artery (LAD) occlusion (OR: 2.990; 95 % CI: 1.163–7.691; p = 0.023), D-dimer level (OR: 1.002; 95 % CI: 1.000–1.004; p = 0.029), WBC count (OR: 1.190; 95 % CI: 11.032–1.371; p = 0.016), LVEF (OR: 0.946; 95 % CI: 0.904–0.990; p = 0.017), and postinterventional no-reflow (OR: 3.231; 95 % CI: 1.011–10.33; p = 0.038) were independent predictors of in-hospital MACE (Tab. 3). Logistic regression analysis also revealed that the D-dimer level was an independent predictor of poor postinterventional myocardial blush (OR: 1.009; 95 % CI: 1.005–1.012; p < 0.001). ROC analysis provided a cut-off value of 549 μg/ml for D-dimer in predicting no-reflow with an 83 % sensitivity and an 81 % specificity; the area under the ROC curve was 0.88 (95 % CI 0.82–0.94; p < 0.001) and 544 μg/ml for predicting in-hospital MACE with a 69 % sensitivity and a 67 % specificity, with the area under the ROC curve being 0.72 (95 % CI 0.60–0.83; p < 0.001, Fig. 3).
Discussion
The present study clearly shows that in patients with STEMI and postinterventional TIMI < grade 3 flow, D-dimer level is significantly higher than in those with postinterventional TIMI grade 3 flow. Our study also shows that the D-dimer level at presentation may be an independent predictor of postinterventional no-reflow, poor postinterventional MBG, and in-hospital MACE.
STEMI is one of the leading causes of death globally. Excellent improvement in survival has been observed in the last two decades among patients with STEMI owing to the development of catheter-based reperfusion strategies [12, 13]. Substantial data have demonstrated the superiority of primary PCI with stents over alternative reperfusion strategies. However, in a substantial proportion of patients presenting with STEMI, despite achievement of optimal epicardial coronary flow with primary PCI, microvascular reperfusion cannot be gained owing to the no-reflow phenomenon [14]. Angiographic no-reflow is defined as less than TIMI 3 flow without any arterial obstruction, dissection, or spasm on angiography [15]. Although the pathophysiology of no-reflow has not been fully elucidated, its etiology appears to be multifactorial. These factors include ischemic endothelial damage, microvascular leukocytes and platelet plugging, reactive oxygen species, and complex interactions between leukocytes and platelets induced by the inflammatory process. However, distal microembolization is thought to be the leading process in the occurrence of no-reflow [16]. There is evidence to suggest that coronary microembolization caused by mechanical crushing and fragmentation of the thrombus in the culprit lesion during PCI is the major cause of no-reflow in humans [5, 17]. High thrombus burden, presence of floating thrombus, a longer time to reperfusion, an IRA > 4 mm, admission mean platelet volume, high endothelin-1 and thromboxane-A2 levels, and using thrombus aspiration have been shown as predictors of no-reflow [6, 18, 19, 20]. A series of consistent data have clearly shown that early postinfarct complications, left ventricular adverse remodeling, and mortality are more frequently observed in patients with no-reflow [21, 22, 23]. Therefore, demonstrating the underlying mechanisms of no-reflow, developing new treatment strategies, and the prevention of no-reflow may have an important impact on the outcome of primary PCI.
Acute myocardial infarction (AMI) is the result of occlusive coronary thrombosis, owing to the exposure of blood to atherosclerotic plaque contents. In the setting of STEMI, a growing thrombus subsequently limits or completely blocks coronary blood flow. Limbruna et al. [24] showed that high thrombus burden at the site of the IRA is predictive of distal embolization, which is accepted as the leading cause of no-reflow. During primary PCI, fragmentation of epicardial coronary thrombus into microspheric embolic particles of different sizes leads to obstruction in the microvascular coronary circulation [25]. In experimental observations, over 50 % of obstructions of coronary capillaries by microspheres have been shown to lead to irreversible decrease in myocardial blood flow [26].
D-dimer is a primary degradation product of cross-linked fibrin, an indicator of ongoing fibrinolysis and the severity of a hypercoagulable state. D-dimer is widely used in the initial evaluation of patients suspected of having deep vein thrombosis and acute pulmonary embolism (PE) [27]. Moreover, several studies conducted in the past decade have shown that D-dimer testing might be helpful in the diagnosis and prognosis of patients with acute chest pain, unstable angina pectoris, and non-STEMI [28, 29]. However, data concerning the role of D-dimer testing in STEMI are still unclear. In a recent study, Akgul et al. [30] showed that 6-month cardiovascular mortality was significantly higher in patients with STEMI and high D-dimer levels on admission. They also found that the admission D-dimer level was an independent predictor of 6-month cardiovascular mortality. However, the association between high D-dimer level and cardiovascular mortality needs to be clarified. In our study, we found that admission D-dimer level is an independent predictor of no-reflow, which may result in increased cardiovascular mortality. With this background in mind, we speculate that in patients with STEMI and high D-dimer level, postinterventional no-reflow, which can be predicted by high admission D-dimer levels, is the leading cause of cardiovascular death.
D-dimer is a reliable and sensitive index of fibrin deposition and hypercoagulable state [5]. It has been suggested that D-dimer levels reflect a systemic prothrombotic state and focal vessel wall-related fibrin formation with unstable atherosclerotic plaque activity [30]. Therefore, its presence in plasma should be indicative of thrombus formation [9]. Hochuli et al. [6] have shown that D-dimer level is associated with clot burden in patients with PE. Thrombus burden, which may be associated with high D-dimer levels, is a well-known independent predictor of slow-flow or no-reflow [31]. In our study, high levels of D-dimer observed in patients with no-reflow are probably a consequence and reflection of a preexisting high thrombus burden in the IRA.
Study limitations
Our study has some limitations. It is a single-center experience and represents a small proportion of patients. However, our population contains homogeneous unselected patients with STEMI who underwent primary PCI within 12 h of symptom onset, thereby mirroring the real-world scenario. In our study we presented in-hospital events. Lack of follow-up data may be a limitation for our study. In addition, lack of data regarding magnetic resonance imaging is another limitation. Also, we did not evaluate high-sensitivity C-reactive protein, other proinflammatory cytokines, or markers of oxidative stress.
Conclusion
In conclusion, D-dimer level measured on admission may be a predictor of postinterventional no-reflow and in-hospital MACE in patients with STEMI undergoing primary PCI. More aggressive treatment including thrombus aspiration and upstream Gp IIb/IIIa administration might be useful in preventing postinterventional no-reflow and slow-flow in patients with STEMI and high D-dimer level. However, congestive heart failure that is a major determinant of intermediate and long-term mortality in STEMI patients should be taken into consideration as a goal of treatment in follow-up. Apart from their predictive value, D-dimer levels may be useful as a biomarker for stratification of risk; they provide valuable and timely information about post-PCI adverse outcomes in patients with STEMI and may also lead to further therapeutic implications.
References
Kaya MG, Uyarel H, Akpek M et al (2012) Prognostic value of uric acid in patients with ST-elevated myocardial infarction undergoing primary coronary intervention. Am J Cardiol 109:486–491
Cura F, Albertal M, Thierer J et al (2011) Quality of myocardial reperfusion according to ischemic time and infarcted territory. Coron Artery Dis 22:92–95
Buyukkaya E, Poyraz F, Karakas MF et al (2013) Usefulness of monocyte chemoattractant protein-1 to predict no-reflow and three-year mortality in patients with ST-Segment Elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol 112:187–193
Akpek M, Kaya MG, Lam YY et al (2012) Relation of neutrophil/lymphocyte ratio to coronary flow to in-hospital major adverse cardiac events in patients with ST-elevated myocardial infarction undergoing primary coronary intervention. Am J Cardiol 110:621–627
Tripodi A (2011) D-dimer testing in laboratory practice. Clin Chem 57:1256–1262
Yip HK, Chen MC, Chang HW et al (2002) Angiographic morphologic features of infarct-related arteries and timely reperfusion in acute myocardial infarction: predictors of slow-flow and noreflow phenomenon. Chest 122:1322–1332
Sianos G, Papafaklis MI, Daemen J et al (2007) Angiographic stent thrombosis after routine use of drug-eluting stents in ST-segment elevation myocardial infarction: the importance of thrombus burden. J Am Coll Cardiol 50:573–583
Kirma C, Izgi A, Dundar C et al (2008) Clinical and procedural predictors of no-reflow phenomenon after primary percutaneous coronary interventions: experience at a single center. Circ J 72:716–721
Hochuli M, Duewell S, Frauchiger B (2007) Quantitative d-dimer levels and the extent of venous thromboembolism in CT angiography and lower limb ultrasonography. Vasa 36:267–274
Rezkalla SH, Dharmashankar KC, Abdalrahman IB et al (2010) No-reflow phenomenon following percutaneous coronary intervention for acute myocardial infarction: incidence, outcome, and effect of pharmacologic therapy. J Interv Cardiol 23:429–436
Niccoli G, Lanza GA, Spaziani C et al (2007) Baseline systemic inflammatory status and no-reflow phenomenon after percutaneous coronary angioplasty for acute myocardial infarction. Int J Cardiol 117:306–311
Sarli B, Baktir AO, Saglam H et al (2013) Mean platelet volume is associated with poor postinterventional myocardial blush grade in patients with ST-segment elevation myocardial infarction. Coron Artery Dis 24:285–289
Kırma C, Oduncu V, Tanalp AC et al (2011) Primary angioplasty in a high-volume tertiary center in Turkey: in-hospital clinical outcomes of 1625 patients. Turk Kardiyol Dern Ars 39:300–307
Niccoli G, Burzotta F, Galiuto L et al (2009) Myocardial no-reflow in humans. J Am Coll Cardiol 54:281–292
Resnic FS, Wainstein M, Lee MK et al (2003) No-reflow is an independent predictor of death and myocardial infarction after percutaneous coronary intervention. Am Heart J 145:42–46
Topol EJ, Yadav JS (2000) Recognition of the importance of embolization in atherosclerotic vascular disease. Circulation 101:570–580
Ramjane K, Han L, Jin C (2008) The diagnosis and treatment of the no-reflow phenomenon in patients with myocardial infarction undergoing percutaneous coronary intervention. Exp Clin Cardiol 13:121–128
Nallamothu BK, Bradley EH, Krumholz HM (2007) Time to treatment in primary percutaneous coronary intervention. N Engl J Med 357:1631–1638
Niccoli G, Giubilato S, Russo E et al (2008) Plasma levels of thromboxane A2 on admission are associated with no-reflow after primary percutaneous coronary intervention. Eur Heart J 29:1843–1850
Niccoli G, Lanza GA, Shaw S (2006) Endothelin-1 and acute myocardial infarction: a no-reflow mediator after successful percutaneous myocardial revascularization. Eur Heart J 27:1793–1798
Brosh D, Assali AR, Mager A et al (2007) Effect of no-reflow during primary percutaneous coronary intervention for acute myocardial infarction on six-month mortality. Am J Cardiol 99:442–445
Henriques JP, Zijlstra F, Hof AW van ‘t et al (2003) Angiographic assessment of reperfusion in acute myocardial infarction by myocardial blush grade. Circulation 107:2115–2119
Gibson CM, Cannon CP, Murphy SA et al (2002) Relationship of the TIMI myocardial perfusion grades, flow grades, frame count, and percutaneous coronary intervention to long-term outcomes after thrombolytic administration in acute myocardial infarction. Circulation 105:1909–1913
Limbruno U, De Carlo M, Pistolesi S et al (2005) Distal embolization during primary angioplasty: histopathologic features and predictability. Am Heart J 150:102–108
Skyschally A, Leineweber K, Gres P et al (2006) Coronary microembolization. Basic Res Cardiol 101:373–382
Hori M, Inoue M, Kitakaze M et al (1986) Role of adenosine in hyperemic response of coronary blood flow in microembolization. Am J Physiol 250:H509–H518
Goldhaber SZ, Bounameaux H (2012) Pulmonary embolism and deep vein thrombosis. Lancet 379:1835–1846
Turker Y, Dogan A, Ozaydin M et al (2010) Association of thrombotic and fibrinolytic factors with severity of culprit lesion in patients with acute coronary syndromes without ST elevation. South Med J 103:289–294
Saigo M, Hsue PY, Waters DD (2004) Role of thrombotic and fibrinolytic factors in acute coronary syndromes. Prog Cardiovasc Dis 46:524–538
Akgul O, Uyarel H, Pusuroglu H et al (2013) Predictive value of elevated D-dimer in patients undergoing primary angioplasty for ST elevation myocardial infarction. Blood Coagul Fibrinolysis 24:704–710
Davies MJ (1990) A macro and micro view of coronary vascular insult in ischemic heart disease. Circulation 82:II38–II46
Compliance with ethical guidelines
Conflict of interest. B. Sarli, M. Akpek, A.O. Baktir, O. Sahin, H. Saglam, H. Arinc, H, Odabasi, S. Dogan, S. Kurtul, Y. Dogan, and M.G. Kaya state that there are no conflicts of interest. All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sarli, B., Akpek, M., Baktir, A. et al. Impact of D-dimer level on postinterventional coronary flow and in-hospital MACE in ST-segment elevation myocardial infarction. Herz 40, 507–513 (2015). https://doi.org/10.1007/s00059-013-4029-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-013-4029-2
Keywords
- D-dimer
- ST-segment elevation myocardial infarction
- Primary percutaneous coronary intervention
- TIMI flow grade
- Major adverse cardiovascular events