Abstract
Background: Risk stratification is currently recommended for the initial management of patients with acute pulmonary embolism (PE). Methods: We performed a meta-analysis of studies in patients with acute PE to assess the prognostic value of elevated D-dimer levels for short-term (within 30 days) and 3-month mortality. The association between D-dimer levels and markers of PE severity was also reviewed. Unrestricted searches were performed using the terms D-dimer and pulmonary embolism. Studies reporting on D-dimer levels and mortality and/or markers of PE severity were included in the review. A random-effects model was used to pool study results, funnel-plot inspection to evaluate publication bias and I squared testing to test for heterogeneity. Results: Five studies (2,885 patients) reported on D-dimer levels and short-term mortality. D-dimer levels above a prognostic cut-off were significantly associated with short-term mortality in the overall population (OR: 2.76; 95% CI: 1.83–4.14; I2 = 0%) and in hemodynamically stable patients (three studies, 874 patients; OR: 4.28; 95% CI: 1.88–9.71; I2 = 0%). Four studies (1,254 patients) reported on D-dimer levels and 3-month mortality. D-dimer levels above a prognostic cut-off were associated with 3-month mortality (OR: 4.29; 95% IC: 1.70–10.79; I2 = 0%). Overall, 14 studies assessed the association between D-dimer and markers of PE severity. An association has been observed between D-dimer levels and the degree of pulmonary artery obstruction. Conclusion: In patients with acute PE elevated D-dimer is associated with increased short-term and 3-month mortality, suggesting the potential of using this test for both diagnosis and risk stratification.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute pulmonary embolism (PE) remains associated with a substantial risk of death during the hospital stay, outcomes varying depending on patient characteristics [1]. In-hospital mortality ranges from 5.4 to 15% in recent studies in patients with acute PE [2, 3]. Current guidelines recommend that patients with acute PE should be stratified according to the risk of in-hospital death [4]. Combinations of clinical features and signs of right ventricular dysfunction or injury (right ventricle assessment at echocardiography or at computed tomography, BNP and troponins) allow prognostic stratification and could drive the early management of patients with PE [1, 4, 5]. The need for rapid and around-the-clock available tools for prognostic stratification derives from the observation that the majority of deaths for acute PE occurs during the first hours after hospital admission [6].
D-Dimer, a product of fibrin degradation, has been widely recognized to be useful in the diagnostic work-up of PE [7]. High-sensitive D-dimer tests have been proved to have a high negative predictive value in ruling out PE in patients with non-high clinical probability [7–9]. The potential role of D-dimer in risk stratification in patients with acute PE has been assessed in several studies with a particular attention to intermediate risk patients.
The aim of this paper is to report on a meta-analysis on the prognostic value of D-dimer for short-term and 3-month mortality and on a systematic review on the association between D-dimer levels and markers of PE severity.
Materials and methods
Study objectives
The objectives of this meta-analysis and review in patients with acute PE were: (1) to assess the prognostic value of elevated D-dimer levels for short-term and 3-month mortality, (2) to assess the correlation between D-dimer levels and currently accepted prognostic factors (clinical scores, right ventricular dysfunction and degree of pulmonary artery obstruction at CT scan).
For the purpose of this study, short-term death was defined as death occurring within 30 days from diagnosis, as reported in the individual studies.
Study identification
An unrestricted electronic search was performed in MedLine and Embase. Search criteria included the terms “pulmonary embolism and D-dimer”. Studies were included in this study if they had reported on: (1) patients with an objective diagnosis of PE, (2) D-dimer sampling at diagnosis of PE and (3) short-term or 3-month death and/or results of prognostic stratification. Only those studies enrolling five or more patients were considered. Studies reporting data allowing the creation of a 2 × 2 table were also included in a formal meta-analysis.
One author (A. Lignani) initially performed study selection by reviewing titles and abstracts. Candidate abstracts were then reviewed and selected for data retrieval. Only full articles were considered for analysis. Two authors (A. Lignani and M. B. Forte) reviewed each study for quality assessment and extracted data on studies and patient characteristics as well as outcomes, using standardized extraction forms. Disagreements were resolved by consensus and through revision by an additional reviewer (C. Becattini).
Because no standardized quality scoring system is available for quality assessment of observational studies, the components of the quality review were derived largely from the Egger’s quality checklist for prognostic studies [10].
Studies were assessed for the presence of eight features: description of patient characteristics, description of inclusion and exclusion criteria, potential selection bias (e.g. consecutiveness), completeness of follow-up, a priori definition of study outcomes, objectivity of outcomes, and definition and measurement of prognostic variables and treatment.
For each study, the following individual data were extracted: general data (study design, duration of follow up), patients (number of included patients, inclusion and exclusion criteria), type of patients (in-patients or out-patients), D-dimer assays (type of test, cut-off level, and overall D-dimer-positive/negative patients), number of patients who died among D-dimer-positive or -negative patients; methods for prognostic stratification (e.g. clinical score, troponin, degree of embolic obstruction at computed tomography (CT), RVD at echocardiography); study outcome: correlation between D-dimer and markers of prognosis; clinical outcome: death.
Statistical analysis
Meta-analyses of all outcomes are reported using random-effects models because fixed- and random-effects results were similar. Cochran’s Chi-square test and the I2 test for heterogeneity were used to assess between-study heterogeneity. Statistically significant heterogeneity was considered present at P < 0.10 and I2 > 50%. Pooled odds ratios (ORs) were reported with 95% confidence intervals (CIs). Publication bias was assessed visually by the use of funnel plot analysis and by Duval and Tweedie’s Trim and Fill statistics as well as Begg and Mazumdar rank correlation test when funnel plot could not definitively rule out publication bias. Analyses were performed with Review Manager 5 (The Cochrane Collaboration, Oxford, England) and Comprehensive Meta-analysis V2.
Results
Overall, 1,010 articles were found by searching “pulmonary embolism and D-dimer”. Seven-hundred-sixty-four articles were excluded by review of the title and abstracts as they were studies on diagnosis of venous thromboembolism (n = 334), review articles or editorials (n = 195), studies on laboratory or animal research (n = 82), epidemiology (n = 57), therapy (n = 37), pathophysiological value of D-dimer (n = 17) or case reports (n = 21), evaluation of D-dimer in patients without PE (n = 16) or pediatric patients (n = 5) (Fig. 1). Two-hundred-forty-six studies were reviewed as a full text version and 22 studies were retained for inclusion in the systematic review (Table 1).
In four studies [11–14] the numbers of patients with normal/elevated D-dimer who had died were not reported. For two of these studies, these numbers were obtained by contacting the authors [12, 13].
Eight different assays for D-dimer assessment were used across the considered studies (Table 2). In 11 studies an ‘ad hoc’ D-dimer cut-off for prognostic assessment was used different from the diagnostic cut-off.
D-dimer and mortality
The association between D-dimer levels and clinical outcome was reported in 11 studies [11–21] (Table 3). In nine of these studies a prognostic cut off level of D-dimer, generally higher than the diagnostic one, was identified [11–15, 17, 18, 20, 21]. These prognostic cut offs varied between studies.
Seven studies reported on the correlation between D-dimer levels and short-term outcome [11–14, 20–22]. Short-term was intended as in-hospital (two studies), 10 or 15 days (three studies), 30 days and 6 weeks (one study each). Four studies assessed the correlation between D-dimer levels and short-term adverse outcome events while specific data on death and D-dimer levels were not reported [11–14]. Data on short term mortality adequate for meta-analysis were obtained by directly contacting the authors for two of the selected studies [12, 13].
Eight studies assessed the correlation between D-dimer levels and 3-month mortality [11, 12, 15–19, 21]. All these studies reported a higher mortality in patients with elevated levels of D-dimer. D-Dimer resulted to be an independent predictor of mortality at 3 months in two of these studies [12, 18]. In two of these studies the numbers of patients with elevated/normal D-dimer levels who died/survived were not available [14, 19].
Short-term mortality
Five of the studies (2,885 patients) evaluating the correlation between short-term mortality (in four studies in hospital or 15 days and in one study at 30 days) and D-dimer levels were included in a meta-analysis [12, 13, 18, 20, 21]. A correlation was found between D-dimer levels and short-term mortality in four studies. In one study this correlation with mortality was not observed during the hospital stay but at 3 months [21].
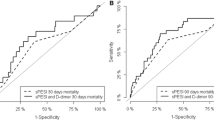
D-Dimer was above or below the prognostic cut-off in 890 and 2,027 patients, respectively. Death occurred within 30 days from diagnosis of PE in 56 and 57 patients with D-dimer levels above and below the prognostic cut-off. D-Dimer levels above the prognostic cut-offs were associated with high risk of short-term mortality (OR: 2.76; 95% CI: 1.83–4.14) with no evidence of between-studies heterogeneity (I2 = 0%) (Fig. 2a). As funnel plot inspection could not rule out definitely publication bias, further analyses were performed. Although the impact of bias probably is not trivial, the major finding of the association between elevated D-dimer and short term mortality is still valid (adjusted OR: 2.50; 95% CI: 1.69–3.68) (see Supplementary material). The association between elevated D-dimer and short term mortality was confirmed after excluding the study with the larger sample size that could dominate the analysis (OR: 4.66; 95% CI: 2.18–9.98; I2 = 0%) (Supplementary material). The association between D-dimer levels above the prognostic cut-offs and short-term mortality was confirmed in the analysis of studies only including hemodynamically stable patients (three studies, 874 patients; OR: 4.28; 95% CI: 1.88–9.71; I2 = 0%) (Fig. 2b).
Mortality at 3 months
Four studies (1,254 patients) evaluated the correlation between 3-month mortality and D-dimer levels and were included in the meta-analysis [15–17, 21]. D-Dimer was above or below the prognostic cut-off in 961 and 293 patients, respectively. Death occurred within 3 months in 96 and seven of these patients, respectively. D-Dimer levels above the prognostic cut-off were associated with increased mortality at 3 months (OR: 4.29; 95% IC: 1.70–10.79) with no evidence of between-studies heterogeneity (I2 = 0%) (Fig. 3). Given the small number of studies, publication bias could not be rule out by funnel plot inspection (see Supplementary material). Thus, further analyses were performed showing that the association between elevated D-dimer and short term mortality is valid (adjusted OR: 3.93; 95% CI: 1.64–9.44) (see Supplementary material).
D-dimer and determinants of prognosis
The correlation between D-dimer levels and tests for risk stratification in patients with acute PE was reported in 14 studies [11, 15, 16, 18, 22–31]. Different tools were used across the considered studies for prognostic assessment (Table 4).
In one observational study an association was found between PESI risk class and D-dimer levels [12].
The association between D-dimer levels and the presence of right ventricle dysfunction at CT angiography was evaluated in four studies [16, 28, 30, 31] (Table 3). In all these studies the criterion for right ventricle dysfunction at CT was the right to left ventricle diameter ratio. In two of these studies [16, 31] a positive correlation was found between right ventricle dysfunction at CT angiography and D-dimer levels while in the remaining two studies this correlation was not confirmed [28, 30]. A positive association was found in one study between D-dimer levels and right ventricle dysfunction at echocardiography [25].
The correlation between D-dimer levels and the burden of PE as assessed by CT angiography was evaluated in nine studies [16, 18, 22, 24, 26–30]. The burden of PE was evaluated by quantitative or qualitative methods in different studies (Table 4). In five studies [16, 18, 24, 27, 28] a correlation was found between a proximal location of emboli within the pulmonary vessels and D-dimer levels. Similarly, in five studies a direct correlation was observed between D-dimer levels and a quantitative measure of the burden of emboli according to the Qanadli score [32] in four studies [16, 22, 28, 30] and different scores in one [26].
Two studies evaluated the association between troponin and D-dimer levels in patients with acute PE [16, 28]. In one of these studies an association was found between D-dimer and troponin levels [16] that was not confirmed in the other study [28].
A meta-analysis of these studies was not possible, because of differences in study methodology for the assessment of severity of PE and because of absence of data, allowing the creation of a 2 × 2 table and for the different methods employed in the studies for risk stratification.
Discussion
This meta-analysis suggests that high D-dimer levels are associated with short-term and 3-month mortality in patients with acute PE. This is particularly the case when D-dimer levels are above a prognostic cut-off value. The association is confirmed in studies only including hemodynamically stable patients.
Indeed, risk stratification remains a critical point in the acute management of patients with acute PE to tailor medical and interventional therapies to appropriate patients [1]. Recent guidelines recommend risk stratification to drive admission and treatment [4]. Patients at high risk of mortality should receive thrombolytic treatment. High risk is defined based on hemodynamic status. In non-high risk patients risk stratification according to markers of right ventricle dysfunction and injury could influence decision making on in-hospital or home-treatment as well as on the need for monitoring and even on treatment upgrading. Numerous clinical predictors are available for risk stratification in these patients including biomarkers, imaging tests, ECG and clinical decision rules. Based on our results, D-dimer could have a role in risk stratification and this seems to be the case also for hemodynamically stable patients. Indeed, a definite prognostic cut-off value can not be identified as both, the D-dimer assay and the cut-off levels, vary among the studies and because the cut-offs were often defined post hoc. Thus, although our analyses show an association between D-dimer levels and mortality, this association should be interpreted as hypothesis-generating and is not ready for clinical use. More specifically, the association between high D-dimer levels and mortality needs confirmation in prospectively designed management studies with pre-defined prognostic cut-off before clinical use. The accuracy of elevated levels of D-dimer for the assessment of prognosis was compared to that of other predictors in three studies (13, 31–32). In these studies the accuracy of D-dimer compared with that of the other predictors (mainly troponin levels, echocardiography and PESI score) varied based on the selected cut-off value. Thus, a direct comparison results difficult. Moreover, as D-dimer can be influenced by several conditions (age, cancer, pregnancy, infections, etc.) we believe that its use as a single predictor of prognosis could be seen as inappropriate for its low specificity. In alternative, the clinical value of integrating D-dimer levels into clinical scores should be defined. This strategy could be of value as it offers the opportunity of using the same test for diagnosis and risk stratification, this resulting in reduction of time and costs.
The association between D-dimer levels and short-term mortality could be related to a potential link between D-dimer and PE severity. As an hypothesis, D-dimer levels could be related to the extent of thrombotic load. This hypothesis seems to be supported by the data described on Table 3 on the association between the embolic load as assessed by CT angiography and D-dimer levels. The systematic review shows that a correlation was found between D-dimer levels and markers of adverse outcome in patients with acute PE in several studies. Indeed, while conflicting results were obtained on the correlation between D-dimer levels and right ventricle dysfunction or elevated troponin, consensus exists regarding the association between elevated D-dimer and the burden of PE as assessed at CT angiography.
An association has also been suggested between D-dimer levels and PESI score.
Particularly elevated D-dimer levels in patients with acute PE could even be the result of both, the acute thromboembolic event and comorbidities. In this view, D-dimer could be very high as a result of concomitant cancer or COPD. These conditions are known predictors of outcome in patients with acute PE.
Currently, the main role of D-Dimer in the acute management of PE is in ruling out the diagnosis in patients with non high pre test clinical probability. A role has been suggested in making decision on whether discontinuing or not the long-term treatment after the first episode of unprovoked PE. Our systematic review suggests that when diagnosis of PE is performed, D-dimer values could have a role in prognostic assessment.
Our study has some limitations. A meta-analysis has the intrinsic limit of combining heterogeneous datasets. The studies included in this analysis differ for number of included patients, for duration of follow-up and, in some cases, for the main features of patients (in and out patients, inclusion of hemodynamically unstable patients, etc.). Regarding D-dimer measurements, it should be taken into account that a number of different assays have been used across the considered studies. Moreover, all the studies that evaluated the prognostic value of D-dimer used ‘ad hoc’ arbitrary prognostic cut-off. Finally, funnel plots inspection could not definitively rule out publication bias. This may be due to the limited number of available studies. However, after further specific tests were performed, publication bias could be confidently ruled out.
In conclusion, a relationship has been shown between elevated D-dimer levels and short-term and 3 months mortality in patients with acute PE. Further studies are needed to assess whether D-dimer, alone or combined with other prognostic tools for PE, may be useful to identify low-risk patients with PE who are potential candidates for outpatient treatment or an abbreviated hospital stay.
References
Jaff MR, McMurtry S, Archer SL et al (2011) Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension. A scientific statement from the American Heart Association. Circulation 123(16):1788–830
Pollack CV, Schreiber D, Goldhaber SZ et al (2011) Clinical characteristics, management, and outcomes of patients diagnosed with acute pulmonary embolism in the emergency department: initial report of EMPEROR (Multicenter Emergency Medicine Pulmonary Embolism in the Real World Registry). J Am Coll Cardiol 57:700–706
Laporte S, Mismetti P, Decousus H et al (2008) Clinical predictors for fatal pulmonary embolism in 15,520 patients with venous thromboembolism: findings from the Registro Informatizado de la Enfermedad Tromboembolica Venosa (RIETE) Registry. Circulation 117:1711–1716
Torbicki A, Perrier A, Konstantinides S et al (2008) Guidelines on the diagnosis and management of acute pulmonary embolism of the European society of cardiology. Eur Heart J 29:2276–2315
Agnelli G, Becattini C (2010) Acute pulmonary embolism. N Engl J Med 363:266–274
Wood KE (2002) Major pulmonary embolism. Review of a pathophysiologic approach to the golden hour of hemodynamically significant pulmonary embolism. Chest 121:877–905
Righini M, Perrier A, De Moerloose P et al (2008) D-Dimer for venous thromboembolism diagnosis: 20 years later. J Thromb Haemost 6:1059–1071
Writing Group for Christopher Study Investigator (2006) Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computer tomography. JAMA 295: 172–179
Le Gal G, Righini M, Roy PM et al (2006) Prediction of pulmonary embolism in the emergency department: the revised Geneva score. Ann Intern Med 144:165–171
Altman DG, Chalmers I, Egger M et al (2001) Systematic reviews in health care: meta-analysis in context, 2nd edn. UK Blackwell BMJ Books, London
Kline J, Hernandez-Nino J, Rose GA et al (2006) Surrogate markers for adverse outcomes in normotensive patients with pulmonary embolism. Crit Care Med 36:2773–2780
Agterof MJ, van Bladel E, Schutgens R et al (2009) Risk stratification of patients with pulmonary embolism based on pulse rate and D-dimer concentration. Thromb Haemost 102:683–687
Singanayagam A, Scally C, Al-khairalla MZ et al (2011) Are biomarkers additive to pulmonary embolism severity index for severity assessment in normotensive patients with acute pulmonary embolism? QJM 104:125–131
Klok FA, van der Bijl N, Eikenboom HCJ et al (2010) Comparison of CT assessed right ventricular size and cardiac biomarkers for predicting short-term clinical outcome in normotensive patients suspected of having acute pulmonary embolism. J Thromb Haemost 8:853–856
Aujesky D, Roy PM, Guy M et al (2006) Prognostic value of D-dimer in patients with pulmonary embolism. Thromb Haemost 96:478–482
Ghanima W, Abdelnoor M, Holmen LO et al (2007) D-Dimer level is associated with the extent of pulmonary embolism. Thromb Res 120:281–288
Grau E, Tenías JM, Soto MJ et al (2007) RIETE Investigators. D-dimer levels correlate with mortality in patients with acute pulmonary embolism: findings from the RIETE registry. Crit Care Med 35:1937–1941
Klok FA, Djurabi RK, Nijkeuter M et al (2008) High D-dimer level is associated with increased 15-d and 3 months mortality through a more central localization of pulmonary emboli and serious comorbidity. Br J Haematol 140:218–222
Kabbara R, Labarere J, Pernod G et al (2008) D-Dimer level is not a prognostic biomarker specific for pulmonary embolism. Crit Care Med 36:652–653
Lobo JL, Zorilla V, Aizpuru F et al (2009) RIETE investigators. D-Dimer levels and 15-day outcome in acute pulmonary embolism. Finding in the RIETE registry. J Thromb Haemost 7:1795–1801
Bova C, Pesavento R, Marchiori A et al (2009) TELESIO study group. Risk stratification and outcomes in hemodynamically stable patients with acute pulmonary embolism: a prospective, multicenter, cohort study with three months follow up. J Thromb Haemost 7:938–944
Hochuli M, Duewell S, Frauchiger B (2007) Quantitative D-dimer levels and the extent of venous thromboembolism in CT angiography and lower limb ultrasonography. Vasa 36:267–274
Gallè C, Papazyan JP, Miron MJ et al (2001) Prediction of pulmonary embolism extent by clinical findings, D-dimer level and deep vein thrombosis shown by ultrasound. Thromb Haemost 86:1156–1160
De Monyé W, Sanson BJ, Mac Gillavry MR et al (2002) ANTELOPE-study group. Embolus location affects the sensitivity of a rapid quantitative D-dimer assay in the diagnosis of pulmonary embolism. Am J Respir Crit Care Med 165:345–348
Masotti L, Antonelli F, Venturini E et al (2007) Cardiac troponin I and plasma D-dimer are related to proximal and bilateral extension of clots and right cardiac dysfunction in patients with pulmonary embolism. J Intern Med 262:588–589
Goldin Y, Berliner S, Rogowski O et al (2008) Correlated expression of D-dimer concentrations with thrombotic burden in acute pulmonary embolism. Blood Coagul Fibrinolysis 19:153–158
Sen E, Arslan F, Eladag Y et al (2009) Clinical and radiological finding in patients diagnosed with pulmonary thromboembolism by pulmonary computerized tomography angiography. Tuberk Toraks 57:5–13
Jeebun V, Doe SJ, Singh L et al (2010) Are clinical parameters and biomarkers predictive of severity of acute pulmonary emboli on CTPA? QJM 103:91–97
Nakada K, Okada T, Osada H et al (2010) Relation between pulmonary embolus volume quantified by multi detector computed tomography and clinical status and out come for patients with acute pulmonary embolism. Jpn J Radiol 28:34–42
Turedi S, Karahan SC, Mentese A et al (2010) Investigation of the relationship between D-dimer and ischemia-modified albumin levels with the radiological imaging-based pulmonary embolism severity score in acute pulmonary embolism. Anadolu Kardiyol Derg 10:346–352
Gutte H, Mortesen J, Jensen CV et al (2010) ANP, BNP, and D-dimer predict right ventricular dysfunction in patients with acute pulmonary embolism. Clin Physiol Funct Imaging 30:466–472
Qanadli SD, El Hajjam M, Viellard-Baron A et al (2001) New CT index to quantify arterial obstruction in pulmonary embolism: comparison with angiographic index and echocardiography. AJR Am J Roentgenol 176:1415–1420
Vuillemier N, Le Gal G, Verschuren F et al (2008) Cardiac biomarkers for risk stratification in non-massive pulmonary embolism: a multicenter prospective study. J Thrombo Haemost 7:391–398
Acknowledgments
We acknowledge Dr Mariette Agterof, Dr James Chalmers and Dr Aran Singanayagam for contributing to this study by sending original unpublished data.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was performed without any external support.
Electronic supplementary material
Below is the link to the electronic supplementary material.
11239_2011_648_MOESM1_ESM.eps
Figure 1. Forest plot of prognostic value of D-dimer for short-term mortality after excluding the larger study (24) (EPS 400 kb)
Rights and permissions
About this article
Cite this article
Becattini, C., Lignani, A., Masotti, L. et al. D-Dimer for risk stratification in patients with acute pulmonary embolism. J Thromb Thrombolysis 33, 48–57 (2012). https://doi.org/10.1007/s11239-011-0648-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-011-0648-8