Abstract
Pancreatic ductal adenocarcinoma (PDAC) is one of the most aggressive malignant tumors and represents the fifth most common cause of cancer-related deaths. It is associated with a poor prognosis, likely due to the tendency of the tumor for early local and distant spread. One of the major obstacles of effectively treating PDAC is the often late diagnosis. Among all options currently available for PDAC, surgical resection offers the only potential cure with 5-year survival rate of approximately 15–20 %. However, in the absence of metastatic disease, which precludes resection, assessment of vascular invasion is an important parameter for determining resectability for pancreatic cancer. The vascular involvement in patients with pancreatic carcinoma ranges between 21 and 64 %. Historically, vascular involvement has been considered a contraindication to resective cure. Meanwhile, the surgical approach of pancreatoduodenectomy (PD) combined with vascular resection and reconstruction has been widely applied in clinical practice to remove the tumor completely. Therefore, vascular invasion is no longer a surgical contraindication and the rate of surgical resection has greatly increased. Moreover, PD combined with vascular resection can account for 20 to 25 % of the total cases of PD surgery in a number of the larger pancreas treatment centers. The aim of this review is to provide an overview of management and outcome of vascular resection in PDAC surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pancreatic ductal adenocarcinoma (PDAC) is one of the few cancers with increasing incidence. It is associated with a poor prognosis, with less than 5 % of patients surviving 5 years after the diagnosis. Surgical resection remains the only chance for curative therapy in these patients. However, only 10–20 % of patients are candidates for resection as approximately 50 % present with metastatic and 35 % with locally advanced surgically unresectable disease. The dismal prognosis of PDAC is mainly associated with late diagnosis [1, 2]. Accurate preoperative staging of PDAC is essential to avoid unnecessary surgery in those with unresectable disease and, at the same time, in order not to deny the opportunity for cure in patients with resectable disease [3]. Traditionally, the standard approach for potentially resectable disease has been surgery followed by adjuvant therapy. With the recent improvement of perioperative management techniques and multimodal treatment strategy for PDAC, concomitant major vessel resection and reconstruction have thus been aggressively attempted in association with comparatively better pathologically negative surgical margins and postoperative survival [4–7].
Surgery plays a critical role in the management of PDAC, and centralization of pancreatoduodenectomy (PD), for example, to higher-volume centers with higher-volume surgeons, has contributed to a reduction in postoperative mortality, such that the risk of mortality at high-volume centers is currently as low as 3 % [5, 6].
Historically, pancreatic tumors were considered either resectable or unresectable. The first published definition for borderline resectable PDAC, which refers to tumors that are involved with nearby structures so as to be neither clearly resectable nor clearly unresectable, was by the National Comprehensive Cancer Network (NCCN) [8]. Aggressive management of this group of patients with neoadjuvant chemotherapy has made surgery feasible, and extended surgical approaches in PDAC have become commonly performed, which include vascular as well as multivisceral resections [8, 9].
This review gives an overview of the management and current state of vascular resection in PDAC surgery.
Assessment of Resectability
Determining resectability of the primary tumor is the most important goal in initial patient evaluation. High-quality computed tomography (CT) scanning can be used to classify pancreatic tumors into resectable (stage I or II), locally advanced, surgically unresectable (stage III), or metastatic (stage IV) disease [3]. In recent years, with further advances in imaging techniques, a new subgroup of patients, previously considered poor candidates for resection because of the relationship of their primary tumor to surrounding vasculature, has been detected and may benefit from resection [3, 4]. This stage of disease, termed borderline resectable PDAC, has become of increasing interest.
The International Study Group for Pancreatic Surgery (ISGPS) has published a consensus statement to define borderline resectable diseases in accordance with the guidelines of the National Comprehensive Cancer Network (NCCN) as well as the definition of extended resections [8, 10, 11]. At this consensus conference, expert participants expanded criteria for resectability on the basis of radiographic findings, including CT with a pancreas-specific protocol, the presence/absence of metastases, and the tumor’s association with blood vessels.
Three grades of resectability are defined for localized PDAC as resectable, borderline resectable, and unresectable, summarized in Table 1 [10]. PDAC is defined as resectable if tumor extension to the celiac and superior mesenteric artery (SMA) is absent, the superior mesenteric vein (SMV) and portal vein (PV) are patent, and there are no distant metastases. However, with the development of more sophisticated imaging tools and surgical techniques, more patients have been included in a growing category of borderline resectable disease [10, 11].
Those patients present with focal tumor abutment (<180°) of the SMA, encasement of the gastroduodenal artery up to the hepatic artery, or involvement of the SMV/PV that is potentially resectable and reconstructable [10].
Consequently, unresectability is defined as an encasement (more than one half of the vessel circumference) or occlusion/thrombus of the SMA, unreconstructable SMV or SMV-PV confluence occlusion, or direct involvement of the inferior vena cava, aorta, or celiac axis. The rationale for pancreatectomy combined with vascular resection is to increase the possibility to achieve a curative R0 resection. In venous borderline resectability, no neoadjuvant treatment is recommended, instead upfront surgery should be performed and—if the intraoperative finding matches the presumed borderline situation as defined above—completed as an en bloc tumor removal with venous replacement [10, 11].
Patients categorized as borderline resectable on the basis of features of arterial involvement seen at imaging should undergo surgical exploration in order to obtain further verification of any arterial infiltration, and if an arterial borderline resectability is confirmed intraoperatively as a true arterial involvement, palliative treatment should be regarded as the standard of care [10, 11]. Treatment modifications can be considered after interdisciplinary board decisions for individual patients including neoadjuvant treatment with a consecutive re-exploration and eventually resection as well as direct arterial resection in exceptional cases or under study conditions.
Up to 50 % of tumors thought to have vascular invasion intraoperatively have been found subsequently to have only inflammatory adhesions to the PV after histologic examination. This finding underlines the difficulty in determining tumoral venous invasion before and during surgery, since peritumoral inflammation may simulate true tumor infiltration. However, because current imaging cannot distinguish between cancer-associated desmoplasia and (radio) chemotherapy-induced fibrosis or fibrosis due to tumor regression [12], a surgical exploration should be performed in patients with tumor regression as well as in patients with a stable disease status after neoadjuvant therapy [13]. Patients with a clear tumor progression under neoadjuvant treatment should be excluded from secondary exploration.
Venous Resections
Historically, major vessel involvement has been a contraindication to resection in patients with PDAC. In 1973, Fortner described a surgical approach of regional pancreatectomy involving en bloc resection of peripancreatic soft tissue, regional lymph nodes with resection of the PV (type I), or resection and reconstruction of a major artery (type II). Although these extended resections achieved improved resectability rates, associated high morbidity (67 %) and mortality (23 %) with low survival rates (3-year survival rate 3 %) discouraged generalized adoption of major vessel resection and reconstruction [14]. However, major advances in radiological and surgical techniques resulting in improved preoperative staging, better patient selection, and reduced surgical morbidity and mortality could be achieved [12].
Contrary to arterial involvement, the invasion of the SMV or PV is not in itself a criterion of unresectability [15–18]. In contrast to arterial resection, PD with PV approaches gained widespread acceptance in centers around the world and can be performed safely with no increase in perioperative morbidity or mortality compared to standard PD [15–20].
When the PV or SMV is involved, it is legitimate to attempt a resection and venous excision is done either by a segmental resection or by a tangential resection [21, 22]. Figures 1 and 2 show the preoperative CT imaging with SMV infiltration and the intraoperative reconstruction. In case of segmental resection, the reconstruction requires an end-to-end anastomosis either by direct suture or by using an interposition venous or prosthetic graft. For this purpose, autologous grafting (e.g., renal vein, saphenous vein) is possible but requires venous harvesting before clamping and resection [18]. Alternatively, synthetic grafts, i.e., a ringed goretex prosthesis, can be chosen to bridge the resected vein segment [20]. For minimal tumor invasion into the PV, autologous saphenous vein patches can be used [21, 23]. Wide resection of the PV may require transection of the splenic vein. To avoid segmental portal hypertension, end-to-side reanastomosis of the splenic vein to the interposition graft is recommended. If the tumor invades the superior mesenteric vein, complete resection of the tumor is done either by tangential excision or by excision-reconstruction. When a tangential vein resection is not possible, the mesenteric root should be mobilized completely by resolving the attachment of the right hemicolon to the retroperitoneal adhesions [17]. When other surgical outcome parameters are considered, it has been demonstrated that both the resection with a direct anastomosis and the interposition of a graft can be performed safely. Numerous authors have reported a mortality rate below 5 % in patients undergoing venous resection with PD, similar to that of standard PD [17, 18, 22, 24].
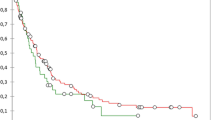
However, Siriwardana and Siriwardena [22] performed a systematic review of the outcome of synchronous PV-SMV resection during pancreatectomy for cancer. Their analysis evaluated a total of 52 studies encompassing 1646 patients undergoing vein resection mainly together with partial PD (71 %) or total PD (24 %). The median morbidity rate for patients undergoing PD with venous resection was 42 %, and the mortality rate was 5.9 %. The reported long-term survival in the review for 1351 patients was 13 months, with 1-, 3-, and 5-year overall survival rates of 50, 18, and 8 %, respectively. This demonstrates that resection of the PV or SMV is potentially curative and the involvement of the SMV or PV seems to be rather a consequence of the tumor located close to these structures than a reflection of an uncommonly aggressive tumor biology.
A more recent meta-analysis by Zhou et al. [24] involved 19 studies of pancreatectomies for pancreatic cancer and included 661 patients with and 2247 patients without portomesenteric venous resections. Both groups were characterized by comparable surgical outcome. In contrast to the study by Siriwardana and Siriwardena [22], Zhou et al. [24] found no difference in the overall survival between the cohorts with and without vascular resection. Furthermore, in terms of oncological results, no difference in overall survival between both patient collectives was found, resulting in a 5-year survival rate of 12.3 %, certainly superior to palliative treatment.
Various studies show that venous resection in PDAC is a feasible technique and relatively reliable [17–19, 22, 25]. At least favorable morbidity and mortality rates and long-term survival after these resections are much better compared to patients with only palliative management. Therefore, resection of the PV and SMV can be regarded as a standard procedure in experienced hands and should be performed in a routine setting to achieve a complete removal of the tumor.
Arterial Resections
Arterial resection for PDAC has remained an area of controversy since Fortner first introduced the concept as part of regional pancreatectomy. Currently, venous resection and reconstruction have become a somewhat routine when the pancreatic tumor cannot be separated from the adjacent SMV or PV. However, many authors regard the invasion of hepatic artery, the celiac axis of the SMA, as a contraindication to surgery, because of the high morbidity and mortality rates associated with arterial resection and reconstruction [15, 16].
Recently, with the advent of more effective systemic therapies, attention is being refocused on the potential benefit of removing the primary tumor, even in the setting of complex arterial abutment or encasement, when it is the only site of measurable disease, after neoadjuvant therapy [26]. Although in some patients arterial invasion is considered as borderline resectable according to the ISGPS consensus statement, an upfront resection is rarely recommendable, even if it can technically be performed [10]. Furthermore, arterial invasion usually predicts extensive involvement of the mesenteric neural plexus with an inability to achieve a negative retroperitoneal resection margin even with radical extended surgery.
After re-staging, patients should be subjected to surgical exploration as long as no signs of systemic tumor spread are present. Using this approach, in 33–50 % of all primarily unresectable patients, a radical resection is possible which achieves R0 resection rates comparable to standard resections [26].
The SMA first approach should be routinely used early during surgical resection in order to explore retroperitoneal tumor invasion. This artery-first approach during PD is generally carried out through a right-sided route after Kocher maneuver but can also be done through a left-sided route after lowering the duodenojejunal flexure or by an infracolic route [27]. This technique offers several oncological benefits, such as facilitating interaortocaval lymphadenectomy at the origin of the SMA and checking resectability at the retroperitoneal margin, but it also has some technical advantages, such as preventing hemorrhage by preservation of the venous return and facilitating venous resection during PD.
In a meta-analysis by Mollberg et al. [28] that included 26 studies (published from 1977 to 2010) with 366 patients undergoing arterial resection and 2243 patients without arterial resection, perioperative morbidity (median 53.6 %) and mortality (median 11.8 %) in patients undergoing arterial resection were significantly higher. Survival analysis did not show a benefit compared with patients who underwent only venous resection; however, compared with patients who did not undergo resection, the 1-year survival was favorable being threefold greater for patients with arterial resection.
Regarding resection of the SMA, only five studies were available, including a total number of less than 30 patients. All authors showed that the resection is technically possible, and grafting with the saphenous vein was the most commonly used method for reconstruction. However, morbidity of this approach is high and the oncological outcome is not yet convincing from the limited evidence.
Celiac axis or hepatic artery resection is performed more often. Current literature includes approximately 200 patients [29] on this topic. Surgical morbidity is up to 40 %, and mortality in PD with arterial resection ranges from 0 to 35 %, showing the inconsistent data basis of this approach. However, overall outcomes following PD with arterial resection seem to justify the approach especially in distal pancreatectomy and were comparable to previous reports of major cancer operations commonly performed in long-term survival and oncological results.
In summary, arterial resection can be carried out safely in experienced hands, but so far, it does not represent a standard procedure.
From the technical point of view, celiac or hepatic invasion, discovered during the operation, can be the object of a resection and a reconstruction, either by direct anastomosis or by interposition of a venous graft (for example, reverse saphenous or internal jugular vein) or with a prosthesis. The celiac axis might be resected down to its aortal orifice in PD as well as in DP or TP. As long as the proper hepatic artery can be preserved, a reconstruction is possible. An arterial graft (i.e., splenic artery) can also be used [29]. Figure 3 shows the hepatic artery reconstruction by splenic artery interposition.
Regarding the en bloc resection of the celiac trunk with distal pancreatectomy and total gastrectomy for advanced cancers of the body and tail of the pancreas, several groups propose an extended resection of the celiac trunk, splenic artery, common hepatic artery, and/or SMA, resulting in 5–6 months of average survival. Importantly, hepatic vascularization must be maintained and evaluated during the whole operation and, if necessary, compensated, because perfusion failure can cause postoperative problems like liver ischemia, necrosis, and infection and be a risk factor for bile duct-associated complications in the long-term follow-up [30].
In conclusion, arterial resection is only justified in highly selected patients and can be carried out safely in experienced hands.
Combined Vascular Resections
Data on combined vascular procedures (venous and arterial resection) are scarce. There is only very limited literature published on this topic, and no conclusive evidence with regard to perioperative morbidity and oncological outcome is available. The approach is technically feasible but is not recommended as a standard procedure and must be based on individual decisions. Further studies are needed.
Conclusions
Radical R0 resection surgery is the standard for achieving curative treatment of PDAC. Combining venous resection during PD meets this oncological requirement without increasing the morbidity and mortality of the procedure. Therefore, major venous involvement should not be considered a contraindication to resection of borderline resectable PDAC when a margin-negative resection is anticipated. Concerning arterial resection, the disappointing results might justify such extended surgery only in selected cases. All surgical approaches must be part of interdisciplinary multimodal concepts as radical resection alone cannot achieve optimal patient outcome and always needs to be followed by adjuvant treatment. Pancreatic surgery with vascular resection should be performed in a high-volume center with acceptable morbidity and mortality rates.
References
Hartwig W, Hackert T, Hinz U, Gluth A, Bergmann F, Strobel O, Büchler MW, Werner J (2011) Pancreatic cancer surgery in the new millennium: better prediction of outcome. Ann Surg 254(2):311–9
Hackert T, Büchler MW (2013) Pancreatic cancer: advances in treatment, results and limitations. Dig Dis 31(1):51–6
Soriano A, Castells A, Ayuso C, Ayuso JR, de Caralt MT et al (2004) Preoperative staging and tumor resectability assessment of pancreatic cancer: prospective study comparing endoscopic ultrasonography, helical computed tomography, magnetic resonance imaging, and angiography. Am J Gastroenterol 99:492–501
Schnelldorfer T, Ware AL, Sarr MG, Smyrk TC, Zhang L, Qin R, Gullerud RE, Donohue JH, Nagorney DM, Farnell MB (2008) Long-term survival after pancreatoduodenectomy for pancreatic adenocarcinoma: is cure possible? Ann Surg 247(3):456–62
Birkmeyer JD, Siewers AE, Finlayson EV et al (2002) Hospital volume and surgical mortality in the United States. N Engl J Med 346(15):1128–1137
McPhee JT, Hill JS, Whalen GF, Zayaruzny M, Litwin DE, Sullivan ME, Anderson FA, Tseng JF (2007) Perioperative mortality for pancreatectomy: a national perspective. Ann Surg 246(2):246–53
Hackert T, Büchler MW, Werner J (2009) Surgical options in the management of pancreatic cancer. Minerva Chir 64(5):465–76
National Comprehensive Cancer Network. Clinical practice guidelines in oncology: pancreatic adenocarcinoma. Version 1.2008 and 1.2014. Available from http://www.nccn.org
Hackert T, Tjaden C, Büchler MW (2014) Developments in pancreatic surgery during the past ten years. Zentralbl Chir 139(3):292–300
Bockhorn M, Uzunoglu FG, Adham M, Imrie C, Milicevic M, International Study Group of Pancreatic Surgery et al (2014) Borderline resectable pancreatic cancer: a consensus statement by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 155(6):977–88
Hartwig W, Vollmer CM, Fingerhut A, Yeo CJ, Neoptolemos JP, International Study Group on Pancreatic Surgery et al (2014) Extended pancreatectomy in pancreatic ductal adenocarcinoma: definition and consensus of the International Study Group for Pancreatic Surgery (ISGPS). Surgery 156(1):1–14
Bang S, Chung HW, Park SW, Chung JB, Yun M, Lee JD, Song SY (2006) The clinical usefulness of 18-fluorodeoxyglucose positron emission tomography in the differential diagnosis, staging, and response evaluation after concurrent chemoradiotherapy for pancreatic cancer. J Clin Gastroenterol 40:923–929
Habermehl D, Kessel K, Welzel T, Hof H, Abdollahi A, Bergmann F, Rieken S, Weitz J, Werner J, Schirmacher P, Büchler MW, Debus J, Combs SE (2012) Neoadjuvant chemoradiation with gemcitabine for locally advanced pancreatic cancer. Radiat Oncol 7:28
Fortner JG (1973) Regional resection of cancer of the pancreas: a new surgical approach. Surgery 73:307–320
Fuhrman GM, Leach SD, Staley CA, Cusack JC, Charnsangavej C, Cleary KR, El-Naggar AK, Fenoglio CJ, Lee JE, Evans DB (1996) Rationale for en bloc vein resection in the treatment of pancreatic adenocarcinoma adherent to the superior mesenteric-portal vein confluence. Pancreatic Tumor Study Group. Ann Surg 223:154–162
Harrison LE, Klimstra DS, Brennan MF (1996) Isolated portal vein involvement in pancreatic adenocarcinoma. A contraindication for resection? Ann Surg 224:342–347
Müller SA, Hartel M, Mehrabi A et al (2009) Vascular resection in pancreatic cancer surgery: survival determinants. J Gastrointest Surg 13:784–92
Kim PT, Wei AC, Atenafu EG, Cavallucci D, Cleary SP, Moulton CA, Greig PD, Gallinger S, Serra S, McGilvray ID (2013) Planned versus unplanned portal vein resections during pancreaticoduodenectomy for adenocarcinoma. Br J Surg 100(10):1349–56
Riediger H, Makowiec F, Fischer E, Adam U, Hopt UT (2006) Postoperative morbidity and long-term survival after pancreaticoduodenectomy with superior mesenterico-portal vein resection. J Gastrointest Surg 10:1106–1115
Hartel M, Niedergethmann M, Farag-Soliman M, Sturm JW, Richter A, Trede M, Post S (2002) Benefit of venous resection for ductal adenocarcinoma of the pancreatic head. Eur J Surg 168:707–712
Sasson A, Hoffmann J, Ross E et al (2002) En bloc resection for locally advanced cancer of the pancreas: is it worthwhile? J Gastrointest Surg 6:147–158.51
Siriwardana H, Siriwardena A (2006) Systematic review of outcome of synchronous portal-superior mesenteric vein resection during pancreatectomy for cancer. Br J Surg 93:662–673
Weitz J, Kienle P, Schmidt J et al (2007) Portal vein resection for advanced pancreatic head cancer. J Am Coll Surg 204:712–6
Zhou Y, Zhang Z, Liu Y, Li B, Xu D (2012) Pancreatectomy combined with superior mesenteric vein-portal vein resection for pancreatic cancer: a meta-analysis. World J Surg 36(4):884–91
Sindelar WF (1989) Clinical experience with regional pancreatectomy for adenocarcinoma of the pancreas. Arch Surg 124:127–132
Strobel O, Berens V, Hinz U, Hartwig W, Hackert T, Bergmann F, Debus J, Jäger D, Büchler MW, Werner J (2012) Resection after neoadjuvant therapy for locally advanced, “unresectable” pancreatic cancer. Surgery 152(3 Suppl 1):S33–42
Weitz J, Rahbari N, Koch M, Buchler MW (2010) The “artery first” approach for resection of pancreatic head cancer. J Am Coll Surg 210:e1–4
Mollberg N, Rahbari NN, Koch M, Hartwig W, Hoeger Y, Büchler MW, Weitz J (2011) Arterial resection during pancreatectomy for pancreatic cancer: a systematic review and meta-analysis. Ann Surg 254(6):882–93
Chua TC, Saxena A (2010) Extended pancreaticoduodenectomy with vascular resection for pancreatic cancer: a systematic review. J Gastrointest Surg 14(9):1442–52
Hackert T, Stampfl U, Schulz H, Strobel O, Büchler MW, Werner J (2011) Clinical significance of liver ischaemia after pancreatic resection. Br J Surg 98:1760–1765
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Luketina, R.R., Hackert, T. & Büchler, M.W. Vascular Resection in Pancreatic Cancer. Indian J Surg 77, 381–386 (2015). https://doi.org/10.1007/s12262-015-1364-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-015-1364-y