Abstract
Background
Pancreatectomy combined with superior mesenteric vein–portal vein resection (VR) for pancreatic cancer remains a matter of debate. The present study is a meta-analysis of the available evidence.
Methods
Articles published until end of March 2011, comparing the results of pancreatic resections with VR versus without VR, were searched. Pooled odds ratios (OR) and weighted mean differences (WMD; with 95% Confidence Intervals [95% CI]) were calculated using either the fixed effects model or the random effects model.
Results
Nineteen nonrandomized studies met the inclusion criteria, comprising 2,247 patients. There was no difference in perioperative morbidity (OR: 0.95; 95% CI: 0.74–1.21; P = 0.67), mortality (OR: 1.19; 95% CI: 0.73–1.96; P = 0.48), or 5-year overall survival (OR: 0.57; 95% CI: 0.32–1.02; P = 0.06) between patients with VR and those without VR.
Conclusions
Pancreatectomy combined with VR resection for pancreatic cancer is justified because it can result in good perioperative outcome and long-term survival comparable to that obtained with standard resection. Owing to the selection bias and low level of clinical evidence available so far, the results should be interpreted with caution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer is one of the most aggressive malignancies in the gastrointestinal system. Surgery may provide the only chance for long-term survival. Unfortunately, because of the presence of distant metastases or locally advanced disease in the form of vascular involvement, only 15%–20% of patients are suitable candidates for surgery [1]. Pancreatic tumor frequently extends directly into the retroperitoneal spaces and involves the superior mesenteric vein–portal vein (SMV-PV). In a further effort to improve life expectancy, in many centres a more aggressive approach involving SMV-PV resection (VR) has been performed to increase the curability of pancreatic cancer [2–11]. However, these reports have shown contradictory results. For example, Allema et al. [3] and Roder et al. [4] observed VR resection did not offer survival benefit for patients undergoing pancreaticoduodenectomy for carcinoma of the pancreas. By contrast, Takahashi et al. [5] found this procedure is associated with an improved long-term survival for patients with pancreatic cancer. In the light of this controversy, the present study used meta-analytical techniques to provide an evidence-based evaluation regarding the perioperative outcomes and long-term survival of patients undergoing VR in pancreatectomy for pancreatic cancer, compared with outcomes and survival of patients without VR.
Materials and methods
Study selection
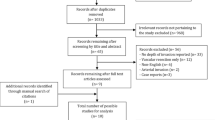
A computerized search was made of Medline and PubMed from the time of inception to July 2011. The following Mesh search headings were used: “pancreatic cancer,” “portal vein,” and “superior mesenteric vein.” Only studies on humans and in the English language were considered for inclusion. Reference lists of all retrieved articles were manually searched for additional studies.
Data extraction
Two reviewers (B.L. and Y.Z.) independently extracted the following parameters from each study: first author, year of publication, study population characteristics, study design, inclusion and exclusion criteria, number of subjects operated on with each procedure, procedure-related morbidity and mortality, and overall survival. All relevant text, tables, and figures were reviewed for data extraction.
Criteria for inclusion and exclusion
For inclusion in the meta-analysis, a study had to fulfil the following criteria: (1) compare the results of pancreatic resections with VR versus without VR for pancreatic cancer; (2) report on at least one of the outcome measures mentioned below, noting whether the standard deviation of the mean for continuous outcomes of interest was reported or could be calculated; (3) when dual (or multiple) studies were reported by the same institution and/or authors, either the one of higher quality or the most recent publication was included in the analysis.
Abstracts, letters, editorials and expert opinions, reviews without original data, case reports, and studies lacking control groups were excluded.
Outcomes of interest
Perioperative outcomes included operative time, operative blood loss, number of patients requiring blood transfusion, morbidity, and mortality. Long-term outcomes included 1-, 3-, and 5-year overall survival.
Statistical analysis
The meta-analysis was performed using the Review Manager (RevMan) software, version 4.2.7. We analyzed dichotomous variables with estimation of odds ratios (OR) together with a 95% CI, and we analyzed continuous variables with weighted mean difference (WMD) and a 95% CI. Pooled effect was calculated using either the fixed effects model or the random effects model. Statistical heterogeneity between trials was evaluated by χ2 and I2, with significance being set at p < 0.10. In the absence of statistically significant heterogeneity, the fixed-effect method was used to combine the results. When heterogeneity was confirmed (p ≤ 0.10), the random-effect method was used. Publication bias was assessed visually with a funnel plot.
Results
Eligible studies
The literature search identified 21 comparable studies that met the selection criteria. In three of the 21 studies, the VR cases and arterial resection cases were analyzed in aggregate, so no conclusions can be drawn about the outcomes for those patients undergoing VR [11–13]. Finally, a total of 19 nonrandomized studies were included for analysis [1, 3, 6–10, 14–25]. Demographics information (sex and age) was available in 17 studies [1, 3, 7, 9, 10, 14–25], and all had matched patients in the two groups. The two reviewers had 100% agreement in their reviews of the data extraction.
The 19 studies included a total of 2,247 patients: 661 with VR and 1,586 without VR. Five studies were conducted in the United States [1, 6, 7, 16, 22], three in France [8, 9, 19], five in Japan [10, 15, 17, 21, 23], two in Germany [14, 20], one in Hong Kong [18], one in the Netherlands [3], one in Taiwan [24], and one in Belgium [25].The sample size of each study varied from 45 to 158 patients. The rate of VR varied from 11.7 to 65.1%. Information on the histopathology of resected vessels was available in 15 studies [3, 7–10, 14–22, 25]. Tumor invasion was found microscopically in 279 of the 490 patients who underwent VR (56.9%; range 21–100%), while 211 had inflammatory adhesions without cancer invasion (43.1%).The characteristics of the included studies are shown in Table 1.
Meta-analysis of perioperative outcomes
Results from overall meta-analysis are outlined in Table 2. Pooled analysis of studies furnishing data found VR was associated with longer operative time (six trials reported this data, WMD: 78.77; 95% CI: 56.6–100.95; p < 0.001) and higher blood loss (four trials reported this data, WMD: 483.33; 95% CI: 142.98–823.68; P = 0.005). Concerning transfusion requirements, despite there being a trend toward a greater number in the VR group, this difference failed to reach statistical significance (four trials reported these data, OR: 1.96; 95% CI: 0.87–4.43; P = 0.11).
Meta-analysis of the 13 that reported overall morbidity showed no difference between the two groups (OR: 0.95; 95% CI: 0.74–1.21; P = 0.67) (Fig. 1). Subanalysis showed that the occurrence of pancreatic fistula was significantly lower in the patients with VR resection (OR: 0.53; 95% CI: 0.35–0.79; P = 0.002). In contrast, reoperation (with VR, 9.1%; without VR, 10.0%; P = 0.92), wound infection (with VR, 4.5%; without VR, 8.0%; P = 0.09), bleeding (with VR, 7.1%; without VR, 6.4%; P = 0.42), intestinal occlusion (with VR, 1.0%; without VR, 1.1%; P = 0.94), delayed gastric emptying (with VR, 18.8%; without VR, 16.4%; P = 0.57), intra-abdominal abscess (with VR, 3.4%; without VR, 6.3%; P = 0.13), biliary complications (with VR, 4.6%; without VR, 4.1%; P = 0.59), sepsis (with VR, 9.0%; without VR, 2.8%; P = 0.08), and gastric ulcer (with VR, 2.9%; without VR, 2.2%; P = 0.93) were similar between the two groups.
All 19 studies reported on mortality. There were 22 deaths reported in the patients with VR, and 60 in the group without VR, giving a mean mortality rate of 3.3 and 3.7%, respectively (P = 0.48) (Fig. 2).
Meta-analysis of survival
There was no significant difference in overall survival between the two groups at 1 year (17 trials reported these data, OR: 0.92, 95% CI: 0.66–1.28; P = 0.62), at 3 years (14 trials reported these data, OR: 0.71, 95% CI: 0.47–1.06; P = 0.09), and at 5 years (11 trials reported these data, OR: 0.61, 95% CI: 0.37–1.02; P = 0.06) (Fig. 3).
The estimated 1-, 3-, and 5-year overall survival rates for the patients with VR and without VR were 61.3, 19.4, 12.3 and 61.8, 26.6, 17.0%, respectively.
Publication bias
A funnel plot of the studies used in the meta-analysis reporting on mortality is shown in Figure 4. This is a scatter plot of the treatment effects estimated from individual studies plotted on the horizontal axis (OR) against the standard error of the estimate shown on the vertical axis (SE). Only one study lies outside of the 95% CI limits.
Discussion
The first case of pancreatectomy with VR was reported by Moore et al. [26] in 1951. In 1973, Fortner [27] proposed the concept of “regional pancreatectomy,” which included venous (type I) and arterial (type II) resection, in an effort to improve the resectability rates and curability rates for patients with pancreatic cancer. These regional pancreatectomy procedures were gradually abandoned because the results were poor. In recent years, advances in surgical techniques and postoperative care have improved the safety of pancreatic surgery. However, arterial resection in pancreatectomy remains a challenging procedure with significantly high morbidity and mortality rates [28]. In contrast, VR can be safely performed. As demonstrated in the present study, although duration of operation was longer and operative blood loss was greater in patients undergoing VR than in patients not undergoing VR, mortality and overall morbidity rates were comparable between the two groups. The present results showed acceptable rates of mortality (3.3%) and morbidity (41.9%). It is reasonable to assume that as a surgeon’s experience increases, operative time and blood loss will likely decrease [6]. In the present study, the incidence of pancreatic fistula was significantly lower in the VR group, a difference due mainly to the results reported by Carrère et al. [19] in whose series there were more patients with fibrotic texture of the pancreatic remnant in the VR group. Concerning complications specific to VR, in this review, no study reported any case of bleeding in relation to venous resection. Three studies observed a total of four patients developed mesentericoportal vein thrombosis [9, 19, 25]. In one study, Leach et al. [7] reported that the venous occlusion after VR occurred in 22% (7) of 31 patients: five were asymptomatic and the remaining two died of the condition.
In treatment for pancreatic tumors with SMV-PV involvement, results from two prospective randomized studies showed that the surgery group had significantly better survival than the palliative gastrobiliary bypass group or radiochemotherapy group [29, 30]. Our study demonstrates that this patient subset can benefit from aggressive en bloc VR, with an estimated 5-year survival rate of 12.3%. Therefore, it is clear that acceptable benefits in terms of long-term survival were achieved with this procedure. Furthermore, the overall survival did not differ between operation with VR and without. This is consistent with the hypothesis that tumor with portal vein adherence or invasion may represent a function of tumor location, and possibly tumor size, rather than an indicator of aggressive tumor biology [6]. In addition, tumor extension to the SMV-PV does not necessarily indicate tumor invasion. In the present study, histopathology evaluations revealed that a considerable percentage of patients (43.1%) who underwent VR for pancreatic cancer were found to have inflammatory adhesions without cancer invasion.
There is still no consensus on the specific indications for vascular resection of the SMV-PV. Tumor involvement of the proximal SMA or celiac axis, in contrast to involvement of the SMV-PV, usually includes extensive involvement of the lymphatic tissue as well as the nerve plexus. As a consequence, oncologic curability is limited by retroperitoneal margin positivity. Thus, some authors advocate that venous resection should not be performed when pretreatment imaging demonstrates tumor extension to the SMA or celiac axis [6, 10, 22]. However, recently, a case-matched control study found that pancreatic resections with arterial resection for adenocarcinoma were associated with a 3-year survival rate similar to that of a group of patients not requiring arterial resection [31]. In contrast, the depth of SMV-PV wall invasion is an indicator of poor outcome after curative pancreatic resection combined with VR [10, 32, 33]. However, occasional long-term survival could be observed after curative resection in patients with deep venous wall invasion [33]. In addition, before or during surgery, it is difficult to differentiate malignant from inflammatory adherence of the SMV-PV. Detecting the precise site of tumor infiltration is only possible by histopathological analysis [15].
The present study has several limitations, and therefor conclusions should be drawn with caution. First, to maintain a homogeneous group of patients, three studies were not included in the meta-analysis because data of patients with venous resections were not separable from data of patients with arterial resections [11–13]. This could have caused a selection bias. Second, all of the data in the present study come from nonrandomized studies, and the overall level of clinical evidence is low. Although randomized controlled trials represent the preferred study design for evaluating the safety and efficacy of a surgical procedure, randomized evaluation of VR during pancreatectomy is difficult due to a lack of patient compliance and some ethically unsustainable positions. Third, considering these reports over a 16-year period, it is important to realize that the results were influenced by differences in the treatment protocols, patient selection, and perioperative care. As a consequence, a test for heterogeneity was significant for some of the outcomes analyzed. We applied a random-effect model that takes possible heterogeneity into consideration.
In conclusion, pancreatectomy combined with VR resection for pancreatic cancer is justified because it can result in a positive perioperative outcome and long-term survival comparable to that obtained with standard resection. Owing to the selection bias and the low level of clinical evidence available so far, the results should be interpreted with caution.
References
Harrison LE, Klimstra DS, Brennan MF (1996) Isolated portal vein involvement in pancreatic adenocarcinoma. A contraindication for resection? Ann Surg 224:342–347
Launois B, Franci J, Bardaxoglou E et al (1993) Total pancreatectomy for ductal adenocarcinoma of the pancreas with special reference to resection of the portal vein and multicentric cancer. World J Surg 17:122–126. doi:10.1308/003588409X392045a
Allema JH, Reinders ME, van Gulik TM et al (1994) Portal vein resection in patients undergoing pancreatoduodenectomy for carcinoma of the pancreatic head. Br J Surg 81:1642–1646
Roder JD, Stein HJ, Siewert JR (1996) Carcinoma of the periampullary region: who benefits from portal vein resection? Am J Surg 171:170–174
Takahashi S, Ogata Y, Tsuzuki T (1994) Combined resection of the pancreas and portal vein for pancreatic cancer. Br J Surg 81:1190–1193
Fuhrman GM, Leach SD, Staley CA et al (1996) Rationale for en bloc vein resection in the treatment of pancreatic adenocarcinoma adherent to the superior mesenteric-portal vein confluence. Pancreatic tumor study group. Ann Surg 223:154–162
Leach SD, Lee JE, Charnsangavej C et al (1998) Survival following pancreaticoduodenectomy with resection of the superior mesenteric-portal vein confluence for adenocarcinoma of the pancreatic head. Br J Surg 85:611–617
Launois B, Stasik C, Bardaxoglou E et al (1999) Who benefits from portal vein resection during pancreaticoduodenectomy for pancreatic cancer? World J Surg 23:926–929. doi:10.1007/s002689900601
Bachellier P, Nakano H, Oussoultzoglou PD et al (2001) Is pancreaticoduodenectomy with mesentericoportal venous resection safe and worthwhile? Am J Surg 182:120–129
Shibata C, Kobari M, Tsuchiya T et al (2001) Pancreatectomy combined with superior mesenteric-portal vein resection for adenocarcinoma in pancreas. World J Surg 25:1002–1005. doi:10.1007/s00268-001-0070-z
Aramaki M, Matsumoto T, Etoh T et al (2003) Clinical significance of combined pancreas and portal vein resection in surgery for pancreatic adenocarcinoma. Hepatogastroenterology 50:263–266
Tseng JF, Raut CP, Lee JE et al (2004) Pancreaticoduodenectomy with vascular resection: margin status and survival duration. J Gastrointest Surg 8:935–949
Yekebas EF, Bogoevski D, Cataldegirmen G et al (2008) En bloc vascular resection for locally advanced pancreatic malignancies infiltrating major blood vessels: perioperative outcome and long-term survival in 136 patients. Ann Surg 247:300–309
Hartel M, Niedergethmann M, Farag-Soliman M et al (2002) Benefit of venous resection for ductal adenocarcinoma of the pancreatic head. Eur J Surg 168:707–712
Kawada M, Kondo S, Okushiba S et al (2002) Reevaluation of the indications for radical pancreatectomy to treat pancreatic carcinoma: is portal vein infiltration a contraindication? Surg Today 3:598–601
Howard TJ, Villanustre N, Moore SA et al (2003) Efficacy of venous reconstruction in patients with adenocarcinoma of the pancreatic head. J Gastrointest Surg 7:1089–1095
Nakagohri T, Kinoshita T, Konishi M et al (2003) Survival benefits of portal vein resection for pancreatic cancer. Am J Surg 186:149–153
Poon RT, Fan ST, Lo CM et al (2004) Pancreaticoduodenectomy with en bloc portal vein resection for pancreatic carcinoma with suspected portal vein involvement. World J Surg 28:602–608. doi:10.1007/s00268-004-7250-6
Carrère N, Sauvanet A, Goere D et al (2006) Pancreaticoduodenectomy with mesentericoportal vein resection for adenocarcinoma of the pancreatic head. World J Surg 30:1526–1535. doi:10.1007/s00268-005-0784-4
Riediger H, Makowiec F, Fischer E et al (2006) Postoperative morbidity and long-term survival after pancreaticoduodenectomy with superior mesenterico-portal vein resection. J Gastrointest Surg 10:1106–1115
Shimada K, Sano T, Sakamoto Y et al (2006) Clinical implications of combined portal vein resection as a palliative procedure in patients undergoing pancreaticoduodenectomy for pancreatic head carcinoma. Ann Surg Oncol 13:1569–1578
Al-Haddad M, Martin JK, Nguyen J et al (2007) Vascular resection and reconstruction for pancreatic malignancy: a single center survival study. J Gastrointest Surg 11:1168–1174
Kurosaki I, Hatakeyama K, Minagawa M et al (2008) Portal vein resection in surgery for cancer of biliary tract and pancreas: special reference to the relationship between the surgical outcome and site of primary tumor. J Gastrointest Surg 12:907–918
Chakravarty KD, Hsu JT, Liu KH et al (2010) Prognosis and feasibility of en-bloc vascular resection in stage II pancreatic adenocarcinoma. World J Gastroenterol 16:997–1002
Ouaissi M, Hubert C, Verhelst R et al (2010) Vascular reconstruction during pancreatoduodenectomy for ductal adenocarcinoma of the pancreas improves resectability but does not achieve cure. World J Surg 34:2648–2661. doi:10.1007/s00268-010-0699-6
Moore GE, Sako Y, Thomas LB (1951) Radical pancreaticoduodenectomy with resection and reanastomosis of the superior mesenteric vein. Surgery 30:550–553
Fortner JG (1973) Regional resection of cancer of the pancreas: a new surgical approach. Surgery 73:307–320
Bockhorn M, Burdelski C, Bogoevski D et al (2011) Arterial en bloc resection for pancreatic carcinoma. Br J Surg 98:86–92
Lygidakis NJ, Singh G, Bardaxoglou E et al (2004) Mono-bloc total spleno-pancreaticoduodenectomy for pancreatic head carcinoma with portal-mesenteric venous invasion. A prospective randomized study. Hepatogastroenterology 51:427–433
Doi R, Imamura M, Hosotani R et al (2008) Japan pancreatic cancer study group. Surgery versus radiochemotherapy for resectable locally invasive pancreatic cancer: final results of a randomized multi-institutional trial. Surg Today 38:1021–1028
Bachellier P, Rosso E, Lucescu I et al (2011) Is the need for an arterial resection a contraindication to pancreatic resection for locally advanced pancreatic adenocarcinoma? A case-matched controlled study. J Surg Oncol 103:75–84
Nakao A, Harada A, Nonami T et al (1995) Clinical significance of portal invasion by pancreatic head carcinoma. Surgery 117:50–55
Fukuda S, Oussoultzoglou E, Bachellier P et al (2007) Significance of the depth of portal vein wall invasion after curative resection for pancreatic adenocarcinoma. Arch Surg 142:172–179
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhou, Y., Zhang, Z., Liu, Y. et al. Pancreatectomy Combined with Superior Mesenteric Vein–Portal Vein Resection for Pancreatic Cancer: A Meta-analysis. World J Surg 36, 884–891 (2012). https://doi.org/10.1007/s00268-012-1461-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1461-z