Abstract
Renal cell carcinoma accounts for two to three percent of adult malignancies and can lead to inferior vena cava (IVC) thrombosis. This condition can decrease the rate of 5-year survival for patients to 60%. The treatment of choice in such cases is radical nephrectomy and inferior vena cava thrombectomy. This surgery is one of the most challenging due to many perioperative complications. There are many controversial methods reported in the literature. Achieving the free of tumor IVC wall and the possibility of thrombectomy in cases of level III and level IV IVC thrombosis are two essential matters previously advocated open approaches. Nevertheless, open approaches are being replaced by minimally invasive techniques despite the difficulty of the surgical management of IVC thrombectomy. This paper aims to review recent evidence about new surgical methods and a comparison of open, laparoscopic, and robotic approaches. In this review, we present the latest surgical strategies for IVC thrombectomy and compare open and minimally invasive approaches to achieve the optimal surgical technique. Due to the different anatomy of the left and right kidneys and variable extension of venous thrombosis, we investigate surgical methods for left and right kidney cancer and each level of IVC venous thrombosis separately.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) is the most common type of renal cancer, which accounts for 90% of renal malignancies and 2–3% of adult malignancies [1, 2]. RCC has the ability to invade the inferior vena cava (IVC). IVC invasion of RCC occurs in 4–10% of patients [3]. IVC invasion can lead to IVC thrombosis. This condition can decrease the rate of 5-year survival for patients to 60% [4].
In patients who have had resection surgery of the invaded IVC, the rate of 5-year survival is 31% more than in patients who have not had this surgery [5]. According to this, patients with the discussed condition must undergo surgical interventions, such as partial or radical nephrectomy, IVC thrombectomy, and lymphadenectomy [1]. In cases of localized RCC, radical nephrectomy is the treatment gold standard which is curative [6] According to medical guidelines, open surgery is the standard approach for this operation [7]. Due to successful outcomes of laparoscopic radical nephrectomy (LRN) and IVC thrombectomy, recently, a higher number of LRNs have been performed by surgeons [8].
Open surgery is an invasive surgery that has a mortality of 4–10% [1]. Because of the high mortality rate and surgery-associated complications of open surgery, laparoscopic robot-assisted radical nephrectomy (LRA-RN) and IVC thrombectomy seem to be appropriate alternatives to open surgery. LRA-RN is less invasive than open surgery, and it can help surgeons have better operation management, and patients experience fewer complications. Laparoscopic surgery is as efficient as open surgery but, in comparison with open surgery, has some advantages, such as a shorter duration of hospitalization, a higher rate of accuracy, and a lower rate of blood loss [1]. This review will discuss the necessity of surgical treatment in RCC patients and compare open and robot-assisted laparoscopic radical nephrectomy and IVC thrombectomy.
Renal cancer
2% of all diagnosed cancers are kidney cancer. Recent epidemiological assessments have shown an increased rate of incidence and decreased mortality rate of kidney cancer [9, 10]. About 209,000 new RCC cases are identified annually, accounting for approximately 102,000 deaths worldwide [11, 12]. The median 5-year survival for localized renal cancer is about 95% [13]. RCC is the most common type of renal cancer, accounting for 90% of all renal cancers, with a mean age of diagnosis of 60 years [1, 2, 14]. Clear cell RCC (ccRCC) is the most common type of RCC, which accounts for 70% of RCC cases [15]. Papillary RCC with an incidence of 10–15%, Chromophobe RCC with an incidence of 4%, and collecting duct RCC with an incidence of less than 1% are among the less common types of RCC. About 3–5% of RCCs are unclassified [16,17,18,19]. Five-year survival for sporadic papillary RCC is about 90%. Clear cell RCC tends to metastasize more than papillary RCC; nevertheless, metastatic papillary RCC has a worse prognosis than clear cell RCC [19].
RCC can be either sporadic or hereditary [19]. Aging, obesity, hypertension, diabetes mellitus, cigarette smoking, previous kidney disease, and previous kidney cancer are the most common risk factors for kidney cancer [20,21,22,23,24]. RCCs can be asymptomatic or present with a triad of flank pain, hematuria, and abdominal mass. 20–30% of patients are metastatic at diagnosis [20]. Ultrasound (US) technology helps in the assessment of kidney lesions. Color Doppler US can show the vascular invasion of the tumor, for instance, IVC invasion and IVC thrombosis [21]. However, the Gold standard imaging method for renal cancer is a contrast-enhanced CT scan [13].
Surgery is the curative treatment in isolated RCC without any metastasis in which both partial nephrectomy (PN) and radical nephrectomy (RN) can be used. Also, ablation is an approach used for small renal masses. The choice between these three methods depends on tumor size and stage [7]. In small and isolated renal masses (under 4 cm), PN is more suitable than RN [22]. The laparoscopic approach is preferred over the open surgery approach in PN due to the advantages of laparoscopy and equivalent oncological outcomes of open and laparoscopic techniques [23].
Renal cell carcinoma invasion to inferior vena cava
IVC and renal vein venous tumor thrombosis (VTT) can occur in 10% of patients with RCC. This type of VTT can also extend to the right atrium. This rare condition occurs in 1% of patients [5]. VTT can decrease patients’ 5-year overall survival to 48% in patients with renal vein involvement, 35% in patients with sub-diaphragmatic IVC involvement, and 13% in patients with supra-diaphragmatic IVC involvement. IVC thrombosis occurs more commonly on the right side [24].
VTT occurs in non-metastatic and metastatic RCCs [25]. Renal vein and IVC VTT can lead to lower-limb edema, varicocele, and peripheral lymphadenopathy [20]. Color Doppler US, contrast-enhanced CT scan, and MRI are appropriate imaging studies in cases of VTT [26]. The interval between imaging and surgery should not be longer than 30 days [27]. IVC VTT in RCC is classified by the level of thrombosis extension in IVC into five levels, illustrated, and summarized in Fig. 1 and Table 1, respectively [28].
Renal vein involvement with/without IVC involvement
Isolated renal vein wall involvement is more commonly observed. But after renal vein wall involvement, tumor cells can invade the IVC. Observing thrombosis in the lumen of IVC does not necessarily mean IVC wall involvement since the tumor can be floating in the vein. In the case of floating tumor thrombosis, the IVC wall does not have malignant cell infiltration. Isolated renal vein wall involvement is seen in this condition. In cases of malignant cell infiltration into the IVC wall, the tumor thrombus is not floating and adheres to the IVC wall (Table 1) [4]. Due to the poor prognosis in patients without resection of invaded vein wall by tumor (5-year survival of 26%), resection of the invaded wall is indicated in cases with RCC and IVC VTT [29].
Nephrectomy and IVC thrombectomy
Pre-operative and post-operative care
Anticoagulation therapy has no significant advantages and does not significantly reduce perioperative VTT risk [30]. IVC filter should be used in patients with pulmonary embolism who are not responsive to anticoagulation therapy or in case of any contraindications for anticoagulation therapy [37]. However, pre-operative IVC filter placement probably leads to tumor disruption on placement or tumor growth onto the filter. Therefore, pre-operative IVC filter placement should not be performed in all patients [37]. Also, patients with extended VTTs close to the right atrium benefit from IVC filter placement during operation due to a high risk of pulmonary embolism [26, 31]. Anesthesia consultations are recommended for high-risk patients. Cardiology consultations are recommended in patients with a risk of coronary artery disease or patients with prior cardiologic disorders. Forty-eight hours after surgery, anticoagulation therapy should be started for a duration of 6 months in patients with complete resection of the tumor. Chest X-ray, CT scan, and lower-limb color Doppler US are useful for post-operative assessment [13, 32].
The aim of RN and IVC thrombectomy is complete resection of the vein wall invaded by the tumor and having a free-of-tumor margin in IVC. Choosing an appropriate surgery method depends on the tumor side, left-sided or right-sided, tumor level, and the tumor’s extent of vein wall involvement [29]. Pre-operative MRI can determine the need for cavotomy by measuring the anterior–posterior diameter of IVC and renal vein entrance involvement [33, 34]. Pre-operative CT angiography and three-dimensional CT are non-invasive methods that help surgeons choose the optimum surgical method depending on kidney anatomy and renal mass situation [35]. Intraoperative IVC lumen exploration for assessment of the need for IVC resection is of great importance. In cases of IVC wall involvement, resection to attain to negative margin is necessary, but in floating thrombosis without IVC wall involvement, IVC wall resection is not required [33, 36].
PRAE (pre-operative renal artery embolization) is still a controversial issue. For open approach surgery, PRAE is recommended only in patients with advanced RCCs; though in other patients, PRAE increases blood loss and operation time [28]. In minimally invasive approaches such as robot-assisted approaches, PRAE has benefits such as decompression of collateral veins, decreased blood loss, and reduced intraoperative oozing [37]. For left-sided RCCs with IVC VTT, renal artery embolization is mandatory due to the difficulty of renal artery access in the left decubitus position [28].
The IVC incision type depends on the tumor extension of the IVC incision, which relies on the extension of the tumor to the contralateral renal vein entrance to IVC. In cases without opposite side renal vein entrance involvement by VTT, incision of IVC should be oblique for saving opposite side renal vein flow to IVC; however, in cases with contralateral renal vein entrance involvement by IVC VTT, opposite side renal vein should be separately incised to help the preservation of healthy kidney’s blood flow [29].
According to the less favorable collateral circulation of the right kidney in comparison with the left kidney, in the cases of left-sided RCC with IVC VTT, the right renal artery should be blocked to prevent congestion of the healthy kidney subsequent to renal vein blockage except in patients with right renal vein excluded by IVC rerouting. However, in the right-sided RCC with IVC VTT, blocking the left renal artery is not mandatory [33, 38]. To reduce the operation time in left-sided RCCs, partial blocking of IVC after thrombectomy provides unblocking of the right renal artery and vein before closure. For this approach, using a balloon catheter before thrombectomy is beneficial [38]. For right-sided tumors, the left renal vein can be blocked safely without requiring left renal artery blockage [5].
The possibility of primary closure of IVC depends on the percentage of IVC circumference resection; in cases with resection of less than 50% of IVC circumference, primary closure or venous patches can be used. In cases of supra-renal IVC resection, IVC reconstruction by grafts, such as bovine pericardium, and prosthesis is necessary except in patients with appropriate collateral abdominopelvic circulation [33, 39]. There is no significant difference between transected and en bloc techniques in matters of surgical complications; though, in laparoscopic or robotic approaches, transected methods have advantages such as better IVC mobilization and decreased risk of embolization in left-sided tumors due to PRAE [28]. Due to the large lumen of IVC and the numerous veins that join it, dissection of IVC without blood flow control can lead to severe bleeding and an increased risk of tumor embolization during the operation. Several techniques exist for tumor embolization and massive bleeding prevention. Using these techniques depends on tumor levels. In patients with isolated renal artery VTT, partial clamping of IVC should be used. In level 2 VTTs, complete IVC clamping is preferred [40]. Unlike the relatively safe infra-hepatic IVC clamping, supra-hepatic IVC clamping can lead to troublous hypotension and decrease venous return [48].
Regarding the cases in which infra-hepatic IVC clamping is not suitable due to supra-hepatic expansion of tumor, several methods have been discussed in the literature, such as cross-clamping of hepatic hilar or cardiopulmonary bypass [40]. Caval–atrial shunt during the operation and occlusion of intra-pericardial vena cava are alternative options. But in comparison with other techniques, cardiopulmonary bypass with deep hypothermic circulatory arrest (DHCA) is more favorable since this technique offers some advantages [41]. Performing IVC thrombectomy without cardiopulmonary bypass needs several lumbar veins and porta hepatis ligation for bleeding prevention. IVC dissection is possible using a Cardiopulmonary bypass with DHCA. It also assists with performing a complete exploration of the IVC lumen without significant bleeding risk and with decreased risk of tumor embolization [41].
Intraoperative transesophageal echocardiography (TEE) is helpful for cardiac assessment and tumor movement control. It can help surgeons perform appropriate action at a punctual time for tumor embolism prevention [49]. This approach is used frequently in level 3 and 4 patients [33]. Intraoperative ultrasonography can confirm the level of VTT extension, which is beneficial for choosing the appropriate surgical method [33]. Attainment of negative vein wall margin is vital due to its effect on local recurrence rate, even in non-metastatic patients. A positive microscopic margin can decrease the free-of-tumor interval about 48 months in non-metastatic patients with RCC and VTT [4].
Surgical management with an open approach based on tumor classification
Level 1
In level 1 IVC VTTs, a flank incision can be used due to the lower necessity of broad IVC access [27]. Subcostal and midline incisions are also suitable due to the lower probability of using a bypass. Similar to other levels, early ligation of the renal artery is a priority to prevent massive intraoperative blood loss [5, 27, 33]. The surgical method used in level 1 tumors depends on the possibility of the IVC thrombosis being pulled back into the renal vein, determined by thrombus size and shape [33, 42]. If VTT is small and milkable, a Satinsky vascular clamp can be placed on the IVC wall around the renal ostium. However, in cases of large VTTs where milking the thrombus is impossible due to the risk of thrombus disintegration, IVC control should be performed in the proximal and distal end of VTT in addition to contralateral renal vein control [33]. Thereafter, the ostium must be opened and incised to provide kidney and renal vein removal [5].
Cavotomy and large IVC wall incision are not necessary. Therefore, caval defects can be sutured by running 3–0 or 4–0 Polypropylene [27, 43]. The robot-assisted approach should be performed in a 60° left lateral decubitus position (right-sided RCC) or supine steep Trendelenburg position (left-side RCC). The laparoscopic and robot-assisted approach’s surgical steps are similar to the open approach [44].
Level 2
Level 2 patients do not need bypasses; therefore, surgery can be performed via anterior subcostal or midline incision [42]. These patients need a more exhaustive IVC wall dissection due to the need for IVC and contralateral renal vein mobilization [45]. According to the higher demand for IVC wall dissection in these patients, ligation of lumbar branches, as much as possible, in addition to renal artery ligation, is necessary for better IVC control [27]. If more infra-hepatic IVC exposure is needed, ligating minor hepatic veins is beneficial [46].
After performing the mentioned steps, infra-renal IVC, contralateral renal vein, and supra-renal IVC clamping must be performed [46]. IVC occlusion using a balloon is an alternative option in patients at risk of intraoperative bleeding due to the difficulty of distal IVC control [47]. After attaining well-controlled blood flow of IVC by clamping, cavotomy by an anterior incision should be done, starting from the ostium of the renal vein and ascending along the IVC [48]. The following steps depend on the existence of a floating thrombus or a thrombus with IVC wall involvement. In case of the absence of IVC wall involvement, thrombectomy is the plan of choice. After thrombectomy, the IVC wall can be assessed to find involvement by direct vision or with venacavoscopy using a cystoscope. Due to the importance of gaining a negative margin, questionable regions can be biopsied or resected [4, 49]. In direct IVC wall involvement by a thrombus, a Penfield dissector can salvage the IVC wall [27]. After thrombectomy, the IVC lumen should be cleared by flushing heparinized saline, and the IVC defect is closed by running a Prolene 4–0 suture [42]. During the tightening of the last suture, distal IVC clamping is released, and residual clots and air are pulled out [5].
Level 3
Since more exposure is needed in level 3 patients, an anterior midline incision is made [50]. Due to the need for bypass in level 3 cases, midline abdominal median sternotomy is also an appropriate incision for some cases, such as cases with large tumors in the upper kidney pole, patients in need of retro-hepatic IVC exposure, and cases with challenging anatomical situations. Also, bilateral subcostal incision has advantages in comparison with sternotomy, such as preventing post-operative thoracic complications such as atelectasis [27, 51].
These patients generally need a bypass, and after arterial ligation, the need for a bypass should be reassessed by surgeons. The need for vascular bypass depends on the extent of IVC lumen occlusion by tumor thrombosis. Due to the inappropriate development of collateral veins, patients with partial occlusion of IVC by VTT have less tolerance for supra-hepatic IVC cross-clamping, and bypass is advantageous. According to the mentioned facts, in patients with complete occlusion of IVC by VTT, cross-clamping can safely be used to facilitate VTT resection. An increased risk of bleeding from collaterals is possible and should be considered in cross-clamping. Veno-venous bypass (VVBP) and cardiopulmonary bypass (CPB) are two options for patients who require bypass. VVBP is performed by placing a 20F venous cannula below the VTT into the IVC and an 8–14F cannula into the right atrium or brachial vein and then connecting the tubing to an electromagnetic centrifugal pump [5, 33]. Placing the cannula into the IVC lumen occluded with VTT should be avoided because it can lead to thrombosis movement to the right atrium [5]. A cardiopulmonary bypass is an alternative option for patients requiring bypass. Compared with VVBP, CPB can maintain cardiac output, but it can increase the risk of cerebrovascular emboli, renal dysfunction, and organ failure [27]. CPB, in combination with DHCA, can be an appropriate option for patients with level 3 and 4 IVC VTT due to its ability to decrease perioperative mortality [52, 53].
After attaining appropriate vascular control, cavotomy should be initiated as described in level 2. VTT should be pulled down between infra-renal, supra-renal, and contralateral renal vein controls, if possible. TEE should be performed to help surgeons determine the appropriate site of clamping located above the VTT [50]. Gaining appropriate IVC exposure is one of the most critical issues in level 3 patients. In cases of small level 3 VTTs, short hepatic veins ligation and intra-hepatic IVC release can provide enough exposure. But in larger VTTs, mobilization of the caudal lobe of the liver may be necessary [50].
Despite all these measures, if IVC clamping above the VTT is impossible, complete liver mobilization via incising falciform, round, and coronal hepatic ligament should be performed to access IVC above the supra-hepatic veins. In clamping IVC above the hepatic veins, the Pringle maneuver should be performed to prevent hepatic congestion [54]. The Pringle maneuver is occluding the hepatic artery provisionally by clamping the hepatic pedicle [54]. IVC clamping should be performed via anterior approach in small VTTs, and it is better to be done via lateral approach in cases of larger tumors. If cavoatrial junction control is necessary, a thoracoabdominal incision is recommended [33]. Cavotomy should be performed as described in level 2 tumors. After cavotomy in cases of incomplete resection of the vena cava, reconstruction of the vena cava by grafts can be achieved [56].
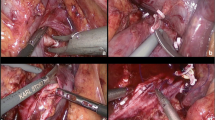
The most challenging part of minimally invasive approaches in level 3 patients is supra-hepatic IVC control. The role of hepatic mobilization in robot-assisted surgery has been described in recent studies. In right-sided IVC VTT, the patient should be secured at the left semi-lateral position then the bed should be rotated away from the operative side. It can also be performed in the dorsal elevated lithotomy position. After releasing the liver from its connections (ligaments), medial rotation of the liver is possible. The right and left lobes of the liver can be mobilized off the IVC [55,56,57,58]. Balloon catheters provide thrombectomy without liver mobilization. A cystoscope can visualize the IVC lumen and assess IVC wall invasion via robotic approach [57].
Level 4
The surgical approach should be chosen after intraoperative TEE [27]. If TEE shows nonadherent (floating) VTT, surgery is performable via thoracoabdominal or midline approach. Thrombus can be pulled down below the diaphragm, and the cavoatrial junction can be controlled by the Rummel tourniquet. In adherent VTT, CPB with DHCA and sternotomy is advantageous [53, 59]. In the case of VTT extension to the right atrium, PRAE and caval filter may be required [26]. The robot-assisted approach can be performed with thoracoscopy assistance under CBP in level 4 patients. Cavectomy and thrombectomy can be done via a robot-assisted approach [56]. Current surgical methods for each level of IVC VTT are summarized in Fig. 2.
Comparison of open and minimally invasive approaches for RN and IVC thrombectomy
RN and IVC thrombectomy is one of the most challenging urological surgeries that leads to major surgical complications and has a high rate of intraoperative mortality and post-operative morbidity based on incision size, need for CPB, DHCA, and IVC cross-clamping [1, 55]. The open approach is still the standard for RN and IVC thrombectomy. Although, minimally invasive approaches (laparoscopic and robot-assisted surgery) seem to be quickly replacing open approaches due to their advantages [28].
Robot-assisted laparoscopic RN and IVC thrombectomy can provide three-dimensional visualization, reduction of blood loss, early post-operative rehabilitation, and reduction of hospital stay time [1]. Patients who have undergone surgery via laparoscopic approaches experience fewer post-operative complications, decreased operation time, and increased time of cancer-specific survival [60]. But it should be considered that robot-assisted RN and IVC thrombectomy has significantly more operation time in comparison with open surgery [8]. Thekke et al. reported a mean robot-assisted operation time of about 329 min among 13 patients with level 1–3 IVC VTT [44]. However, Shao et al. revealed that the laparoscopic approach’s mean operation time for level 2 and 4 patients is about 210 min. They also separately reported 155 min for level 2 and 275 min for level 4 [61]. Also, the mean operation time in open approach surgery was about 249 min [62]. Reducing IVC clamping time is necessary according to its complications. The mean IVC clamping time in minimally invasive approaches is about 19–20 min [44, 61]. The median blood loss in the open approach is about 1900–3000 mL; however, the robot-assisted approach estimated about 395–500 mL [44, 61, 62]. 5 out of 11 patients in the Shao et al. study population and 4 out of 13 in another study required intraoperative or post-operative blood transfusion [44, 61]. Lue et al. reported that the median length of the hospital stay in patients who underwent open surgery is about 7 days. On the other hand, the mean duration of hospital stay was reported as 7.8–9 days in minimally invasive approaches [44, 61, 62]. One study reported that 28% of non-metastatic patients who underwent open surgery developed metastasis after about 22 months of follow-up. Another study showed that after about 19 months of follow-up, 10 out of 13 patients who underwent robot-assisted surgery were disease free [44, 63]. Lue et al. showed that 50% of open surgery patients had post-operative complications [62]. Also, they reported that 12.6% of the patients died after surgery. Approximately 35% of PCNL patients experienced post-operative complications which require pharmacological treatments, such as tachyarrhythmias, pneumonia, and transient ischemic attack. In addition, about 20% of the patients had complications requiring surgical or radiological treatments. On the other hand, Wang et al. reported a mortality rate of only 7.7% among level 3 and 4 patients who underwent robot-assisted surgery. Also, 5 out of 101 patients had post-operative renal, and 3 had liver dysfunction, which improved with medical interventions [56]. However, Shao et al. reported no post-operative complications after laparoscopic surgery. Also, they mentioned that all patients had normal post-operative kidney and liver function, and among patients who underwent CBP, no patients had post-operative cardiopulmonary or cerebral complications [61]. According to the large incision needed in the open approach, wound healing time is longer, and the incidence of associated complications such as wound infection is higher in the open approach [44]. Among 13 RCC patients with IVC VTT in Thekke et al. study population, they achieved negative surgical margins in the robot-assisted approach in all patients. Also, they reported 100% overall survival after a median 19-month follow-up [44]. Minimally invasive approaches may have advantages superior to the open approach. Still, it is notable that studies that show lower blood loss and post-operative complications in minimally invasive procedures have been conducted on selected and smaller populations compared with studies in an open approach. Furthermore, minimally invasive approaches are routinely performed on patients with lower levels of IVC VTT. The ability to use laparoscopic and robot-assisted approaches depends on tumor size and level, collateral vessels, and surgeon’s experience [33]. On the other hand, the open approach provides more exposure and safer IVC control [28]. In cases of RCC and IVC VTTs which open approaches provide more advantages than minimally invasive approaches, they should not be performed at any cost. Also, minimally invasive approaches need a multidisciplinary and experienced team [34].
In patients with level 1, level 2, and level 3a IVC VTTs, RN and IVC thrombectomy can be performed safely via minimally invasive approaches; however, the laparoscopic approach and robot-assisted approaches both were reported for each level of IVC VTT [64]. Nevertheless, the laparoscopic approach has advantages compared to the robot-assisted approach due to being closer to the patient in case of the surgery approach’s conversion to open approach and the benefits of choosing the site [28, 60]. Minimally invasive approaches may require conversion to open approach due to unpredictable issues such as thrombosis, inflammation, and adenopathy [65]. Specific patients can benefit from the safety of the open approach and the advantages of minimally invasive approaches simultaneously via open IVC thrombectomy after laparoscopic thrombectomy [66]. The robot-assisted approach can also be advantageous to patients with level 2 IVC VTT [67]. Recent studies have also shown the safety and advantages of robot-assisted RN and IVC thrombectomy for level 3 and 4 patients [56]. Minimally invasive approaches can be different depending on the tumor side. According to the left renal vein’s greater length than the right renal vein, surgery in a left-sided tumor should be performed via a combined retroperitoneal and transperitoneal approach [60].
Complications and challenges
Depending on tumor shape and thrombosis classification, surgical methods differ based on patient characteristics [29]. The surgical technique depends on the tumor’s laterality due to the different anatomy of collateral circulation of the right and left kidneys. The left kidney has a better collateral circulation than the right kidney, making left-sided tumor surgery more complex than right-sided tumors. Therefore, patients with left-sided tumors are more exposed to renal dysfunction and ischemia as a complication of surgery [38]. Myocardial injury is seen in 37.8% of patients, and acute kidney injury is seen in 42.7% of patients undergoing radical nephrectomy and IVC thrombectomy [40]. Microscopic positive margin after extended follow-up after surgery occurs in 18.4% of patients and can reduce the patient’s disease-free interval [4]. Depending on the tumor’s expansion in IVC, appropriate access to IVC can be one of the most challenging parts of this surgery. In cases with IVC VTT expansion to retro-hepatic IVC, having suitable access is one of the most challenging parts of this surgery [26]. IVC VTT expansion to the right atrium forces surgeons to use the cardiopulmonary bypass. It can lead to several complications [40]. Intraoperative pulmonary embolization of IVC VTT is one of the most challenging complications that leads to several morbidities [28]. Therefore, due to anatomical variations, perioperative comorbidities, and the majority of this surgery, radical nephrectomy and IVC thrombectomy is one of the most challenging surgeries.
In patients with several comorbidities, surgical treatment is challenging. Neoadjuvant immunochemotherapy can be an alternative choice for immediate surgery. A case report showed the complete response of level 4 IVC VTT to nivolumab and ipilimumab. This neoadjuvant treatment made it possible to completely resect the kidney tumor with negative margins [68]. In addition, one of the rare presentations of RCC with VTT is Budd–Chiari syndrome. Due to the presence of coagulopathy and severe hepatic dysfunction, surgery is not recommended except in cases diagnosed in the early stages [33].
Conclusions
IVC wall involvement in renal cell carcinoma can decrease the 5-year survival rate and increase the recurrence rate. Due to this patient’s high amount of perioperative complications, choosing an effective surgical method is crucial. To choose the best surgical methods for patients with RCC and IVC VTT, thrombus level, extension to contralateral renal vein, thrombus adherence to IVC wall, and laterality of RCC should be assessed. In level 1 and 2 patients, CBP should be avoided as much as possible due to the associated complications. In level 3 and 4 patients, IVC access is the most challenging part of the surgery, which can be achieved by short hepatic vein ligation and hepatic mobilization in cases of high-extent VTT. Minimally invasive approaches have been recently reported in the literature for each level of VTT. But choosing between open and minimally invasive approaches should be performed via accurate decision. In conclusion, RN and IVC thrombectomy has been described in this review level by level and approach by approach. According to the difficulty and complexity of the surgeries and the variation of techniques in patients with higher-level IVC VTTs, bigger studies should be performed to compare the effectiveness and safety of different techniques, especially in minimally invasive approaches.
Data availability
Data availability is not applicable in our manuscript.
References
Ma S, Jia W, Hou G, Quan P, Zhang L, Fan X, et al. Case reports of robot-assisted laparoscopic radical nephrectomy and inferior vena cava tumor thrombectomy. Medicine. 2021;100:e26886.
Velasquez MC, Mouzannar ALI, Swain S, Ciancio G. Rarely described renal malignancies associated with venous tumor thrombus. Anticancer Res. 2022;42:1351–8.
Marshall FF, Dietrick DD, Baumgartner WA, Reitz BA. Surgical management of renal cell carcinoma with intracaval neoplastic extension above the hepatic veins. J Urol. 1988;139:1166–71.
Abel EJ, Carrasco A, Karam J, Tamboli P, Delacroix S, Vaporciyan AA, et al. Positive vascular wall margins have minimal impact on cancer outcomes in patients with non-metastatic renal cell carcinoma (RCC) with tumour thrombus. BJU Int. 2014;114:667–73.
Blute ML, Leibovich BC, Lohse CM, Cheville JC, Zincke H. The Mayo Clinic experience with surgical management, complications and outcome for patients with renal cell carcinoma and venous tumour thrombus. BJU Int. 2004;94:33–41.
Novick AC. Laparoscopic and partial nephrectomy. Clin Cancer Res. 2004;10:6322S-6327S.
Ljungberg B, Albiges L, Abu-Ghanem Y, Bensalah K, Dabestani S, Fernández-Pello S, et al. European Association of urology guidelines on renal cell carcinoma: the 2019 update. Eur Urol. 2019;75:799–810.
Vuong N-S, Ferriere J-M, Michiels C, Calen L, Tesi L, Capon G, et al. Robot-assisted versus open surgery for radical nephrectomy with level 1–2 vena cava tumor thrombectomy: a French monocenter experience (UroCCR study #73). Minerva Urol Nephrol. 2021. https://doi.org/10.23736/S2724-6051.20.04052-7.
Hsieh JJ, Purdue MP, Signoretti S, Swanton C, Albiges L, Schmidinger M, et al. Renal cell carcinoma. Nat Rev Dis Primers. 2017;3:17009.
Hollingsworth JM, Miller DC, Daignault S, Hollenbeck BK. Rising incidence of small renal masses: a need to reassess treatment effect. JNCI J Natl Cancer Inst. 2006;98:1331–4.
Gupta K, Miller JD, Li JZ, Russell MW, Charbonneau C. Epidemiologic and socioeconomic burden of metastatic renal cell carcinoma (mRCC): a literature review. Cancer Treat Rev. 2008;34:193–205.
Rini BI, Campbell SC, Escudier B. Renal cell carcinoma. The Lancet. 2009;373:1119–32.
Bigot P, Barthelemy P, Boissier R, Khene Z-E, Pettenati C, Bernhard J-C, et al. French AFU Cancer Committee Guidelines—update 2022–2024: management of kidney cancer. Prog Urol. 2022;32:1195–274.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Jonasch E, Walker CL, Rathmell WK. Clear cell renal cell carcinoma ontogeny and mechanisms of lethality. Nat Rev Nephrol. 2021;17:245–61.
Mendhiratta N, Muraki P, Sisk AE, Shuch B. Papillary renal cell carcinoma: review. Urol Oncol Semin Orig Investig. 2021;39:327–37.
Garje R, Elhag D, Yasin HA, Acharya L, Vaena D, Dahmoush L. Comprehensive review of chromophobe renal cell carcinoma. Crit Rev Oncol Hematol. 2021;160: 103287.
Vanderbruggen W, Claessens M , De Coninck V, Duchateau A , Gevaert T , Joniau S , et al. Collecting duct renal cell carcinoma: a single centre series and review of the literature. Cent Eur J Urol. 2022;75(3):252–56. https://doi.org/10.5173/ceju.2022.0143.
Cohen HT, McGovern FJ. Renal-cell carcinoma. N Engl J Med. 2005;353:2477–90.
Bahadoram S, Davoodi M, Hassanzadeh S, Bahadoram M, Barahman M, Mafakher L. Renal cell carcinoma: an overview of the epidemiology, diagnosis, and treatment. Giornale Italiano di Nefrologia. 2022;39(3):2022-vol3.
Novacescu D, Feciche BO, Cumpanas AA, Bardan R, Rusmir AV, Bitar YA, et al. Contemporary clinical definitions, differential diagnosis, and novel predictive tools for renal cell carcinoma. Biomedicines. 2022;10:2926.
Alam R, Patel HD, Osumah T, Srivastava A, Gorin MA, Johnson MH, et al. Comparative effectiveness of management options for patients with small renal masses: a prospective cohort study. BJU Int. 2019;123:42–50.
Gill IS, Kavoussi LR, Lane BR, Blute ML, Babineau D, Colombo JR, et al. Comparison of 1,800 laparoscopic and open partial nephrectomies for single renal tumors. J Urol. 2007;178:41–6.
Sidana A, Goyal J, Aggarwal P, Verma P, Rodriguez R. Determinants of outcomes after resection of renal cell carcinoma with venous involvement. Int Urol Nephrol. 2012;44:1671–9.
Bhindi B, Abel EJ, Albiges L, Bensalah K, Boorjian SA, Daneshmand S, et al. Systematic review of the role of cytoreductive nephrectomy in the targeted therapy era and beyond: an individualized approach to metastatic renal cell carcinoma. Eur Urol. 2019;75:111–28.
Fontana F, Deho F, Piacentino F, Curti M, Capogrosso P, Coppola A, et al. Management of renal cell carcinoma with extensive caval thrombosis utilizing a temporary atrial caval filter through a combined endovascular and open surgical technique. Vasc Endovascular Surg. 2021;55:505–9.
Lawindy SM, Kurian T, Kim T, Mangar D, Armstrong PA, Alsina AE, et al. Important surgical considerations in the management of renal cell carcinoma (RCC) with inferior vena cava (IVC) tumour thrombus. BJU Int. 2012;110:926–39.
Jurado A, Romeo A, Gueglio G, Marchiñena PG. Current trends in management of renal cell carcinoma with venous thrombus extension. Curr Urol Rep. 2021;22:23.
Liu Z, Zhang Q, Zhao X, Zhu G, Tang S, Hong P, et al. Inferior vena cava interruption in renal cell carcinoma with tumor thrombus: surgical strategy and perioperative results. BMC Surg. 2021;21:402.
Kaptein FHJ, van der Hulle T, Braken SJE, van Gennep EJ, Buijs JT, Burgmans MC, et al. Prevalence, treatment, and prognosis of tumor thrombi in renal cell carcinoma. JACC CardioOncol. 2022;4:522–31.
Duda A, Hanak C, Wirtz P, Lipscomb A, Mitiek M. Single-stage resection with intraoperative filter placement for right renal carcinoma with vena cava extension. J Vasc Surg Cases Innov Tech. 2021;7:691–3.
Woodruff DY, van Veldhuizen P, Muehlebach G, Johnson P, Williamson T, Holzbeierlein JM. The perioperative management of an inferior vena caval tumor thrombus in patients with renal cell carcinoma. Urol Oncol Semin Orig Investig. 2013;31:517–21.
Ghoreifi A, Djaladat H. Surgical tips for inferior vena cava thrombectomy. Curr Urol Rep. 2020;21:51.
Adams LC, Ralla B, Bender Y-NY, Bressem K, Hamm B, Busch J, et al. Renal cell carcinoma with venous extension: prediction of inferior vena cava wall invasion by MRI. Cancer Imaging. 2018;18:17.
Toprak U, Erdoğan A, Gülbay M, Karademir MA, Paşaoğlu E, Akar OE. Pre-operative evaluation of renal anatomy and renal masses with helical CT, 3D-CT and 3D-CT angiography. Diagn Interv Radiol. 2005;11:35–40.
Ciancio G. Inferior vena cava reconstruction using a ringed polytetrafluoroethylene interposition graft and inferior vena cava filter placement following resection of renal cell carcinoma with a tumor thrombus directly infiltrating the inferior vena cava. Vasc Endovasc Surg. 2022;56:5–10.
Salsano G, Palermo B, Barattini M, Puccianti F, Gentilli S, Romano N, et al. Pre-operative renal artery embolization in laparoscopic radical and partial nephrectomy: a multidisciplinary approach to renal tumors. Surg Technol Int. 2020;36:23–8.
Zhuo L, Guodong Z, Xun Z, Shiying T, Peng H, Li Z, et al. A modified surgical technique of shortening renal ischemia time in left renal cancer patients with Mayo level II-IV tumor thrombus. BMC Surg. 2020;20:120.
Morris PD, Furtado R, Pulitano C, Crawford M, Yeo D, Vasilaras A, et al. Inferior vena cava resection and reconstruction with bovine pericardium for renal cell carcinoma: complications and outcomes. Urology. 2019;134:143–7.
Hua Y-B, Li X, Wang D-X. Prevalence and risk factors of myocardial and acute kidney injury following radical nephrectomy with vena cava thrombectomy: a retrospective cohort study. BMC Anesthesiol. 2021;21:243.
Novick AC, Kaye MC, Cosgrove DM, Angermeier K, Pontes JE, Montie JE, et al. Experience with cardiopulmonary bypass and deep hypothermic circulatory arrest in the management of retroperitoneal tumors with large vena caval thrombi. Ann Surg. 1990;212:472–7.
Kalapara AA, Frydenberg M. The role of open radical nephrectomy in contemporary management of renal cell carcinoma. Transl Androl Urol. 2020;9:3123–39.
Joseph S, Stuart H, Glenn P, Roger D. Surgical approaches for open renal surgery, including open radical nephrectomy. Hinman’s Atlas of urologic surgery. 4th ed. Philadelphia: Elsevier; 2019. p. 61–75.
Kishore TA, Pathrose G, Raveendran V, Ganpule A, Gautam G, Laddha A, et al. Robot-assisted laparoscopic radical nephrectomy and inferior vena cava thrombectomy: a multicentre Indian experience. Arab J Urol. 2020;18:124–8.
Pulford C, Keating K, Rohloff M, Peifer D, Eames R, Shakuri-Rad J, et al. Robotic-assisted nephrectomy with level II IVC thrombectomy using Rummel Tourniquets. Int Braz J Urol. 2022;48:196–7.
Chopra S, Simone G, Metcalfe C, de Castro Abreu AL, Nabhani J, Ferriero M, et al. Robot-assisted level II–III inferior vena cava tumor thrombectomy: step-by-step technique and 1-year outcomes. Eur Urol. 2017;72:267–74.
Metcalfe C, Chang-Kit L, Dumitru I, MacDonald S, Black P. Antegrade balloon occlusion of inferior vena cava during thrombectomy for renal cell carcinoma. Can Urol Assoc J. 2013;4:105.
Crisan N, Andras I, Grad D-L, Telecan T, Coman R-T, de Cobelli O, et al. Dual combined laparoscopic approach for renal-cell carcinoma with renal vein and level I–II inferior vena cava thrombus: our technique and initial results. J Endourol. 2018;32:837–42.
Swierzewski DJ, Swierzewski MJ, Libertino JA. Radical nephrectomy in patients with renal cell carcinoma with venous, vena caval, and atrial extension. Am J Surg. 1994;168:205–9.
Ciancio G, Shirodkar SP, Soloway MS, Salerno TA. Techniques for avoidance of sternotomy and cardiopulmonary bypass during resection of extensive renal cell carcinoma with vena caval tumor thrombus extension above the diaphragm. J Card Surg. 2009;24:657–60.
Bokka S, Manikandan R, Dorairajan LN, Srivathsa K, Sreenivasan Sreerag K, Kalra S, et al. Perioperative and oncological outcomes of renal cell carcinoma with venous tumour thrombus. Urol J. 2022;89:31–7.
Shuch B, Crispen PL, Leibovich BC, LaRochelle JC, Pouliot F, Pantuck AJ, et al. Cardiopulmonary bypass and renal cell carcinoma with level IV tumour thrombus: can deep hypothermic circulatory arrest limit perioperative mortality? BJU Int. 2011;107:724–8.
Marshall FF, Reitz BA, Diamond DA. A new technique for management of renal cell carcinoma involving the right atrium: hypothermia and cardiac arrest. J Urol. 1984;131:103–7.
Pouliot F, Shuch B, LaRochelle JC, Pantuck A, Belldegrun AS. Contemporary management of renal tumors with venous tumor thrombus. J Urol. 2010;184:833–41.
Sood A, Jeong W, Barod R, Bahnson E, Kirura P, Abdollah F, et al. Robot-assisted hepatic mobilization and control of suprahepatic infradiaphragmatic inferior vena cava for level 3 vena caval thrombectomy: an IDEAL stage 0 study. J Surg Oncol. 2015;112:741–5.
Wang B, Huang Q, Liu K, Fan Y, Peng C, Gu L, et al. Robot-assisted level III–IV inferior vena cava thrombectomy: initial series with step-by-step procedures and 1-year outcomes. Eur Urol. 2020;78:77–86.
Kundavaram C, de Castro Abreu AL, Chopra S, Simone G, Sotelo R, Aron M, et al. Advances in robotic vena cava tumor thrombectomy: intracaval balloon occlusion, patch grafting, and vena cavoscopy. Eur Urol. 2016;70:884–90.
Ciancio G, Hawke C, Soloway M. The use of liver transplant techniques to aid in the surgical management of urological tumors. J Urol. 2000. https://doi.org/10.1097/00005392-200009010-00012.
Serag H, Featherstone JM, Griffiths DF, Mehta D, Dunne J, Hughes O, et al. Radical nephrectomy and intracaval thrombectomy for advanced renal cancer with extensive inferior vena cava involvement utilising cardiopulmonary bypass and hypothermic circulatory arrest: is it worthwhile? Arab J Urol. 2018;16:378–85.
Liu Z, Zhao X, Ge L, Wu B, Tang S, Hong P, et al. Completely laparoscopic versus open radical nephrectomy and infrahepatic tumor thrombectomy: comparison of surgical complexity and prognosis. Asian J Surg. 2021;44:641–8.
Shao P, Li J, Qin C, Lv Q, Ju X, Li P, et al. Laparoscopic radical nephrectomy and inferior vena cava thrombectomy in the treatment of renal cell carcinoma. Eur Urol. 2015;68:115–22.
Lue K, Russell CM, Fisher J, Kurian T, Agarwal G, Luchey A, et al. Predictors of post-operative complications in patients who undergo radical nephrectomy and IVC thrombectomy: a large contemporary tertiary center analysis. Clin Genitourin Cancer. 2016;14:89–95.
Ciancio G, Manoharan M, Katkoori D, De Los SR, Soloway MS. Long-term survival in patients undergoing radical nephrectomy and inferior vena cava thrombectomy: single-center experience. Eur Urol. 2010;57:667–72.
Tabbara MM, González J, Ciancio G. The surgical evolution of radical nephrectomy and tumor thrombectomy: a narrative review. Ann Transl Med. 2023;11:262–262.
Bansal RK, Tu HYV, Drachenberg D, Shayegan B, Matsumoto E, Whelan JP, et al. Laparoscopic management of advanced renal cell carcinoma with renal vein and inferior vena cava thrombus. Urology. 2014;83:812–7.
Disanto V, Pansadoro V, Portoghese F, Scalese GA, Romano M. Retroperitoneal laparoscopic radical nephrectomy for renal cell carcinoma with infrahepatic vena caval thrombus. Eur Urol. 2005;47:352–6.
Gu L, Ma X, Gao Y, Li H, Li X, Chen L, et al. Robotic versus open level I–II inferior vena cava thrombectomy: a matched group comparative analysis. J Urol. 2017;198:1241–6.
Labbate C, Hatogai K, Werntz R, Stadler WM, Steinberg GD, Eggener S, et al. Complete response of renal cell carcinoma vena cava tumor thrombus to neoadjuvant immunotherapy. J Immunother Cancer. 2019;7:66.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
AF and AM wrote the main documents and prepared figures and tables. NR reviewed the manuscript and supervised the project.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval (Research involving human participants and/or animals) and Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Faegh, A., Moeinafshar, A. & Rezaei, N. Nephrectomy and IVC thrombectomy in renal cancer: a narrative review. Clin Transl Oncol 26, 574–583 (2024). https://doi.org/10.1007/s12094-023-03302-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03302-6