Abstract
Purpose
To determine the outcomes and to identify prognostic variables determining mortality and recurrence after surgery for renal cell cancer (RCC) with venous involvement.
Methods
Retrospective evaluation of the medical records of 132 patients with RCC and tumor thrombi treated at Johns Hopkins Hospital (1997–2008) was done. Kaplan–Meier analysis was used to determine survivals. Uni- and multivariate Cox proportional analysis was done to identify predictors for recurrence, all-cause mortality (ACM) and cancer-specific mortality (CSM).
Results
Mean follow-up was 30.3 (0.03–159.5) months. Sixty-four (48.5 %) patients had renal vein thrombus (Group 1), 55 (41.7 %) had subdiaphragmatic inferior vena cava (IVC) tumor thrombus (Group 2), while 13 (9.8 %) had involvement of IVC above diaphragm or atrial extension (Group 3). IVC thrombus was more common from the right-sided tumors. Patients with higher thrombus levels had more blood loss and complicated and longer hospital stay.
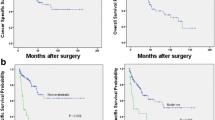
Thrombus level was not found to be a predictor of recurrence, ACM and CSM. One- and three-year recurrence-free survivals for non-metastatic patients were 69 and 53 %. Tumor size (p = 0.015), grade (p = 0.007) and venous wall invasion (p = 0.027) were predictors for recurrence. Five-year overall survival was 48, 35 and 13 % for 3 groups, respectively. Presence of distant metastasis (p = 0.032), size (p = 0.002), histology (p = 0.020) and grade (p = 0.013) were predictors of ACM. Five-year cancer-specific survival was 65, 43 and 36 for 3 groups, respectively. Tumor size (p = 0.001) and distant metastasis at presentation (p = 0.025) were the predictors of CSM.
Conclusions
Tumor thrombus level does not predict recurrence or mortality in RCC with venous involvement. Survival is determined by inherent aggressiveness of the cancer manifested by tumor size, grade and distant metastasis at presentation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) is the third most common urological malignancy. It is a highly vascular neoplasm with tendency to invade the venous system resulting in tumor thrombus in the renal vein and/or inferior vena cava (IVC) in 4–10 % of the cases [1]. Unlike the vast majority of patients with renal masses, patients with venous involvement are often symptomatic either because of large tumor size causing flank pain and hematuria or because of tumor thrombus causing venous congestion and increased risk of embolism [2]. The most effective therapeutic option in patients with RCC and venous involvement is aggressive surgical resection, including radical nephrectomy and thrombectomy, even in the presence of metastases [3, 4]. The level of tumor thrombus dictates the surgical approach and invasiveness of the procedure; however, the role of tumor thrombus level as a predictor for prognosis in these patients has been debated. While some studies have shown better survival with only renal vein involvement compared to IVC thrombus [5–7], others have shown long-term outcomes to be independent of thrombus levels [4, 8, 9].
We hereby present a single institution review of patients with RCC and venous involvement with an aim to determine the oncological outcomes and to identify prognostic variables determining mortality and disease recurrence in this patient population.
Methods
After obtaining approval from the Institutional Review Board, a retrospective evaluation of the medical records of patients who underwent radical nephrectomy at Johns Hopkins Hospital between 1997 and 2008 was done. We identified 132 patients with RCC and venous involvement. Patients were divided into 3 groups according to level of venous involvement: Group 1 with tumor invasion limited to renal vein or its segmental muscle containing branches, Group 2 with IVC involvement below diaphragm and Group 3 with IVC involvement above diaphragm or atrial involvement. Patient demographics, tumor characteristics, peri-operative variables, complications and the course of the disease were studied. Histology subtype, determined according to Heidelberg classification, was split into clear cell and non-clear cell RCC. Complications were graded according to Clavien-Dindo classification of surgical complications [10] (data not shown).
Follow-up
Patients were followed up every 6–12 months. Physical examination, imaging (abdominal CT and chest X-ray) and laboratories were done at each follow-up. Disease recurrence was defined as detection of new suspicious lesion by imaging with or without biopsy confirmation. Disease progression was defined as increase in size and/or number of metastatic lesions on imaging. Patient’s survival status was determined from medical records and social security death index registry. All-cause mortality (ACM) was defined as death from any cause. Cancer-specific mortality (CSM) was defined as death attributed to renal cancer in medical records. Survival was determined from the date of surgery to the date of last follow-up or death. Overall survival (OS) was defined as the interval from surgery to death from any cause. Cancer-specific survival (CSS) was defined as the interval from surgery to death from renal cancer.
Statistical analysis
Statistical analysis was done using statistical package for social sciences version 19 (Chicago, IL, USA). Kruskal–Wallis test or Mann–Whitney U test was run to compare means of continuous variables. Chi-square was run to compare proportions. Logistic regression analysis was done to identify predictors for complications. Uni- and multivariate Cox proportional hazard regression analysis was done to identify significant predictors of disease recurrence, ACM and CSM. OS and CSS were estimated and compared using Kaplan–Meier survival analysis. Statistical significance was considered at p ≤ 0.05.
Results
The mean follow-up was 30.3 (0.03–159.5) months. Patent demographics, peri-operative variable and tumor characteristics are summarized in Table 1. Sixty-four (48.5 %) patients had renal vein thrombus (Group 1), 55 (41.7 %) had subdiaphragmatic inferior vena cava (IVC) tumor thrombus (Group 2), while 13 (9.8 %) had involvement of IVC above diaphragm or atrial extension (Group 3). IVC thrombus was more common from the right-sided tumors (82 %, p < 0.001). All 27 patients with distant metastasis had lung metastases, 3 patients had bone, 2 had liver and 1 each had breast and retroperitoneal metastatic implant.
Patients with renal vein involvement had a smaller tumor size compared to patients with IVC thrombus (p = 0.009). No difference in tumor size was seen between Group 2 and 3. Tumor size was correlated with intra-operative blood loss (p < 0.001), tumor grade (p < 0.001) and venous wall invasion (p = 0.006).
Peri-operative period
Group 1 patients who underwent laparoscopic nephrectomy had smaller mean tumor size (7.5 vs 10.1 cm, p = 0.008), lesser mean intra-operative blood loss (249 vs 865 ml, p = 0.001) and shorter hospital stay (3.5 vs 7.0, p < 0.001) compared to open approach.
Complications during hospital stay were reported in 34.8 % of the procedures. Patients with higher thrombus levels had more intra-operative blood loss and had more complicated and longer hospital stay (Table 1). On logistic regression, thrombus level was the sole predictor for significant complications (grade 2–5) (p = 0.002, HR = 2.69 95 % CI = 1.45–4.98). There were no intra-operative deaths. Five deaths were reported in peri-operative period. One patient developed bilateral pulmonary embolism and was started on heparin, subsequently had extensive hemorrhagic stroke resulting in death. Refractory hemorrhage, multiorgan failure, cardiac arrest (unknown etiology) and metabolic acidosis secondary to bilateral iliac artery thrombosis were listed as the reasons of death for the other 4 patients.
Disease recurrence and progression
During the follow-up period, 21 (80.8 %, excluding 1 post-op death) patients with distant metastasis progressed and 39 (38.6 %, excluding 4 post-operative deaths) patients without metastasis had disease recurrence (local or distant). One- and three-year recurrence-free survivals for non-metastatic patients were 69 (±5) and 53 (±6) %. One- and three-year progression-free survivals for patients with metastatic disease at presentation were 15 (±8) and 5 (±5) %. Patients with metastatic disease at presentation were more likely to experience disease progression than disease recurrence in non-metastatic patients (p < 0.001). While no predictors for progression were identified in patients with metastatic disease, tumor size (p = 0.015, HR = 1.10, 95 % CI = 1.02–1.18), tumor grade (p = 0.007, HR = 1.86, 95 % CI = 1.19–2.91) and venous wall invasion (p = 0.027, HR = 2.14, 95 % CI = 1.09–4.22) were predictors for disease recurrence in non-metastatic disease. On multivariate analysis, only tumor size (p = 0.018) was found to be a significant factor dictating recurrence.
All-cause mortality and overall survival
Twenty-six (40 %), 39 (70.9 %) and 10 (76.9 %) patients of the Group 1–3 patients, respectively, died by the time of conclusion of study period. Overall survivals of different groups are listed in Table 2. Patient with only renal vein involvement survived longer than patient with IVC thrombus (Gr. 1 vs Gr. 2 p = 0.050, Gr. 1 vs Gr. 3 p = 0.025). No difference in survival was seen in Group 2 and 3 (p = 0.323). Overall survival in patients with metastatic disease at presentation was shorter than patients with non-metastatic disease (p = 0.030 by log rank test, p = 0.054 by generalized Wilcoxon test). Overall survival curves are depicted in Fig. 1.
On univariate analysis, presence of distant metastasis (p = 0.032, HR = 1.75, 95 % CI = 1.05–2.91), tumor size (p = 0.002, HR = 1.10, 95 % CI = 1.03–1.17), histology (p = 0.020, HR = 1.91, 95 % CI = 1.11–3.31) and tumor grade (p = 0.013, HR = 1.53, 95 % CI = 1.10–2.13) were found to be significant predictors for all-cause mortality. On multivariate analysis, tumor size (p = 0.001) and non-clear cell histology (p = 0.022) were found to be independent predictors.
Cancer-specific mortality and survival
Out of the 52 patients, for whom information on reason of death was available, 37 (71.2 %) patients died of renal cancer, 14 (24.1 %), 19 (47.5 %) and 4 (36.4 %) in Group 1, 2 and 3, respectively. Cancer-specific survivals of different groups are listed in Table 2. No difference in cancer-specific survivals was found between groups with different level of thrombus. Patients with metastatic disease at presentation had shorter cancer-specific survival compared to non-metastatic patients (p = 0.015 by log rank test, p = 0.053 by generalized Wilcoxon test). Cancer-specific survival curves are depicted in Fig. 2. On uni- and multivariate Cox regression analysis, tumor size (p = 0.001, HR = 1.16, 95 % CI = 1.07–1.27) and distant metastasis at presentation (p = 0.025, HR = 2.22, 95 % CI = 1.11–4.45) were found to be significant predictors of cancer-specific death.
Comment
In patients with renal cancer and venous involvement, aggressive surgical resection remains a mainstay of therapy and ensures reasonable long-term survival [1–4, 11, 12]. Surgical resection is done for curative intent in non-metastatic patients, while in the presence of distant metastasis, surgical resection is recommended for cytoreduction and/or palliation of symptoms [13–15]. The aim of current study is to study outcomes and identify prognostic variables after surgical treatment for renal cell cancer with venous involvement.
Five-year overall survival rate for non-metastatic patients in our cohort is 43 %. Five-year survival rates after radical nephrectomy and thrombectomy for the same group reported in literature varies from 34 to 72 % [2, 11, 16]. The wide variation in reported outcomes could be secondary to varied pre-operative assessment, surgical era, tumor biology, comorbidities of patient population and improvements in adjuvant therapy. In our study, patients with only renal vein involvement have better overall survival than patients with IVC thrombus. No difference in overall survival was seen according to level of IVC involvement. These results are similar to findings reported by Wagner et al. [6] from analysis of a multicenter study. Others have also not found proximal extent of thrombus to determine overall survival [8, 17]. In contrast, a recent analysis from multicentre study involving 1122 patients revealed survival rates to be different between renal vein, IVC below diaphragm and IVC above diaphragm involvement [18].
Five-year cancer-specific survivals for non-metastatic and metastatic renal cancer with tumor thrombus described in literature are 40–65 % and 6.5–28 %, respectively [15]. Our cancer-specific outcomes are toward higher limits of the range probably secondary to increased effectiveness of adjuvant therapy in current era. In our study, the five-year cancer-specific survival rates decrease with cranial extent of tumor but the difference was not statistically significant. In contrast, Dr. Blute’s group from Mayo Clinic found significantly longer cancer-specific survival in patient with only renal vein involvement compared to IVC thrombus [19–21]. The prognostic value of thrombus level, however, remains controversial. We did not find tumor thrombus level to be a predictor for disease recurrence or survival similar to findings of Klatte et al., Wagner et al. and others [6, 16, 17], while Klaver et al. [22] and Martinez-Salamanca et al. [18] have found thrombus level to be an independent predictor for cancer-specific survival.
Seventy-five patients died during the follow-up period. On univariate analysis, tumor grade, size, histology and presence of distant metastasis were significant predictors of all-cause mortality which correlates with findings of other studies [6, 8, 18]. Only size and non-clear cell histology was significant on multivariate analysis. In our study, tumor size, not the Fuhrman grade, was an independent predictor similar to the studies by Wagner et al. and Parekh et al. [6, 8], while other studies have found tumor grade to independently determine overall survival [18, 23, 24]. Our results could be explained by presence of strong correlations between the tumor size and grade. Tumor size was also an independent predictor of cancer-specific death.
The other important factor determining cancer death was presence of distant metastasis at presentation. Patients with metastatic disease at presentation had significantly shorter overall and cancer-specific survival compared to rest of cohort. This result is in conformity with the literature [3, 6, 20, 25]. In addition, the most common cause of death after surgical resection in these patients is metastatic RCC as reflected by our results and findings from other studies.
Presence of lymph nodes involvement was found to be another independent prognostic factor determining survival in some studies [6, 16]. Since lymphadenectomy was not routinely performed, pathological data on lymph node involvement were present in only 40 patients with 16 of them positive for cancer. Presence of lymph node disease was not found to be a significant factor determining survival in our analysis, similar to results published by Montie et al. [25].
The importance of tumor fat invasion as a predictor for cancer-specific mortality in renal cancer with tumor thrombus has recently been described [16, 20, 21, 26]. These studies have demonstrated fat invasion by tumor as a poor prognostic variable. Also, some studies have demonstrated venous wall invasion to be an important prognostic variable [6, 17, 27]. Our study did not find peri-nephric fat or venous wall invasion to be a predictor of survival.
Tumor grade, size and venous wall invasion predicted disease recurrence in our patients. Tumor size was found to be the only independent factor determining disease recurrence. Again the strong correlation between the three factors explains only the tumor size to be an independent predictor. While the three-year recurrence-free survival for non-metastatic patients was 53 %, the progression-free survival for patients with metastatic disease was only 5 %, highlighting the fact that patients with metastatic disease at presentation have more aggressive cancer.
We report a peri-operative mortality 1.6 % in RV group and 5.9 % in IVC thrombus group which has been comparable to other contemporary studies [6, 8, 19]. The difference between peri-operative mortality between renal vein versus IVC thrombus was not significant. Bleeding and thromboembolism complications were the most common in our cohort. Early surgical complications were associated with higher thrombus level with rate as high as 61 % in patients with supra-diaphragmatic IVC thrombus. These findings are similar to the results reported by Blute et al. and Klatte et al. [16, 19].
The study is limited by retrospective analysis of outcomes of a single institution and small sample size. By limiting the study period to 10 years, we have tried to minimize the variability introduced by changes in pre-operative assessment, surgical technique and post-operative care in these patients. Also, some of our patients had received neoadjuvant and/or adjuvant immunotherapy at different stages in their disease course which might have affected survival rates in an unpredictable fashion.
Conclusion
Patients with RCC and venous involvement usually have bigger tumors and are symptomatic at presentation; therefore, aggressive surgical resection is warranted for palliation of symptoms and cancer control. Characteristics of primary tumor including tumor size, grade and presence of distant metastasis at presentation were predictors of cancer-specific survival in this cohort. Thrombus level was not a significant predictor for recurrence and survival but predicted the risk of complicated and prolonged hospital stay.
References
Marshall FF, Dietrick DD, Baumgartner WA, Reitz BA (1988) Surgical management of renal cell carcinoma with intracaval neoplastic extension above the hepatic veins. J Urol 139(6):1166–1172
Gettman MT, Blute ML (2002) Surgical management of renal cell carcinoma invading the vena cava. Curr Urol Rep 3(1):37–43
Staehler G, Brkovic D (2000) The role of radical surgery for renal cell carcinoma with extension into the vena cava. J Urol 163(6):1671–1675
Swierzewski DJ, Swierzewski MJ, Libertino JA (1994) Radical nephrectomy in patients with renal cell carcinoma with venous, vena caval, and atrial extension. Am J Surg 168(2):205–209
Thompson RH, Cheville JC, Lohse CM, Webster WS, Zincke H, Kwon ED, Frank I, Blute ML, Leibovich BC (2005) Reclassification of patients with pT3 and pT4 renal cell carcinoma improves prognostic accuracy. Cancer 104(1):53–60
Wagner B, Patard JJ, Mejean A, Bensalah K, Verhoest G, Zigeuner R, Ficarra V, Tostain J, Mulders P, Chautard D, Descotes JL, de la Taille A, Salomon L, Prayer-Galetti T, Cindolo L, Valeri A, Meyer N, Jacqmin D, Lang H (2009) Prognostic value of renal vein and inferior vena cava involvement in renal cell carcinoma. Eur Urol 55(2):452–459
Moinzadeh A, Libertino JA (2004) Prognostic significance of tumor thrombus level in patients with renal cell carcinoma and venous tumor thrombus extension. Is all T3b the same? J Urol 171(2 Pt 1):598–601
Parekh DJ, Cookson MS, Chapman W, Harrell F Jr, Wells N, Chang SS, Smith JA Jr (2005) Renal cell carcinoma with renal vein and inferior vena caval involvement: clinicopathological features, surgical techniques and outcomes. J Urol 173(6):1897–1902
Polascik TJ, Partin AW, Pound CR, Marshall FF (1998) Frequent occurrence of metastatic disease in patients with renal cell carcinoma and intrahepatic or supradiaphragmatic intracaval extension treated with surgery: an outcome analysis. Urology 52(6):995–999
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Libertino JA, Zinman L, Watkins E Jr (1987) Long-term results of resection of renal cell cancer with extension into inferior vena cava. J Urol 137(1):21–24
Neves RJ, Zincke H (1987) Surgical treatment of renal cancer with vena cava extension. Br J Urol 59(5):390–395
Skinner DG, Pfister RF, Colvin R (1972) Extension of renal cell carcinoma into the vena cava: the rationale for aggressive surgical management. J Urol 107(5):711–716
Flanigan RC, Mickisch G, Sylvester R, Tangen C, Van Poppel H, Crawford ED (2004) Cytoreductive nephrectomy in patients with metastatic renal cancer: a combined analysis. J Urol 171(3):1071–1076
Pouliot F, Shuch B, Larochelle JC, Pantuck A, Belldegrun AS (2010) Contemporary management of renal tumors with venous tumor thrombus. J Urol 184(3):833–841; quiz 1235
Klatte T, Pantuck AJ, Riggs SB, Kleid MD, Shuch B, Zomorodian N, Kabbinavar FF, Belldegrun AS (2007) Prognostic factors for renal cell carcinoma with tumor thrombus extension. J Urol 178(4 Pt 1):1189–1195; discussion 1195
Manassero F, Mogorovich A, Di Paola G, Valent F, Perrone V, Signori S, Boggi U, Selli C (2011) Renal cell carcinoma with caval involvement: contemporary strategies of surgical treatment. Urol Oncol 29(6):745–750
Martinez-Salamanca JI, Huang WC, Millan I, Bertini R, Bianco FJ, Carballido JA, Ciancio G, Hernandez C, Herranz F, Haferkamp A, Hohenfellner M, Hu B, Koppie T, Martinez-Ballesteros C, Montorsi F, Palou J, Pontes JE, Russo P, Terrone C, Villavicencio H, Volpe A, Libertino JA (2011) Prognostic impact of the 2009 UICC/AJCC TNM staging system for renal cell carcinoma with venous extension. Eur Urol 59(1):120–127
Blute ML, Leibovich BC, Lohse CM, Cheville JC, Zincke H (2004) The Mayo Clinic experience with surgical management, complications and outcome for patients with renal cell carcinoma and venous tumour thrombus. BJU Int 94(1):33–41
Gettman MT, Boelter CW, Cheville JC, Zincke H, Bryant SC, Blute ML (2003) Charlson co-morbidity index as a predictor of outcome after surgery for renal cell carcinoma with renal vein, vena cava or right atrium extension. J Urol 169(4):1282–1286
Leibovich BC, Cheville JC, Lohse CM, Zincke H, Kwon ED, Frank I, Thompson RH, Blute ML (2005) Cancer specific survival for patients with pT3 renal cell carcinoma-can the 2002 primary tumor classification be improved? J Urol 173(3):716–719
Klaver S, Joniau S, Suy R, Oyen R, Van Poppel H (2008) Analysis of renal cell carcinoma with subdiaphragmatic macroscopic venous invasion (T3b). BJU Int 101(4):444–449
Haferkamp A, Bastian PJ, Jakobi H, Pritsch M, Pfitzenmaier J, Albers P, Hallscheidt P, Muller SC, Hohenfellner M (2007) Renal cell carcinoma with tumor thrombus extension into the vena cava: prospective long-term followup. J Urol 177(5):1703–1708
Kim HL, Zisman A, Han KR, Figlin RA, Belldegrun AS (2004) Prognostic significance of venous thrombus in renal cell carcinoma. Are renal vein and inferior vena cava involvement different? J Urol 171(2 Pt 1):588–591
Montie JE, el Ammar R, Pontes JE, Medendorp SV, Novick AC, Streem SB, Kay R, Montague DK, Cosgrove DM (1991) Renal cell carcinoma with inferior vena cava tumor thrombi. Surg Gynecol Obstet 173(2):107–115
Bertini R, Roscigno M, Freschi M, Angiolilli D, Strada E, Petralia G, Sozzi F, Capitanio U, Cremonini A, Rigatti P (2011) The extent of tumour fat invasion affects survival in patients with renal cell carcinoma and venous tumour thrombosis. BJU Int 108(6):820–824
Terrone C, Gontero P, Volpe A, Porpiglia F, Bollito E, Zattoni F, Frea B, Tizzani A, Fontana D, Scarpa RM, Rossetti SR (2008) Proposal of an improved prognostic classification for pT3 renal cell carcinoma. J Urol 180(1):72–78
Conflict of interest
The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sidana, A., Goyal, J., Aggarwal, P. et al. Determinants of outcomes after resection of renal cell carcinoma with venous involvement. Int Urol Nephrol 44, 1671–1679 (2012). https://doi.org/10.1007/s11255-012-0314-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-012-0314-x