Abstract
Status epilepticus (SE) can lead to serious neuronal damage and act as an initial trigger for epileptogenic processes that may lead to temporal lobe epilepsy (TLE). Besides promoting neurodegeneration, neuroinflammation, and abnormal neurogenesis, SE can generate an extensive hypometabolism in several brain areas and, consequently, reduce intracellular energy supply, such as adenosine triphosphate (ATP) molecules. Although some antiepileptic drugs show efficiency to terminate or reduce epileptic seizures, approximately 30% of TLE patients are refractory to regular antiepileptic drugs (AEDs). Modulation of glucose availability may provide a novel and robust alternative for treating seizures and neuronal damage that occurs during epileptogenesis; however, more detailed information remains unknown, especially under hypo- and hyperglycemic conditions. Here, we review several pathways of glucose metabolism activated during and after SE, as well as the effects of hypo- and hyperglycemia in the generation of self-sustained limbic seizures. Furthermore, this study suggests the control of glucose availability as a potential therapeutic tool for SE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Status epilepticus (SE) is a clinical emergency characterized by either a continuous self-sustained seizure or a sequence of short seizures with no return to baseline, unleashing a high mortality rate [1,2,3,4,5,6,7,8]. SE can be convulsive or nonconvulsive [9,10,11,12,13,14,15,16], and it is capable of promoting neuronal death, gliosis, and wide molecular changes in several brain areas [4, 11, 12, 17, 18]. Furthermore, SE leads to temporal lobe epilepsy (TLE), which is characterized by spontaneous recurrent seizures, abnormal synaptic reorganization, mossy fiber sprouting, hippocampal neurodegeneration, and neurogenesis [19,20,21,22,23]. SE induction in rodents by electrical or chemical stimulation have been used to model epileptogenesis process and TLE clinical features [4, 8, 10,11,12,13, 24,25,26,27,28,29,30,31,32]. Local or systemic administration of the pilocarpine (PILO) or kainic acid leads to a pattern of repeated limbic seizures and/or SE, which can endure for many hours [4, 8, 19, 30, 32].
Recent [18F]fluorodeoxyglucose positron emission tomography (FDG-PET) studies with patients and animal models showed that SE induces secondary hypometabolism in the epileptogenic areas, including hippocampus, cortex, and striatum [33,34,35,36,37,38,39,40]. Secondary hypometabolism has also been associated to specific patterns of SE in studies with humans and animal models [33, 41,42,43]. During an epileptic seizure or SE, the overexcited neurons must increase glucose uptake [44,45,46] above organism’s supply capacity, resulting in adenosine triphosphate (ATP) deficit in the nervous tissue [47], where energy consumption is much higher than in several other body tissues [48]. Glucose is taken up into brain cells by two major groups of transporters: (1) glucose transporters (GLUTs) for facilitated diffusion and (2) sodium/glucose cotransporters (SGLTs) for its secondary active transport [49,50,51,52,53,54]. Glucose transporter 1 (GLUT1) is expressed in both blood–brain barrier and glial cells [55], while glucose transporter 3 (GLUT3) presents high glucose affinity and transport capacity in neurons [54, 56,57,58,59]. Sodium/glucose cotransporters 1 and 2 (SGLT1 and SGLT2) have been observed in hippocampus [50, 51]. Despite the evidence of glucose availability modulating brain damage, it has been difficult to define the role of glucose transporters and associated glucose metabolism in isolated epileptic seizures or during and after SE.
Here, we review recent advances regarding regulation of glucose supply during self-sustained epileptic seizures. Our purpose was to survey the main data associated with the modulation of glucose in seizures, in order to discuss the possible pathways that could explain the alterations on seizures susceptibility in hypo- and hyperglycemic conditions. Furthermore, we summarize these findings and draw an overview to contribute for new insights in treatment strategies that could effectively reduce neuronal damage associated with TLE, in the absence of counteractive side effects.
Intracellular Metabolism of Glucose and SE
The physiological pattern of the brain requires high amounts of energy supply, in constant demand, comprising an average of 20% of the body’s energetic consumption [60]. Glucose is converted into glucose-6-phosphate (glucose-6P) immediately after being transported to the intracellular environment. Glucose-6P is processed through glycolysis, resulting in two molecules of pyruvate which are metabolized during the tricarboxylic acid cycle and the oxidative phosphorylation in the mitochondria [61].
Functional brain imaging techniques, such as FDG-PET and functional magnetic resonance imaging (fMRI), allowed for the conduction of integrative studies between regional brain energy metabolism (energy delivery and use) and neural cell activity [62,63,64,65]. FDG-PET detects alterations in regional cerebral blood flow, as well as in glucose and oxygen consumption [9, 66,67,68] while fMRI provides data on regional blood oxygenation levels [69]. It was demonstrated that cerebral glucose metabolism is altered in epilepsy as well as in other neurological disorders [70,71,72,73,74,75].
Glucose Metabolism in Clinical Studies
SE promotes a sharp increase of regional cerebral blood flow and oxygen consumption correlated with enhancement in glucose utilization [76]. In an 11-year-old girl, an intense hypometabolism was observed in most of the left hemisphere, 6 weeks, and 8 months after one SE episode. The right hemisphere, however, showed a heterogeneous increase in the metabolic rate of glucose only at 8 months after the SE occurred [77]. Similarly, a severe hypometabolism was observed in the left hemisphere of a 48-year-old right-handed man with Alien hand syndrome after a complex partial SE. Notably, the periodic lateralized epileptiform discharges (PLEDs) generated during the SE were only detected in the left hemisphere, especially in areas such as basal ganglia and thalamus [78]. Moreover, a patient presenting right hemispheric PLEDs due to SE showed right hypometabolism in the temporal, parietal, and occipital lobes [79]. The same pattern has been seen in an elderly patient with permanent sensorimotor dysphasia after SE [42]. These authors suggest that both lateralized seizures and hypometabolism are directly correlated with the pattern of neuronal death observed in hippocampal formation and adjacent areas [11, 12, 80].
In other clinical studies, FDG-PET showed scattered areas of regional hypometabolism in pediatric and adult patients with refractory and nonconvulsive SE [9, 81, 82]. A recent study showed hypometabolism in cortical areas, such as frontal, parietal, and posterior cingulate cortices, and hypermetabolism in thalamic, caudate and dentate nuclei, and cerebellar vermis, of a 17-year-old girl with absence of SE [83]. According to the authors, these findings indicate a relevance of the thalamus in absence of SE, as well as modulation of cortical and cerebellar regions associated with the control of epileptiform discharges. Table 1 shows a summary of clinical studies related to cerebral glucose metabolism.
Glucose Metabolism in Animal Models
Since the 1990s, distinct animal models of SE have shown alterations in the metabolism of cerebral glucose during or after self-sustained seizures [10, 28]. In 1991, VanLandingham and Lothman, using continuous hippocampal stimulation (CHS), developed a nonconvulsive model of self-sustained limbic SE (SSLSE). This model was used to evaluate the regional cerebral glucose utilization (RCGU) after 90 min of CHS [10, 28]. RCGU was observed in acute (1 h after induction) and chronic (1 week or 1 month) periods. During the acute period, RCGU was elevated in some brain regions, such as hippocampus, retrohippocampal area, and limbic and nonlimbic structures, while hypometabolism was observed in neocortical structures. In the chronic period, 1 week after SE, an increase of RCGU was recorded in some limbic regions, but RCGU levels returned to baseline at 30 days after SE [10]. On another study, rats were submitted to the same protocol with or without hippocampal commissurotomies, in order to evaluate whether hippocampal commissures were necessary for the initiation and maintenance of SSLSE. These studies showed RCGU was bilaterally and symmetrically enhanced in hippocampus and other areas (retrohippocampal, limbic, and nonlimbic structures) in the group with preserved commissures, while both groups presented bilateral hypometabolism in neocortical regions [28].
Glucose hypometabolism was also shown in rodent SE models induced by kainic acid or PILO. In lithium-PILO model of SE in rats, a severe glucose hypometabolism occurred in hippocampus, cortex, and striatum during epileptogenesis, and this alteration was associated to other pathological changes, such as hippocampal, atrophy, neuronal death, and gliosis [33, 84]. This hypometabolism was partially recovered in the chronic phase, maybe due to increased cell number associated with astrogliosis [68]. Similarly, in the early phase after systemic PILO-induced SE, glucose utilization was reduced severely in limbic structures, such as hippocampus; however, glucose levels were restored during the chronic period [39]. Controversially, other authors have reported that reduced glucose metabolism gradually expands to limbic regions in the chronic phase [36]. Furthermore, in the kainic acid-induced SE model in rats, FDG-PET demonstrated hippocampal hypometabolism after 24 h of SE, which tended to decrease in the early phase of epileptogenesis and then stood out again with the emergence of CREs, what was accompanied by an increase in the expression of GLUT1 and synaptophysin in the same area [43]. These authors concluded that the glucose hypometabolism precedes neuronal loss and CRE. In addition, in a mouse model of PILO-induced SE, mitochondria were metabolically dysfunctional in hippocampal formation and cortex, 3.5 to 4 weeks after SE [85]. Moreover, a recent study showed a significant increase in glucose uptake in rat hippocampus after 4 and 24 h of SE induced by lithium-PILO, later returning to baseline levels [86]. Controversially, these same authors observed a hippocampal hypometabolism in chronic epileptic rats [86]. Table 2 shows a summary of preclinical studies of SE related to cerebral glucose metabolism.
Taken together, these clinical and experimental findings support the idea that SE compromises intracellular glucose metabolism, which may contribute to the activation of inflammatory mechanisms, neuronal loss and gliosis, and may also predispose the brain to develop epilepsy [87]. Therefore, restoring glucose metabolism during and after continuous self-sustained seizures may be an effective way of dealing with epileptogenesis and its complications. Additionally, because of the different pathophysiological findings, experimental models, brain areas, and phases of epileptogenesis, the precise mechanism among the possible factors that contribute to hypometabolism or hypermetabolism in these conditions has not been reported in current literature. Therefore, new clinical and preclinical trials should be carried out to address this issue.
Hypo- and Hyperglycemic Mechanisms Associated with SE Generation
Metabolic disorders are often associated with epileptic seizures; however, their relationship is poorly understood. The importance of glucose balance has emerged from studies demonstrating that epileptic seizures can be accentuated under conditions of hyper- or hypoglycemia [47].
Hypoglycemia and SE
Hypoglycemia is a clinical condition characterized by low plasma glucose concentration affecting both diabetic and nondiabetic patients. Hypoglycemia and hypoglycemic seizures may occur due to an increase in the amount of insulin in the plasma, being common in patients who are under treatment with insulin [88].
Neuronal excitation is tightly tied to brain energy metabolism. Severe hypoglycemia represents a serious threat for normal brain metabolism causing unbalance between inhibitory and excitatory neuronal networks, what leads to increased seizure susceptibility and risk for brain damage. The functional and structural injuries induced by severe hypoglycemia may persist when normal glucose levels are restored, leading to permanent cognitive dysfunction, EEG abnormalities, and predisposition for unprovoked seizures [89].
According to several studies, there is a not fully understood relationship between hypoglycemia and epileptic seizures [90,91,92,93,94]. It is well established that low glucose concentrations can change cortical excitability [95] and stimulate glutamate release, inducing cerebral hyperexcitability and, consequently, NMDA receptor-mediated excitotoxicity [96], with hippocampus showing particular susceptibility to these effects [97].
Studies aiming to describe epileptic manifestations associated with hypoglycemia have been carried out since the 1980s. Sapolsky and Stein [98], following a kainic acid-induced SE in rats, showed that hippocampus of hypoglycemic animals presented more damage when compared with normoglycemic or hyperglycemic ones, suggesting that limited energy compromises the survival of neurons in seizures. Severe acute cases of hypoglycemia in humans as a complication of therapy for insulin-dependent diabetes mellitus [90] or due to the excessive consumption of alcohol [99] are often associated with neurological side-effects [100, 101], resulting frequently in generalized seizures [102, 103]. A study evaluated causes of symptomatic convulsive SE in children, and found that most of them had metabolic disorders, such as electrolyte imbalance, hypoglycemia, hypocalcemia, or hypomagnesemia [91]. Other authors found that 11% of adult patients with SE presented a metabolic disfunction as cause of convulsive SE [104]. Unfortunately, these studies did not separate the isolating effect of blood glucose from other metabolic disturbances [105]. In rats, insulin-induced hypoglycemia also leads to generalized seizures [92, 106].
There is relative limitation in studies that have evaluated the relationship between hypoglycemia and epilepsy in animal models. One such study investigated this relationship by evaluating the modulation, by glycemic levels, of kainate-induced seizure susceptibility, as well as its neuropathological consequences [47]. These authors found no difference in the severity of seizures between hypoglycemic mice and other groups, as evidenced by similar latency at the onset of the first severe seizure and its duration. However, their results demonstrated that mice with insulin-induced hypoglycemia had an increase in hippocampal neurodegeneration, with significant loss of cells in three hippocampal subfields (dentate hilus, CA3 and CA1) [47].
Diabetes is not directly related to seizures, however the hypoglycemic conditions eventually generated in this process may be associated. Seizures can occur in diabetic and non-diabetic rats [94], and seizures may be associated with acute hypoglycemia, as well as the death of animals is related to the frequency of seizures and not to blood glucose levels. This suggests that hypoglycemia would be a predisposing factor to seizures, therefore a morbidity and not a mortality factor. Furthermore, the same authors showed that severe hypoglycemia as a precondition for seizures was associated with animal deaths, and suggest that this is probably due to the brainstem involvement in the seizures, which may affect the cardiorespiratory system and lead to mortality [93, 94].
Unlike animal model studies, in the last years several, mostly cohort, studies in human patients have been conducted to elucidate the relationship between hypoglycemia and epilepsy. In 2015, Halawa and colleagues investigated an association between different levels of hypoglycemia and the occurrence of epileptic seizures in patients without previous diagnosis of epilepsy; as a result, coma was reported as the neurological symptom mostly caused by hypoglycemia, with convulsions being a rare event. In addition, a cohort study with more than 2,000 patients with type 1 diabetes identified an increased risk for epilepsy in these patients with a history of hypoglycemia (16,5%) compared with patients without hypoglycemia (2,67%) [107]. Moreover, an elegant study showed that seizures associated with hypoglycemia occurred in 90 of 170 patients aged 0 to 4 years; in 68% of the patients, the first hypoglycemic seizure was brief and fast, whereas the remaining 32% had more severe conditions and evolved to SE or coma [108]. The evaluation of such events according to the age of the patients demonstrated that brief seizures were more frequent than SE in both age groups studied: 63% versus 37% in neonates and 71% versus 29% in infants/children; in fact, blood glucose levels seem to be critical for the type of seizures presented by these patients, as they were significantly lower in SE than in brief seizures events [108].
Comparing neonatal period with childhood, the sequelae of SE are more intense in early ages [108]. Hypoglycemia in the neonatal period is relatively more common than in the older age groups and is considered a possible cause of seizures in the first year of life [109]. The relationship between the first hypoglycemic event and seizures was observed and this outcome was more frequent in children under 3 years old [108]. In the first years of life, seizures may initially appear as spasms [110].
It is important to note that SE is not necessarily associated with systemic factors, including hypoglycemia, in human patients, therefore hypoglycemia does not work as an etiological agent of SE [111]. Although this study was performed through medical records and electroencephalograms of only three patients without systemic complications who had died between 11 and 27 days after triggering SE, other authors found a weak correlation between hypoglycemia and epileptic seizures [88, 112]. For example, in a case of 229 diabetic patients, only 2 presented hypoglycemia and epileptic seizures concomitantly, representing a total of 0.8% of the diabetic patients evaluated [88]. Table 3 shows a summary of clinical and preclinical studies that correlate hypoglycemia and SE.
Hyperglycemia and SE
Among metabolic disturbances, hyperglycemia has frequently associated with deleterious effects on the central nervous system (CNS) induced by epileptic seizures [113]. Both type I and type II diabetes increase the susceptibility to epileptic seizures in these patients, emphasizing the importance of glycemic control for seizure treatment [114, 115]. Neuronal excitability and epileptic seizures are related to the rapid use of glucose and glycolysis [116, 117]. Hyperglycemia may also be associated with other factors to become the cause of SE. It is known that age can influence the outcome and severity of convulsive SE [118, 119].
As in the clinical studies, it has been shown that diabetic animals frequently develop seizures, depending on the severity of an ischemic insult and blood glucose concentration [113, 120]. Additionally, rats with diabetic hyperglycemia had a higher severity of seizures which induced a greater damage of the hippocampus after SE, followed by a higher mortality rate, or worsening of the cognitive capacity for learning in surviving animals [117]. This corroborates with another study that showed an increase of kainate-induced cell loss after SE in mice with non-ketotic hyperglycemia and diabetes-induced hyperglycemia [47].
Currently, there are some studies that point out that hyperglycemia can facilitate the entry of glucose into the brain and be involved in cell death during SE [121], also triggering morphological changes at the presynaptic terminals of mossy fibers that play important roles in increasing neuronal damage. Acute and chronic hyperglycemia produces increased susceptibility to excitotoxic cell death, the same effect observed as a consequence of seizures [47, 122]. High levels of glucose in the brain may increase the amount of ATP, facilitating ATP-dependent brain reactions. These results show that hyperglycemia by itself is able to kill neurons, especially in the hilus region of hippocampus [121]. On the other hand, infusing a certain concentration of glucose after kainic acid-induced SE can be profoundly neuroprotective against seizure-induced neuronal damage [47, 121]. In this context, this brain glucose modulation can protect neurons of specific hippocampi regions. Table 4 shows a summary of clinical and preclinical studies that correlate hyperglycemia and SE.
Glucose Transporters in the Brain and Their Involvement in SE Modulation
Although the brain accounts for only 2% of body mass, it receives 15% of cardiac output and 25% of glucose supply, being responsible for 20% of the organism’s oxygen consumption [123]. Glucose is transported through the blood-brain barrier (BBB) to the cerebrospinal fluid via glucose transporters or by the capillaries of the circumventricular organs which do not have tight junctions nor exert barrier properties [60, 124,125,126]. Glucose passes through the cell membrane by a specific transport system, which includes two types of glucose transporters: (1) the facilitated diffusion GLUTs that transport glucose in favor of its concentration gradient and 2) the SGLTs that transport glucose in favor of the sodium concentration gradient [127].
Glucose Transporters
GLUT1 is expressed in the basal and luminal membranes of the BBB endothelial cells, as well as in astrocytes and cell bodies of neurons, but it has not been described in microglia [55]. GLUT3 is the most abundant in the brain and is expressed in neurons, mainly in axons and dendrites, having a transport capacity five times greater than that of GLUT1 [128]. Furthermore, GLUT3 adapts to the demands of neuronal metabolism [53]. Currently, it is known that other types of GLUTs are expressed in the brain. GLUT2 protein is present in hypothalamic neurons and serves as a glucose sensor in the regulation of food intake [129]; moreover, GLUT2 regulates synaptic activity and contributes to neurotransmitters release in hippocampal neurons. Besides, GLUT5 has been described only in microglia as a hexose transporter and its regulation is still poorly understood. Finally, GLUT4 and GLUT8 are insulin-regulated glucose transporters and these transporters, although expressed in cell bodies of cortex and cerebellum neurons, are mainly found in the hippocampus and amygdala [130].
Hypo- and hyperglycemia have been shown to be able to modulate the expression of GLUTs in the brain [131]. An interesting study showed that chronic hypoglycemia induced by insulin infusion for 1 week increased the expression of GLUT3, but not GLUT1, showing a correlation between the rate of cerebral glucose metabolism and GLUTs [132]. Similarly, upregulation of GLUT3 protein was observed in the brain of rats subjected to insulin infusion (25 U/kg) for 8 days, indicating that this transporter adapts to metabolic disorders such as chronic hypoglycemia [133]. Recently, other authors have shown the expression of GLUT3 in several models of hypoglycemia [134]. In this study, mice with severe insulin-induced hypoglycemia experienced seizures and a trended higher GLUT3 in the hippocampus and cortex, which returned to baseline levels after glucose reperfusion. In addition, these authors related the change in GLUT3 expression to the upregulation of the nitric oxide marker (nitrotyrosin), indicating that this scenario triggered by severe hypoglycemia with seizures may be associated with glutamate/NMDAreceptor/nitric oxide/GLUT3 axis pathway [135, 136]. Interestingly, Pitchaimani et al. [134] also showed a change in p-BADser155 expression, suggesting a metabolic preference for ketone bodies during hypoglycemia. In summary, severe insulin-induced hypoglycemia alters the expression of GLUT3 possibly as a way of adapting the brain to glucose uptake in order to preserve normal neuronal functioning [134, 137].
Additionally, it was showed that chronic streptozotocin-induced hyperglycemia was able to increase the use of local cerebral glucose, as well as promoting a moderate (7.5%) reduction in the average density of GLUT1, but not GLUT3 [138]. The reduction of GLUT1 expression in BBB suggests a neuronal protective effect of hyperglycemia in brain. Likewise, these authors have observed a downregulation of GLUT1 in brain regions, including cortex, amygdala, thalamus, and cerebellum. Similar data showed that GLUT1 expression is downregulated in the BBB after a week of diabetes in rats [139].
GLUTs are crucial energy sources for the brain and their disorder can lead to a series of neurological manifestations. Considered an epileptic encephalopathy, GLUT1 deficiency syndrome (GLUT1DS) is caused by de novo heterozygous mutation in SLC2A1 gene, and it affects the CNS due to impaired cerebral glucose uptake through the BBB, which also culminates in reduced glucose levels in the cerebral spinal fluid (hypoglycorrhachia) [140,141,142,143]. A number of clinical phenotypes are observed in GLUT1DS patients, such as delayed development, cognitive and learning deficits with mental retardation, movement damage, including ataxia, dystonia, or dyskinesia, as well as absence seizures and generalized tonic–clonic seizures [144,145,146,147]. GLUT1 deficiency or persistent childhood hypoglycemia can trigger neuroglycopenia, caused by a partial and persistent damage to the CNS glucose supply and that culminates in hyperexcitability, epilepsy, movement disorders and other neuropsychopharmacology manifestation [148]. These results in GLUT1 deficiency patients, may be associated with the activation of anaerobic glycolysis, flux from fatty acids to triglyceride, production of fatty acids and cholesterol esters, acting as a trigger for epileptogenesis [149]. The ketogenic diet has been used as the therapy of choice in GLUT1DS patients for reducing seizures and motility disabilities leading to remission of paroxysmal symptoms [142, 150, 151]. However, this treatment has already failed in GLUT1DS patients with refractory epilepsy [152]. In addition, it has been reported that acute hyperglycemia was able to promote a transient improvement in seizures and EEG recording, as well as in attention and motor activity of GLUT1DS patients [153]. Figure 1 summarizes the glucose transporters regulation in normoglycemic, hypoglycemic, hyperglycemic and GLUT1DS conditions.
Schematic drawing of the modulation of GLUTs expression in the brain under normal and pathological conditions. Under normoglycemic conditions, GLUT1 and GLUT3 are at baseline levels (a). However, when glucose concentration decreases in CSF during chronic insulin-induced hypoglycemia, GLUT3 expression increases as an adaptive mechanism (b). On the other hand, streptozotocin-induced hyperglycemia moderately decreases the expression of GLUT1 (c). During GLUT1DS, glucose concentration in the CSF decreases due to de novo heterozygous mutation in the SLC2A1 gene, compromising glucose uptake via the BBB (d). BBB (blood-brain barrier); CSF (cerebrospinal fluid); GLUT (glucose transporter); GLUT1DS (GLUT1 deficiency syndrome)
Sodium/Glucose Cotransporters
SGLTs are transmembrane proteins that contribute to cellular homeostasis by performing secondary active glucose transport in favor of the electrochemical gradient of sodium ions. These proteins were initially identified in the brush border membrane of enterocytes and in the proximal kidney tubule cells [154]. SGLT1 is encoded by the SLC5A1 gene and is composed of 14 transmembrane segments, whose N-terminal face is directed towards the interstitial and the C-terminal face is anchored inside the plasma membrane [155]. A powerful role of water transport was associated with SGLT1, once the stoichiometric relationship of transport capacity was observed to be 2Na+:1glucose:264 H2O molecules [156]. Sodium ions initially bind to the extracellular side of SGLT1, promoting a conformational change that allows glucose to attach to the binding site. A new conformational change of the protein allows the release of sodium ions and glucose in the intracellular environment, after what the transport cycle is completed, allowing for the return of the protein to its initial conformation [154]. SGLT1 is mainly expressed in the intestine, but is also present in the kidneys, salivary glands, trachea, skeletal muscle, heart, liver, testis, prostate and brain [49, 154, 157, 158]. Recently, expression of SGLT1 has been shown in various regions of the CNS, such as hippocampus (CA1 and CA3), parietal and frontal cortices, putamen, paraventricular nucleus of the hypothalamus, amygdala, and in the Purkinje cells of the cerebellum [51].
SGLT2 isoform is encoded by the SLC5A2 gene and carries the transport of only one sodium ion for each glucose molecule [159]. SGLT2 has been observed in the hippocampus and cerebellum. Functional assays with mouse brain slices suggest that SGLT2 is responsible for capturing 20% of total methyl-4-[F-18] fluoro-4-deoxy-d-glucopyranoside (Me-4FDG), a highly specific substrate of SGLT not transported by GLUTs [50].
Functional Role of Brain SGLTRegulation in Limbic Seizures and Neurodegeneration After PILO-Induced SE
In conditions of normoglycemia and adequate oxygen perfusion, glucose transport is probably mediated by GLUT3 and facilitated glucose diffusion may be sufficient for the energy supply of neurons [154]. However, reality may be different when energy supply is reduced and/or energy consumption is enhanced in pathological situations such as ischemia, hypoxemia, hypoglycemia, or epileptic seizures. The concentration of glucose in the firing microenvironment of the neurons can decrease greatly, being lower than the Km value of GLUT3 [49]. These authors induced an epileptic focus with penicillin in the frontal cortex and observed increased uptake of glucose via SGLTs, reflecting the upregulation of this protein in neurons. These findings show that on a low-glucose concentration, as what occurs during seizures, SGLTs may be essential for the survival of neurons.
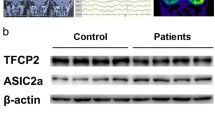
Few studies have associated the SGLTs in SE modulation [11, 49,50,51]. Our group has recently demonstrated for the first time an intrinsic association of SGLTs with neuronal survival during limbic self-sustained seizures induced by intrahippocampal PILO microinjection [11]. In this study, SGLTs were blocked by intrahippocampal administration of phlorizin (PZN), a nonspecific inhibitor of SGLTs, 30 min prior to PILO administration. Inhibition of SGLTs increased the number of wet dog shakes that occur during SE and can serve as an indicator of SE severity. In addition, aggravated self-sustained limbic seizures occurred during the 90 min of SE, showing a higher frequency of the most severe behaviors described by the Racine’s scale (class 5) [160] in the PZN group. These behavioral findings indicate that the blockage of SGLTs intensify limbic seizures during SE.
Additionally, 24 h after SE, the PZN increased the number of Fluoro-Jade-positive neurons, a marker of neural cells in degeneration [12, 161], in the regions of the dentate gyrus (DG), the hilus of the DG, CA3, and CA1 of hippocampus [11]. Taken together, these behavioral and histopathological results support the idea that SGLTs are fundamental tools in low-glucose concentration and high metabolic demand conditions, such as during prolonged limbic seizures, thus protecting neurons against degeneration.
New Insights for Action Mechanism of Glucose in the SE
Under normal physiological situation, glucose crosses the BBB through GLUT1 and can enter directly into neurons through GLUT3. Glucose is metabolized in cytoplasm by conversion into molecules of pyruvate, which pass through the tricarboxylic acid cycle and oxidative phosphorylation in mitochondria [60].
On the other hand, during prolonged epileptic seizures, such as seen in SE, glucose metabolism is compromised, which is directly associated with mitochondrial dysfunction, as well as increased reactive oxygen species levels. This metabolic deficit impairs cell survival, aggravating cell death rates. In an attempt to protect neurons against neuronal death, according to some authors [11, 50, 51], the affected brain areas increase uptake of glucose via SGLT1 [49], possibly by enhancing the expression of this transporter. Although greater GLUT3 expression also occurs during SE [43] to support the increased energy demand and glucose metabolism [33, 68, 82,83,84], SGLT1 expression is necessary in order to transport glucose in lower concentrations, that are below the Km of GLUT3 [49]. Therefore, increased expression of SGLT1 may function as an additional support to GLUT3, contributing to the survival of neurons in hypoglycemic conditions.
So far, control of glucose availability by modulating their transporters may be a form of protection against damage from SE. It is known that glucose sensors, such as T1R2/T1R3 heterodimer, are expressed in the hippocampus [162], and these sensors transduce signals for the translocation of SGLTs into enterocytes [163]. Our hypothesis is that increased hippocampal glucose concentration activates a higher SGLT translocation in neurons via T1R2/T1R3, protecting the neurons from degeneration. Figure 2 summarizes the glucose transporters and metabolic regulation in control, SE and SE associated with intracerebroventricular treatment of glucose.
Schematic drawing on glucose modulation during SE and intracerebroventricular glucose treatment. In a physiological condition, glucose enters neurons through GLUT3, and it is metabolized to pyruvate, following the citric acid (TCA) cycle to generate ATP (a). However, neuronal hyperexcitability associated with hypermetabolism occurs during SE settlement, activating a compensatory pathway mediated by SGLTs’ translocation in order to transport glucose in lower concentrations and attempt to protect neurons against degeneration (b). As this epileptogenic insult is continuous and self-sustaining, a mitochondrial dysfunction is triggered followed by oxidative stress, culminating in excitotoxic neuronal death. Possibly, increased SGLTs’ translocation through modulation of brain glucose levels may protect neurons in the acute phase of epileptogenesis (c).
Conclusion and Future Perspectives
During the early epileptogenesis, shortly after SE, glucose metabolism is elevated, suffering a significant decrease in the chronic phase [86]. Furthermore, glycemic disorders may increase the susceptibility to the genesis of epileptic seizures. As seen previously, hypo- and hyperglycemia can function as crucial factors for the SE generation, although the intrinsic pathophysiological mechanisms responsible for this association remain unclear. In addition, hypo- and hyperglycemia are able to accentuate SE-induced hippocampal damage in animal models [47]. Interestingly, these authors showed that adequate glucose supply protects hippocampal cells against seizure-induced excitotoxic cell death. Considering these, regulation of glucose availability appears to be a promising pathway capable of attenuating the severity of seizures as well as the seizure-induced brain damage in the earlier phase of epileptogenesis generated by SE. Likewise, the intracellular mechanisms of hypo- and hyperglycemia and glucose modulation associated with SE as possible therapeutic targets need to be further investigated.
References
Sloviter RS (1999) Status epilepticus-induced neuronal injury and network reorganization. Epilepsia 40:34–39. https://doi.org/10.1111/j.1528-1157.1999.tb00876.x
Sánchez S, Rincon F (2016) Status epilepticus: epidemiology and public health needs. J Clin Med 5. https://doi.org/10.3390/jcm5080071
Mohapel P, Ekdahl CT, Lindvall O (2004) Status epilepticus severity influences the long-term outcome of neurogenesis in the adult dentate gyrus. Neurobiol Dis 15:196–205. https://doi.org/10.1016/j.nbd.2003.11.010
Leite JP, Bortolotto ZA, Cavalheiro EA (1990) Spontaneous recurrent seizures in rats: An experimental model of partial epilepsy. Neurosci Biobehav Rev 14:511–517. https://doi.org/10.1016/S0149-7634(05)80076-4
Cole AJ, Koh S, Zheng Y (2002) Are seizures harmful: what can we learn from animal models?
Meldrum BS, Horton RW (1973) Physiology of status epilepticus in primates. Arch Neurol 28:1–9
Meldrum BS, Brierley JB (1973) Prolonged epileptic seizures in primates. Ischemic cell change and its relation to ictal physiological events. Arch Neurol 28:10–17
W a T, E a C, Schwarz M et al (1983) Limbic seizures produced by pilocarpine in rats: behavioural, electroencephalographic and neuropathological study. Behav Brain Res 9:315–335. https://doi.org/10.1016/0166-4328(83)90136-5
Pari E, Rinaldi F, Premi E et al (2014) A follow-up 18F-FDG brain PET study in a case of Hashimoto’s encephalopathy causing drug-resistant status epilepticus treated with plasmapheresis. J Neurol 261:663–667. https://doi.org/10.1007/s00415-013-7228-0
VanLandingham KE, Lothman EW (1991) Self-sustaining limbic status epilepticus. I. Acute and chronic cerebral metabolic studies: limbic hypermetabolism and neocortical hypometabolism. Neurology 41:1942–1949
Melo IS, Santos YMO, Costa MA et al (2016) Inhibition of sodium glucose cotransporters following status epilepticus induced by intrahippocampal pilocarpine affects neurodegeneration process in hippocampus. Epilepsy Behav 61:258–268. https://doi.org/10.1016/j.yebeh.2016.05.026
Castro OW, Furtado MA, Tilelli CQ et al (2011) Comparative neuroanatomical and temporal characterization of FluoroJade-positive neurodegeneration after status epilepticus induced by systemic and intrahippocampal pilocarpine in Wistar rats. Brain Res 1374:43–55. https://doi.org/10.1016/j.brainres.2010.12.012
Islas-Espinoza AM, Campos-Rodriguez C, San Juan ER (2018) Thalidomide protects against acute pentylenetetrazol and pilocarpine-induced seizures in mice. J Toxicol Sci 43:671–684. https://doi.org/10.2131/jts.43.671
Wong M, Wozniak DF, Yamada KA (2003) An animal model of generalized nonconvulsive status epilepticus: immediate characteristics and long-term effects. Exp Neurol 183:87–99
Wang W, Lou Y, Li P et al (2008) Changes in learning and memory functions in rats with status epilepticus and generalized nonconvulsive status epilepticus. Nan Fang Yi Ke Da Xue Xue Bao 28:255–259
Kršek P, Mikulecká A, Druga R et al (2004) Long-term behavioral and morphological consequences of nonconvulsive status epilepticus in rats. Epilepsy Behav 5:180–191. https://doi.org/10.1016/j.yebeh.2003.11.032
Trinka E, Kälviäinen R (2017) 25 years of advances in the definition, classification and treatment of status epilepticus. Seizure 44:65–73. https://doi.org/10.1016/j.seizure.2016.11.001
Rami A, Niquet J, Konoplew A (2018) Early aberrant growth of mossy fibers after status epilepticus in the immature rat brain. Mol Neurobiol. https://doi.org/10.1007/s12035-018-1432-y
De Furtado MA, Braga GK, Oliveira JAC et al (2002) Behavioral, morphologic, and electroencephalographic evaluation of seizures induced by intrahippocampal microinjection of pilocarpine. Epilepsia 43:37–39. https://doi.org/10.1046/j.1528-1157.2002.043s2037.x
Sharma AK, Reams RY, Jordan WH et al (2007) Mesial temporal lobe epilepsy: pathogenesis, induced rodent models and lesions. Toxicol Pathol 35:984–999. https://doi.org/10.1080/01926230701748305
Upadhya D, Castro OW, Upadhya R, Shetty AK (2018) Prospects of cannabidiol for easing status epilepticus-induced epileptogenesis and related comorbidities. Mol Neurobiol 55:6956–6964. https://doi.org/10.1007/s12035-018-0898-y
Castro OW, Upadhya D, Kodali M, Shetty AK (2017) Resveratrol for easing status epilepticus induced brain injury, inflammation, epileptogenesis, and cognitive and memory dysfunction—are we there yet? Front Neurol 8:603. https://doi.org/10.3389/fneur.2017.00603
Van Liefferinge J, Massie A, Portelli J et al (2013) Are vesicular neurotransmitter transporters potential treatment targets for temporal lobe epilepsy? Front Cell Neurosci 7:139. https://doi.org/10.3389/fncel.2013.00139
Cavalheiro EA, Silva DF, Turski WA et al (1987) The susceptibility of rats to pilocarpine-induced seizures is age-dependent. Dev Brain Res 37:43–58. https://doi.org/10.1016/0165-3806(87)90227-6
Mishra V, Shuai B, Kodali M et al (2015) Resveratrol treatment after status epilepticus restrains neurodegeneration and abnormal neurogenesis with suppression of oxidative stress and inflammation. Sci Rep 5. https://doi.org/10.1038/srep17807
Hester MS, Hosford BE, Santos VR et al (2016) Impact of rapamycin on status epilepticus induced hippocampal pathology and weight gain. Exp Neurol 280:1–12. https://doi.org/10.1016/j.expneurol.2016.03.015
Danzer SC, He X, Loepke AW, McNamara JO (2009) Structural plasticity of dentate granule cell mossy fibers during the development of limbic epilepsy. Hippocampus 20. https://doi.org/10.1002/hipo.20589
VanLandingham KE, Lothman EW (1991) Self-sustaining limbic status epilepticus. II. Role of hippocampal commissures in metabolic responses. Neurology 41:1950–1957
Rodrigues MCA, Rossetti F, Foresti ML et al (2005) Correlation between shaking behaviors and seizure severity in five animal models of convulsive seizures. Epilepsy Behav 6:328–336. https://doi.org/10.1016/j.yebeh.2005.02.005
Leite JP, Garcia-Cairasco N, Cavalheiro EA (2002) New insights from the use of pilocarpine and kainate models. Epilepsy Res 50:93–103. https://doi.org/10.1016/S0920-1211(02)00072-4
Turski WA, Cavalheiro EA, Turski L, Kleinrok Z (1983) Intrahippocampal bethanechol in rats: behavioural, electroencephalographic and neuropathological correlates. Behav Brain Res 7:361–370. https://doi.org/10.1016/0166-4328(83)90026-8
W a T, E a C, Z a B et al (1984) Seizures produced by pilocarpine in mice: a behavioral, electroencephalographic and morphological analysis. Brain Res 321:237–253. https://doi.org/10.1016/0006-8993(84)90177-X
García-García L, Shiha AA, Fernández de la Rosa R et al (2017) Metyrapone prevents brain damage induced by status epilepticus in the rat lithium-pilocarpine model. Neuropharmacology 123:261–273. https://doi.org/10.1016/j.neuropharm.2017.05.007
Ding Y-S, Chen B-B, Glielmi C et al (2014) A pilot study in epilepsy patients using simultaneous PET/MR. Am J Nucl Med Mol Imaging 4:459–470
Wong CH, Bleasel A, Wen L et al (2010) The topography and significance of extratemporal hypometabolism in refractory mesial temporal lobe epilepsy examined by FDG-PET. Epilepsia 51:1365–1373. https://doi.org/10.1111/j.1528-1167.2010.02552.x
Lee EM, Park GY, Im KC et al (2012) Changes in glucose metabolism and metabolites during the epileptogenic process in the lithium-pilocarpine model of epilepsy. Epilepsia 53:860–869. https://doi.org/10.1111/j.1528-1167.2012.03432.x
Kumar A, Chugani HT (2013) The role of radionuclide imaging in epilepsy. Part 1: sporadic temporal and extratemporal lobe epilepsy. J Nucl Med Technol 45:14–21. https://doi.org/10.2967/jnumed.112.114397
Shiha AA, de Cristóbal J, Delgado M et al (2015) Subacute administration of fluoxetine prevents short-term brain hypometabolism and reduces brain damage markers induced by the lithium-pilocarpine model of epilepsy in rats. Brain Res Bull 111:36–47. https://doi.org/10.1016/j.brainresbull.2014.12.009
Guo Y, Gao F, Wang S et al (2009) In vivo mapping of temporospatial changes in glucose utilization in rat brain during epileptogenesis: an 18F-fluorodeoxyglucose–small animal positron emission tomography study. Neuroscience 162:972–979. https://doi.org/10.1016/j.neuroscience.2009.05.041
Goffin K, Van PW, Dupont P, Van LK (2009) Longitudinal microPET imaging of brain glucose metabolism in rat lithium–pilocarpine model of epilepsy. Exp Neurol 217:205–209. https://doi.org/10.1016/j.expneurol.2009.02.008
Farooque P, Hirsch L, Levy S et al (2017) Surgical outcome in adolescents with mesial temporal sclerosis: is it different? Epilepsy Behav 69:24–27. https://doi.org/10.1016/j.yebeh.2016.10.028
Fernández-Torre JL, Pascual J, Quirce R et al (2006) Permanent dysphasia after status epilepticus: long-term follow-up in an elderly patient. Epilepsy Behav 8:677–680. https://doi.org/10.1016/j.yebeh.2006.01.014
Jupp B, Williams J, Binns D et al (2012) Hypometabolism precedes limbic atrophy and spontaneous recurrent seizures in a rat model of TLE. Epilepsia 53:1233–1244. https://doi.org/10.1111/j.1528-1167.2012.03525.x
Chugani HT, Chugani DC (1999) Basic mechanisms of childhood epilepsies: studies with positron emission tomography. Adv Neurol 79:883–891
McDonald TS, Carrasco-Pozo C, Hodson MP et al (2017) Alterations in cytosolic and mitochondrial [U-13C]-glucose metabolism in a chronic epilepsy mouse model. eNeuro 4:ENEURO.0341-16.2017. https://doi.org/10.1523/ENEURO.0341-16.2017
Vielhaber S, Von Oertzen JH, Kudin AF et al (2003) Correlation of hippocampal glucose oxidation capacity and interictal FDG-PET in temporal lobe epilepsy. Epilepsia 44:193–199
Schauwecker PE (2012) The effects of glycemic control on seizures and seizure-induced excitotoxic cell death. BMC Neurosci 13:94. https://doi.org/10.1186/1471-2202-13-94
Lundgaard I, Li B, Xie L et al (2015) Direct neuronal glucose uptake heralds activity-dependent increases in cerebral metabolism. Nat Commun 6:6807. https://doi.org/10.1038/ncomms7807
Poppe R, Karbach U, Gambaryan S et al (1997) Expression of the Na+-D-glucose cotransporter SGLT1 in neurons. J Neurochem 69:84–94
Yu AS, B a H, Timbol G et al (2010) Functional expression of SGLTs in rat brain. Am J Phys Cell Phys 299:C1277–C1284. https://doi.org/10.1152/ajpcell.00296.2010
Yu AS, B a H, Timbol G et al (2013) Regional distribution of SGLT activity in rat brain in vivo. Am J Phys Cell Phys 304:C240–C247. https://doi.org/10.1152/ajpcell.00317.2012
Zhao Y, Fung C, Shin D et al (2010) Neuronal glucose transporter isoform 3 deficient mice demonstrate features of autism spectrum disorders. Mol Psychiatry 15:286–299. https://doi.org/10.1038/mp.2009.51
Maher F, Davies-Hill TM, Simpson IA (1996) Substrate specificity and kinetic parameters of GLUT3 in rat cerebellar granule neurons. Biochem J 315(Pt 3):827–831
Mantych GJ, James DE, Chung HD, Devaskar SU (1992) Cellular localization and characterization of Glut 3 glucose transporter isoform in human brain. Endocrinology 131:1270–1278. https://doi.org/10.1210/endo.131.3.1505464
Devaskar S, Zahm DS, Holtzclaw L et al (1991) Developmental regulation of the distribution of rat brain insulin-insensitive (Glut 1) glucose transporter. Endocrinology 129:1530–1540. https://doi.org/10.1210/endo-129-3-1530
Dakic T, Jevdjovic T, Lakic I et al (2018) Food for thought: short-term fasting upregulates glucose transporters in neurons and endothelial cells, but not in astrocytes. Neurochem Res. https://doi.org/10.1007/s11064-018-2685-6
Simpson IA, Carruthers A, Vannucci SJ (2007) Supply and demand in cerebral energy metabolism: the role of nutrient transporters. J Cereb Blood Flow Metab 27:1766–1791. https://doi.org/10.1038/sj.jcbfm.9600521
Simpson IA, Dwyer D, Malide D et al (2008) The facilitative glucose transporter GLUT3: 20 years of distinction. Am J Physiol Metab 295:E242–E253. https://doi.org/10.1152/ajpendo.90388.2008
Maher F, Davies-Hill TM, Lysko PG et al (1991) Expression of two glucose transporters, GLUT1 and GLUT3, in cultured cerebellar neurons: evidence for neuron-specific expression of GLUT3. Mol Cell Neurosci 2:351–360. https://doi.org/10.1016/1044-7431(91)90066-W
Magistretti PJ, Allaman I (2015) A cellular perspective on brain energy metabolism and functional imaging. Neuron 86:883–901. https://doi.org/10.1016/j.neuron.2015.03.035
Allaman I, Magistretti PJ (2013) Brain energy metabolism. In: Fundamental neuroscience. Elsevier, pp. 261–284
Logothetis NK, Pauls J, Augath M et al (2001) Neurophysiological investigation of the basis of the fMRI signal. Nature 412:150–157. https://doi.org/10.1038/35084005
Raichle ME (1983) Positron emission tomography. Annu Rev Neurosci 6:249–267. https://doi.org/10.1146/annurev.ne.06.030183.001341
Magistretti PJ (2000) Cellular bases of functional brain imaging: insights from neuron-glia metabolic coupling 11. Published on the World Wide Web on 12 October 2000. Brain Res 886:108–112. https://doi.org/10.1016/S0006-8993(00)02945-0
Raichle ME (1998) Behind the scenes of functional brain imaging: a historical and physiological perspective. Proc Natl Acad Sci U S A 95:765–772
Frackowiak RS, Lenzi GL, Jones T, Heather JD (1980) Quantitative measurement of regional cerebral blood flow and oxygen metabolism in man using 15O and positron emission tomography: theory, procedure, and normal values. J Comput Assist Tomogr 4:727–736
Phelps ME, Huang SC, Hoffman EJ et al (1979) Tomographic measurement of local cerebral glucose metabolic rate in humans with (F-18)2-fluoro-2-deoxy-D-glucose: validation of method. Ann Neurol 6:371–388. https://doi.org/10.1002/ana.410060502
Zhang L, Guo Y, Hu H et al (2015) FDG-PET and NeuN-GFAP immunohistochemistry of hippocampus at different phases of the pilocarpine model of temporal lobe epilepsy. Int J Med Sci 12:288–294. https://doi.org/10.7150/ijms.10527
Ogawa S, Tank DW, Menon R et al (1992) Intrinsic signal changes accompanying sensory stimulation: functional brain mapping with magnetic resonance imaging. Proc Natl Acad Sci U S A 89:5951–5955
Galeano P, Leal MC, Ferrari CC et al (2018) Chronic hippocampal expression of notch intracellular domain induces vascular thickening, reduces glucose availability, and exacerbates spatial memory deficits in a rat model of early alzheimer. Mol Neurobiol 55:8637–8650. https://doi.org/10.1007/s12035-018-1002-3
Liguori C, Ruffini R, Olivola E et al (2019) Cerebral glucose metabolism in idiopathic REM sleep behavior disorder is different from tau-related and α-synuclein-related neurodegenerative disorders: a brain [18F]FDG PET study. Parkinsonism Relat Disord 64:97. https://doi.org/10.1016/j.parkreldis.2019.03.017
Piquet J, Toussay X, Hepp R et al (2018) Supragranular pyramidal cells exhibit early metabolic alterations in the 3xTg-AD mouse model of Alzheimer’s disease. Front Cell Neurosci 12:216. https://doi.org/10.3389/fncel.2018.00216
Kang H, Jo A, Kim H et al (2018) PARIS reprograms glucose metabolism by HIF-1α induction in dopaminergic neurodegeneration. Biochem Biophys Res Commun 495:2498–2504. https://doi.org/10.1016/j.bbrc.2017.12.147
Contreras CM, Gutiérrez-García AG (2017) Cognitive impairment in diabetes and poor glucose utilization in the intracellular neural milieu. Med Hypotheses 104:160–165. https://doi.org/10.1016/j.mehy.2017.06.007
Bathina S, Das UN (2018) Dysregulation of PI3K-Akt-mTOR pathway in brain of streptozotocin-induced type 2 diabetes mellitus in Wistar rats. Lipids Health Dis 17:168. https://doi.org/10.1186/s12944-018-0809-2
Franck G, Sadzot B, Salmon E et al (1986) Regional cerebral blood flow and metabolic rates in human focal epilepsy and status epilepticus. Adv Neurol 44:935–948
Van Bogaert P, Goldman S, Rodesch G et al (1994) Cerebral lesions following convulsive partial status epilepticus. Clinical, neuroradiologic and PET study of a case. J Neuroradiol 21:176–180
Kim HY, Kim JY, un KG et al (2012) Alien hand syndrome after epilepsia partialis continua: FDG PET and MRI studies. Epilepsy Behav 23:71–73. https://doi.org/10.1016/j.yebeh.2011.08.043
Sakakibara E, Takahashi Y, Murata Y et al (2014) Chronic periodic lateralised epileptic discharges and anti-N-methyl-D-aspartate receptor antibodies. 16:218–222. https://doi.org/10.1684/epd.2014.0655
Wasterlain CG, Fujikawa DG, Penix L et al (1993) Pathophysiological mechanisms of brain damage from status epilepticus. Epilepsia 34:S37–S53. https://doi.org/10.1111/j.1528-1157.1993.tb05905.x
Duane DC, Ng Y, Rekate HL et al (2004) Treatment of refractory status epilepticus with hemispherectomy. Epilepsia 45:1001–1004. https://doi.org/10.1111/j.0013-9580.2004.60303.x
Barros P, Brito H, Ferreira PC et al (2014) Resective surgery in the treatment of super-refractory partial status epilepticus secondary to NMDAR antibody encephalitis. Eur J Paediatr Neurol 18:449–452. https://doi.org/10.1016/j.ejpn.2014.01.013
Shimogori K, Doden T, Oguchi K, Hashimoto T (2017) Thalamic and cerebellar hypermetabolism and cortical hypometabolism during absence status epilepticus. BMJ Case Rep 2017. https://doi.org/10.1136/bcr-2017-220139
García-García L, Shiha AA, Bascuñana P et al (2016) Serotonin depletion does not modify the short-term brain hypometabolism and hippocampal neurodegeneration induced by the lithium–pilocarpine model of status epilepticus in rats. Cell Mol Neurobiol 36:513–519. https://doi.org/10.1007/s10571-015-0240-4
Smeland OB, Hadera MG, McDonald TS et al (2013) Brain mitochondrial metabolic dysfunction and glutamate level reduction in the pilocarpine model of temporal lobe epilepsy in mice. J Cereb Blood Flow Metab 33:1090–1097. https://doi.org/10.1038/jcbfm.2013.54
Bascuñana P, Brackhan M, Leiter I et al (2018) Divergent metabolic substrate utilization in brain during epileptogenesis precedes chronic hypometabolism. J Cereb Blood Flow Metab 40:204. https://doi.org/10.1177/0271678X18809886
Zilberter Y, Zilberter M (2017) The vicious circle of hypometabolism in neurodegenerative diseases: ways and mechanisms of metabolic correction. J Neurosci Res 95:2217. https://doi.org/10.1002/jnr.24064
Falip M, Miró J, Carreño M et al (2014) Hypoglycemic seizures and epilepsy in type I diabetes mellitus. J Neurol Sci 346:307–309. https://doi.org/10.1016/j.jns.2014.08.024
Hyllienmark L, Maltez J, Dandenell A et al (2005) EEG abnormalities with and without relation to severe hypoglycaemia in adolescents with type 1 diabetes. Diabetologia 48:412–419. https://doi.org/10.1007/s00125-004-1666-2
Leckie AM, Graham MK, Grant JB et al (2005) Frequency, severity, and morbidity of hypoglycemia occurring in the workplace in people with insulin-treated diabetes. Diabetes Care 28:1333–1338
Chin RF, Neville BG, Peckham C et al (2006) Incidence, cause, and short-term outcome of convulsive status epilepticus in childhood: prospective population-based study. Lancet 368:222–229. https://doi.org/10.1016/S0140-6736(06)69043-0
Chapman AG, Engelsen B, Meldrum BS (1987) 2-Amino-7-phosphonoheptanoic acid inhibits insulin-induced convulsions and striatal aspartate accumulation in rats with frontal cortical ablation. J Neurochem 49:121–127
Moseley B, Bateman L, Millichap JJ et al (2013) Autonomic epileptic seizures, autonomic effects of seizures, and SUDEP. Epilepsy Behav 26:375–385. https://doi.org/10.1016/j.yebeh.2012.08.020
Maheandiran M, Mylvaganam S, Wu C et al (2013) Severe hypoglycemia in a juvenile diabetic rat model: presence and severity of seizures are associated with mortality. PLoS One 8:e83168. https://doi.org/10.1371/journal.pone.0083168
Verrotti A, Scaparrotta A, Olivieri C, Chiarelli F (2012) Mechanisms in endocrinology: Seizures and type 1 diabetes mellitus: current state of knowledge. Eur J Endocrinol 167:749–758. https://doi.org/10.1530/EJE-12-0699
McCall AL (2004) Cerebral glucose metabolism in diabetes mellitus. Eur J Pharmacol 490:147–158. https://doi.org/10.1016/j.ejphar.2004.02.052
Auer RN (2004) Hypoglycemic brain damage. Metab Brain Dis 19:169–175. https://doi.org/10.1023/B:MEBR.0000043967.78763.5B
Sapolsky RM, Stein BA (1989) Status epilepticus-induced hippocampal damage is modulated by glucose availability. Neurosci Lett 97:157–162
Hart SP, Frier BM (1998) Causes, management and morbidity of acute hypoglycaemia in adults requiring hospital admission. QJM 91:505–510
Limbert C, Schwingshandl J, Haas J et al (1993) Severe hypoglycemia in children and adolescents with IDDM: frequency and associated factors. J Diabetes Complicat 7:216–220
MacLeod KM, Hepburn DA, Frier BM (1993) Frequency and morbidity of severe hypoglycaemia in insulin-treated diabetic patients. Diabet Med 10:238–245
Malouf R, Brust JCM (1985) Hypoglycemia: causes, neurological manifestations, and outcome. Ann Neurol 17:421–430. https://doi.org/10.1002/ana.410170502
Davis EA, Keating B, Byrne GC et al (1997) Hypoglycemia: incidence and clinical predictors in a large population-based sample of children and adolescents with IDDM. Diabetes Care 20:22–25
Towne AR, Pellock JM, Ko D, DeLorenzo RJ (1994) Determinants of mortality in status epilepticus. Epilepsia 35:27–34
Neil WP, Hemmen TM (2011) Neurologic manifestations of hypoglycemia. Tech
Panickar KS, Purushotham K, King MA et al (1998) Hypoglycemia-induced seizures reduce cyclic AMP response element binding protein levels in the rat hippocampus. Neuroscience 83:1155–1160
Chou I-C, Wang C-H, Lin W-D et al (2016) Risk of epilepsy in type 1 diabetes mellitus: a population-based cohort study. Diabetologia 59:1196–1203. https://doi.org/10.1007/s00125-016-3929-0
Gataullina S, Delonlay P, Lemaire E et al (2015) Seizures and epilepsy in hypoglycaemia caused by inborn errors of metabolism. Dev Med Child Neurol 57:194–199. https://doi.org/10.1111/dmcn.12574
Cross JH (2015) Seizures associated with hypoglycaemia and subsequent epilepsy. Dev Med Child Neurol 57:117–118. https://doi.org/10.1111/dmcn.12595
Kumaran A, Kar S, Kapoor RR, Hussain K (2010) The clinical problem of hyperinsulinemic hypoglycemia and resultant infantile spasms. Pediatrics 126:e1231–e1236. https://doi.org/10.1542/peds.2009-2775
Fujikawa DG (1996) The temporal evolution of neuronal damage from pilocarpine-induced status epilepticus. Brain Res 725:11–22. https://doi.org/10.1016/S0006-8993(96)00203-X
O’Connell MA, Harvey AS, Mackay MT, Cameron FJ (2008) Does epilepsy occur more frequently in children with type 1 diabetes? J Paediatr Child Health 44:586–589. https://doi.org/10.1111/j.1440-1754.2008.01387.x
Xia L, Lei Z, Shi Z et al (2016) Enhanced autophagy signaling in diabetic rats with ischemia-induced seizures. Brain Res 1643:18–26. https://doi.org/10.1016/j.brainres.2016.04.054
Lavin PJM (2005) Hyperglycemic hemianopia: a reversible complication of non-ketotic hyperglycemia. Neurology 65:616–619. https://doi.org/10.1212/01.wnl.0000173064.80826.b8
Lee J-J, Jung J, Kang K et al (2014) Recurrent seizures following focal motor status epilepticus in a patient with non-ketotic hyperglycemia and acute cerebral infarction. J Epilepsy Res 4:28–30
Greene AE, Todorova MT, Seyfried TN (2003) Perspectives on the metabolic management of epilepsy through dietary reduction of glucose and elevation of ketone bodies. J Neurochem 86:529–537
Huang EJ, Reichardt LF (2001) NEUROTROPHINS: roles in neuronal development and function. Annu Rev Neurosci 24:677–736. https://doi.org/10.1146/annurev.neuro.24.1.677
Rathakrishnan R, Sidik NP, Huak CY et al (2009) Generalised convulsive status epilepticus in Singapore: clinical outcomes and potential prognostic markers. Seizure 18:202–205. https://doi.org/10.1016/j.seizure.2008.09.005
Toledo M, Purroy F, Río J, Rovira A (2005) Epileptic status due to non-ketotic hyperglycemia. Med Clin (Barc) 124:398–399
Li C, Li P-A, He Q-P et al (1998) Effects of Streptozotocin-Induced Hyperglycemia on Brain Damage Following Transient Ischemia. Neurobiol Dis 5:117–128. https://doi.org/10.1006/nbdi.1998.0189
Santiago JFC, Carvalho FF, Perosa SR et al (2006) Effect of glycemic state in rats submitted to status epilepticus during development. Arq Neuropsiquiatr 64:233–239. https://doi.org/10.1590/S0004-282X2006000200012
Magariños AM, McEwen BS (2000) Experimental diabetes in rats causes hippocampal dendritic and synaptic reorganization and increased glucocorticoid reactivity to stress. Proc Natl Acad Sci U S A 97:11056–11061
Sokoloff L (1981) Relationships among local functional activity, energy metabolism, and blood flow in the central nervous system. Fed Proc 40:2311–2316
Young JK, Chung W (1990) Glucose transporter immunoreactivity in the hypothalamus and area postrema. Brain Res Bull 24:525–528. https://doi.org/10.1016/0361-9230(90)90106-A
Zeller K, Vogel J, Kuschinsky W (1996) Postnatal distribution of Glut1 glucose transporter and relative capillary density in blood-brain barrier structures and circumventricular organs during development. Brain Res Dev Brain Res 91:200–208
Rahner-Welsch S, Vogel J, Kuschinsky W (1995) Regional congruence and divergence of glucose transporters (GLUT1) and capillaries in rat brains. J Cereb Blood Flow Metab 15:681–686. https://doi.org/10.1038/jcbfm.1995.84
Sabino-Silva R, Mori RC, David-Silva a et al (2010) The Na +-/glucose cotransporters: from genes to therapy. Braz J Med Biol Res 43:1019–1026. https://doi.org/10.1590/S0100-879X2010007500115
McEwen BS, Reagan LP (2004) Glucose transporter expression in the central nervous system: relationship to synaptic function. Eur J Pharmacol 490:13–24. https://doi.org/10.1016/j.ejphar.2004.02.041
Levin BE, Dunn-Meynell AA, Routh VH (2001) Brain glucosensing and the K(ATP) channel. Nat Neurosci 4:459–460. https://doi.org/10.1038/87405
Jurcovicova J (2014) Glucose transport in brain - effect of inflammation. Endocr Regul 48:35–48. https://doi.org/10.4149/endo_2014_01_35
Duelli R, Kuschinsky W (2001) Brain glucose transporters: relationship to local energy demand. News Physiol Sci 16:71–76. https://doi.org/10.1152/physiologyonline.2001.16.2.71
Duelli R, Staudt R, Duembgen L, Kuschinsky W (1999) Increase in glucose transporter densities of Glut3 and decrease of glucose utilization in rat brain after one week of hypoglycemia. Brain Res 831:254–262. https://doi.org/10.1016/S0006-8993(99)01463-8
Uehara Y, Nipper V, McCall AL (1997) Chronic insulin hypoglycemia induces GLUT-3 protein in rat brain neurons. Am J Physiol Endocrinol Metab 272. https://doi.org/10.1152/ajpendo.1997.272.4.e716
Pitchaimani V, Arumugam S, Thandavarayan RA et al (2020) Brain adaptations of insulin signaling kinases, GLUT 3, p-BADser155 and nitrotyrosine expression in various hypoglycemic models of mice. Neurochem Int 137. https://doi.org/10.1016/j.neuint.2020.104745
McGowan JE, Haynes-Laing AG, Mishra OP, Delivoria-Papadopoulos M (1995) The effect of acute hypoglycemia on the cerebral NMDA receptor in newborn piglets. Brain Res 670:283–288. https://doi.org/10.1016/0006-8993(94)01289-T
Ferreira JM, Burnett AL, Rameau GA (2011) Activity-dependent regulation of surface glucose transporter-3. J Neurosci 31:1991–1999. https://doi.org/10.1523/JNEUROSCI.1850-09.2011
Litvin M, Clark AL, Fisher SJ (2013) Recurrent hypoglycemia: bthe brain’s metabolic flexibility. J Clin Invest 123:1922–1924
Duelli R, Maurer MH, Staudt R et al (2000) Increased cerebral glucose utilization and decreased glucose transporter Glut1 during chronic hyperglycemia in rat brain. Brain Res 858:338–347. https://doi.org/10.1016/S0006-8993(00)01942-9
Pardridge WM, Triguero D, Farrell CR (1990) Downregulation of blood-brain barrier glucose transporter in experimental diabetes. Diabetes 39:1040–1044. https://doi.org/10.2337/diab.39.9.1040
Klepper J, Leiendecker B (2007) GLUT1 deficiency syndrome - 2007 update. Dev Med Child Neurol 49:707–716. https://doi.org/10.1111/j.1469-8749.2007.00707.x
Gras D, Roze E, Caillet S et al (2014) GLUT1 deficiency syndrome: An update. Rev Neurol (Paris) 170:91–99. https://doi.org/10.1016/j.neurol.2013.09.005
Kim H, Lee JS, Lee Y et al (2019) Diagnostic challenges associated with GLUT1 deficiency: Phenotypic variabilities and evolving clinical features. Yonsei Med J 60:1209–1215. https://doi.org/10.3349/ymj.2019.60.12.1209
de Vivo DC, Trifiletti RR, Jacobson RI et al (1991) Defective glucose transport across the blood-brain barrier as a cause of persistent hypoglycorrhachia, seizures, and developmental delay. N Engl J Med 325:703–709. https://doi.org/10.1056/NEJM199109053251006
Koch H, Weber YG (2019) The glucose transporter type 1 (Glut1) syndromes. Epilepsy Behav 91:90–93. https://doi.org/10.1016/j.yebeh.2018.06.010
Furuse T, Mizuma H, Hirose Y et al (2019) A new mouse model of GLUT1 deficiency syndrome exhibits abnormal sleep-wake patterns and alterations of glucose kinetics in the brain. Dis Model Mech 12:dmm038828. https://doi.org/10.1242/dmm.038828
Tchapyjnikov D, Mikati MA (2018) Acetazolamide-responsive episodic ataxia without baseline deficits or seizures secondary to GLUT1 deficiency: a case report and review of the literature. Neurologist 23:17–18
Ismayilova N, Hacohen Y, MacKinnon AD et al (2018) GLUT-1 deficiency presenting with seizures and reversible leukoencephalopathy on MRI imaging. Eur J Paediatr Neurol 22:1161–1164. https://doi.org/10.1016/j.ejpn.2018.02.002
Pascual JM, Wang D, Hinton V et al (2007) Brain glucose supply and the syndrome of infantile neuroglycopenia. Arch Neurol 64:507. https://doi.org/10.1001/archneur.64.4.noc60165
Marin-Valencia I, Good LB, Ma Q et al (2012) Glut1 deficiency (G1D): Epilepsy and metabolic dysfunction in a mouse model of the most common human phenotype. Neurobiol Dis 48:92–101. https://doi.org/10.1016/j.nbd.2012.04.011
Sandu C, Burloiu CM, Barca DG et al (2019) Ketogenic diet in patients with GLUT1 deficiency syndrome. Maedica (Buchar) 14, 93. https://doi.org/10.26574/maedica.2019.14.2.93
Ji XN, Xu CJ, Gao ZJ et al (2018) Glucose transporter 1 deficiency syndrome: Features of movement disorders, diagnosis and treatment. Chinese J Contemp Pediatr 20:209–213. https://doi.org/10.7499/j.issn.1008-8830.2018.03.009
Bekker YAC, Lambrechts DA, Verhoeven JS et al (2019) Failure of ketogenic diet therapy in GLUT1 deficiency syndrome. Eur J Paediatr Neurol 23:404–409. https://doi.org/10.1016/j.ejpn.2019.02.012
Akman CI, Engelstad K, Hinton VJ et al (2010) Acute hyperglycemia produces transient improvement in glucose transporter type 1 deficiency. Ann Neurol 67:31–40. https://doi.org/10.1002/ana.21797
Wright E, Loo D, Hirayama B (2011) Biology of human sodium glucose transporters. Physiol Rev 91:733–794. https://doi.org/10.1152/physrev.00055.2009
Wright EM, Turk E (2004) The sodium/glucose cotransport family SLC5. Pflugers Arch - Eur J Physiol 447:510–518. https://doi.org/10.1007/s00424-003-1063-6
Zeuthen T (2000) Molecular water pumps. Rev Physiol Biochem Pharmacol 141:97–151
Takata K, Kasahara T (1992) Cell & Tissue immunohistochemical localization of Na + -dependent glucose transporter in rat jejunum. 3–9
Balen D, Ljubojevic M, Breljak D et al (2008) Revised immunolocalization of the Na+-D-glucose cotransporter SGLT1 in rat organs with an improved antibody. Am J Phys Cell Phys 295:C475–C489. https://doi.org/10.1152/ajpcell.00180.2008
Zhao F-Q, Keating AF (2007) Functional properties and genomics of glucose transporters. Curr Genomics 8:113–128
Racine RJ (1972) Modification of seizure activity by electrical stimulation. II. Motor seizure. Electroencephalogr Clin Neurophysiol 32:281–294
Do Nascimento AL, Dos Santos NF, Campos Pelágio F et al (2012) Neuronal degeneration and gliosis time-course in the mouse hippocampal formation after pilocarpine-induced status epilepticus. Brain Res 1470:98–110. https://doi.org/10.1016/j.brainres.2012.06.008
Ren X, Zhou L, Terwilliger R et al (2009) Sweet taste signaling functions as a hypothalamic glucose sensor. Front Integr Neurosci 3:12. https://doi.org/10.3389/neuro.07.012.2009
Dyer J, Vayro S, King TP et al (2003) Glucose sensing in the intestinal epithelium. Eur J Biochem 270:3377–3388
Funding
DLGG was supported by the Research Productivity Scholarship Program in Brazilian National Council for Scientific and Technological Development (CNPq). We thank CAPES-Brazil for PhD Research Fellowship to ISM, YMOS, ALDP, and LCS. Sabino-Silva, R received a fellowship from PrInt CAPES/UFU. This project was supported by FAPEAL, FAPEMIG (APQ-02872-16), and National Institute of Science and Technology in Theranostics and Nanobiotechnology - INCT-Teranano (CNPq-465669/2014-0).
Author information
Authors and Affiliations
Contributions
ISM, RSS, and OWC conceived the original idea and designed the outlines of the study. ISS, ALDP, YMOS, LMF, and DCSPN wrote the draft of the manuscript. ISS, ALDP, and OWC prepared the figures for the manuscript. ISS, LCS, MD, DLGG, CQT, RSS, and OWC performed the literature review and aided in revising the manuscript. All authors have read and agreed to the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Melo, I.S., Pacheco, A.L.D., dos Santos, Y.M.O. et al. Modulation of Glucose Availability and Effects of Hypo- and Hyperglycemia on Status Epilepticus: What We Do Not Know Yet?. Mol Neurobiol 58, 505–519 (2021). https://doi.org/10.1007/s12035-020-02133-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-020-02133-8