Abstract
Background
Prolonged external ventricular drainage (EVD) in patients with subarachnoid hemorrhage (SAH) leads to morbidity, whereas early removal can have untoward effects related to recurrent hydrocephalus. A metric to help determine the optimal time for EVD removal or ventriculoperitoneal shunt (VPS) placement would be beneficial in preventing the prolonged, unnecessary use of EVD. This study aimed to identify whether dynamics of cerebrospinal fluid (CSF) biometrics can temporally predict VPS dependency after SAH.
Methods
This was a retrospective analysis of a prospective, single-center, observational study of patients with aneurysmal SAH who required EVD placement for hydrocephalus. Patients were divided into VPS-dependent (VPS+) and non–VPS dependent groups. We measured the bicaudate index (BCI) on all available computed tomography scans and calculated the change over time (ΔBCI). We analyzed the relationship of ΔBCI with CSF output by using Pearson’s correlation. A k-nearest neighbor model of the relationship between ΔBCI and CSF output was computed to classify VPS.
Results
Fifty-eight patients met inclusion criteria. CSF output was significantly higher in the VPS+ group in the 7 days post EVD placement. There was a negative correlation between delta BCI and CSF output in the VPS+ group (negative delta BCI means ventricles become smaller) and a positive correlation in the VPS- group starting from days four to six after EVD placement (p < 0.05). A weighted k-nearest neighbor model for classification had a sensitivity of 0.75, a specificity of 0.70, and an area under the receiver operating characteristic curve of 0.80.
Conclusions
The correlation of ΔBCI and CSF output is a reliable intraindividual biometric for VPS dependency after SAH as early as days four to six after EVD placement. Our machine learning model leverages this relationship between ΔBCI and cumulative CSF output to predict VPS dependency. Early knowledge of VPS dependency could be studied to reduce EVD duration in many centers (intensive care unit length of stay).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute hydrocephalus is a known complication of subarachnoid hemorrhage (SAH), with an incidence of 15–87% [1,2,3,4]. Acute hydrocephalus requires the placement of an external ventricular drain (EVD), but the disturbance of cerebrospinal fluid (CSF) hydrodynamics persists in almost half (45%) of these patients requiring a ventriculoperitoneal shunt (VPS) [5,6,7]. The optimal management of EVD in the setting of SAH remains controversial. Prolonged use of EVD is associated with complications and worse functional outcomes, and premature removal of EVD might put the patients at risk of recurrent hydrocephalus with adverse consequences for recovery from SAH [8,9,10,11,12]. There are conflicting recommendations in the literature regarding the optimal timing and method of EVD weaning [4, 13,14,15]. Early recognition of VPS dependency or EVD liberation may prevent prolonged EVD duration and complications while expediting transfer out of the intensive care unit in many centers.
Several studies have identified risk factors associated with VPS dependency; few have created classifiers to support individual prediction, and none have used time-varying measurements. The examined risk factors include high Hunt and Hess scale, low Glasgow Coma Scale score at presentation, high Graeb and LeRoux score, high Fisher grade, older age (≥60 years of age), computed tomography (CT) findings (hemorrhage, third ventricle diameter, bicaudate index), posterior circulation aneurysm, aneurysm treatment modality (surgical clipping vs. endovascular coiling), and CSF output [1, 12, 16,17,18,19,20,21,22]. All these risk factors were assessed once at the onset of SAH (CSF output was evaluated immediately after EVD placement). Bicaudate index (BCI), defined as the ratio of the distance encompassing the lateral ventricles and the distance between the inner tables of the skull at the level of the caudate nucleus [23], has been assessed as a risk factor either at the onset of SAH [1, 3, 24] or right before VPS placement [2].
We hypothesized that time-varying features related to CSF hydrodynamics could accurately identify VPS dependence by using a machine learning statistical classification model. Among known risk factors for VPS, the BCI and CSF output offer dynamic or time-varying information, as opposed to static clinical scales and aneurysm characteristics.
Methods
Study Population
We studied consecutive patients with aneurysmal SAH who had an EVD placed and who were admitted to the neurological intensive care unit. They were enrolled in a prospective observational study of SAH outcomes. Consent was obtained from the patient or a surrogate. The medical center’s institutional review board approved the study. This was a retrospective analysis of the prospective observational study.
Patients were divided into two groups: the VPS-dependent group (VPS+) and the non–VPS dependent group (VPS−). They were the patients who required or did not require a VPS placement prior to hospital discharge, respectively. We collected data on demographics, neuroimaging, Hunt and Hess grades, Fisher scale [3, 17, 25], CSF output, EVD, and VPS placement date. Exclusion criteria were patients who died in the hospital, as VPS planning would not be relevant. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology reporting guidelines.
EVD Management and Weaning Practices
In our institution, EVDs are placed for the treatment of symptomatic hydrocephalus and kept open at 20 cm H2O until the aneurysm is secured. After aneurysm securement, the EVD is set open to drain continuously at 10 cm H2O during the vasospasm window. EVD weaning trials are started after the vasospasm window and whether the patient has a good neurological examination to follow. Weaning trials include raising the EVD by increments of 5 cm H2O daily, and then clamping after reaching 20 cm H2O for 24 hours. The clamp trial is aborted if there are adverse clinical changes (headache, vomiting, or deterioration of consciousness level), intracranial pressure elevations exceeding 20 mm Hg for more than 20 minutes, or CSF leakage. At the end of the clamp trial, if there is radiographic evidence of hydrocephalus, this is also considered a failed clamp trial. Patients are considered candidates for VPS placement after failing two clamp trials. Ventriculitis can delay VPS placement until CSF profiles are adequately normalized with antibiotic treatment.
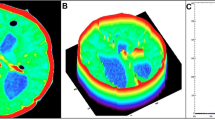
Neuroimaging and CSF Data
We measured BCIs in all available CT studies during the patient’s hospital stay. Readers were blinded to demographic data, clinical baseline, CSF output, and VPS outcome. The BCI was calculated by using a linear measure of the width of the frontal horns where the heads of the caudate nuclei produced the maximum indentation of the lateral ventricle, divided by the corresponding distance between the inner tables of the skull at this level [23]. The measurement was obtained at the CT section that included the foramen of Monro. When the foramen of Monro was not clearly seen, the measure was made in two adjacent CT sections, and the mean value of the BCI was used. All readers (CR, KT, BW, LC, JF, RR, HK, and AA) participated in group and individual training sessions for BCI measurements. The training materials contained radiological neuroanatomy imaging and examples of BCI measurements. Adequate time was allocated to each reader to understand the interpretative and measurement process fully. Readers had the training materials available later in the active phase of the study. To evaluate the reader’s agreement, readers were paired. Two authors measured the BCI in ten CT scans together; afterward, they separately measured BCI in an additional 20 CT scans and crosschecked their results.
Delta BCI were calculated by subtracting the BCI value of the first CT scan (after EVD placement) from the BCI value of subsequent candidate CTs. CSF output data was available from nursing flowsheets in 2 hour intervals. Cumulative CSF volumes (in mL) were calculated to correspond to the timing of each CT scan (starting from and accumulating since the time of the first post-EVD scan). Delta BCIs and corresponding cumulative CSF outputs were calculated for seven consecutive days after EVD placement. For example, on day 4 after EVD placement, delta BCI would equal day 4 BCI (if CT available) minus BCI of the first post-EVD CT, and the corresponding CSF output would be cumulative between the times of those two scans.
Statistical Analysis
Pearson correlation coefficients were calculated between BCI and cumulative CSF output and between ΔBCI and cumulative CSF output for each day. A p value <0.05 was considered statistically significant. Figures 1 and 2 demonstrate Fisher’s Z-transformation that was performed between the correlation values of VPS+ group and VPS− group for each day from days one to seven after EVD placement.
Correlation coefficient between ΔBCI and CSF output. Horizontal lines are lines of best fit on the basis of the Pearson correlation coefficient on days one to seven (a to g, respectively) and change in correlation over the period of 7 days (h). BCI, bicaudate index, CSF, cerebrospinal fluid, VP, ventriculoperitoneal.
Correlation coefficient between average BCI and CSF output. Horizontal lines are lines of best fit based on Pearson correlation coefficient on days one to seven (a to g, respectively) and change in correlation over the period of 7 days (h). BCI, bicaudate index, CSF, cerebrospinal fluid, VP, ventriculoperitoneal.
Weighted k-nearest neighbor (KNN) [26] was applied to compute a classification model for VPS dependency. KNN is an algorithm that classifies an object by a majority vote on the basis of the k number of neighbors from the feature map, in which k is an integer. KNN is a Lazy Learner (meaning that it does not require training) and works well with smaller data sets. Weighted KNN is a type of KNN, but it gives a different weight on each neighbor according to its distance. A neighbor with a closer distance has a higher weight compared with a neighbor with more space away from the data point.
Two models were generated on the basis of ΔBCI or daily BCI. Other features that were used as inputs were cumulative CSF output, age, Hunt and Hess score, Fisher Score, and sex. A tenfold cross-validation method was used to evaluate the models. The whole data set was divided randomly into ten different subsamples; nine subsamples were used to train the model, and the remaining subsample was used for validation. This process was repeated ten times, using a different subsample for validation each time. The models were further examined by using the area under the receiver operating characteristic curve (AUC).
All data analysis was performed by using MATLAB 2020a (MathWorks, MA) and Microsoft Excel 2010 (Microsoft, Redmond, WA).
Results
A total of 119 consecutive patients with SAH with EVD placement who were admitted between April 2006 and September 2014 were included. Sixty-one patients were removed on the basis of the following criteria: missing CSF output data (n = 41), patients who died in the hospital (n = 13), patients without ΔBCI value after EVD placement (n = 7) (Supplemental Digital Content Fig. 1). The study was undertaken during a transition between electronic medical record systems, and some flowsheets and images were no longer accessible. There was no significant difference in age, sex, clinical SAH presentation severity, and Fisher score between the two groups (Table 1). CSF output was significantly higher in the VPS+ than the VPS− group over the 7 days after EVD placement (p= 0.008) (Table 1). The average overall EVD duration was 11.8 ± 4.7 days (range 3.5–24.3). The EVD duration in the VPS+ group was 12.8 ± 6 days and 8.6 ± 4.7 days in the VPS− group (p = 0.003). The rate of ventriculitis in the VPS+ group was 7 (23.3%), and the rate in the VPS− group was 5 (17.9%; p = 0.749). There was no difference in the mean BCI and ΔBCI between the two groups (Fig. 3).
Delta BCI and CSF output negatively correlated in the VPS(+) groups on days two to seven after EVD placement (Figure 1). (Delta DCI is negative when ventricles become smaller from post-EVD CT to subsequent CT). In contrast, there was a positive correlation between delta BCI and CSF output in the VPS(-) group. (Figure 1) The correlation of delta BCI and CSF output was statistically significantly different between VPS(+) and VPS(-) from days four to six. (Table 2) There was no significant difference between groups in the correlations between mean daily BCI and CSF output. (Figure 2)
The classification accuracy of predicting VPS dependency with the ΔBCI model was 0.72, with a sensitivity of 0.75, a specificity of 0.70, and an AUC of 0.80 (Fig. 4). The result of mean daily BCI model was 0.64, 0.68, and 0.60, respectively, for accuracy, sensitivity, and specificity, with an AUC of 0.63 (Fig. 4). The specificity and sensitivity are reported at an optimal threshold of 0.53 for the ΔBCI model (and 0.44 for the mean BCI model), corresponding to the maximum Youden index [27].
Weighted KNN analysis. Showing receiver operating characteristic curve for ventriculoperitoneal shunt dependency based on A) average BCI model, B) delta BCI model, and confusion matrices for C) average BCI model and D) delta BCI model. Other features that were used as inputs were cumulative CSF output, age, Hunt and Hess score, Fisher score, and gender. BCI=bicaudate index.; KNN=k-nearest neighbor; VPS=ventriculoperitoneal shunt.
Discussion
Our study showed that the intra-individual correlation between decreasing BCI and increasing CSF output on days four to six after EVD placement is associated with VPS dependency in patients with SAH. Our model showed that we can leverage this correlation as a feature to classify or predict patients who will need VPS with moderately good accuracy (AUC 0.8). The negative correlation of delta BCI and CSF output in the VPS dependent group suggests a ventricular system which, unaided, can not independently accommodate for either high resistance to CSF outflow or CSF overproduction requiring a drain or shunt to release the pressure. The positive correlation of delta BCI and CSF output in the VPS- group suggests an appropriately accommodating ventricular system.
Several risk factors have been used in prior models, such as patient baseline characteristics (age and sex) [7, 17, 25], SAH severity [28, 29], aneurysm location [20, 21], laboratory studies [30], aneurysm treatment modality [25, 31, 32], EVD weaning [33,34,35], EVD drainage volume [12, 36,37,38,39,40], and course of disease [3, 17, 25], but no time-varying biometrics have yet been used. For example, although BCI has been validated as an objective measurement of hydrocephalus, all studies looking for an association of BCI with VPS dependency have used the BCI at a single point during the hospitalization. Two studies measured BCI in the admission CT scan and showed that VPS was required in patients with a BCI greater than 0.2 [3, 24]. An older study used the measured BCI at the time of shunting. In that study, BCI was stratified by the patients’ normal upper age limit and divided the patients into three relative BCI groups. They found that patients with higher relative BCI values were associated with VPS placement [2]. To our knowledge, our study is the first study to incorporate BCI at multiple time points into a model for VPS dependency, and notably it outperformed a model using single measurements of BCI.
CSF output alone has also been studied as a predictor of VPS dependency [12, 36,37,38,39,40], but although some have suggested an important threshold (>214 mL/day in first 72 hours [38], >204 mL/day [12], >201 mL/day [40]), others have found a lower threshold (>130 mL/day) [37] that directly contradicts important thresholds for VPS− prediction (<162 mL/day) [40]. Moreover, some studies did not even find an association between the CSF output and VPS dependency after SAH [36].
Existing scoring systems, such as the CHESS [41], SDASH [28], PS3 [29], and CARAS [42], use variables present at the time the patient presents with acute hydrocephalus requiring EVD placement, but these are unable to give time-varying knowledge of shunt dependency (or ability to wean from EVD) or have an AUC that is comparable with our model. The recent MAGE [12] score also included mean daily CSF output, but the model’s AUC was only 0.6. There is wide diversity among these scores’ prognostic factors [1, 7, 28, 29, 41,42,43], their variable accuracy in their predictions [44], and their applicability in modern practice [45].
We relate CSF output with the change in ventricle size over time, which could be considered a biometric informed by intracranial compliance and resistance to CSF outflow. The correlation of decreasing hydrocephalus and CSF output suggests a ventricular system that, unaided, cannot independently accommodate for either high resistance to CSF outflow or CSF overproduction. Our model incorporates dynamism or change over time in ventricular size in relation to CSF drainage and improves upon a model using standalone BCI values. Our model may serve as a tool for early estimation of shunt dependency and recognition of patients requiring relative pressures to drive flow through CSF efflux pathways to decrease EVD placement days and associated complications. Our study is a positive step toward the development of objective and reproducible dynamic parameters that can help identify patients that will become VPS dependent.
There are limitations to our study. First, this study had a small sample size (n = 58), limiting the complexity of the model that we can derive. Although the classification performance is good, it does not achieve a level of sensitivity and specificity to be clinically useful yet. We seek to increase the sample size for enhanced model development. Further, the model results depend on the BCI, which requires (albeit minimal effort from) skilled individuals. The automatic calculation of BCI would make our methodology even more feasible. Additionally, our model doesn’t include an EVD level relative to the tragus, which might be a confounder in our study. Although the practice of keeping the EVD level at 10 cm H2O above the tragus during the vasospasm window is standard at our institution, we cannot exclude the possibility that the rare instance of an EVD being set unusually low or high could introduce bias by the changes in CSF output in relation to the EVD setting. This should be data that will be included in future validation of this model.
Conclusions
Our study suggests that using validated, objective, and reproducible biometrics of CSF hydrodynamics, CSF output, and ΔBCI can help physicians recognize patients destined for VPS dependency or patients with the ability for EVD to be weaned in a timely way. The model showed moderate accuracy (comparable performance with other well-known scoring systems). Future studies are needed to validate our findings.
Data availability
Data relating to the findings of this study are available from the corresponding author on reasonable request.
References
Chan M, Alaraj A, Calderon M, et al. Prediction of ventriculoperitoneal shunt dependency in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg. 2009;110(1):44–9.
Little AS, Zabramski JM, Peterson M, et al. Ventriculoperitoneal shunting after aneurysmal subarachnoid hemorrhage: analysis of the indications, complications, and outcome with a focus on patients with borderline ventriculomegaly. Neurosurgery. 2008;62(3):618–26.
Rincon F, Gordon E, Starke RM, et al. Predictors of long-term shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage: clinical article. J Neurosurg. 2010;113(4):774–80.
Connolly ES, Rabinstein AA, Chair V, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage. A guideline for healthcare professonals from the American Heart Association/American Stroke Association. Stroke. 2012;43:1711–37.
O’Kelly CJ, Kulkarni AV, Austin PC, et al. Shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage: incidence, predictors, and revision rates. J Neurosurg. 2009;111(5):1029–35.
Varelas P, Helms A, Sinson G, et al. Clipping or coiling of ruptured cerebral aneurysms and shunt-dependent hydrocephalus. Neurocrit Care. 2006;4(3):223–8.
Adams H, Ban VS, Leinonen V, et al. Risk of shunting after aneurysmal subarachnoid hemorrhage a collaborative study and initiaiont of a consortioum. Stroke. 2016;47(10):2488–96.
Graff-Radford N, Torner J, Adams H, Kassell N. Factors associated with hydrocephalus after subarachnoid hemorrhage. A report of the Cooperative Aneurysm Study. Arch Neurol. 1989;46(7):744–52.
Hütter B, Kreitschmann-Andermahr I, Gilsbach J. Cognitive deficits in the acute stage after subarachnoid hemorrhage. Neurosurgery. 1998;43(5):1054–64.
Milhorat T. Acute hydrocephalus after aneurysmal subarachnoid hemorrhage. Neurosurgery. 1987;20(1):15–20.
Sheehan J, Polin R, Sheehan J, et al. Factors associated with hydrocephalus after aneurysmal subarachnoid hemorrhage. Neurosurgery. 1999;45(5):1120–8.
Perry A, Graffeo CS, Kleinstern G, et al. Quantitative modeling of external ventricular drain output to predict shunt dependency in aneurysmal subarachnoid hemorrhage: cohort study. Neurocrit Care. 2020;33(1):218–29.
Klopfenstein JD, Kim LJ, Feiz-Erfan I, et al. Comparison of rapid and gradual weaning from external ventricular drainage in patients with aneurysmal subarachnoid hemorrhage: a prospective randomized trial. J Neurosurg. 2004;100(2):225–9.
Ascanio LC, Gupta R, Adeeb N, et al. Relationship between external ventricular drain clamp trials and ventriculoperitoneal shunt insertion following nontraumatic subarachnoid hemorrhage: a single-center study. J Neurosurg. 2019;130(3):956–62.
Chung DY, Mayer SA, Rordorf GA. External ventricular drains after subarachnoid hemorrhage: is less more? Neurocrit Care. 2018;28(2):157.
Czorlich P, Ricklefs F, Reitz M, et al. Impact of intraventricular hemorrhage measured by Graeb and LeRoux score on case fatality risk and chronic hydrocephalus in aneurysmal subarachnoid hemorrhage. Acta Neurochir (Wien). 2015;157(3):409–15.
Wilson CD, Safavi-Abbasi S, Sun H, et al. Meta-analysis and systematic review of risk factors for shunt dependency after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2017;126(2):586–95.
Lewis A, Kimberly T. Prediction of ventriculoperitoneal shunt placement based on type of failure during external ventricular drain wean. Clin Neurol Neurosurg. 2014:109–13.
Yamada S, Nakase H, Park YS, et al. Discriminant analysis prediction of the need for ventriculoperitoneal shunt after subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 2012;21(6):493–7.
Garcia S, Torne R, Hoyos JA, et al. Quantitative versus qualitative blood amount assessment as a predictor for shunt-dependent hydrocephalus following aneurysmal subarachnoid hemorrhage. J Neurosurg. 2018;131(6):1743–50.
Lewis A, Irvine H, Ogilvy C, Kimberly T. Predictors for delayed ventriculoperitoneal shunt placement after external ventricular drain removal in patients with subarachnoid hemorrhage. Br J Neurosurg. 2015;29(2):219–24.
Pinggera D, Kerschbaumer J, Petr O, et al. The volume of the third ventricle as a prognostic marker for shunt dependency after aneurysmal subarachnoid hemorrhage. World Neurosurg. 2017;108:107–11.
Van Gijn J, Hijdra A, Wijdicks E, Vermeulen M, van Crevel H. Acute hydrocephalus after aneurysmal subarachnoid hemorrhage. J Neurosurg. 1985;63(3):355–62.
Aboul-Ela HM, Salah El-Din AM, Zaater AA, Shehab M, El Shahawy OA. Predictors of shunt-dependent hydrocephalus following aneurysmal subarachnoid hemorrhage: a pilot study in a single Egyptian institute. Egypt J Neurol Psychiat Neurosurg. 2018;54(1):1–6.
Xie Z, Hu Z, Zan X, et al. Predictors of shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage? A systematic review and meta-analysis. World Neurosurg. 2017;106:844-60.e6.
Cunningham P, Delany SJ. k-Nearest neighbour classifiers - a tutorial. ACM Comput Surv. 2022;54(6):1–25.
Youden W. Index for rating diagnostic tests. Cancer. 150AD;3(1):32–5.
Diesing D, Wolf S, Sommerfeld J, et al. A novel score to predict shunt dependency after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2018;128:1273–9.
Gupta R, Ascanio LC, Enriquez-Marulanda A, et al. Validation of a predictive scoring system for ventriculoperitoneal shunt insertion after aneurysmal subarachnoid hemorrhage. World Neurosurg. 2018;109:e210-6.
Lenski M, Biczok A, Huge V, et al. Role of cerebrospinal fluid markers for predicting shunt-dependent hydrocephalus in patients with subarachnoid hemorrhage and external ventricular drain placement. World Neurosurg. 2019;121:e535-42.
Zeng JP, Qin LP, Wang DB, et al. Comparing the risk of shunt-dependent hydrocephalus in patients with ruptured intracranial aneurysms treated by endovascular coiling or surgical clipping: an updated meta-analysis. World Neurosurg. 2019;121:e731-8.
Koyanagi M, Fukuda H, Saiki M, et al. Effect of choice of treatment modality on the incidence of shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2018;130(3):949–55.
Akinduro OO, Vivas-Buitrago TG, Haranhalli N, et al. Predictors of ventriculoperitoneal shunting following subarachnoid hemorrhage treated with external ventricular drainage. Neurocrit Care. 2019;32(3):755–64.
Jabbarli R, Pierscianek D, Rölz R, et al. Gradual external ventricular drainage weaning reduces the risk of shunt dependency after aneurysmal subarachnoid hemorrhage: a pooled analysis. Oper Neurosurg. 2018;15(5):498–504.
Chung DY, Thompson BB, Kumar MA, et al. Association of external ventricular drain wean strategy with shunt placement and length of stay in subarachnoid hemorrhage: a prospective multicenter study. Neurocrit Care. 2022;36:536–45.
Auer LM, Mokry M. Disturbed cerebrospinal fluid circulation after subarachnoid hemorrhage and acute aneurysm surgery. Neurosurgery. 1990;26:804–8.
Zolal A, Juratli T, Dengl M, et al. Daily drained CSF volume is a predictor for shunt dependence - a retrospective study. Clin Neurol Neurosurg. 2015;138:147–50.
García-Armengol R, Puyalto P, Misis M, et al. Cerebrospinal fluid output as a risk factor of chronic hydrocephalus after aneurysmal subarachnoid hemorrhage. World Neurosurg. 2021;154:e572-9.
Erixon HO, Sorteberg A, Sorteberg W, Eide PK. Predictors of shunt dependency after aneurysmal subarachnoid hemorrhage: results of a single-center clinical trial. Acta Neurochir (Wien). 2014;156(11):2059–69.
Lewis A, Kimberly WT. A retrospective analysis of cerebrospinal fluid drainage volume in subarachnoid hemorrhage and the need for early or late ventriculoperitoneal shunt placement. J Neurosurg Sci. 2016;60(3):289–95.
Jabbarli R, Bohrer AM, Pierscianek D, et al. The CHESS score: a simple tool for early prediction of shunt dependency after aneurysmal subarachnoid hemorrhage. Eur J Neurol. 2016;23:912–8.
Motiei-Langroudi R, Adeeb N, Foreman P, et al. Predictors of shunt insertion in aneurysmal subarachnoid hemorrhage. World Neurosurg. 2017;98:421–6.
Wilson D, Nakaji P, Abla A, et al. A simple and quantitative method to predict symptomatic vasospasm after subarachnoid hemorrhage based on computed tomography: beyond the Fisher scale. Neurosurgery. 2012;71(4):869–75.
García-Armengol R, Puyalto de Pablo P, Misis M, et al. Validation of shunt dependency prediction scores after aneurysmal spontaneous subarachnoid hemorrhage. Acta Neurochir. 2021;163(3):743–51.
Vyas D, Booker J, Smith D, Al-Tamimi YZ. External validation of scoring models to predict shunt insertion after aneurysmal subarachnoid hemorrhage. World Neurosurg. 2021;146:e1255-61.
Funding
Dr. Park reports research support from the National Institutes of Health (R21 NS113055); Dr. Megjhani reports research support from the American Heart Association (20POST35210653); and Dr. Rubinos is supported by the University of North Carolina School of Medicine Physician Scientist Training Program.
Author information
Authors and Affiliations
Contributions
The authors contributed to this article as follows: Drs. Park, Rubinos, and Megjhani and Ms. Terilli conceptualized and designed the study, oversaw data acquisition, and intellectually revised the article. Dr. Rubinos drafted the article and intellectually revised it. Drs. Rubinos, Ford, Alkhachroum, Kirsch, and Megjhani, Ms. Wong, Ms. Cespedes, Ms. Terilli, and Mr. Renz were responsible for data acquisition and critically revised the article. Drs. Kwon and Park performed the statistical analysis and critically revised the article. Drs. Velazquez, Roh, Agarwal, Claassen, Connolly, and Park revised the article for intellectual content. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Ethical approval/informed consent
This study adheres to ethical guidelines and has approval from the local institutional review board of Columbia University (AAAL4106), including waiver of consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplemental Digital Content Fig. 1
Flowchart of participants selection. BCI, bicaudate index, CSF, cerebrospinal fluid, EVD, external ventricular drain. (PNG 63 KB)
Rights and permissions
About this article
Cite this article
Rubinos, C., Kwon, S.B., Megjhani, M. et al. Predicting Shunt Dependency from the Effect of Cerebrospinal Fluid Drainage on Ventricular Size. Neurocrit Care 37, 670–677 (2022). https://doi.org/10.1007/s12028-022-01538-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01538-8