Abstract
The incidence of thyroid cancer has been greatly increasing. Several studies aimed to investigate biomarkers for prediction of thyroid cancer. Some of these studies have suggested that thyroid autoantibodies (TAb) could be used as predictors of thyroid cancer risk, but the correlation between TAb and PTC is still a matter of debate. The aim of this study is to evaluate thyroid autoimmunity and TAbs in patients with PTC and benign multinodular goiter (MNG) to investigate if TAbs and autoimmune thyroid disease (ATD) could predict thyroid malignancy. A total of 577 patients with thyroid papillary carcinoma (PTC) and 293 patients with benign MNG disease were enrolled postoperatively. Demographic features, thyroglobulin (TgAb) and thyroid peroxidase antibodies (TPOAb) and histologic outcome of the patients were evaluated. The prevalence of ATD and TgAb or TPOAb measurements was not statistically different in PTC and MNG groups. However, tumors were significantly smaller and tumor capsule invasion was seen less frequently in patients with PTC and ATD than without ATD. Patients without ATD had more advanced stage (TNM stage III/IV) tumors than with ATD. Only one of the 11 patients with distant organ metastasis had ATD. The present study demonstrated that the prevalence of ATD diagnosed even with histology or TAb positivity was not different in patients with PTC and MNG. However, having ATD might be associated with a better prognosis in PTC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid cancer is the most frequent cancer among endocrine tumors, accounting for approximately 1% of all malignancies [1]. Its incidence has been greatly increasing due to the increased detection of subclinical cancer with advanced diagnostic technologies [2]. Several studies aimed to investigate biomarkers that predicted thyroid cancer. Some of these studies have suggested that thyroid autoantibodies (TAb) could be used as predictors of thyroid cancer risk based on the association between thyroid autoimmune disease and thyroid cancer [3–6]. The association between Hashimoto’s thyroiditis (HT) and papillary thyroid carcinoma (PTC) has been discussed in several studies and contradictory data have been obtained [7–11]. PTC commonly develops in patients with autoimmune thyroiditis [4–6], raising the question if autoimmune thyroiditis develop because of antitumor immune response or vice versa? Serum TAb, including thyroglobulin antibodies (TgAb) and thyroid peroxidase antibodies (TPOAb), are diagnostic hallmarks of HT [12]. Although TAb can be detected in 10% of the general population [13], the incidence of positive TgAb and TPOAb is approximately two fold greater in DTC patients than in the general population [14]. Therefore, an association between TAb and DTC could be predicted, but the correlation between TAb and PTC is still a matter of debate.
In this study, we aimed to evaluate thyroid autoimmunity and TAbs in patients with PTC and benign multinodular goiter (MNG) to show if there is an association between autoimmune thyroid disease (ATD) and thyroid malignancy.
Materials and methods
Study population
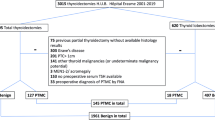
This is a retrospective, nonrandomised, population based study. A total of 876 patients with thyroid papillary carcinoma (PTC) during the period between January 2009 and December 2014 in our adult endocrinology clinic were retrospectively reviewed. Patients without postoperative pathology specimens, TgAb and TPOAb measurements before operation, and patients with history of neck radiation were excluded. Finally, 577 patients with PTC were enrolled to the study. In addition, 293 patients diagnosed as benign MNG postoperatively between January 2009 and December 2014 with known TgAb and TPOAb measurements before operation were evaluated as control group. Demographical data of the patients were obtained from our clinical records.
Existence of ATD was defined as either having both TgAb and TPOAb positivity and/or histological changes of ATD in postoperative surgical pathologic evaluation. TgAb and TPOAb measurements were also evaluated separately in subgroup analyses.
Histological diagnosis
Histological data were obtained from the postoperative paraffin histological reports, provided by our Pathology Department. The histological diagnoses were confirmed by single independent experienced pathologists. The entire gland and additional nodal tissue was evaluated using 1-mm-thick anatomical slices. Histopathologic results were reported, including tumor size, tumor capsule invasion, and extrathyroidal extension that included T3 (minimal) and T4 (extensive), lymph node, and distant organ metastasis according to the seventh edition of TNM classification by the American Joint Committee on Cancer staging system [15]. These prognostic factors were compared in patients according to ATD status.
The histological criteria for ATD included diffuse lymphocytic infiltration, germinal centers, enlarged epithelial cells with large nuclei and eosinophilic cytoplasm (Askanazy or Hurthle cells), and variable amounts of stromal fibrosis throughout the thyroid gland [16].
Laboratory procedures
TgAb and TPOAb were measured by a chemiluminescence microparticle immunoassay using a commercial kit (TgAb:Architect Anti-Tg Reagent Kit; Fisher Scientific, Middletown, VA, USA; TPOAb: Architect Anti-Tpo Reagent Kit; Fisher Scientific, Middletown, VA, USA).
The normal range of thyroid function was established by the Laboratory; TgAb 0.00–4.11 IU/mL; TPOAb 0.00–9.00 IU/mL.
Statistical analysis
Data analysis was performed using the statistical software (IBM SPSS v20.0). Continuous data were presented as mean and standard deviations with median values. The Chi-squared test, Student’s t test, and other nonparametric tests were performed when appropriate. P < 0.05 was considered statistically significant.
The study protocol was approved by the local ethics committee.
Results
A total of 577 patients with PTC and 293 patients with MNG were evaluated. Characteristics of the patients with MNG and PTC were given in Table 1. Patients with PTC were significantly younger (47 ± 12 vs. 53 ± 12 years; P = 0.01), and there was slightly female predominance in PTC group [471 (82%) of the PTC patients that were female vs. 219 (75%) patients which were female in MNG group; P = 0.021].
The prevalence of ATD was not statistically different in PTC and MNG groups (30 vs. 31%, respectively; P = 0.3). In addition, no significant differences were observed for either TgAb or TPOAb measurements in both groups (Table 1).
In subgroup analysis of the patients with PTC, there was increased female predominance (P = 0.01) but no age difference between patients with and without ATD. In addition, tumors were significantly smaller (13.9 ± 12.4 vs. 18.4 ± 16.4 mm, P = 0.002) and tumor capsule invasion was seen less frequently in patients with PTC and ATD than without ATD, but there was no difference in case of extra thyroidal extension (Table 2). 81% of the PTC patients with ATD had stage one tumors (TNM stage I), while 72% of the patients without ATD. Patients without ATD had more advanced stage (TNM stage III/IV) tumors than with ATD [26 (6.4%) vs. 1 (0.6%); P = 0.001]. Conversely, patients with ATD had more multicentric tumors than patients without ATD [67 (39%) vs. 113 (28%); P = 0.01] (Table 2). Lymph node metastasis was found similarly in patients with and without ATD. There were 11 (2.5%) patients with distant organ metastasis and only 1 (0.6%) of them had ATD.
Discussion
The present study evaluated ATD diagnosed even with histology or TAb positivity in patients with PTC and MNG and showed no association between ATD and thyroid malignancy. The retrospective analyses of the patients revealed the same prevalence of ATD in PTC and MNG cases. However, having ATD might be associated with a better prognosis in PTC patients. PTC cases with ATD had smaller tumors, less advanced disease, and less frequent tumor capsule invasion than without ATD. In addition, among patients with distant organ metastasis, only one had ATD.
The incidence of thyroid cancer has been increasing due to several factors. A parallel increase has been observed in the ATDs. These two diseases share some epidemiological features, such as the relationship with ionizing radiation exposure [17, 18] and dietary iodine [19, 20], and are more likely to occur in women [21–23]. However, the clinical data suggesting the causative relationship between ATD and PTC remain unclear. This might be a result of heterogeneity of the diagnostic criteria for ATD. In the present study, we defined ATD as either having both TgAb and TPOAb and/or histological changes of ATD in postoperative surgical pathologic evaluation.
The prevalence of ATD in differentiated thyroid cancer patients has been reported ranging from 14 to 37% in different studies [24]. In our study, the prevalence of ATD was 30% in PTC patients consistent with the literature, but it was not different from the prevalence of the patients having MNG. There are a numerous number of studies evaluating thyroid autoimmunity and thyroid cancer debating the relation in the literature, but this issue is still remaining controversial. A series of reports indicate a close association between ATD and malignancy [3, 25], while others, like our study, were not able to confirm this association [26–29].
The studies suggesting increased incidence of PTC in patients having ATD are usually retrospective in nature. Therefore, they are unsatisfactory to explain underlying mechanisms [30]. However, studies with molecular aspects concluded possible molecular link between thyroid cancer and chronic lymphocytic thyroiditis (LT). Some authors have found RET/PTC rearrangements in non-neoplastic thyroid lesions, such as chronic LT [31–33]. Chronic inflammation might facilitate the rearrangement, or conversely, RET/PTC rearrangement might promote chronic inflammation [34]. BRAFV600E mutation is another common genetic alteration in PTC. Muzza et al. found BRAFV600E being more represented in PTC without concurrent autoimmunity [34]. In addition, tumor defense-induced autoimmunity might be another pathogenic mechanism for the synchronous existence of PTC and ATD. Although there is growing evidence, it is still a matter of debate; whether PTC develops despite autoimmunity or as a result of an immune response. Due to the retrospective design of our study, we could not be able to investigate any pathogenic mechanism. However, we evaluated TgAb and TPOAb measurements separately to specify any correlation, but no significant differences were observed in both groups. Wu et al. have shown higher PTC incidence in patients with Tab positivity, but they have not found any difference between TgAb and TPOAb measurements [12].
Although the present study could not demonstrate any correlation between ATD and PTC incidence, we have found better prognostic markers of PTC in patients having ATD. We showed that PTC patients with ATD were more likely to be female, and had a smaller tumor size and less tumor capsule invasion than PTC patients without ATD. Patients with ATD are usually followed more closely; this might cause early diagnosis of PTC, therefore, smaller tumor size. The TNM stages of the PTC patients with ATD tended to be less advanced suggesting a better prognosis. The effect of ATD on the prognosis of PTC is another debate of this topic; most of the studies in the literature showed either a protective [36–40] or a neutral [35, 41] effect of thyroid autoimmunity on PTC behavior. There were 11 patients with distant organ metastasis in our cohort, and only one of them had ATD. This was also an important issue to predict a better prognosis of PTC in patients with thyroid autoimmunity. Interestingly, we observed more often multicentric tumors in ATD patients. This finding was compatible with the results of Kim et al. who found more frequent, multifocality, and bilaterality in metastatic papillary thyroid microcarcinomas with LT than without LT [42]. In addition, similar findings were reported in some studies in the literature [43, 44]. Although it is difficult to suggest this result from a retrospective study, PTC of the patients with ATD might be at risk of multifocality that might effect surgical treatment choice in case of preoperative diagnosis.
Our study has some limitations; this was a retrospective study. The number of control group was small that might effect the ATD prevalence results. We only evaluate histology, TgAb, and TPOAb measurements for the diagnosis of ATD; therefore, we could not suggest any underlying mechanism for autoimmunity.
In conclusion, this study showed that the prevalence of ATD was not increased in patients with PTC. However, in patients with PTC, coexisting ATD might result a better prognosis, such as smaller and less invasive tumors, and decreased distant organ metastases incidence.
References
Pellegriti G, Frasca F, Regalbuto C et al (2013) Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol 2013:965212 (Epub 7 May 2013)
Verkooijen HM, Fioretta G, Pache JC et al (2003) Diagnostic changes as a reason for the increase in papillary thyroid cancer incidence in Geneva, Switzerland. Cancer Causes Control 14(1):13–17
Kim ES, Lim DJ, Baek KH et al (2010) Thyroglobulin antibody is associated with increased cancer risk in thyroid nodules. Thyroid 20(8):885–891
Fiore E, Rago T, Latrofa F et al (2011) Hashimoto’s thyroiditis is associated with papillary thyroid carcinoma: role of TSH and of treatment with l-thyroxine. Endocr Relat Cancer 18(4):429–437
Caturegli P, De Remigis A, Chuang K et al (2013) Hashimoto’s thyroiditis: celebrating the centennial through the lens of the Johns Hopkins hospital surgical pathology records. Thyroid 23(2):142–150
Chen YK, Lin CL, Cheng FT et al (2013) Cancer risk in patients with Hashimoto’s thyroiditis: a nationwide cohort study. Br J Cancer 109(9):2496–2501
Cunha LL, Morari EC, Guihen AC et al (2012) Infiltration of a mixture of immune cells may be related to good prognosis in patients with differentiated thyroid carcinoma. Clin Endocrinol (Oxf) 77(6):918–925
French JD, Kotnis GR, Said SJ et al (2012) Programmed death-1+ T cells and regulatory T cells are enriched in tumor-involved lymph nodes and associated with aggressive features in papillary thyroid cancer. J Clin Endocrinol Metab 97(6):E934–E943
Qing W, Fang WY, Ye L et al (2012) Density of tumor associated macrophages correlates with lymph node metastasis in papillary thyroid carcinoma. Thyroid 22(9):905–910
Xu WC, Li ZB, Chen YR et al (2011) Expression and distribution of S-100, CD83, and costimulatory molecules (CD80 and CD86) in tissues of thyroid papillary carcinoma. Cancer Invest 29(4):286–292
Yu H, Huang X, Liu X et al (2013) Regulatory T cells and plasmacytoid dendritic cells contribute to the immune escape of papillary thyroid cancer coexisting with multinodular non-toxic goiter. Endocrine 44(1):172–181
Wu X, Lun Y, Jiang H et al (2014) Coexistence of thyroglobulin antibodies and thyroid peroxidase antibodies correlates with elevated thyroid-stimulating hormone level and advanced tumor stage of papillary thyroid cancer. Endocrine 46(3):554–560
Hollowell JG, Staehling NW, Flanders WD et al (2002) Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 87:489–499
Spencer CA (2011) Clinical review: clinical utility of thyroglobulin antibody (TgAb) measurements for patients with differentiated thyroid cancers (DTC). J Clin Endocrinol Metab 96:3615–3627
Edge SB, Byrd DR, Compton C et al (2010) AJCC cancer staging manual, 7th edn. Springer, New York
Lun Y, Wu X, Xia Q et al (2013) Hashimoto’s thyroiditis as a risk factor of papillary thyroid cancer may improve cancer prognosis. Otolaryngol Head Neck Surg 148:396–402
Wartofsky L (2010) Increasing world incidence of thyroid cancer: increased detection or higher radiation exposure. Hormones 9(2):103–108
Ostroumova E, Brenner A, Oliynyk V et al (2009) Subclinical hypothyroidism after radioiodine exposure: Ukrainian–American cohort study of thyroid cancer and other thyroid diseases after the chornobyl accident (1998–2000). Environ Health Perspect 117(5):745–750
Gomez Segovia I, Gallowitsch HJ, Kresnik E et al (2004) Descriptive epidemiology of thyroid carcinoma in Carinthia, Austria: 1984–2001. Histopathologic features and tumor classification of 734 cases under elevated general iodination of table salt since 1990: population-based age-stratified analysis on thyroid carcinoma incidence. Thyroid 14(4):277–286
Laurberg P, Cerqueira C, Ovesen L et al (2010) Iodine intake as a determinant of thyroid disorders in populations. Best Pract Res 24(1):13–27
Bloodworth JMB, Lechago J, Gould VE (1996) Bloodworth’s endocrine pathology, 3rd edn. Williams & Wilkins, Baltimore
Singh B, Shaha AR, Trivedi H et al (1999) Coexistent Hashimoto’s thyroiditis with papillary thyroid carcinoma: impact on presentation, management, and outcome. Surgery 126(6):1070–1077
Ward LS, Assumpção LV (2007) The impact of gender in differentiated thyroid cancer. Clin Endocrinol 66(5):752–753
Cunha LL, Ferreira RC, Marcello MA et al (2011) Clinical and pathological implications of concurrent autoimmune thyroid disorders and papillary thyroid cancer. J Thyroid Res 17(2011):387062
Boi F, Lai ML, Marziani B et al (2005) High prevalence of suspicious cytology in thyroid nodules associated with positive thyroid autoantibodies. Eur J Endocrinol 153(5):637–642
Fiore E, Rago T, Scutari M et al (2009) Papillary thyroid cancer, although strongly associated with lymphocitic infiltration on histology, is only weakly predicted by serum thyroid autoantibodies in patients with nodular thyroid disease. J Endocrinol Invest 32(4):344–351
Boelaert K, Horacek J, Holder RL et al (2006) Serum thyrotropin concentration as a novel predictor of malignancy in thyroid nodules investigated by fine-needle aspiration. J Clin Endocrinol Metab 91(11):4295–4301
Rago T, Di Coscio G, Ugolini C et al (2007) Clinical features of thyroid autoimmunity are associated with thyroiditis on histology and are not predictive of malignancy in 570 patients with indeterminate nodules on cytology who had a thyroidectomy. Clin Endocrinol (Oxf) 67(3):363–369
Fiore E, Rago T, Provenzaleetal MA et al (2009) Lower levels of TSH are associated with a lower risk of papillary thyroid cancer in patients with thyroid nodular disease: thyroid autonomy may play a protective role. Endocr Relat Cancer 16(4):1251–1260
Jankovic B, Le KT, Hershman JM (2013) Clinical review: Hashimoto’s thyroiditis and papillary thyroid carcinoma: is there a correlation? J Clin Endocrinol Metab 98(2):474–482
Wirtschafter A, Schmidt R, Rosen D et al (1997) Expression of the RET/PTC fusion gene as a marker for papillary carcinoma in Hashimoto’s thyroiditis. Laryngoscope 107(1):95–100
Sheils OM, O’Leary JJ, Uhlmann V et al (2000) Ret/PTC-1 activation in Hashimoto thyroiditis. Int J Surg Pathol 8(3):185–189
Elisei R, Romei C, Vorontsova T et al (2001) RET/PTC rearrangements in thyroid nodules: studies in irradiated and not irradiated, malignant and benign thyroid lesions in children and adults. J Clin Endocrinol Metab 86(7):3211–3216
Guarino V, Castellone MD, Avilla E et al (2010) Thyroid cancer and inflammation. Mol Cell Endocrinol 32(1):94–102
Muzza M, Degl’Innocenti D, Colombo C et al (2010) The tight relationship between papillary thyroid cancer, autoimmunity and inflammation: clinical and molecular studies. Clin Endocrinol 72(5):702–708
Kashima K, Yokoyama S, Noguchi S et al (1998) Chronic thyroiditis as a favorable prognostic factor in papillary thyroid carcinoma. Thyroid 8(3):197–202
Loh KC, Greenspan FS, Dong F et al (1999) Influence of lymphocytic thyroiditis on the prognostic outcome of patients with papillary thyroid carcinoma. J Clin Endocrinol Metab 84(2):458–463
Kim EY, Kim WG, Kim WB et al (2009) Coexistence of chronic lymphocytic thyroiditis is associated with lower recurrence rates in patients with papillary thyroid carcinoma. Clin Endocrinol 71(4):581–586
Gupta S, Patel A, Folstad A et al (2001) Infiltration of differentiated thyroid carcinoma by proliferating lymphocytes is associated with improved disease-free survival for children and young adults. J Clin Endocrinol Metab 86(3):1346–1354
Medenica S, Radojevic N, Stojkovic M et al (2015) Autoimmunity and thyrotropin level in developing thyroid malignancy. Eur Rev Med Pharmacol Sci 19(15):2824–2829
Yano Y, Shibuya H, Kitagawa W et al (2007) Recent outcome of grave’s disease patients with papillary thyroid cancer. Eur J Endocrinol 157(3):325–329
Kim HS, Choi YJ, Yun JS (2010) Features of papillary thyroid microcarcinoma in the presence and absence of lymphocytic thyroiditis. Endocr Pathol 21(3):149–153
Sakorafas GH, Giotakis J, Stafyla V (2005) Papillary thyroid microcarcinoma: a surgical perspective. Cancer Treat Rev 31(6):423–438
Falvo L, D’Ercole C, Sorrenti S et al (2003) Papillary microcarcinoma of the thyroid gland: analysis of prognostic factors including histological subtype. Eur J Surg Suppl 588:28–32
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest that could be perceived as prejudicing the impartiality of this research.
Ethical approval
The study protocol was approved by the local ethics committee, and the informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Selek, A., Cetinarslan, B., Tarkun, I. et al. Thyroid autoimmunity: is really associated with papillary thyroid carcinoma?. Eur Arch Otorhinolaryngol 274, 1677–1681 (2017). https://doi.org/10.1007/s00405-016-4414-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4414-6