Abstract
Parathyroid carcinoma (PC) is an extremely rare malignant tumor of the parathyroid glands, accounting for less than 1% of primary hyperparathyroidism, commonly characterized by severe and unmanageable hypercalcemia, aggressive behavior, high metastatic potential, and poor prognosis. PC manifests prevalently as a sporadic tumor and only occasionally it is part of congenital syndromic and non-syndromic endocrine diseases. Molecular pathogenesis of this form of parathyroid tumor is not fully elucidated and it appears to be caused by multiple genetic and epigenetic drivers, differing among affected patients and not yet clearly stated in distinguishing PC from the benign parathyroid adenoma (PA). Congenital forms of PC have been prevalently associated with germline heterozygous loss-of-function mutations of the CDC73 tumor suppressor gene, both in the context of the hyperparathyroidism jaw-tumor syndrome (HPT-JT) and of the isolated familial hyperparathyroidism (FIPH). Currently, surgical en bloc resection of affected gland(s) and other involved structures is the elective therapy for both primary and recurrent PC. However, it usually results ineffective for advance and metastatic disease, and a high percentage of post-operative recurrence is reported. Targeted medical therapies for surgically untreatable PC, based on the molecular profile of PC samples, are, therefore, needed. The characterization of genetic and epigenetic alterations and deregulated pathways in PC samples will be of fundamental importance to tailor treatment for each patient. Here, we reviewed main findings on molecular pathogenetic aspects of PC, and the current state of the art of therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parathyroid carcinoma (PC) is the, extremely rare, malignant form of parathyroid tumors, accounting for less than 1% of primary hyperparathyroidism (PHPT) in Western Europe and North America and about 5–7.1% in China and Japan [1].
Clinical presentation of PC is similar to the benign counterpart, consisting in PHPT and hypercalcemia-derived signs and symptoms, such as fatigue, bone and joint pain, nephrolithiasis, decreased glomerular filtration rate, osteoporosis, fragility fracture, and neurocognitive and cardiac dysfunctions. Unlike the benign counterpart, PC is often associated with severe, commonly unmanageable, and drug-refractory hypercalcemia, and more likely to induce hypercalcemic crisis.
PC prognosis and overall survival depend on primary tumor size, tumor stage, and invasion at the time of diagnosis and on the possibility to early remove all the cancer tissue by surgery; the presence of one or more metastatic lesions at diagnosis worsens the prognosis [2, 3]. About 10–30% of PC patients have distant metastases at presentation, mainly in lung, liver or bone. Unfortunately, in about half of the cases, principally in advanced and metastatic carcinomas, surgery is not curative, and disease persistence and/or relapse occur in over 50% of patients [4]. The estimated overall survival rate in PC is 78–85% and 49–70%, respectively at 5 and 10 years, after the first diagnosis [4, 5].
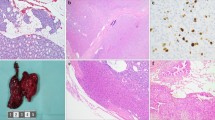
Pre-operative diagnosis of PC is difficult and rare. Markedly elevated serum calcium (>14 mg/dl or >3.5 mmol/l) and/or parathyroid hormone (PTH) levels 3–10 times higher than the upper limit of normal are suspicious of malignancy, but they are not present in all PC cases, and, alone, are not sufficient in clearly distinguishing PC from parathyroid adenoma (PA). Imaging techniques are useful to localize parathyroid tumor(s), but they are not sufficiently specific or sensitive to assess malignancy. Identification of lymphadenopathy in the neck region and/or of presence of tumor local invasion by pre-operative imaging could be a suspicion of PC and an indication for surgeon to perform a more extensive surgery. Fine-needle tumor biopsy should be avoided because of the risk of tumor capsule rupture and tumor cell spreading. Intra-operative finding of local and/or vascular invasion and/or a tumor mass greater than 3 cm in diameter are suspects of malignancy and should be a guidance for a more aggressive surgery. Definitive diagnosis of PC is usually made in the post-operative setting, based on specific histological and cytological characteristics of malignancy, such as signs of capsular disruption and angiolymphatic invasion, thick fibrous bands, presence of more than 6 mitoses per 10 high power field, atypical mitotic figures, cell reduced cytoplasm/nucleus ratio, signs of necrosis and Ki67 marker higher than 5% [4, 6], but in the majority of cases it is operator-dependent. Reduction/absence of nuclear parafibromin immunostaining in the tumor specimen may further confirm the intra-operative and histological suspicion of PC. Genetic profile of the resected tumor may aid in the definitive diagnosis of PC.
Molecular pathogenesis of PC
Molecular pathogenesis of PC appears as a complex picture. In addition to germline mutations in specific genes, associated with inherited syndromic and non-syndromic forms of PC, such as CDC73, and, in extremely rare cases, MEN1 and RET, various somatic genetic and epigenetic alterations were identified in cancer cells from both congenital and sporadic PCs, differing among affected patients and not yet clearly stated in distinguishing PC from the benign PA.
Whole-genome and whole-exome sequencing analyses and studies of global gene and protein expression in PC samples identified several mutated/altered genes and deregulated epigenetic regulators, some of them specifically found in malignant cancers compared to benign PA and/or healthy parathyroid tissue. However, great variability in the genetic/epigenetic profile was evidenced among different PC samples, even in different tumor specimens from the same patient, not allowing clearly identify which are the effective molecular drivers of parathyroid cancer development and malignant progression that could represent molecular targets for PC medical therapies.
Loss of the tumor suppressor activity of the CDC73 gene is the most common hallmark of PC, both in the inherited and sporadic forms of the disease. Germline heterozygote loss-of-function mutations of the CDC73 tumor suppressor gene are detected in 50–75% of hyperparathyroidism jaw tumor syndrome (HPT-JT) pedigrees, and in about 8% of families with familial isolated hyperparathyroidism (FIHP) [6], usually in association with somatic loss of heterozygosity at the 1q31.2 locus or inactivation of the second CDC73 allele, in cancer cells. Somatic inactivation or loss of at least one CDC73 allele is found in 9–100% of sporadic PC, depending on the analyzed series [7], and homozygote CDC73 inactivation/loss is reported in 9–70% of cases. Conversely, biallelic inactivation/loss of the CDC73 gene is found in less than 5% of PAs. CDC73 encodes a ubiquitously expressed, evolutionarily conserved, protein, named parafibromin. In normal parathyroid cells, parafibromin is located in the nucleus. Loss of nuclear immunostaining of parafibromin is a common hallmark of PC cells, found in 33.3–100% of cases, compared to only 0–3.7% of multiglandular parathyroid hyperplasia and 0–17.6% of PAs [8]. Parafibromin is an essential component of the Polymerase-Associated Factor 1 (PAF1) that is involved in the regulation of gene transcription, elongation of gene transcripts and mRNA 3’-end processing, in the control of cell cycle and apoptosis, in the maintenance of chromosome stability, and in the modulation of canonical Wnt and p53 signaling. Loss of parafibromin activity is implicated in carcinogenesis, aggressive PC behavior, and poor prognosis. Restoring wild type parafibromin expression and activity could represent a suitable genetic therapy for the treatment of CDC73-mutated PCs. Currently, no specific targeted therapy or clinical trial has been conducted for treatment of PC cases with germline or somatic CDC73 mutations.
Over-expression of cyclin D1, a positive regulator of the cell cycle through the promotion of G1-S phase transition via the activation of the cyclin-dependent kinases CDK4/CDK6, is a common event in PC (29–71% of PC cases depending on the analyzed series) [9, 10], caused by copy number amplification of the cyclin D1-encoding gene CCND1. Interestingly, 80% of PC cases with the CCND1 amplification were mutually exclusive with cases with somatic inactivation/loss of the CDC73 gene [10]. The cyclin D1 over-expression was frequently found also in benign PAs, excluding this molecular alteration as responsible for malignancy and suggesting that other concomitant somatic genetic or epigenetic alterations may synergically concur to the development of the malignant phenotype.
Various genes have been found mutated, at germinal and/or somatic level, in PC tissues, by whole-genome and whole-exome sequencing studies [9, 11,12,13,14].
Among the most commonly identified mutated genes in PC there are those related to two important signaling pathways, the PI3K/AKT/mTOR pathway [9, 12,13,14] and the Wnt signaling [9, 11].
The PI3K/AKT/mTOR pathway is a critical regulator of cell growth and survival in physiological and pathological conditions. Activating mutations in the PIK3CA gene and inactivating mutation in the PTEN gene commonly occur in diverse human tumors, resulting in constitutive activation of the PI3K/AKT/mTOR signaling and being a key pathway in carcinogenesis [15]. Also in PC samples were identified somatic mutations in genes of the PI3K/AKT/mTOR pathway, such as the PIK3CA gene (p.Lys111Glu, p.Gly118Asp, p.Glu545Ala, p.Gln546Arg, p.Gln564Arg, p.His1047Arg) [9, 13, 14], the mTOR gene (p.Leu1460Pro, p.Gln2524Leu) [9], and the PTEN gene (p.Asp107Tyr, p.Arg130Gln, p.Phe90fsX1) [13, 14], or in genes involved in the regulation of mTOR activity, such as TSC1 (p.Val25Met, p.Arg177X, p.Arg228X) [5, 14] and TSC2 (p.Ser9X, p.G654fsX2) [13]. Globally, somatic genetic alterations that can activate the PI3K/AKT/mTOR pathway were found in up to 20% of analyzed PC cases [16], representing a major deregulated signaling pathway in parathyroid carcinogenesis and a potential therapeutic target for PC. A recent study by Riccardi et al. [17] found somatic, heterozygous, activating mutations of the PIK3CA gene in only 1% of the 391 analyzed typical, sporadic PAs, suggesting that tumorigenic activation of the PIK3CA enzyme could be strongly associated with malignant PC rather than benign PA.
Wnt signaling pathways are implicated in the regulation of cell growth and survival, and apoptosis through the modulation of target gene expression. Deregulation of Wnt signaling cascade has been tightly associated with various types of human malignancies, in which Wnt signaling affects maintenance of cancer stem cells, metastasis, and immune surveillance [18]. Svedlund et al. [19] found an absent or markedly reduced expression of APC protein, a major inhibitor of activation of the beta-catenin the intracellular signal transduction effector in the Wnt canonical pathway, in 5 analyzed PC samples, caused by hypermethylation of the promoter 1A of the APC gene, resulting in an increased cytoplasmatic accumulation of the non-phosphorylated active form of the beta-catenin, and subsequent Wnt pathway activation, compared to the adjacent normal parathyroid tissues. Moreover, somatic inactivating mutations of the APC gene (p.Thr297Ile, p.Glu1284Lys, p.Ala1793Gly) [9, 11], as well as of another gene involved in the negative regulation of both the canonical and the non-canonical Wnt pathways, the RNF43 gene (p.Gly659fs) [9] were identified in PC tissues. Amplification of the EZH2 gene at the 7q36.1 locus, encoding a histone 3 lysine 27 methyltransferase, was found in 60% of malignant PCs, showing a significant over-expression of EZH2 mRNA and protein compared to PAs and hyperplastic parathyroid glands, associated with increased trimethylation of histone 3 on lysine residue 27 (H3K27me3) [20]. In normal conditions, the EZH2 enzyme epigenetically mediates, via H3K27me3, the transcription repression of several Wnt antagonists, including the growth-suppressive AXIN2 protein, a negative regulator of beta-catenin stability and cytoplasmatic accumulation, in the absence of Wnt ligand. Over-expression of EZH2 enzyme represses AXIN2, significantly contributing to an aberrant accumulation of the active form of beta-catenin in the cytoplasm and the consequent nuclear translocation, resulting in the nuclear transduction of Wnt signaling that leads to increased cyclin D1 expression and enhanced cell proliferation [20]. Interestingly the hypermethylation of promoters, and the subsequent expression repression, of genes involved in the negative regulation of the Wnt pathway was found in PC specimens: 1) APC [21], 2) SFRP1, SFRP2, and SFRP4 [22], encoding three antagonist decoy receptors of Wnt ligands, 3) RASSF1A [21, 23], a tumor suppressor whose silencing leads to the accumulation of active beta-catenin and activation of Wnt-signaling-regulated gene transcription, and 4) HIC1 [24], encoding a transcription repressor that directly binds beta-catenin and the TCF4 transcription factor, preventing them from activating Wnt-induced TCF-mediated gene transcription. Finally, a significant up-regulation the miR-222 was found in PC, with respect to PA and normal parathyroid tissue [25]. Among known mRNA targets, whose translation is inhibited by this microRNA (miRNA), there are various negative regulators of the Wnt/beta-catenin pathway, including DKK2, WIF2, SFRP2, and AXIN2 [26]. Another miRNA that promotes cell proliferation by regulating the Wnt/beta-catenin pathway, the miR-372, was found to be over-expressed in PC [25]. Data from all these studies evidenced the importance of aberrant activation of the Wnt signaling cascades in the carcinogenesis of parathyroid tissue, and suggested the possibility to therapeutically target these pathways, mainly the activation of beta-catenin in the Wnt canonical pathway, to control cancer burden and progression.
In the last decade, whole-exome and whole-genome sequencing studies identified somatic variants/alterations in various genes in PC samples [5, 9, 11, 13, 14]; identified mutated genes have been summarized in a recent review by Marini et al. [27]. The pathogenic role of these genes in PC carcinogenesis is still unknown. Interestingly, no variants in the glial cells missing-2 (GCM2) gene, encoding a parathyroid cell-specific transcription factor, were found in whole-exome sequencing studies targeted on PC samples, however, rare activating variants of the GCM2 gene were found in patients who developed PC, either in the context of FIHP (Tyr394Ser, Ile383Met) [28, 29] or in sporadic PHPT (Lys388Glu, Val382Met) [29,30,31].
Accumulating evidence indicates that deregulated expression of non-coding RNAs, including both miRNAs and long non-coding RNAs (lncRNAs), which are important epigenetic regulators of gene expression, play a role in cancer biology. Recent studies showed significant up-regulation or down-regulation of specific miRNAs and lncRNAs in PC samples, which could exert a pro-oncogenic role in the carcinogenesis of parathyroid cells.
Among the deregulated miRNAs, miR-517c was the one showing the most significant expression difference between PC and PA, with the expression in PA being comparable with that observed in normal parathyroids. In PC samples, the up-regulation of miR-517c significantly correlated with over-expression of miR-371 and miR-372, all these three miRNAs maintaining the same deregulated expression profiles both in primary PC and in matched metastases. miR-517c over-expression also positively correlated with higher serum levels of calcium and PTH, and a greater weight of the resected tumor [25]. These findings indicated miR-517c as potentially involved in determining the malignant phenotype, and suggested this miRNA as a potential target for molecular therapy in PC.
Interestingly, miR-126-5p was found to be down-regulated both as intracellular miRNA in PC samples [32] and as circulating miRNA in the serum samples of patients with PC [33]. miR-126-5p is an endothelial-specific miRNA having a tumor suppressor activity, which was shown to modulate the vascular endothelial differentiation from embryonic stem cells, and whose down-regulation showed to induce cancer cell proliferation, migration, and invasion. Indeed, among targets of miR-126-5p there are genes involved in the regulation of cell adhesion and mobility, such as CRK, EGFL7, and ADAM9, and in the regulation of angiogenesis, such as EGFL7 and VEGF [34].
Higher levels of lncRNA BC200, a lncRNA whose up-regulation was reported in a broad spectrum of tumor cells, presumably being responsible for cell viability, invasion, and migration, characterized both PC tissues [35] and serum samples [36] from PC patients, compared with PAs. Intracellular lncRNA BC200 levels allowed to categorize PCs apart from both PAs and atypical parathyroid adenoma (aPAs), and to selectively discriminate among the three different tumor histotypes. Interestingly, serum levels of circulating lncRNA BC200 in PC patients showed to significantly reduce after parathyroidectomy [36] appearing as directly correlated with the presence of parathyroid malignancy. In addition, lncRNA BC200 resulted significantly more up-regulated in the group of PCs with CDC73 mutations compared to those with wild type parafibromin, in association with a more aggressive clinical phenotype characterized by higher levels of calcium ion and PTH [35].
The present and the future of therapy for PC
Conventional therapies
Surgical eradication is the first-choice therapy, and, currently, remains the primary and most effective management modality in the treatment of PC, either for primary tumors or for recurrent disease. Severe hypercalcemia should be controlled before surgery. Intra-operative recognition of malignancy is extremely important to optimize surgery and decide the extension of neck exploration and surgical resection, since PC treatment requires a more radical surgery than the benign counterpart. Initial surgery for PC should involve the en bloc resection of the primary tumor and ipsilateral thyroid lobectomy with gross clear margins, paying particular attention to avoid the rupture of tumor capsule, associated with the excision of adjacent involved structures and/or local metastatic lymph nodes. Occasionally, largely invasive tumors may request the resection of trachea, portion of the esophagus, blood vessels, or bone. The recurrent laryngeal nerve has to be preserved to maintain vocal cord function and be resected only in case of tumor invasion. Prophylactic dissection of non-metastatic lymph nodes in the central neck nodal compartment did not demonstrate to grant disease-free or survival benefit [37]. Intra-operative PTH dosage is not always informative to assess the complete resection of cancerous gland(s), since elevated PTH levels may be due to PHT-secreting distant metastases. Disease relapse occurs in over 50% of operated cases [38], generally after 2–3 years from surgery, mainly in cases of advance and metastatic PC, and patients may require reoperation. In recurrent and metastatic patients, the prognosis is often poor, and metastatic cases usually die of severe, drug-refractory hypercalcemia and renal insufficiency, rather than of the tumor burden itself.
Prophylactic parathyroidectomy to prevent PC in patients with germline CDC73 mutations is not indicated, since not all the carriers develop the malignant tumor. In these patients, annual measurement of calcium, PTH, and 25(OH)-vitamin D, and periodic neck ultrasounds are indicated. The suggested surgical approach for CDC73 mutation carriers consists of bilateral exploration of the neck with identification of all the parathyroids and selective resection of the affected gland(s), followed by post-operative life-long surveillance for PC recurrence.
Adjuvant treatments with chemotherapy agents or external beam radiation showed to be scarcely effective in PC in terms of overall survival, since they appear unable to control severe hypercalcemia and tumor progression. PC is considered a chemo- and radioresistant cancer. These therapies are, thus rarely used and prevalently restricted to palliative therapy of inoperable advanced metastatic disease, or recurrent, disseminated PC not solved by surgery.
Storvall et al. [39] demonstrated long-term cancer remission after 17-year of combined treatment with surgery, external radiotherapy, cinacalcet, zoledronic acid, and the chemotherapic molecule temozolomide (TEM) in a 48-year-old woman with a recurrent metastasized PC. Interestingly, the PC tissue showed a high methylation status in the promoter of the O6-methylguanine DNA methyltransferase (MGMT) gene, encoding a DNA-repairing enzyme that counteracts the DNA-damaging effects of alkylating agents, such as TEM. MGMT promoter high methylation enhances the cytotoxic effects of TEM on cancer cells and it is known to be a predictor of positive response to TEM treatment in some tumors, such as aggressive pituitary tumors and pancreatic neuroendocrine tumors. MGMT promoter methylation status has not been systematically investigated in PC, and hypermethylation of MGMT promoter was not reported among hypermethylated promoters found in PC samples. To assess if high MGMT promoter methylation status is common in malignant PCs and if MGMT promoter methylation testing in PC samples could identify those patients with advanced and disseminated PC who can benefit from TEM administration, Storvall et al. [40] analyzed the state of MGMT promoter methylation in tumor specimens from 11 PCs (including also the PC case previously reported to be positively treated with TEM, named as PC9 [39]) and one aPA from the daughter of PC9. The presence of high MGMT promoter methylation was found only in the PC9 patient, while all the other cases, included the aPA, showed a low-methylated status, indicating that the hypermethylation of MGMT promoter is an extremely rare event in PC. However, despite the result of the study, authors [40] recommended MGMT promoter methylation testing in recurrent PCs, not curable by surgery, since, even if highly rare, the presence of high methylation status could pharmacoepigenetically predict a good treatment response to TEM.
Pharmacological therapies for the control of calcemia
PC patients with an inoperable primary tumor, unresectable neck recurrence, or PTH-secreting distant metastases may experience hypercalcemic crisis, requiring hospitalization with intravenous hydration, and administration of loop diuretics, calcitonin and of bisphosphonates (usually intravenous pamidronate or zoledronic acid). Long-term control of chronic hypercalcemia is required in these cases, mainly consisting of bisphosphonates, the human anti-RANKL monoclonal antibody denosumab, or receptor agonists of the calcium-sensing receptor (calcimimetic molecules), either administered alone or in combination. Cinacalcet, a long-acting calcimimetic agent, showed to be effective in reducing both PTH and serum calcium levels in about two-thirds metastatic and inoperable PCs [41, 42].
When parathyroid surgery is followed by chronic hypocalcemia and hypophosphatemia, life-long therapy with calcium and calcitriol, or active vitamin D analogs, is required.
Promising targeted therapies
The off-label administration of some medical therapies targeting molecular pathways that resulted to be deregulated in a percentage of PC cases and, currently, approved for the treatment of some human malignancies, but not PC, was reported in clinical case reports of selected PC patients, mainly based on the individual PC genetic profile, showing promising results that need to be confirmed in larger case series.
The PI3K/AKT/mTOR signaling represents the second most frequently altered pathway, after the p53 pathway in human cancer [43], playing a central role in cancer initiation and progression. Therapies utilizing mTOR inhibitors are used to reduce the high mTOR signaling levels in various cancer types [43]. Somatic gene mutations that constitutively activate the PI3K/AKT/mTOR pathway were found in about up to 20% of PC cases [16], thus, the use of mTOR inhibitors could be an effective therapy in PC patients having these mutations. Currently, only one study [14] reported systemic therapy with everolimus, an mTOR inhibitor, in association with vendetanib, (an antiangiogenic drug), in a patient with metastatic PC and recurrent severe hypercalcemia and primary hyperparathyroidism after two not resolving surgeries (a unilateral parathyroidectomy and a neck dissection), positive for two somatic mutations in the TSC1 gene (Arg228X and Val25Met), a known regulator of the PI3K/AKT/mTOR pathway (Table 1). After 2 months and half of treatment, the patient presented a better control of hypercalcemia (dropping from 12.6 to 13.7 mg/dl before treatment to 10–11 mg/dl) and a stable disease both at the neck and the liver metastases. No long-term effects of treatment could be assessed since the patient voluntarily withdrew from drug use to undergo reoperation of the neck and radiofrequency ablation of multiple liver metastases, which allowed the biochemical and biological control of her disease.
Angiogenesis plays a critical role in the growth of solid tumors that need a blood supply of oxygen and nutrients if they are to grow beyond a few millimeters in size, and several angiogenesis inhibitors are approved to treat various types of human malignancies. Lazaris et al. [44] showed increased angiogenesis in PAs compared with parathyroid proliferative lesions, by positive immunohistochemical staining of three markers of angiogenic endothelial cells, the endoglin (CD105), an endothelial cell proliferation-associated protein, the angiogenesis inductor VEGF, and the VEGF-R2 a tyrosine kinase receptor expressed by endothelial cell precursors. The study of Lazaris et al. did not include PC samples, however, genetic alterations suspected to promote angiogenesis have been reported in PCs, suggesting the possibility to use antiangiogenic drugs to prevent/block tumor growth in primary tumors and matched metastases in a percentage of patients, based on their PC somatic genetic profile. A study of Kang et al. [13] found mutations in the KDR gene, encoding the pro-angiogenic VEGF-R2 protein, in 13% of analyzed PC cases, and mutations in other genes involved in the regulation of angiogenesis were reported in PCs (i.e., EPHB4, PTPRB, VCAN) [5, 14]. Recently, Chen et al. [45] reported that somatic mutations in KDM5C, a gene encoding a lysine histone demethylase and found mutated in PCs by three different studies [5, 9, 13], correlate with high angiogenesis.
Results of off-label treatment with specific antiangiogenic inhibitors, the tyrosine kinase inhibitors (TKIs), were published in six PC case reports [13, 14, 46,47,48], one with a somatic mutation of the KDR gene and one with a somatic mutation of the KDM5C gene, all six showing a positive response to therapy in terms of better control of hypercalcemia, stabilization of cancer, and/or reduction of size of metastases (Table 1). TKIs appear to be a suitable medical therapy for PC, since they not only are effective in suppressing angiogenesis and growth in solid tumors but they were shown to be able to effectively control hypercalcemia and inhibit bone resorption [48].
Clinical and genetic features of off-label treated PC case reports, administered treatment(s) and main outcomes are resumed in Table 1.
Conclusions
The extreme rarity of PC made it impossible to date to have standardized information and guidelines on diagnosis and treatment for primary tumors, advanced and metastatic disease, and recurrences. Pre-operative biochemical and instrumental diagnosis remains a challenge, letting the decision for the most adequate surgical approach only on the judgment of the surgeon based on intra-operative findings about tumor size and aspect, and presence of local and/or vascular invasion. In case of suspicion for possible malignancy, the best initial surgery is the en bloc resection of tumor(s) and all the involved structures in the neck compartment. However, in case of advanced and/or metastatic disease, surgery is often ineffective, and permanence of hypercalcemia and disease recurrence are frequent, associated with a poor prognosis. Control of hypercalcemia is achieved in some inoperable cases by pharmacological treatments with bisphosphonates, denosumab, and calcimimetics, alone or in combination. Radiotherapy and systemic chemotherapy appear to be ineffective for PC, and they are rarely used only in selected cases of metastatic tumors. Few case reports demonstrated the efficacy of some targeted therapies, focusing on the importance of personalized precision medicine based on the somatic genetic profile of PC. Collaborative research and the creation of international multicentre patient databases and tumor biobanks are of vital importance to improve PC diagnosis and optimize treatment options.
References
Y. Gao, P. Wang, J. Lu, B. Pan, D. Guo, Z. Zhang, A. Wang, M. Zhang, J. Sun, W. Wang, Z. Liang, Diagnostic significance of parafibromin expression in parathyroid carcinoma. Hum. Pathol. 127, 28–38 (2022). https://doi.org/10.1016/j.humpath.2022.05.014
S. Leonard-Murali, T. Ivanics, D.S. Kwon, X. Han, C.P. Steffes, R. Shah, Local resection versus radical surgery for parathyroid carcinoma: a national cancer database analysis. Eur. J. Surg. Oncol. 47, 2768–2773 (2021). https://doi.org/10.1016/j.ejso.2021.06.026
W.M. Lo, M.L. Good, N. Nilubol, N.D. Perrier, D.T. Patel, Tumor size and presence of metastatic disease at diagnosis are associated with disease-specific survival in parathyroid carcinoma. Ann. Surg. Oncol. 25, 2535–2540 (2018). https://doi.org/10.1245/s10434-018-6559-6
L.K. Long, R.S. Sippel, Current and future treatment for parathyroid carcinoma. Int. J. Endo. Oncol. 5(1), IJE06 (2018). https://doi.org/10.2217/ije-2017-0011
C.N. Clarke, P. Katsonis, T.K. Hsu, A.M. Koire, A. Silva-Figueroa, I. Christakis, M.D. Williams, M. Kutahyalioglu, L. Kwatampora, Y. Xi, J.E. Lee, E.S. Koptez, N.L. Busaidy, N.D. Perrier, O. Lichtarge, Comprehensive genomic characterization of parathyroid cancer identifies novel candidate driver mutations and core pathways. J. Endocr. Soc. 3(3), 544–559 (2018). https://doi.org/10.1210/js.2018-00043
F. Marini, F. Giusti, G. Palmini, G. Perigli, R. Santoro, M.L. Brandi, Genetics and epigenetics of parathyroid carcinoma. Front. Endocrinol. 13, 834362 (2022). https://doi.org/10.3389/fendo.2022.834362
N.D. Perrier, A. Arnold, J. Costa-Guda, N.L. Busaidy, H. Nguyen, H.H. Chuang, M.L. Brandi, Hereditary endocrine tumours: current state-of-the-art and research opportunities: new and future perspectives for parathyroid carcinoma. Endocr. Relat. Cancer 27(8), T53–T63 (2020). https://doi.org/10.1530/ERC-20-0018
R. Uljanovs, S. Sinkarevs, B. Strumfs, L. Vidusa, K. Merkurjeva, I. Strumfa, Immunohistochemical profile of parathyroid tumours: a comprehensive review. Int. J. Mol. Sci. 23(13), 6981 (2022). https://doi.org/10.3390/ijms23136981
C. Pandya, A.V. Uzilov, J. Bellizzi, C.Y. Lau, A.S. Moe, M. Strahl, W. Hamou, L.C. Newman, M.Y. Fink, Y. Antipin, W. Yu, M. Stevenson, B.M. Cavaco, B.T. The, R.V. Thakker, H. Morreau, E.E. Schadt, R. Sebra, S.D. Li, A. Arnold, R. Chen, Genomic profiling reveals mutational landscape in parathyroid carcinomas. Jci. Insight 2(6), e92061 (2017). https://doi.org/10.1172/jci.insight.92061
L. Zhao, L.H. Sun, D.M. Liu, X.Y. He, B. Tao, G. Ning, J.M. Liu, H.Y. Zhao, Copy number variation in CCND1 gene is implicated in the pathogenesis of sporadic parathyroid carcinoma. World J. Surg. 38(7), 1730–1737 (2014). https://doi.org/10.1007/s00268-014-2455-9
H.S. Park, Y.H. Lee, N. Hong, D. Won, Y. Rhee, Germline mutations related to primary hyperparathyroidism identified by next-generation sequencing. Front. Endocrinol. 13, 853171 (2022). https://doi.org/10.3389/fendo.2022.853171
Y. Hu, X. Zhang, O. Wang, Y. Bi, X. Xing, M. Cui, M. Wang, W. Tao, Q. Liao, Y. Zhao, The genomic profile of parathyroid carcinoma based on whole-genome sequencing. Int. J. Cancer 147(9), 2446–2457 (2020). https://doi.org/10.1002/ijc.33166
H. Kang, D. Pettinga, A.D. Schubert, P.W. Ladenson, D.W. Ball, J.H. Chung, A.B. Schrock, R. Madison, G.M. Frampton, P.J. Stephens, J.S. Ross, V.A. Miller, S.M. Ali, Genomic profiling of parathyroid carcinoma reveals genomic alterations suggesting benefit from therapy. Oncologist 24(6), 791–797 (2019). https://doi.org/10.1634/theoncologist.2018-0334
M. Kutahyalioglu, H.T. Nguyen, L. Kwatampora, C. Clarke, A. Silva, E. Ibrahim, S.G. Waguespack, M.E. Cabanillas, C. Jimenez, M.I. Hu, S.I. Sherman, S. Kopetz, R. Broaddus, R. Dadu, K. Wanland, M. Williams, M. Zafereo, N. Perrier, N.L. Busaidy, Genetic profiling as a clinical tool in advanced parathyroid carcinoma. J. Cancer Res. Clin. Oncol. 145(8), 1977–1986 (2019)
H.L. Robbins, A. Hague, The PI3K/Akt pathway in tumors of endocrine tissues. Front. Endocrinol. 6, 188 (2015). https://doi.org/10.1007/s00432-019-02945-9
S.H. Kong, Updates of genomics and proteomics of parathyroid carcinoma. Endocrines 3, 745–752 (2022). https://doi.org/10.3390/endocrines3040061
A. Riccardi, C. Lemos, R. Ramos, J. Bellizzi, K. Parham, T.C. Brown, R. Korah, T. Carling, J. Costa-Guda, A. Arnold, PIK3CA mutational analysis of parathyroid adenomas. JBMR 4(6), e10360 (2020). https://doi.org/10.1002/jbm4.10360
T. Zhan, N. Rindtorff, M. Boutros, Wnt signaling in cancer. Oncogene 36, 1461–1473 (2017). https://doi.org/10.1038/onc.2016.304
J. Svedlund, M. Aurén, M. Sundström, H. Dralle, G. Akerström, P. Björklund, G. Westin, Aberrant WNT/β-catenin signaling in parathyroid carcinoma. Mol. Cancer 9, 294 (2010). https://doi.org/10.1186/1476-4598-9-294
J. Svedlund, E. Barazeghi, P. Stålberg, P. Hellman, G. Åkerström, P. Björklund, G. Westin, The histone methyltransferase EZH2, an oncogene common to benign and malignant parathyroid tumors. Endocr. Relat. Cancer 21(2), 231–239 (2014). https://doi.org/10.1530/ERC-13-0497
L. Sulaiman, C.C. Juhlin, I.L. Nilsson, O. Fotouhi, C. Larsson, J. Hashemi, Global and gene-specific promoter methylation analysis in primary hyperparathyroidism. Epigenetics 8, 646–655 (2013). https://doi.org/10.4161/epi.24823
L.F. Starker, J. Svedlund, R. Udelsman, H. Dralle, G. Akerström, G. Westin, R.P. Lifton, P. Björklund, T. Carling, The DNA methylome of benign and malignant parathyroid tumors. Genes. Chromosomes Cancer 50, 735–745 (2011). https://doi.org/10.1002/gcc.20895
C.C. Juhlin, N.B. Kiss, A. Villablanca, F. Haglund, J. Nordenström, A. Höög, C. Larsson, Frequent promoter hypermethylation of the APC and RASSF1A tumour suppressors in parathyroid tumours. PLoS ONE 5, e9472 (2010). https://doi.org/10.1371/journal.pone.0009472
J. Svedlund, S. Koskinen Edblom, V.E. Marquez, G. Åkerström, P. Björklund, G. Westin, Hypermethylated in cancer 1 (HIC1), a tumor suppressor gene epigenetically deregulated in hyperparathyroid tumors by histone H3 lysine modification. J. Clin. Endocrinol. Metab. 2012(97), E1307–E1315 (2012). https://doi.org/10.1210/jc.2011-3136
S. Corbetta, V. Vaira, V. Guarnieri, A. Scillitani, C. Eller-Vainicher, S. Ferrero, L. Vicentini, I. Chiodini, M. Bisceglia, P. Beck-Peccoz, S. Bosari, A. Spada, Differential expression of microRNAs in human parathyroid carcinomas compared with normal parathyroid tissue. Endocr. Relat. Cancer 17(1), 135–146 (2010). https://doi.org/10.1677/ERC-09-0134
S. Liu, Z. Wang, Z. Liu, S. Shi, Z. Zhang, J. Zhang, H. Lin, miR-221/222 activate the Wnt/β-catenin signaling to promote triple-negative breast cancer. J. Mol. Cell. Biol. 10(4), 302–315 (2018). https://doi.org/10.1093/jmcb/mjy041
F. Marini, F. Giusti, G. Palmini, C. Aurilia, S. Donati, M.L. Brandi, Parathyroid carcinoma: update on pathogenesis and therapy. Endocrines 4(1), 205–235 (2023). https://doi.org/10.3390/endocrines4010018
B. Guan, J.M. Welch, J.C. Sapp, H. Ling, Y. Li, J.J. Johnston, E. Kebebew, L.G. Biesecker, W.F. Simonds, S.J. Marx, S.K. Agarwal, GCM2-activating mutations in familial isolated hyperparathyroidism. Am. J. Hum. Genet. 99(5), 1034–1044 (2016). https://doi.org/10.1016/j.ajhg.2016.08.018
L. Canaff, V. Guarnieri, Y. Kim, B.Y.L. Wong, A. Nolin-Lapalme, D.E.C. Cole, S. Minisola, C. Eller-Vainicher, F. Cetani, A. Repaci, D. Turchetti, S. Corbetta, A. Scillitani, D. Goltzman, Novel Glial Cells Missing-2 (GCM2) variants in parathyroid disorders. Eur. J. Endocrinol. 186(3), 351–366 (2022). https://doi.org/10.1016/10.1530/EJE-21-0433
A. Song, Y. Yang, Y. Wang, S. Liu, M. Nie, Y. Jiang, M. Li, W. Xia, O. Wang, X. Xing, Germline GCM2 Mutation Screening in Chinese Primary Hyperparathyroidism Patients. Endocr. Pract. 26(10), 1093–1104 (2020). https://doi.org/10.4158/EP-2020-0132
R. Rahbari, A.K. Holloway, M. He, E. Khanafshar, O.H. Clark, E. Kebebew, Identification of differentially expressed microRNA in parathyroid tumors. Ann. Surg. Oncol. 18(4), 1158–1165 (2011). https://doi.org/10.1245/s10434-010-1359-7
J. Krupinova, N. Mokrysheva, V. Petrov, E. Pigarova, A. Eremkina, E. Dobreva, A. Ajnetdinova, G. Melnichenko, A. Tiulpakov, Serum circulating miRNA-342-3p as a potential diagnostic biomarker in parathyroid carcinomas: a pilot study. Endocrinol. Diabetes Metab. 4(4), e00284 (2021). https://doi.org/10.1002/edm2.284
C. Verdelli, I. Forno, V. Vaira, S. Corbetta, MicroRNA deregulation in parathyroid tumours suggests an embryonic signature. J. Endocrinol. Investig. 38(4), 383–388 (2015). https://doi.org/10.1007/s40618-014-0234-y
A. Morotti, I. Forno, C. Verdelli, V. Guarnieri, F. Cetani, A. Terrasi, R. Silipigni, S. Guerneri, V. Andrè, A. Scillitani, L. Vicentini, S. Ferrero, S. Corbetta, V. Vaira, The oncosuppressors MEN1 and CDC73 are involved in lncRNA deregulation in human parathyroid tumors. J. Bone Miner. Res 35(12), 2423–2431 (2020). https://doi.org/10.1002/jbmr.4154
A. Morotti, F. Cetani, G. Passoni, S. Borsari, E. Pardi, V. Guarnieri, C. Verdelli, G.S. Tavanti, L. Valenti, C. Bianco, S. Ferrero, S. Corbetta, V. Vaira, The long non-coding BC200 is a novel circulating biomarker of parathyroid carcinoma. Front. Endocrinol. 13, 869006 (2022). https://doi.org/10.3389/fendo.2022.869006
E.A. Asare, C. Sturgeon, D.J. Winchester, L. Liu, B. Palis, N.D. Perrier, D.B. Evans, D.P. Winchester, T.S. Wang, Parathyroid carcinoma: an update on treatment outcomes and prognostic factors from the National Cancer Data Base (NCDB). Ann. Surg. Oncol. 22(12), 3990–3995 (2015). https://doi.org/10.1245/s10434-015-4672-3
F. Cetani, E. Pardi, C. Marcocci, Parathyroid carcinoma. in Parathyroid Disorders. Focusing on Unmet Needs ed. by M.L. Brandi Front. Horm. Res., Kager. 51, pp. 63–76 (2019). https://doi.org/10.1159/isbn.978-3-318-06409-4
S. Storvall, E. Ryhänen, F.V. Bensch, I. Heiskanen, S. Kytölä, T. Ebeling, S. Mäkelä, C. Schalin-Jäntti, Recurrent metastasized parathyroid carcinoma-long-term remission after combined treatments with surgery, radiotherapy, cinacalcet, zoledronic acid, and temozolomide. JBMR 3(4), e10114 (2018). https://doi.org/10.1002/jbm4.10114
S. Storvall, E. Ryhänen, I. Heiskanen, T. Vesterinen, F.V. Bensch, J. Schildt, S. Kytölä, A. Karhu, J. Arola, C. Schalin-Jäntti, MGMT promoter methylation and parathyroid carcinoma. J. Endocr. Soc. 3(11), 2114–2122 (2019). https://doi.org/10.1210/js.2019-00175
S.J. Silverberg, M.R. Rubin, C. Faiman, M. Peacock, D.M. Shoback, R.C. Smallridge, L.E. Schwanauer, K.A. Olson, P. Klassen, J.P. Bilezikian, Cinacalcet hydrochloride reduces the serum calcium concentration in inoperable parathyroid carcinoma. J. Clin. Endocrinol. Metab. 92(10), 3803–3808 (2007). https://doi.org/10.1210/jc.2007-0585
Y. Takeuchi, S. Takahashi, D. Miura, M. Katagiri, N. Nakashima, H. Ohishi, R. Shimazaki, Y. Tominaga, Cinacalcet hydrochloride relieves hypercalcemia in Japanese patients with parathyroid cancer and intractable primary hyperparathyroidism. J. Bone Miner. Metab. 35(6), 616–622 (2017). https://doi.org/10.1007/s00774-016-0797-0
T. Tian, X. Li, J. Zhang, mTOR signaling in cancer and mTOR inhibitors in solid tumor targeting therapy. Int. J. Mol. Sci. 20(3), 755 (2019). https://doi.org/10.3390/ijms20030755
A.C. Lazaris, S. Tseleni-Balafouta, T. Papathomas, T. Brousalis, G. Thomopoulou, G. Agrogiannis, E.S. Patsouris, Immunohistochemical investigation of angiogenic factors in parathyroid proliferative lesions. Eur. J. Endocrinol. 154(6), 827–833 (2006). https://doi.org/10.1530/eje.1.02168
X.J. Chen, A.Q. Ren, L. Zheng, E.D. Zheng, Predictive value of KDM5C alterations for immune checkpoint inhibitors treatment outcomes in patients with cancer. Front. Immunol. 12, 664847 (2021). https://doi.org/10.3389/fimmu.2021.664847
L. Rozhinskaya, E. Pigarova, E. Sabanova, E. Mamedova, I. Voronkova, J. Krupinova, L. Dzeranova, A. Tiulpakov, V. Gorbunova, N. Orel, A. Zalian, G. Melnichenko, I. Dedov, Diagnosis and treatment challenges of parathyroid carcinoma in a 27-year-old woman with multiple lung metastases. Endocrinol. Diabetes Metab. Case Rep. 2017, 16–0113 (2017). https://doi.org/10.1530/EDM-16-0113
H. Makino, M. Notsu, I. Asayama, H. Otani, M. Morita, M. Yamamoto, M. Yamauchi, M. Nakao, H. Miyake, A. Araki, S. Uchino, K. Kanasaki, Successful control of hypercalcemia with sorafenib, evocalcet, and denosumab combination therapy for recurrent parathyroid carcinoma. Intern. Med. 61(22), 3383–3390 (2022). https://doi.org/10.2169/internalmedicine.9261-21
N. Alharbi, S.L. Asa, M. Szybowska, R.H. Kim, S. Ezzat, Intrathyroidal parathyroid carcinoma: an atypical thyroid lesion. Front. Endocrinol. 9, 641 (2018). https://doi.org/10.3389/fendo.2018.00641
K. Vandyke, S. Fitter, J. Drew, S. Fukumoto, C.G. Schultz, N.A. Sims, D.T. Yeung, T.P. Hughes, A.C. Zannettino, Prospective histomorphometric and DXA evaluation of bone remodeling in imatinib-treated CML patients: evidence for site-specific skeletal effects. J. Clin. Endocrinol. Metab. 98(1), 67–76 (2013). https://doi.org/10.1210/jc.2012-2426
Author information
Authors and Affiliations
Contributions
MLB, FM, and FG contributed to the review conception and design. Data research and collection from published literature were performed by GP, CAeSD. The first draft of the manuscript was written by FM, and revised by FG and MLB. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marini, F., Giusti, F., Palmini, G. et al. Parathyroid carcinoma: molecular therapeutic targets. Endocrine 81, 409–418 (2023). https://doi.org/10.1007/s12020-023-03376-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03376-w