Abstract
Context
Parathyroid carcinoma (PC) is a rare endocrine malignancy with no approved systemic therapies for unresectable locally invasive or distant metastatic disease. Understanding the molecular changes in advanced PC can provide better understanding of this disease and potentially help directing targeted therapy.
Objective
To evaluate tumor-specific genetic changes using next-generation sequencing (NGS) panels.
Design
All patients with advanced PC were tested for hot-spot panels using NGS panels including a 50-gene panel, a 409-gene panel if the standard 50-gene panel (Ion Torrent, Life Technology) was negative or a FoundationOne panel.
Setting
The University of Texas MD Anderson Cancer Center, Houston, Texas, USA.
Patients or other participants
11 patients with advanced PC were selected to undergo molecular testing.
Main outcome measure(s)
Genetic profiles of advanced PC.
Results
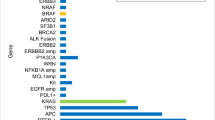
Among the 11 patients, 4 patients had the 50-gene panel only, 6 had 409-gene panel after a negative 50-gene panel and 1 had FoundationOne. One patient who had 50-gene panel only also had his metastatic site (esophagus) of his tumor tested with FoundationOne. The most common mutations identified were in the PI3 K (PIK3CA, TSC1 and ATM) (4/11 patients) and TP53 (3/11) pathways. Genes not previously reported to be mutated in PC included: SDHA, TERT promoter and DICER1. Actionable mutations were found in 54% (6/11) of the patients.
Conclusions
Mutational profiling using NGS panels in advanced PC has yielded important potentially targetable genetic alterations. Larger studies are needed to identify commonly mutated genes in advanced PC patients. Development of novel therapies targeting these cellular pathways should be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parathyroid carcinoma (PC) is a rare endocrine malignancy that has poorly understood risk factors and carries significant morbidity. PC-related death usually results from unremitting hypercalcemia and its complications rather than tumor burden. Surgical resection is the main modality of treatment (Cetani et al. 2016). Because no definitive diagnostic markers exist to differentiate PC from benign disease, parathyroid tumors are resected en bloc. However, initial surgical intervention is usually not curative, and PC tends to persist or recur locoregionally or metastasize to distant organs (Cetani et al. 2016; Schulte and Talat 2012; Busaidy et al. 2004). When local recurrence occurs, subsequent surgeries are hampered by scarring and fibrosis from previous operations and/or external beam radiation therapy.
Medical management using anti-resorptive therapies and/or calcimimetic agents to control hypercalcemia is often transient and unsuccessful. There is no evidence that controlling hypercalcemia with these medications modifies the outcome of the disease such as slowing the progression or prolonging survival for patients with PC (Cetani et al. 2016).
The etiology of PC is largely unknown. Due to the lack of studies and the rarity of cases, it is not known whether the disease arises de novo or from parathyroid adenoma. PC is usually a sporadic disease, but familial cases have been reported in the literature. Germline mutations in the tumor suppressor gene CDC73 (also known as HRPT2) are seen in hyperparathyroidism-jaw tumor (HPT-JT) and familial isolated primary hyperparathyroidism, and somatic mutations of CDC73 are well known to develop in sporadic cases of PC (Jackson et al. 1993). Indeed, CDC73 mutations have been reported in 15–100% of sporadic PC cases, compelling the necessity for routine germline screening (Schulte and Talat 2012; Frank-Raue et al. 2011; Shattuck et al. 2003). Although rare, PC or atypical parathyroid neoplasia was reported in patients with MEN1 (also called multiple endocrine neoplasia I) syndrome (Agha et al. 2007; Christakis et al. 2016). Other genes and/or their encoded proteins reported to be associated with PC are RB1 (which encodes retinoblastoma protein), CCND1 (also known as cyclin D1 and PRAD1), TP53, and BRCA2 (Cetani et al. 2004; Cetani et al. 2016; Schulte and Talat 2012; Agha et al. 2007; Yu et al. 2015; Cryns et al. 1994).
Recent findings of whole-exome sequencing in patients with sporadic PC and local invasion or distant metastasis revealed previously unrecognized mutations. Mutations were reported in the following genes PRUNE2, ADCK1, APOBEC, FAT3, and TNRC6A (Yu et al. 2015; Pandya et al. 2017). NF1, KDR, and PTEN mutations have also been recently reported in PC (Kang et al. 2017). However, larger sample cohorts are clearly required to validate these findings.
Owing to the rarity and low prevalence of PC and the lack of recognized targetable molecular drivers for the disease, no data exist from therapeutic trials to guide therapy for advanced cases. Cytotoxic chemotherapy is ineffective, and external beam radiation therapy only adds value in very select cases of PC following surgery (Cetani et al. 2016; Schulte and Talat 2012; Christakis et al. 2017). When PC becomes widely metastatic and surgical options are no longer available, clinical management of hypercalcemia becomes the main line of therapy. Molecular profiling of advanced PC cases may enable a more precise diagnosis of the disease and perhaps more importantly provide novel treatment opportunities through targeted therapy. Next-generation sequencing (NGS) panels are now routinely used to screen for mutations to help diagnose and guide the treatment of thyroid, colorectal, lung, brain, and ovarian cancers as well as melanoma and other solid cancers (Singh et al. 2013, 2014).
Understanding the molecular aberrations in PC is crucial to inform the selection of targeted therapy and develop new targeted chemotherapeutic agents. The objective of our study is to analyze genetic profiles and identify mutations that may be targeted in recurrent or persistent and/or metastatic PC. We also present two cases with their mutation profile, choice of systemic therapy based on mutated pathways and their response to demonstrate the importance of understanding PC at the molecular and genetic level.
Patients and methods
This study was approved by the Institutional Review Board of the University of Texas MD Anderson Cancer Center (UTMDACC). All patients consented to participate in the study. Patients with an unequivocal diagnosis of PC based on World Health Organization criteria (DeLellis 2004) and with evidence of local recurrence or distant metastatic disease requiring further therapy at the UTMDACC between July 2014 and January 2016 were selected to undergo molecular testing. All laboratory and molecular testing was performed a part of their routine medical care.
Somatic mutation of tumors was performed in a stepwise manner to increase its ability to find mutational signatures present in few samples as well as mutational signatures exhibiting a low mutational burden (Fig. 1). In 10 of the 11 patients, the tumor was initially sequenced using a 50-gene panel (Ion Torrent, Life Technology). Of individuals who initially tested negative on the 50-gene panel, more comprehensive testing was performed. Six out of the seven patients with no mutation detected on 50-gene panel consented and enrolled for more comprehensive gene studies in which their tumor and paired germline were sequenced with a 409-full-length gene panel (Ion Proton) in the setting of an institutional wide study (Kopetz et al. 2015). Among the ten patients who initially had testing with 50-gene panel, a single patient had follow up tumor testing performed using the FoundationOne NGS panel as part of his clinical work up. One patient out of the total 11 had his tumor testing with FoundationOne as the only gene panel. All three gene panels in this study including 50-gene, 409-gene and FoundationOne were CAP accredited and CLIA approved.
The 409-gene panel is a comprehensive cancer gene panel of 409 full exomes of oncogenes and tumor suppressor genes that are frequently cited in cancer research. Genes tested in the standard 50-gene panel are also included in the 409-gene panel (https://www.thermofisher.com/order/catalog/product/4475346; https://www.thermofisher.com/order/catalog/product/4477685). The 409-gene panel is typically used if no targetable mutations were identified by the standard 50-gene panel and the patient experiences recurrence or residual disease with standard therapy (Singh et al. 2014). It is also known as the Cancer Mutational Scan 400. The genomic reference sequence used is genome GRCh37/hg19. The presence of visualized variants is read against the reference genome to denounce strand biases and sequencing errors.
The 50-gene and 409-gene panels only detect single nucleotide substitutions and small insertions or deletions. They do not cover gene rearrangements or copy number variations. FoundationOne NGS panel, on the other hand, provides data on single nucleotide substitutions, gene rearrangements, copy number variations, insertions or deletions and also information on microsatellite instability/stability and tumor burden (https://assets.ctfassets.net/vhribv12lmne/6YRrchSINOeSu48YwuesoY/0c3651c8421fa3647ccede76de9dce61). The 50-gene and FoundationOne panels did not have normal paired control samples from the same patient, while the 409-gene panel did include normal paired control samples in each patient. Therefore, germline mutations cannot be excluded in the patients who only had their tumor tested using the 50-gene or FoundationOne panel.
For clinical purposes, the effective lower limit of detection of the assay for single nucleotide variations (analytical sensitivity) was in the range of 5–10% by taking into consideration the depth of coverage at a given base and the ability to confirm low-level mutations using independent conventional platforms. All detected mutations were cross-checked with COSMIC and dbSNP genomic databases.
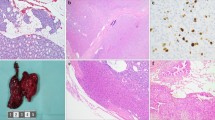
Pathologists in MD Anderson’s Tissue Qualification Laboratory identified the optimal formalin-fixed, paraffin-embedded tissue blocks for the study. Tumor samples could be from primary and recurrent disease. From each paraffin block, a hematoxylin- and eosin-stained slide and unstained section were prepared. The tumor tissue was dissected from unstained section using the stained slide as template. DNA was then extracted from dissected tumor tissue using a QIAamp DNA FFPE Tissue Kit (Qiagen) and used for sequencing of genes in a 409-gene panel. All procedures were well established for the testing of solid tumors.
Results
Patient characteristics
Eleven patients with advanced PC requiring therapy were included in the study. Their demographic and clinical characteristics are shown in Table 1. The median patient age was 51 years and six patients were women. The median highest serum parathyroid hormone level detected was 855 pg/mL [range 119–476,622 pg/mL (normal range (nl): 9–80)], and the median highest serum calcium level was 13.6 mg/dL (range 11.4–16.8 mg/dL (nl: 8.4–10.2). All 11 patients had neck recurrence or persistent neck disease; however, six patients had distant metastasis, namely in the lung, liver, and/or bone. All the patients underwent multiple neck surgeries (median 3; range 2–4); however, only two patients received radiation therapy to the neck after initial surgery. Six patients received systemic chemotherapy, of which three had more than one chemotherapeutic regimen. At last follow-up, nine of the patients were still living with disease, and two patients had died of PC. One patient reported a family history of benign parathyroid disease, and another patient reported a family history of an unknown type of neck tumor.
Mutational analysis
Mutation analysis results of the 11 patients are summarized in Table 2. All of the specimen sites sent for molecular studies were from sites with recurrent or persistent disease. In 8 out of 11 patients, mutations were detected. TP53 and PIK3CA were the only genes found to be recurrently mutated in PC patients, 3 and 2, respectively. When pathways were considered, four patients had mutations within PI3 K pathway (PIK3CA, TSC1 and ATM). Three patients had mutations involving multiple genes. In one of these patients, somatic mutations were found in the MEN1, TERT promoter and DICER1 genes. A second patient had multiple genetic alterations in several genes (TP53, TSC1, BCL2L1, DCC, EP300, EPHB4, GUCY1A2, KDM6A, MAGI1, POT1, RNASEL). A distinct somatic mutation in the tumor suppressor gene CDC73 was detected in one patient who had familial hyperparathyroidism-jaw tumor syndrome. His CDC73 germline mutation was R76X. This patient’s tumor harbored a different pathogenic somatic mutation in the CDC73 gene which was Y55C. No other patients in our cohort had somatic or germline CDC73 mutations. In this study, we also did not find any other familial gene mutations linked to PC (i.e., MEN1 or RET mutations). One patient had a mutation detected in the ATM gene, labeled a variant of unknown significance in 50-gene panel (left thyroid bed tissue) and subsequently had his metastatic tumor (esophagus) test positive SDHA gene mutation in FoundationOne platform. A single patient had no mutation detected in 50-gene panel but declined to enroll in the 409-panel study.
Case studies
Two case examples illustrate how mutational profiles can direct the use of systemic therapies. Described below are the biological reasons of choosing targeted therapy options and the clinical course and outcomes derived from those choices.
Patient No. 5 is a female who was diagnosed with PC at age of 47 years. She initially presented with hypercalcemia (serum calcium 12–14 mg/dl (nl: 8.4–10.2)) and hyperparathyroidism (PTH 320–350 pg/ml (nl: 9–80)). The patient underwent parathyroidectomy and hemithyroidectomy which initially resolved her hypercalcemia. She had a recurrence of her PC (calcium ranging between 12.6 and 13.7 mg/dl) which was treated with neck dissection. Subsequently, she was diagnosed with liver metastasis. Tumor testing identified somatic mutations in TP53 and TSC1, and several other genes (BCL2L1, DCC, EP300, EPHB4, GUCY1A2, KDM6A, MAGI1, POT1, RNASEL) (Table 2). The presence of the TSC1 mutation, a known regulator of the PI3 K/mTOR pathway, provided support for systemic therapy with an mTOR inhibitor. Additionally, because VEGF has been shown to be overexpressed in parathyroid tumors in general, and thought to be a driver (Lazaris et al. 2006), vandetanib (an antiangiogenic drug) and everolimus (mTOR inhibitor) were started. The patient’s best response to treatment was stable disease (observed at two and a half months) and her serum calcium levels were better controlled (10–11 mg/dL) while on drug. She voluntarily withdrew from drug use to attempt surgical metastasectomy of her liver and neck lesions (her only two sites of disease). She also had percutaneous radiofrequency ablations for liver metastases as well as reoperation in the neck with superior mediastinal lymph node and thymus resection, which helped control her disease structurally and biochemically.
Patient No. 7 is a male who was diagnosed with HPT-JT syndrome at age of 57 years. At diagnosis, his serum calcium level was 13 mg/dl with an elevated PTH level of 698 pg/ml. He initially underwent parathyroidectomy of 1 gland and followed by thyroidectomy and removal of other parathyroid glands due to persistent hyperparathyroidism and hypercalcemia. He was later found to have repeat calcium levels in the 15–17 mg/dL range and renal insufficiency (GFR 53) which was linked to recurrent neck disease and pulmonary metastases. These were treated with lung segmentectomy and multiple wedge resections. His hypercalcemia, despite treatment with cinacalcet, intermittent doses of bisphosphonate therapy and intravenous fluids, remained high (12–15 mg/dl with PTH ranging between 710 and 807 pg/ml). In an attempt to identify targets for systemic therapy, mutational profiling was ordered. The 50- and 409-gene panels identified a pathogenic somatic mutation in the CDC73 gene (Y55C). His germline testing was performed as a routinely recommended procedure in our clinic. He was found to have a distinct germline mutation in the CDC73 gene (R76X). The identification of this mutation confirmed his HPT-JT syndrome diagnosis and also supported the two-hit hypothesis in oncogenesis (Knudson 2001). Additional somatic mutation of KDM5C gene was also found. Given evidence that in renal cell carcinoma patients with KDM5C mutations have positive responses with first-line sunitinib, a potent inhibitor of all VEGF and PDGF receptors (Hsieh et al. 2017; Le Tourneau et al. 2007), an antiangiogenic drug was considered for therapy. The patient was treated with sorafenib, which is an antiangiogenic multi-targeted tyrosine kinase inhibitor with a target profile similar to sunitinib (Nexavar prescibing information 2018). Initially, the patient’s hypercalcemia and hyperparathyroidism were well controlled. He became hypocalcemic after 3 months so his cinacalcet was discontinued and remained normocalcemic despite radiography that his neck and lung tumors showed a stable rather than reducing response to treatment. After 3 years on sorafenib therapy, however, his calcium and parathyroid hormone levels started to rise again with progression of disease in the lungs. At this time, his serum calcium was 12.8 mg/dl and PTH was markedly elevated to 1471 pg/ml. Sorafenib was discontinued and a second more potent antiangiogenic inhibitor lenvatinib was initiated (Matsui et al. 2008). The patient has been on lenvatinib for 20 months with radiographically stable disease. Furthermore, his calcium level is well controlled at 9–10 mg/dL without any calcimimetic medication.
Discussion
In this study, we used NGS panels to identify mutations in patients with advanced persistent or recurrent and/or metastatic PC. The majority of the mutations found in our study were loss of function of tumor suppressor genes rather than gain of function mutations of oncogenes (Table 2). Genetic changes in PI3 K and TP53 pathways, which are the common mutations found in advanced PC and similar to what has been reported in other published studies were found in our studies. In addition, new mutations that have not been reported in PC were also identified.
Mutation of TP53, which encodes p53 transcription factor, is the most studied cancer-causing somatic mutation and is associated with many types of cancer, including PC (Stracquadanio et al. 2016). It has been shown to play an important role in multiple cellular processes such as transcriptional regulation, microRNA processing, cell cycle control, and apoptosis (Stracquadanio et al. 2016). We found TP53 somatic mutations in three patients in our cohort. Despite many efforts and ongoing research, targeted therapy for p53 has not yet been identified (Khoo et al. 2014).
The PIK3CA gene encodes the 110 kDa subunit of phosphatidylinositol 3-kinase (PI3 K). The PI3 K/AKT/mTOR pathway is a well-characterized cancer driver pathway. It has crucial roles in cell growth and proliferation and cell survival and is regulated through phosphorylation of key pathway components (Cantley 2002). Mutations of PIK3CA have been studied extensively in breast cancer, colorectal cancer, non-small cell lung cancer, ovarian cancer, thyroid cancer and other solid tumors (Yuan and Cantley 2008;Liu et al. 2008; Shayesteh et al. 1999). It also has been reported in PCs (Pandya et al. 2017; Kasaian et al. 2013). Interestingly, in a single case study by Kasaian et al. (2013), PIK3CA mutation was found in the primary but not recurrent tumor which suggests the role of PIK3CA mutation in tumor initiation. However, the mechanism and meaning of the loss of activating mutation of PIK3CA in recurrent tumor like in this case is not clear. Several inhibitors of PI3 K and AKT are currently being studied in clinical trials (Owonikoko and Khuri 2013).
A distinct somatic mutation in the tumor suppressor gene CDC73 was detected in one patient who had familial HPT-JT syndrome. CDC73 mutations have been previously detected in patients with HPT-JT and also reported in 20–29% of individuals with apparently sporadic PC (Jackson et al. 1993). Interestingly, no other patients in our cohort had somatic or germline CDC73 mutations. In this study, we also did not find any other familial gene mutations linked to PC (i.e., MEN1 or RET mutations).
In this cohort, we identified two patients (patient 5 and 7) with alterations in histone lysine demethylases (KDM genes). KDMs have been observed to be overexpressed/amplified or mutated in other cancers such as hepatocellular carcinoma and kidney cancer (Ji et al. 2015; Hakimi et al. 2013) and have been linked to worse prognosis in some cases (Paolicchi et al. 2013). KDM5C gene is located on chromosome X (Wu et al. 1994). KDM5C loss of function mutations have been reported to be more common in males by escaping X-inactivation (Dunford et al. 2017). Single-allele mutations of KDM5C gene might be more relevant in male than female patients with regard to clinical presentation and therapeutic consideration (Hsieh et al. 2017). Patient 7 who harbored a KDM5C mutation in our study was also a male. He demonstrated stabilization of their tumor growth and good control of their hypercalcemia from anti-VEGF therapy as presented above. This single patient observation will require studies in an expanded population to determine if KDM gene mutation should be used to drive therapy selection or if the antiangiogenic agents should be broadly considered to treat PC.
A single patient within our cohort had a TSC1 gene mutation. This tumor suppressor gene that encodes hamartin, forms the harmartin–tuberin complex that is responsible for the mTOR activity (Curatolo and Maria 2013). Consequently, mTOR increases if the hamartin–tuberin complex is impaired, resulting in dysplasia, angiogenesis, and tumorigenesis (Huang and Manning 2008). The role of TSC1 in tumorigenesis is highlighted in several cases of bladder cancers (Guo et al. 2013; Hornigold et al. 1999). To our knowledge, TSC1 mutation has not been reported in PC. Recently, mTOR inhibitors have been reported to be effective for the treatment of tumors with TSC1 mutations (Iyer et al. 2012) and TSC2 mutations (Huynh et al. 2015). However, despite the promising results attained with everolimus, the occurrence of resistance to mTOR inhibitors is not uncommon (Bihani et al. 2015).
Mutations in SDHA, TERT promoter and DICER1 genes have been reported and studied in other endocrine neoplasia disorders and for the first time reported in PC in this study.
SDHA gene is known as a tumor suppressor gene which plays an important role in the tumorigenesis of pheochromocytoma and paraganglioma (Burnichon et al. 2010). SDHA mutations can also be associated with pituitary adenoma and gastrointestinal stromal tumors ( Dwight et al. 2013a, b). SDHA mutations have not been reported in parathyroid carcinoma. In this study, the SDHA mutation was found in a metastatic site (esophagus) of the tumor. SDHA gene is not included in the 50-gene panel, therefore it is not clear if this was a secondary mutation acquired during his disease progression or had been present in the original tumor.
TERT promoter mutations are relatively common with high frequency in many cancers including the central nervous system, thyroid, bladder and melanoma (Vinagre et al. 2013). The coexistence of TERT mutations with others or their polymorphisms can serve as prognostic factors in certain malignancies, for example, thyroid cancer and primary glioblastoma (Xing et al. 2014; Mosrati et al. 2015). It has been rarely reported in atypical parathyroid adenoma (Haglund et al. 2015) but has never been reported in parathyroid carcinoma. Given the potential therapeutic effects of inhibiting overexpressed telomerase activity in tumor growth, several agents targeting telomerase enzyme in TERT mutated cancers are being studied (Celeghin et al. 2016; Burchett et al. 2014).
DICER1 gene is involved in the modulation of gene expression at the posttranscriptional level through the regulation of microRNAs. Mutations in this gene have been identified in various cancers. Germline loss of function mutations in DICER1 is the hallmark of a tumor susceptibility syndrome, in which individuals carrying the mutations are at higher risk of developing cancers such as cystic nephroma, pleuropulmonary blastoma, pinealblastoma and ovarian sex-cord stromal tumors (Foulkes et al. 2014). DICER 1 mutations have not been described in PC.
Our study is the first to report mutations in SDHA, TERT promoter and DICER1 genes in patients with advanced PC. In our cohort, we also found other gene mutations such as BCL2L1, DCC, EP300, EPHB4, GUCY1A2, MAF11, POT1, RNASEL, ATM, and TLR4. Each has been reported elsewhere to have a role in certain malignancy such as colorectal cancer (DCC) (Gotley et al. 1996), melanoma (POT1) (Robles-Espinoza et al. 2014), lymphoma (ATM) (Schaffner et al. 2000), and prostate cancer (RNASEL) (Rokman et al. 2002). Given that in our study, these mutations were found in a single tumor, the significance of these gene mutations in PC is not quite understood at this point. It will be helpful to perform further studies to elucidate the molecular mechanisms of these mutations in PC tumorigenesis.
Identifying genetic mutations responsible for tumor formation and growth could be crucial in understanding cancer biology and subsequently choosing a systemic therapy for PC patients. In our study, potential actionable mutations were identified in 6/11 (54%) patients (patient 1, 4, 5,6, 7 and 11). ATM, PIK3, TSC, NF1 genetic mutations were potentially targetable in the mTOR/PIK3 pathways. As in the above discussion, there are targeted therapies which have been known to be effective in non-PC tumors with similar mutated genetic pathways. None of these targeted therapies have been approved by the Food and Drug Administration to use for PC. However, in the setting of no established systemic therapies in advanced PC, these therapies can be considered. Genetic testing can yield important information in understanding tumor formation and development as well as guiding the selection of targeted therapies. In this manuscript, we described two case examples of using NGS as a clinical tool to guide targeted therapies. Using this approach, our group now has treated other patients with advanced PC with some success.
It is important to note that our study has limitations. First of all, it is a small study. Given that we examined 11 patients, the identified genes may not have been the driver genes of PC in all cases. However, PC is such a rare disease that conducting a study with a large number of patients is a challenging task. These data are useful, but genetic screening should be done in larger groups of patients. Secondly, the 50-gene and 409-gene panels, despite being extensive panels at this current time point, do not cover all potential genetic defects and most notably do not test for gene rearrangements or copy number variations.
Conclusion
In conclusion, this is the first study to use 50- and 409- gene panels to identify actionable mutations in patients with persistent recurrent and/or metastatic PC that require systemic therapy. Gene analysis may be a useful clinical tool for directing targeted therapy for advanced PC patients. Larger studies are needed to validate these findings and identify targetable mutations in PC patients. Clinical trials targeting these mutations are warranted including the development of new therapies targeting identified mutations.
References
Agha A, Carpenter R, Bhattacharya S, Edmonson SJ, Carlsen E, Monson JP (2007) Parathyroid carcinoma in multiple endocrine neoplasia type 1 (MEN1) syndrome: two case reports of an unrecognised entity. J Endocrinol Invest 30(2):145–149
Bihani T, Ezell SA, Ladd B, Grosskurth SE, Mazzola AM, Pietras M, Reimer C, Zinda M, Fawell S, D’Cruz CM (2015) Resistance to everolimus driven by epigenetic regulation of MYC in ER+breast cancers. Oncotarget 6(4):2407–2420
Burchett KM, Yan Y, Ouellette MM (2014) Telomerase inhibitor imetelstat (GRN163L) limits the lifespan of human pancreatic cancer cells. PLoS One 9(1):e85155
Burnichon N, Briere JJ, Libe R, Vescovo L, Riviere J, Tissier F, Jouanno E, Jeunemaitre X, Benit P, Tzagoloff A, Rustin P, Bertherat J, Favier J, Gimenez-Roqueplo AP (2010) SDHA is a tumor suppressor gene causing paraganglioma. Hum Mol Genet 19(15):3011–3020
Busaidy NL, Jimenez C, Habra MA, Schultz PN, El-Naggar AK, Clayman GL, Asper JA, Diaz EM Jr, Evans DB, Gagel RF, Garden A, Hoff AO, Lee JE, Morrison WH, Rosenthal DI, Sherman SI, Sturgis EM, Waguespack SG, Weber RS, Wirfel K, Vassilopoulou-Sellin R (2004) Parathyroid carcinoma: a 22-year experience. Head Neck 26(8):716–726
Cantley LC (2002) The phosphoinositide 3-kinase pathway. Science 296(5573):1655–1657
Celeghin A, Giunco S, Freguja R, Zangrossi M, Nalio S, Dolcetti R, De Rossi A (2016) Short-term inhibition of TERT induces telomere length-independent cell cycle arrest and apoptotic response in EBV-immortalized and transformed B cells. Cell Death Dis 7(12):e2562
Cetani F, Pardi E, Viacava P, Pollina GD, Fanelli G, Picone A, Borsari S, Gazzerro E, Miccoli P, Berti P, Pinchera A, Marcocci C (2004) A reappraisal of the Rb1 gene abnormalities in the diagnosis of parathyroid cancer. Clin Endocrinol (Oxf) 60(1):99–106
Cetani F, Pardi E, Marcocci C (2016) Update on parathyroid carcinoma. J Endocrinol Invest 39(6):595–606
Christakis I, Busaidy NL, Cote GJ, Williams MD, Hyde SM, Silva Figueroa AM, Kwatampora LJ, Clarke CN, Qiu W, Lee JE, Perrier ND (2016) Parathyroid carcinoma and atypical parathyroid neoplasms in MEN1 patients; a clinico-pathologic challenge The MD Anderson case series and review of the literature. Int J Surg 31:10–16
Christakis I, Silva AM, Williams MD, Garden A, Grubbs EG, Busaidy NL, Lee JE, Perrier ND, Zafereo M (2017) Postoperative local-regional radiation therapy in the treatment of parathyroid carcinoma: the MD Anderson experience of 35 years. Pract Radiat Oncol 7(6):e463–e470
Cryns VL, Rubio MP, Thor AD, Louis DN, Arnold A (1994) p53 abnormalities in human parathyroid carcinoma. J Clin Endocrinol Metab 78(6):1320–1324
Curatolo P, Maria BL (2013) Tuberous sclerosis. Handb Clin Neurol 111:323–331
DeLellis R (2004) Pathology and genetics of tumours of endocrine organs. IARC Press, Lyon, France
Dunford A, Weinstock DM, Savova V, Schumacher SE, Cleary JP, Yoda A, Sullivan TJ, Hess JM, Gimelbrant AA, Beroukhim R, Lawrence MS, Getz G, Lane AA (2017) Tumor-suppressor genes that escape from X-inactivation contribute to cancer sex bias. Nat Genet 49(1):10–16
Dwight T, Mann K, Benn DE, Robinson BG, McKelvie P, Gill AJ, Winship I, Clifton-Bligh RJ (2013a) Familial SDHA mutation associated with pituitary adenoma and pheochromocytoma/paraganglioma. J Clin Endocrinol Metab 98(6):E1103–E1108
Dwight T, Benn DE, Clarkson A, Vilain R, Lipton L, Robinson BG, Clifton-Bligh RJ, Gill AJ (2013b) Loss of SDHA expression identifies SDHA mutations in succinate dehydrogenase-deficient gastrointestinal stromal tumors. Am J Surg Pathol 37(2):226–233
Foulkes WD, Priest JR, Duchaine TF (2014) DICER1: mutations, microRNAs and mechanisms. Nat Rev Cancer 14(10):662–672
FoundationOne. https://assets.ctfassets.net/vhribv12lmne/6YRrchSINOeSu48YwuesoY/0c3651c8421fa3647ccede76de9dce61/MKT-0054-02_F1_TechSpecs_digital.pdf. [3/27/2018]
Frank-Raue K, Haag C, Schulze E, Keuser R, Raue F, Dralle H, Lorenz K (2011) CDC73-related hereditary hyperparathyroidism: five new mutations and the clinical spectrum. Eur J Endocrinol 165(3):477–483
Gotley DC, Reeder JA, Fawcett J, Walsh MD, Bates P, Simmons DL, Antalis TM (1996) The deleted in colon cancer (DCC) gene is consistently expressed in colorectal cancers and metastases. Oncogene 13(4):787–795
Guo Y, Chekaluk Y, Zhang J, Du J, Gray NS, Wu CL, Kwiatkowski DJ (2013) TSC1 involvement in bladder cancer: diverse effects and therapeutic implications. J Pathol 230(1):17–27
Haglund F, Juhlin CC, Brown T, Ghaderi M, Liu T, Stenman A, Dinets A, Prasad M, Korah R, Xu D, Carling T, Larsson C (2015) TERT promoter mutations are rare in parathyroid tumors. Endocr Relat Cancer 22(3):L9
Hakimi AA, Chen YB, Wren J, Gonen M, Abdel-Wahab O, Heguy A, Liu H, Takeda S, Tickoo SK, Reuter VE, Voss MH, Motzer RJ, Coleman JA, Cheng EH, Russo P, Hsieh JJ (2013) Clinical and pathologic impact of select chromatin-modulating tumor suppressors in clear cell renal cell carcinoma. Eur Urol 63(5):848–854
Hornigold N, Devlin J, Davies AM, Aveyard JS, Habuchi T, Knowles MA (1999) Mutation of the 9q34 gene TSC1 in sporadic bladder cancer. Oncogene 18(16):2657–2661
Hsieh JJ, Chen D, Wang PI, Marker M, Redzematovic A, Chen YB, Selcuklu SD, Weinhold N, Bouvier N, Huberman KH, Bhanot U, Chevinsky MS, Patel P, Pinciroli P, Won HH, You D, Viale A, Lee W, Hakimi AA, Berger MF, Socci ND, Cheng EH, Knox J, Voss MH, Voi M, Motzer RJ (2017) Genomic biomarkers of a randomized trial comparing first-line everolimus and sunitinib in patients with metastatic renal cell carcinoma. Eur Urol 71(3):405–414
https://www.thermofisher.com/order/catalog/product/4475346. [cited 2018 3/23]
https://www.thermofisher.com/order/catalog/product/4477685. [cited 2018 3/23]
Huang J, Manning BD (2008) The TSC1–TSC2 complex: a molecular switchboard controlling cell growth. Biochem J 412(2):179–190
Huynh H, Hao HX, Chan SL, Chen D, Ong R, Soo KC, Pochanard P, Yang D, Ruddy D, Liu M, Derti A, Balak MN, Palmer MR, Wang Y, Lee BH, Sellami D, Zhu AX, Schlegel R, Huang A (2015) Loss of tuberous sclerosis complex 2 (TSC2) Is frequent in hepatocellular carcinoma and predicts response to mTORC1 inhibitor everolimus. Mol Cancer Ther 14(5):1224–1235
Iyer G, Hanrahan AJ, Milowsky MI, Al-Ahmadie H, Scott SN, Janakiraman M, Pirun M, Sander C, Socci ND, Ostrovnaya I, Viale A, Heguy A, Peng L, Chan TA, Bochner B, Bajorin DF, Berger MF, Taylor BS, Solit DB (2012) Genome sequencing identifies a basis for everolimus sensitivity. Science 338(6104):221
Jackson MA, Rich TA, Hu MI, Perrier ND, Waguespack SG (1993) CDC73-Related Disorders. In: Adam MP et al (eds) GeneReviews((R)). University of Washington, Seattle
Ji X, Jin S, Qu X, Li K, Wang H, He H, Guo F, Dong L (2015) Lysine-specific demethylase 5C promotes hepatocellular carcinoma cell invasion through inhibition BMP7 expression. BMC Cancer 15:801
Kang H, Schubert AD, Ladenson P, Ball DW, Chung J, Schrock AB, Ross JS, Miller VA, Stephens PJ, Ali SM (2017) Comprehensive genomic profiling of parathyroid carcinoma. J Clin Oncol 35(15 suppl):6088
Kasaian K, Wiseman SM, Thiessen N, Mungall KL, Corbett RD, Qian JQ, Nip KM, He A, Tse K, Chuah E, Varhol RJ, Pandoh P, McDonald H, Zeng T, Tam A, Schein J, Birol I, Mungall AJ, Moore RA, Zhao Y, Hirst M, Marra MA, Walker BA, Jones SJ (2013) Complete genomic landscape of a recurring sporadic parathyroid carcinoma. J Pathol 230(3):249–260
Khoo KH, Verma CS, Lane DP (2014) Drugging the p53 pathway: understanding the route to clinical efficacy. Nat Rev Drug Discov 13(3):217–236
Knudson AG (2001) Two genetic hits (more or less) to cancer. Nat Rev Cancer 1(2):157–162
Kopetz S, Litzenburger B, Kinyua W, Sajan B, Subbiah V, Zinner R, Wheler JJ, Hong DS, Tsimberidou AM, Overman MJ, Pagliaro LC, Busaidy NL, Westin SN, Glisson BS, Heymach J, Meric-Bernstam F, Shaw KR, Lee JJ, Broaddus R (2015) Prospective evaluation of a 409-gene next generation sequencing platform to facilitate genotype-matched clinical trial enrollment. J Clin Oncol 33(15 suppl):3608
Lazaris AC, Tseleni-Balafouta S, Papathomas T, Brousalis T, Thomopoulou G, Agrogiannis G, Patsouris ES (2006) Immunohistochemical investigation of angiogenic factors in parathyroid proliferative lesions. Eur J Endocrinol 154(6):827–833
Le Tourneau C, Raymond E, Faivre S (2007) Sunitinib: a novel tyrosine kinase inhibitor. A brief review of its therapeutic potential in the treatment of renal carcinoma and gastrointestinal stromal tumors (GIST). Ther Clin Risk Manag 3(2):341–348
Liu Z, Hou P, Ji M, Guan H, Studeman K, Jensen K, Vasko V, El-Naggar AK, Xing M (2008) Highly prevalent genetic alterations in receptor tyrosine kinases and phosphatidylinositol 3-kinase/Akt and mitogen-activated protein kinase pathways in anaplastic and follicular thyroid cancers. J Clin Endocrinol Metab 93(8):3106–3116
Matsui J, Funahashi Y, Uenaka T, Watanabe T, Tsuruoka A, Asada M (2008) Multi-kinase inhibitor E7080 suppresses lymph node and lung metastases of human mammary breast tumor MDA-MB-231 via inhibition of vascular endothelial growth factor-receptor (VEGF-R) 2 and VEGF-R3 kinase. Clin Cancer Res 14(17):5459–5465
Mosrati MA, Malmstrom A, Lysiak M, Krysztofiak A, Hallbeck M, Milos P, Hallbeck AL, Bratthall C, Strandeus M, Stenmark-Askmalm M, Soderkvist P (2015) TERT promoter mutations and polymorphisms as prognostic factors in primary glioblastoma. Oncotarget 6(18):16663–16673
NEXAVAR Prescribing Information (2018) Bayer HealthCare Pharmaceuticals, Inc; Whippany, NJ
Owonikoko TK, Khuri FR (2013) Targeting the PI3 K/AKT/mTOR pathway: biomarkers of success and tribulation. Am Soc Clin Oncol Educ Book 33:e395
Pandya C, Uzilov AV, Bellizzi J, Lau CY, Moe AS, Strahl M, Hamou W, Newman LC, Fink MY, Antipin Y, Yu W, Stevenson M, Cavaco BM, Teh BT, Thakker RV, Morreau H, Schadt EE, Sebra R, Li SD, Arnold A, Chen R (2017) Genomic profiling reveals mutational landscape in parathyroid carcinomas. JCI Insight 2(6):e92061
Paolicchi E, Crea F, Farrar WL, Green JE, Danesi R (2013) Histone lysine demethylases in breast cancer. Crit Rev Oncol Hematol 86(2):97–103
Robles-Espinoza CD, Harland M, Ramsay AJ, Aoude LG, Quesada V, Ding Z, Pooley KA, Pritchard AL, Tiffen JC, Petljak M, Palmer JM, Symmons J, Johansson P, Stark MS, Gartside MG, Snowden H, Montgomery GW, Martin NG, Liu JZ, Choi J, Makowski M, Brown KM, Dunning AM, Keane TM, Lopez-Otin C, Gruis NA, Hayward NK, Bishop DT, Newton-Bishop JA, Adams DJ (2014) POT1 loss-of-function variants predispose to familial melanoma. Nat Genet 46(5):478–481
Rokman A, Ikonen T, Seppala EH, Nupponen N, Autio V, Mononen N, Bailey-Wilson J, Trent J, Carpten J, Matikainen MP, Koivisto PA, Tammela TL, Kallioniemi OP, Schleutker J (2002) Germline alterations of the RNASEL gene, a candidate HPC1 gene at 1q25, in patients and families with prostate cancer. Am J Hum Genet 70(5):1299–1304
Schaffner C, Idler I, Stilgenbauer S, Dohner H, Lichter P (2000) Mantle cell lymphoma is characterized by inactivation of the ATM gene. Proc Natl Acad Sci USA 97(6):2773–2778
Schulte KM, Talat N (2012) Diagnosis and management of parathyroid cancer. Nat Rev Endocrinol 8(10):612–622
Shattuck TM, Valimaki S, Obara T, Gaz RD, Clark OH, Shoback D, Wierman ME, Tojo K, Robbins CM, Carpten JD, Farnebo LO, Larsson C, Arnold A (2003) Somatic and germ-line mutations of the HRPT2 gene in sporadic parathyroid carcinoma. N Engl J Med 349(18):1722–1729
Shayesteh L, Lu Y, Kuo WL, Baldocchi R, Godfrey T, Collins C, Pinkel D, Powell B, Mills GB, Gray JW (1999) PIK3CA is implicated as an oncogene in ovarian cancer. Nat Genet 21(1):99–102
Singh RR, Patel KP, Routbort MJ, Reddy NG, Barkoh BA, Handal B, Kanagal-Shamanna R, Greaves WO, Medeiros LJ, Aldape KD, Luthra R (2013) Clinical validation of a next-generation sequencing screen for mutational hotspots in 46 cancer-related genes. J Mol Diagn 15(5):607–622
Singh RR, Patel KP, Routbort MJ, Aldape K, Lu X, Manekia J, Abraham R, Reddy NG, Barkoh BA, Veliyathu J, Medeiros LJ, Luthra R (2014) Clinical massively parallel next-generation sequencing analysis of 409 cancer-related genes for mutations and copy number variations in solid tumours. Br J Cancer 111(10):2014–2023
Stracquadanio G, Wang X, Wallace MD, Grawenda AM, Zhang P, Hewitt J, Zeron-Medina J, Castro-Giner F, Tomlinson IP, Goding CR, Cygan KJ, Fairbrother WG, Thomas LF, Saetrom P, Gemignani F, Landi S, Schuster-Bockler B, Bell DA, Bond GL (2016) The importance of p53 pathway genetics in inherited and somatic cancer genomes. Nat Rev Cancer 16(4):251–265
Vinagre J, Almeida A, Populo H, Batista R, Lyra J, Pinto V, Coelho R, Celestino R, Prazeres H, Lima L, Melo M, da Rocha AG, Preto A, Castro P, Castro L, Pardal F, Lopes JM, Santos LL, Reis RM, Cameselle-Teijeiro J, Sobrinho-Simoes M, Lima J, Maximo V, Soares P (2013) Frequency of TERT promoter mutations in human cancers. Nat Commun 4:2185
Wu J, Ellison J, Salido E, Yen P, Mohandas T, Shapiro LJ (1994) Isolation and characterization of XE169, a novel human gene that escapes X-inactivation. Hum Mol Genet 3(1):153–160
Xing M, Liu R, Liu X, Murugan AK, Zhu G, Zeiger MA, Pai S, Bishop J (2014) BRAF V600E and TERT promoter mutations cooperatively identify the most aggressive papillary thyroid cancer with highest recurrence. J Clin Oncol 32(25):2718–2726
Yu W, McPherson JR, Stevenson M, van Eijk R, Heng HL, Newey P, Gan A, Ruano D, Huang D, Poon SL, Ong CK, van Wezel T, Cavaco B, Rozen SG, Tan P, Teh BT, Thakker RV, Morreau H (2015) Whole-exome sequencing studies of parathyroid carcinomas reveal novel PRUNE2 mutations, distinctive mutational spectra related to APOBEC-catalyzed DNA mutagenesis and mutational enrichment in kinases associated with cell migration and invasion. J Clin Endocrinol Metab 100(2):E360–E364
Yuan TL, Cantley LC (2008) PI3 K pathway alterations in cancer: variations on a theme. Oncogene 27(41):5497–5510
Acknowledgements
We wish to thank Mrs. Jennifer Jordan and Mr. Len Jordan for their generous contributions that made this study possible. We thank Bryan Tutt from the Scientific Publications Department at MD Anderson Cancer Center for editing our manuscript.
Funding
Supported by the NIH/NCI under award number P30CA016672 and philanthropic donation from patients
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
NLB has received grant funding from Novartis and Bayer and consulting fees from Eisai. MEC has received grant funding from Eisai. MK, HTN, LK, CC, AS, EI, SGW, CJ, MH, SS, SK, RB, RD, KW, MW, MZ, NP: nothing to disclose
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kutahyalioglu, M., Nguyen, H.T., Kwatampora, L. et al. Genetic profiling as a clinical tool in advanced parathyroid carcinoma. J Cancer Res Clin Oncol 145, 1977–1986 (2019). https://doi.org/10.1007/s00432-019-02945-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-019-02945-9