Abstract
Purpose
To examine the independent association between type II diabetes and fracture risk in a population of predominantly postmenopausal women referred to a specialist clinic for osteoporosis evaluation.
Methods
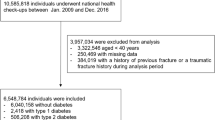
Type II diabetes associated fracture risk were evaluated among to 229 patients with type II diabetes in a cohort of 6285 women followed on average (until major osteoporotic fracture (MOF), death or end of study) for 5.8 years. Information of fracture risk factors was obtained from a clinical database and from national registries.
Results
An elevated fracture risk was present. Prevalent fractures (43.7 vs. 33.2%, p = 0.0010) and prevalent MOF (26.2 vs. 20.5% p = 0.038) were more common among patients with type II diabetes. The unadjusted incident fracture risk was increased with a higher relative risk of 42%. An elevated MOF hazard ratio was present (HR = 1.726, p = 0.0006). Adjustment for prevalent osteoporosis and other possible confounders did not change this finding (HR = 1.558, p = 0.0207).
Conclusions
An association between type II diabetes and an increased risk of MOF primarily driven by an increased hip fracture risk was documented. This finding was independent of the presence of osteoporosis. Clinicians need to be aware of and adjust for these findings when evaluating patients with diabetes. Additional research examining pathophysiological mechanisms are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background and introduction
Type II diabetes is a chronic, metabolic disease characterized by high blood glucose caused by insulin resistance. Type II diabetes is affecting an increasing proportion of individuals all over the world with numbers estimated to around 285 million worldwide and with a major expected increase in the prevalence in the years to come [1]. The disease leads to a wide range of complications. As such complications attributable to neuropathy, nephropathy, and retinopathy are common [2]. Although the most serious consequence of type II diabetes is the observed elevated risk of cardiovascular disease a long list of other comorbid conditions can cause considerable morbidity and reduced quality of life [2]. In recent years increasing evidence that an elevated susceptibility to fractures should be considered a complication of diabetes type II has been documented but is not incorporated into clinical guidelines [3].
The etiology of fractures among patients with type II diabetes are presumably multifactorial and are as of now not fully understood [4]. Possible mechanisms are depicted in Fig. 1. Important disease effects might include a predisposition to falls [5], but also a possible direct detrimental effect on diabetic bone due to changes in blood glucose and insulin levels. Possible reasons for an elevated risk of falling might include impaired vision, episodes of hypoglycemia, peripheral neuropathy, and/or decreased muscle strength [6]. On the other hand changes in architecture and the quality of bone matrix components due to inflammatory cytokines, accumulation of advanced glycation end products (AGE), and oxidative stress have been proposed as an explanation for changes in bone structural and bone strength properties [7, 8]. Furthermore changes due to microvascular disease might play a role.
Special attention in the past decades has been paid to bone collagen cross-link formation. Patients with type II diabetes tend to have a negative shift in the balance between enzymatically and non-enzymatically formed collagen cross-links. The non-enzymatic formation of collagen cross-links in the form of AGEs has unfavorable effects on bone and accumulation of AGEs reduces bone strength in rats without changes in BMD compared to healthy controls [9]. In one human study patients with type II diabetes had an increase in AGEs (as measured by urine pentosidine) which was associated with an increased risk of fractures [10].
In addition to this direct effect on bone biomechanical properties high AGE levels might have a direct negative effect on osteoblasts and enhance osteoclast function [6], which may well impair micro fracture damage repair.
In this study we sought to examine the independent association between type II diabetes and fracture risk in a population of predominantly postmenopausal women referred to a specialist clinic for osteoporosis evaluation. In addition we sought to further characterize fracture risk according to fracture site.
Subjects and methods
This study is a historical cohort study of patients referred to an osteoporosis specialist unit at the Copenhagen University Hospital Hvidovre. The first patients were seen in 2002 and patient risk profile was routinely registered in a clinical database the following decade. All subjects included in the study had information related to self-reported general risk factors of osteoporosis available from the database. Patients who did not have this information recorded or who participated in bone related research before or during follow-up were excluded. The cohort consisted of 6285 women of which 229 had type II diabetes.
A comprehensive description of the available information from both the mentioned database as well as supplementary information from Danish national registries (comorbidities: Danish National Patient Register) [11], mortality: Register of Causes of Death [12] and redeemed medications: The Danish National Prescription Registry [13]) have been described in detail in previous studies within this cohort of patients examining associations of different risk factors and bone mass findings [14, 15]. All data were available in anonymized form only.
Exposure and covariate status was defined based on status at first visit. Relating to medications dosages of redeemed glucocorticoids during the previous year were converted to prednisolone/prednisone equivalent dosages in milligrams/day [16]. Patients were classified as high users if they had redeemed more than 450 mg during the previous year. Other medications including selective serotonin receptor inhibitors (SSRI), tricyclic anti-depressants (TCA) and different types of diuretics and antihypertensives (ACE, ANGII, loop, thiazide) were evaluated and defined daily dosages (DDD) during the previous year were calculated. Current medicine use was thought present if a patient had redeemed any prescriptions of the drug in question within the previous year.
A positive exposure towards diabetes type II was classified based on the presence of a registration in the Danish National Patient Register prior to 3 months after first visit or if they before first visit had redeemed any oral antidiabetic medications. A similar timeframe relating to other individual comorbidities was used. A proxy of excessive alcohol consumption was defined as having an alcohol related diagnosis. Further, prevalent hyperthyroidism, rheumatoid arthritis (RA), inflammatory bowel disease (IBD), major osteoporotic fracture (MOF), and chronic pulmonary disease (CPD) was included in the multivariate analysis, (see supplementary material regarding ICD-8/ICD-10, ATC codes used).
A de novo fracture was only thought present if a registration at the same MOF site was not present within the year predating the fracture in question.
General risk factor status obtained from the database and national registries thus included the following potential predictors of osteoporosis corrected for in this study: history of fractures among parents and siblings, early menopause (before age 45 without hormone replacement therapy), an approximation of daily consumption of dietary calcium (<420, 540–780, and >900 mg/day), use of calcium supplements, exercise less than once a week, current smoking status, age, BMI, modified Charlson index, hyperthyroidism, RA, CPD, prevalent MOF, former osteoporosis treatment, glucocorticoid use >450 prednisone eq, alcohol related diagnoses and current use of ACE, ANGII, loop, thiazide, SSRI, TCA.
BMD measurement by dual-energy X-ray absorptiometry (DXA) at baseline was available on all included patients from which patients were classified as having osteoporosis if T-score was below −2.5 at the femoral neck, total hip or spine [17]. No allocation to specific scanners based on exposure status was done.
Statistics
Baseline characteristics are presented as mean with standard deviations (SD) or in case of continuous variables being non-normally distributed medians with interquartile range (IQR). Categorical variables are presented as number of observations and percentages hereof. Comparison between groups was performed using wilcoxon, χ2-test or student t-test. Calculated p-values using Satterwaite statistics in case of unequal variances were performed. Fisher’s exact test was used when the predicted value of any cell was less than five.
Univariate fracture (overall and site specific) comparisons between groups were done using cox proportional hazard models by running an unadjusted cox proportional hazard model with fracture as response and baseline type II diabetes as an explanatory variable. Included persons were followed until first incident fracture or censored at time of death or the 31/12 2012, whatever came first. Fractures were registered according to fracture site and identified as MOF (femoral, vertebral, humeral, lower arm) or others. Individuals could be included in several site specific outcomes, but only once for any particular site.
Furthermore a comprehensive multivariate cox regression analysis including a wide range of proposed baseline risk factors was performed hereby presenting hazard ratios for baseline type II diabetes with corresponding confidence intervals.
Covariates for the multivariate analysis included use of different medications known to be associated with fracture risk, certain comorbidities as well as general risk factors for osteoporosis. Furthermore, a modified Charlson index score [18] was calculated to adjust for difference in overall comorbidity.
The hazard ratio can be regarded as a relative risk in this study. Risk was calculated for all fractures as well as according to MOF fracture site. Assumptions of proportional hazards and linearity of continuous variables were evaluated. When evidence of violation of these assumptions was detected the corresponding covariate was either categorized into groups or the analysis stratified hereupon.
Results
In total 6285 patients were included in the univariate analysis.
At baseline 229 women were exposed (had diabetes according to our definition). The women with diabetes were significantly older (Table 1), had a higher BMI, more comorbidity and were more often users of a wide variety of medicine. Fewer had osteoporosis by DXA and fewer were exercising more than once weekly. In the total cohort of patients 3563 fractures among 1234 patients had occurred at baseline. On average patients were followed (until MOF, death or end of study) for 5.8 years.
After baseline measurement of bone mineral density 1734 fractures occurred among 1314 persons during follow-up. Among patients with type II diabetes 22.7% sustained an incident fracture whereas that was the case for 19.0% of non-diabetics. As such an unadjusted/crude increased relative risk of 42% was evident (Table 2). Prevalent fractures (43.67 vs. 33.22%, p = 0.0010) at baseline were more common among patients with diabetes. This was likewise the case for MOF 26.2 vs. 20.5% p = 0.038. Among patients entering the multivariate analysis (n = 4587) 599 patients experienced a MOF during follow-up. As expected significantly more patients with type II diabetes died before the end of study 21.8 vs. 11.1%.
When comparing patients with type II diabetes with patients without an elevated hazard ratio for MOF was present HZ = 1.726, p = 0.0006. Adjustment for prevalent osteoporosis and a wide selection of other co-variates did not change these findings HZ = 1.558, p = 0.0207. When looking at all fractures we failed to find any significant association after multivariate adjustment were made (Table 3). As limited number of fracture outcomes made such extensive adjustments impossible when looking at individual MOF sites analysis of these were performed adjusting for fewer risk factors.
When looking at site specific fracture sites (Table 4) only an association with hip fractures (HZ 1.833, p = 0.0442) was significantly present, but the estimated hazard ratios at other fracture sites were all indicating a higher risk in patients with type II diabetes.
Patients with type II diabetes experiencing a MOF during follow up were significantly older (71.2 vs. 64.2, p = 0.001) and correspondingly had a lower T-score at the total hip (−1.63 vs. −0.82, p = < 0.0001) and femoral neck site (−1.83 vs. −1.27, P = 0.0028) at baseline than patients with type II diabetes not experiencing a MOF. No differences in bone mineral density were found when looking at the lumbar spine.
Fewer patients with type II diabetes using a ANGII inhibitor at baseline experienced a MOF (6.5% vs. 18.6%, p = 0.047). When evaluating baseline differences among patients with type II diabetes experiencing a MOF during follow up vs. patients who did not sustain a fracture no other differences in the risk factor profile evaluated in his study (behavioral risk factors, medicinal use, and differences in comorbidity) were identified.
Discussion
Our findings confirm that women with type II diabetes are at an increased risk of sustaining a fracture, but that the risk differs according to site.
We found that women with a registration of type II diabetes at the time of their first visit had a 56% increased risk of sustaining a MOF during an average of 5.8 years of follow-up. This association was independent of age group, BMI, exercise status, and use of different medications and comorbidities as well as osteoporosis status at baseline. Certainly, a noteworthy ability of this study is that we were able to adjust for differences in osteoporosis status based on DXA measurements something only few earlier studies have been able to do. As most studies published only have been able to make a limited adjustment for potential confounders i.e., both differences in bone mass, BMI, physical activity etc. previous findings may to some extent have been affected by a high degree of bias. In this study we tried to adjust for multiple potential confounders attributable to both hereditary, lifestyle, comorbidities, and use of different medications seeking to further elucidate on the possible association.
We found that fracture risk differed according to fracture site. The highest fracture risk and indeed only significant association was documented when looking at hip fractures driving a lot of the significance at the overall fracture sites (all fractures and MOF).
This is in accordance with the majority of existing literature. A meta-analysis by Janghorbani et al. [19] found this risk to be more than doubled among women. Similarly Vestergaard et al. [3] found in a meta-analysis from 2007 that patients with type II diabetes had a 1.38 times risk of sustaining a hip fracture. In a recent meta-analysis including recent studies not included in the earlier meta-analysis there was likewise demonstrated an elevated risk of hip fractures for patients with type II diabetes at 34% [20].
Leslie et al. [21] examined the hazard of MOF according to diabetes type II status adjusted for FRAX risk factors and found an elevated HR of 1.32.
We found an univariate association between type II diabetes and “all fractures”. This association could not be confirmed when more extensive adjustments were made. The failure to document a significant association after adjustments when looking at overall fractures might relate to sample size.
In several other epidemiological studies such a negative overall fracture association has been documented, but results are inconsistent. Janghorbani et al. [19] found that overall risk of any fracture was slightly elevated (summary RR = 1.2). These findings were further supported by a large observational study by Bonds et al. [22] were type II diabetics had a 20% increased overall fracture risk. On the other hand Vestergaard et al. [3] found, using crude estimates of fracture risk, that the relative risk of any fracture in type II diabetics was not increased.
We failed to demonstrate a fracture association at individual fracture sites besides at the hip although risk estimates at all sites indicated a trend towards increased risk of fractures. It is quite possible that the reason why we could not demonstrate an increased fracture risk at individual sites is partly likewise due to low statistical power. On the other hand the Women´s Health Initiative observational study [22] which included more than 90.000 women, the meta-analysis by Janghorbani et al. [19] as well as the nationwide study by Vestergard et al. [4] failed to find any significant associations at specific fractures sites beside either at the feet or forearm. We did as described not specifically investigate foot fractures as the number of those were limited.
The reason why results differ at non-hip fracture sites might reflect differences in study populations in terms of diabetes severity and duration as it has been proposed that fracture risk is predominantly elevated in patients with long duration and severity.
A Canadian observational study even found that newly diagnosed type II diabetics were protected against osteoporotic fractures [23]. The authors of this study suggested that fracture risk in type II diabetes is biphasic, that is patients are protected from fractures during the first years after diagnosis, but prolonged disease duration at some point increases the risk. The osteoprotective effects of hyperinsulinaemia in early stages of the disease may in part account for this. On the other hand in a recent study from Germany including almost 300,000 patients with newly diagnosed diabetes an increased fracture risk was documented at all evaluated specific fracture sites. This was evident as early as the following year after establishment of a diagnosis [24]. Conclusions drawn from this study however is hampered by the fact that no information of BMD was available and because patients with osteoporosis and glucocorticoid users were excluded. Furthermore, evaluation of many potential confounders including inflammatory diseases and use of different medicinal products often used by patients with type II diabetes that might have an effect on fracture risk were not adjusted for.
Our results confirm findings by others that bone density is similar or higher in patients with type II diabetes [3] and that fewer patients with type II diabetes have osteoporosis by DXA compared to controls. In a previous study within this cohort of patients [14] looking at the relationship of different risk factors of osteoporosis we found a strong univariate association between type II diabetes and high bone mass density at all sites. This difference was non-significant when other confounders predominantly differences in BMI were taken into account. Our results thus show that adjustment for prevalent osteoporosis does not change risk estimates. Furthermore, we found that an increased fracture risk is present despite patient with type II diabetes having a higher body weight. Our results thereby also lend support to findings by Schwarz et al. [25] and others showing that estimated fracture risk based on findings of bone mass or commonly used fracture risk algorithms such as FRAX is underestimated [26]. Efforts should therefore be made to establish type II diabetes adjusted treatment thresholds in the future.
Limitations
BMD measurements can be flawed in the very obese [27]. Although this study is not population based it represents a broad selection of people thought to be at risk of osteoporosis by the GP. As almost all fractures are thought to be recorded bias attributable to the registration of fracture outcome is thought to be limited. We were not able to adjust for the severity, level of glycemic control or duration of diabetes, all of which have been documented to affect fracture risk [28, 29]. In other studies insulin use has been associated with an increased fracture risk, but this finding is most likely to reflect diabetes duration and severity of the disease and is not a direct consequence of insulin treatment as such [7]. In this study we did not stratify type II diabetes based on use of insulin as statistical power would be reduced but it is likely that the association found is stronger among patients with more advanced disease.
As the majority of cases with type II diabetes are managed at primary health care level not all patients with type II diabetes are registered in the National Patient Register where only hospital contacts are recorded. In order to partly address this issue patients who had collected oral antidiabetics before first visit were also thought to have type II diabetes. The positive predictive value (PPV) of having a registration of evaluated comorbidities including diabetes has been shown to be high [18]. Patients with type II diabetes treated exclusively with insulin before 1995 who were not registered in LPR will not have been captured, but this will, if it had occurred at all, have been very few. Still patients only treated by lifestyle intervention were not registered as having type II diabetes. These patients will be included in the reference group and will presumably as such weaken the documented association. In spite of this we were still able to show that type II diabetes is associated with an elevated risk of MOF primarily due to the association with hip fractures.
Furthermore a large proportion of people presumably have undiagnosed diabetes and we did not take into account changes in exposure covariate status from initial evaluation to time of event or censoring. These differences would presumably likewise tend to underestimate any association of diabetes type II and fractures. Finally misclassification between type I and II diabetes might have happened but overall possible misclassification in this study is thought to be minimal. In cases where type I diabetes was misclassified this would possibly have affected the result in favor of shoving an increased hazard ratio of fractures as type I diabetes generally has been shown to be stronger associated with fractures than type II diabetics [19]. We saw a limited number of spinal fractures. As the majority of spinal fractures are unrecognized by the patients underestimation of these fractures is clearly evident. A limitation of this study is thus the lack of data regarding prevalence and incidence of morphometric vertebral fractures. Zhukouskaya et al. [30] have previously among others shown prevalence of these fractures to be increased among patients with type II diabetes. As the numbers of spinal fractures were low although the risk estimate was quite high we thus failed to find any significant association. Finally we did not have any information about falls, but literature shows that an increased risk of falling in type II diabetics is evident. This elevated risk of falling has in other studies not been fully able to account for a higher fracture risk [22].
Severe Vitamin D deficiency leads to secondary hyperparathyroidism and thus results in an accelerated bone loss, compromised bone quality and could play a part in type II diabetes related fracture risk. A limitation of this study was that 25-OH vitamin D levels before 2008 where not performed routinely. When comparing the levels of 25-OH vitamin D in patients with and without type II diabetes in the population with available vitamin D measurements (n = 3106) no difference was found (67.3 nmol/L vs. 71.1 nmol/L p = 0.15) however.
A further limitation of the study was that information of actual time since menopause was not available and women were thus only categorized in groups and considered to be estrogen deficient if they indicated to be hormone replacement therapy treatment naive and had had both ovaries surgically removed or experienced menopause before 45 years of age [14].
Conclusion
To conclude our findings strongly support an association between type II diabetes and increased risk of MOF an association primarily driven by an increased hip fracture risk. Increased risk at other individual fracture sites was not confirmed although risk estimates indicated an increased risk.
Our evidence thus suggests that an elevated fracture risk among type II diabetics persists even after adjustment for a wide variety of possible confounders including medicinal use, comorbidities, differences in BMD, and other modifiable risk factors. Clinicians need to be aware of and adjust for these findings when evaluating patients with diabetes. Additional research is needed as to describe pathophysiological mechanisms and to further describe the relation to disease duration and blood glucose regulation. Furthermore studies describing the effect of commonly used drugs used to treat osteoporosis in this population are needed.
References
D.R. Whiting, L. Guariguata, C. Weil, J. Shaw, IDF Diabetes Atlas: Global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin. Pract. 94, 311–321 (2011)
V.V. Shanbhogue, D.M. Mitchell, C.J. Rosen, M.L. Bouxsein, Type 2 diabetes and the skeleton: new insights into sweet bones. Lancet Diabetes Endocrinol. 8587, 1–15 (2015)
P. Vestergaard, Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes--a meta-analysis. Osteoporos. Int. 18, 427–444 (2007)
P. Vestergaard, L. Rejnmark, L. Mosekilde, Relative fracture risk in patients with diabetes mellitus, and the impact of insulin and oral antidiabetic medication on relative fracture risk. Diabetologia 48, 1292–1299 (2005)
A.V. Schwartz, T.A. Hillier, D.E. Sellmeyer, H.E. Resnick, E. Gregg, K.E. Ensrud, P.J. Schreiner, K.L. Margolis, J.A. Cauley, M.C. Nevitt, D.M. Black, S.R. Cummings, Older women with diabetes have a higher risk of falls: a prospective study. Diabetes Care 25, 1749–1754 (2002)
S. Kurra, E. Siris, Diabetes and bone health: the relationship between diabetes and osteoporosis-associated fractures. Diabetes Metab. Res. Rev. 27, 430–435 (2011)
W.D. Leslie, M.R. Rubin, A.V. Schwartz, J.A. Kanis, Type 2 diabetes and bone. J. Bone Miner. Res 27, 2231–2237 (2012)
S. Epstein, G. Defeudis, S. Manfrini, N. Napoli, P. Pozzilli, Diabetes and disordered bone metabolism (diabetic osteodystrophy): time for recognition. Osteoporos. Int. 27, 1931–1951 (2016). https://doi.org/10.1007/s00198-015-3454-x
M. Saito, K. Marumo, Collagen cross-links as a determinant of bone quality: a possible explanation for bone fragility in aging, osteoporosis, and diabetes mellitus. Osteoporos. Int 21, 195–214 (2010)
A.V. Schwartz, P. Garnero, T.A. Hillier, D.E. Sellmeyer, E.S. Strotmeyer, K.R. Feingold, H.E. Resnick, F.A. Tylavsky, D.M. Black, S.R. Cummings, T.B. Harris, D.C. Bauer, Pentosidine and increased fracture risk in older adults with type 2 diabetes. J. Clin. Endocrinol. Metab. 94, 2380–2386 (2009)
E. Lynge, J.L. Sandegaard, M. Rebolj, The Danish National Patient Register. Scand. J. Public Health 39, 30–33 (2011)
K. Helweg-Larsen, The Danish Register of Causes of Death. Scand. J. Public Health 39, 26–29 (2011)
H.W. Kildemoes, H.T. Sørensen, J. Hallas, The Danish National Prescription Registry. Scand. J. Public Health 39, 38–41 (2011)
J.P. Holm, L. Hyldstrup, J.-E.B. Jensen, Time trends in osteoporosis risk factor profiles: a comparative analysis of risk factors, comorbidities, and medications over twelve years. Endocrine 54, 241–255 (2016). https://doi.org/10.1007/s12020-016-0987-5
J.P. Holm, A.O.S. Amar, L. Hyldstrup, J.E.B. Jensen, Hyponatremia, a risk factor for osteoporosis and fractures in women. Osteoporos. Int. 27, 989–1001 (2016)
P. Vestergaard, L. Rejnmark, L. Mosekilde, Fracture risk associated with systemic and topical corticosteroids. J. Intern. Med. 257, 374–384 (2005)
J.T. Schousboe, J.A. Shepherd, J.P. Bilezikian, S. Baim, Executive Summary of the 2013 International Society for Clinical Densitometry Position Development Conference on Bone Densitometry. J. Clin. Densitom. 16, 455–466 (2013)
S.K. Thygesen, C.F. Christiansen, S. Christensen, T.L. Lash, H.T. Sørensen, The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med. Res. Methodol. 11, 83 (2011). https://doi.org/10.1186/1471-2288-11-83
M. Janghorbani, R.M. Van Dam, W.C. Willett, F.B. Hu, Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am. J. Epidemiol. 166, 495–505 (2007)
Y. Fan, F. Wei, Y. Lang, Y. Liu, Diabetes mellitus and risk of hip fractures: a meta-analysis. Osteoporos. Int. 27, 219–222 (2015). https://doi.org/10.1007/s00198-015-3279-7
W.D. Leslie, S.N. Morin, L.M. Lix, S.R. Majumdar, Does diabetes modify the effect of FRAX risk factors for predicting major osteoporotic and hip fracture? Osteoporos. Int. 25, 2817–2824 (2014)
D.E. Bonds, J.C. Larson, A.V. Schwartz, E.S. Strotmeyer, J. Robbins, B.L. Rodriguez, K.C. Johnson, K.L. Margolis, Risk of fracture in women with type 2 diabetes: the Women’s Health Initiative Observational Study. J. Clin. Endocrinol. Metab. 91, 3404–3410 (2006)
W.D. Leslie, L.M. Lix, H.J. Prior, S. Derksen, C. Metge, J.O. Neil, Biphasic fracture risk in diabetes: a population-based study. Bone 40, 1595–1601 (2007)
W. Rathmann, K. Kostev, J. Diabetes, Complications fracture risk in patients with newly diagnosed type 2 diabetes: a retrospective database analysis in primary care. J. Diabetes Complicat. 29, 766–770 (2015)
A.V. Schwartz, E. Vittinghoff, D.C. Bauer, T.A. Hillier, E.S. Strotmeyer, K.E. Ensrud, M.G. Donaldson, J.A. Cauley, T.B. Harris, A. Koster, C.R. Womack, L. Palermo, D.M. Black, Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA 305, 2184–2192 (2011)
L.M. Giangregorio, W.D. Leslie, L.M. Lix, H. Johansson, A. Oden, E. McCloskey, J. a Kanis, FRAX underestimates fracture risk in patients with diabetes. J. Bone Miner. Res. 27, 301–308 (2012)
E.W. Yu, M.L. Bouxsein, A.E. Roy, C. Baldwin, A. Cange, R.M. Neer, L.M. Kaplan, J.S. Finkelstein, Bone loss after bariatric surgery: discordant results. J. Bone Miner. Res 29, 542–550 (2014)
C.I. Li, C.S. Liu, W.Y. Lin, N.H. Meng, C.C. Chen, S.Y. Yang, H.J. Chen, C.C. Lin, T.C. Li, Glycated hemoglobin level and risk of hip fracture in older people with type 2 diabetes: a competing risk analysis of Taiwan Diabetes Cohort Study. J. Bone Min. Res. 30, 1338–1346 (2015)
W.-P. Koh, R. Wang, L.-W. Ang, D. Heng, J.-M. Yuan, M.C. Yu, Diabetes and risk of hip fracture in the Singapore Chinese Health Study. Diabetes Care 33, 1766–1770 (2010)
V.V. Zhukouskaya, C. Eller-Vainicher, A. Gaudio, E. Cairoli, F.M. Ulivieri, S. Palmieri, V. Morelli, E. Orsi, B. Masserini, A.M. Barbieri, E. Polledri, S. Fustinoni, A. Spada, C.E. Fiore, I. Chiodini, In postmenopausal female subjects with type 2 diabetes mellitus, vertebral fractures are independently associated with cortisol secretion and sensitivity. J. Clin. Endocrinol. Metab. 100, 1417–1425 (2015)
Acknowledgements
The study was approved by relevant review authorities including Statens Serum Institute, the Danish Data Protection Agency and Statistics Denmark.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J.H. has participated as a subinvastigator in studies by Amgen and MSD and received payment for lectures by Amgen. L.H. has been giving lectures sponsored by: Novartis, Lilly, Takeda/Nycomed, Novo-Nordisk, Amgen, GlaxoSmithKline, Servier, MSD, Ferrosan, Pfizer, PharmaVinci and Renapharma. J.E.B.J.: Board membership in Amgen, Eli Lilly, MSD, Novartis, Nycomed. Payment for lectures by Amgen, Eli Lilly and MSD. T.J. declares that he has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Holm, J.P., Jensen, T., Hyldstrup, L. et al. Fracture risk in women with type II diabetes. Results from a historical cohort with fracture follow-up. Endocrine 60, 151–158 (2018). https://doi.org/10.1007/s12020-018-1564-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1564-x