Abstract
The aim of this article was to identify prevalent osteoporosis risk factors, medications and comorbidities associated with bone mineral density (BMD). Furthermore to evaluate changes in risk factor profiles over 12 years. 6285 women consecutively referred to an osteoporosis specialist clinic were included. Information of potential risk factors was obtained by questionnaire and clinical examination. Additional information on medication use, comorbidities and fractures were obtained from national registries. An association (<0.05) between well-known risk factors negatively influencing bone health was established in a real-life setting. The prevalence of osteoporosis and proportion of patient’s having comorbidity’s associated with osteoporosis were increasing during the inclusion period (start 23.8 %, end 29.7 %). Increasing age (OR = 1.05), current smoking (OR = 1.18), estrogen deficiency (OR = 1.7), hyperthyroidism (OR = 1.5), previous major osteoporotic fracture (OR = 1.7), former osteoporosis treatment (OR = 3.5), higher BMI (OR = 0.87), use of calcium supplementation (OR = 1.2), high exercise level (OR = 0.7), and use of thiazide diuretics (OR = 0.7) were identified as predictors of osteoporosis by DXA. Rheumatoid arthritis (OR = 2.4) and chronic pulmonary disease (OR = 1.5) was associated with site-specific osteoporosis by DXA at the total hip. Current use of loop diuretics (OR = 1.7) and glucocorticoid use (OR = 1.04–1.06) were associated with both total hip and femoral neck T-score <−2.5. Our data confirms an independent negative association with BMD of many established risk factors, certain comorbidities, and medications. Exercise level, use of loop diuretics, and prevalent chronic pulmonary disease, risk factors not included in fracture risk calculators were associated with osteoporosis by DXA. Time trends indicate risk profile is dynamic, with increasing focus on secondary osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background and introduction
Measurement of bone mineral density (BMD) is still the most widely used method of establishing a diagnosis and evaluating treatment efficacy [1]. Site-specific fracture risk is more than doubled with a decline of one standard deviation in BMD at the hip or lumbar spine [2], but increasing awareness of BMD-independent risk factors for fracture has led to a more widespread use of fracture risk algorithms [3] such as FRAX (https://www.shef.ac.uk/FRAX/).
It is well established that osteoporosis is underdiagnosed and undertreated [1]. To change this, it is essential to develop rational and cost effective strategies for identification of individuals with increased risk of fragility fracture. Increasing awareness of osteoporosis risk factors and secondary causes will help educate health care personnel and the general population. Identification of high-risk patients will presumably lead to allocation of appropriate treatment to those who might benefit the most from preventive measures and treatment.
A dedicated and focused approach via a specialist based unit is likely to accomplish such a goal [4, 5].
Most guidelines include lists of risk factors in peri- and postmenopausal women that should lead to clinical evaluation and BMD measurements.
In Denmark, the main clinical risk factors are considered to be: age above 80, family history of osteoporosis or fractures, former fragility fracture, menopause before the age of 45, excessive alcohol intake, smoking, tendency to fall, aromatase inhibitor, or systemic glucocorticoid treatment (≥5 mg daily in 3 months or 450 mg yearly). Finally some diseases are recognized that should lead to DXA evaluation.
These guidelines do, however, change over time as does the clinicians perceptions of the relative importance of different risk factors.
At our hospital, a specialist unit for osteoporosis evaluation has existed since 1979. In 1999, a database was established, including a risk factor questionnaire, biochemical data, and densitometry results from all patients referred for evaluation. Combining these data with information from national Danish registers gives information on the importance of different risk factors as well as the changing perception among referring physicians and patients of which risk factors that should lead to osteoporosis evaluation.
Materials and methods
Study population
All patients referred from general practice (GP) for osteoporosis evaluation to the Copenhagen University Hospital Hvidovre from 2000 to 2012 were eligible. A total of 8294 women underwent BMD evaluation and were before first visit requested to fill out a questionnaire regarding potential risk factors for osteoporosis. The questionnaire was returned by 6402 women (response rate of 77 %). Non-responders, patients lacking a DXA evaluation, and patients who had participated in clinical research involving prevention or treatment of osteoporosis were not included. Evaluation of hyponatremia as a possible risk factor of low bone mass and fractures in a subpopulation of this cohort of patients has previously been published [6] and supplementary description of included patients and collection of data can be found here.
In total, 6285 women were included in the univariate analysis. Due to missing values, 4599 out of 6285 women were included in the final multivariate analysis corresponding to 73.2 % of women having returned the questionnaire (Fig. 1).
Risk factor registration
The questionnaire was intended to address generally accepted risk factors for osteoporosis in 1999, but a few risk factors, like alcohol consumption, was not accepted by the Danish Data Protection Agency to be part of the registered information in the database. At the beginning of the study, a small number of patients were asked to fill out the questionnaire twice with at least 1 month’s interval, only minor differences were detected between the two. Further, at the examination of the patients, inconsistencies and misunderstandings were corrected. The questionnaire based information included a family history of fractures in first-degree relatives, own fracture history, nutritional factors (daily consumption of milk, cheese etc.), use of calcium and vitamin D supplements, height at age 25, limitations in everyday life, physical function level, work and exercise, age of menarche and menopause, history of gynecological surgery, former estrogen replacement therapy, history of osteoporosis treatment, and current smoking status. Limitations in everyday life were classified as having no/minor or having limitations. Women with a menopausal age <45 years of age or who had undergone ovarian surgery with the removal of both ovaries, both without use of hormone replacement therapy were considered to be estrogen deficient. Patients were categorized as being physically active if they indicated to have exercised at least once a week. Work function was classified based on sitting, standing, or weight lifting components, exemplified by different occupations.
The daily dietary calcium intake was assessed based on the self-reported average daily use of dairy products plus an estimated basal intake of calcium set at 300 mg corresponding to an approximate calcium contribution from non-dairy products in an average Danish diet. Patients were asked about daily consumption of cheese (never, 1–3 slices, more than 3 slices) and amounts of milk/yoghurt etc. being consumed (>half a liter, <half a liter, never).
Contributions from milk/yoghurt etc. were averaged as 120 mg/100 mL whereas the average calcium content of a slice of cheese was approximated at 120 mg as well based on food composition tables from the Danish National Food Agency (2010) [7]. According to their approximated minimum daily consumption, patients were divided into groups (<420, 540–780, and >900 mg/day).
Anthropometric measures included measurements of bodyweight and height. Patients were measured wearing indoor clothes and being barefooted. If the body mass index (BMI) were below 20 kg/m2, patients were categorized as underweight. The questionnaire was used unchanged throughout the entire observation period.
Densitometry measurements
BMD measurement at the lumbar spine, femoral neck, and total hip was conducted using three types of Hologic DXA scanners (Hologic Inc., MA, USA). If bilateral artificial hips were present only BMD measurements at the lumbar spine were performed. Coefficient of variation was calculated from daily DXA scans on a standard phantom and was on the individual scanners below 0.9 % at the lumbar spine. Variation between machines was assessed. Biannually, repeated DXA scans on the same phantom comparing measurements of BMD between machines were conducted. A slight difference corresponding to approximately 1 % of the mean BMD was present between one machine and the others. The difference was deemed clinically insignificant for this study.
Spinal T-scores were derived from the HOLOGIC study [8]. T-scores of hip and femoral neck were calculated using values from the NHANES phase III study [9]. Based on the lowest measured T-scores (if <−2.5) at the femoral neck, total hip or lumbar spine patients were classified as having osteoporosis or not [10].
Laboratory tests
Blood samples were collected in the majority of cases and if feasible this took place on the same day as the DXA scan was performed. Blood samples were analyzed at the local biochemical department (accredited according to ISO 15189 standards) and included measurements of s-PTH, s-25(OH) vitamin D, s-TSH, and s-creatinine from which estimated glomerular filtration rate (eGFR) was calculated, as well as hemoglobin, leucocyte counts, thrombocytes, s-C-reactive protein, serum electrolytes, s-albumin, s-alkaline phosphatases, and s-ALAT. Before 2008, only patients ≥65 years had a s-25(OH)-vitamin D measurement. Onward all patients had D-vitamin status included in the standard blood samples. Patients were divided into groups based on vitamin D levels severe <12.5 nmol/L, moderate/mild <25–50 nmol/L, and normal >50 nmol/L [11]. An adjusted s-25(OH)-vitamin D was calculated as (mean s-25(OH)-vitamin D/mean s-25(OH)-vitamin D in the month of measurement) × the measured value of s-25(OH)-vitamin D.
Registers
In Denmark, every person has a unique registration code that allows detailed registration at the individual level. Registration occurs automatically and this information was consequently available for all patients in the study. This allows linkage of information collected in the clinical database with information from national administrative registers. Linkage and anonymization was done at Statistics Denmark in order to fulfill the Danish Data Protection Act [12].
In this study, information from The Danish Medicines Agency and The National Hospital Discharge Register were used.
The Danish Medicines Agency holds registers of all drugs sold at pharmacies and hereby a complete record of drugs sold from 1996 and onward exits. High-quality individual prescription data covering redeemed medications using ATC codes, dosage, and date of sale was obtained from The Danish National Prescription Registry [13]. Validity and capture of information in this register is high [13]. Patient files were manually checked for information regarding osteoporosis medicines administered at the hospital, mainly IV-bisphosphonates, and (since 2010) denosumab.
Dosages of redeemed glucocorticoids during the previous year before BMD measurement were converted to prednisolone/prednisone equivalent dosages in milligrams/day [14]. Other medications including selective serotonin receptor inhibitors (SSRI), tricyclic anti-depressants (TCA), and thiazides were evaluated and defined daily dosages (DDD) during the previous year were calculated. Current use of loop diuretics was thought present if a patient had redeemed any prescriptions within the previous year. In each tablet of angiotensin II inhibitors/Thiazide combinations, the content of thiazide was set to ½ DDD, unless other dosage was certain.
The Danish National Patient Register [15] provided data on comorbidities and prevalent fractures. The register is regarded as the most comprehensive of its kind and holds information covering the period from 1977 to present (1977–1994 inpatients only, thereafter outpatient and emergency visits as well). Individual contacts are registered and coded using the ICD-8/ICD-10 system. This register has nationwide coverage and captures almost all contacts [15]. It has been reported to be accurate especially for the registration of fractures, where a precision of 97 % has been reported [14, 16].
Fractures were registered according to fracture site and identified as major osteoporotic fractures (MOF = femoral, vertebral, humeral, lower arm) or others.
Prevalent individual comorbidities were defined as a registration of the disease in question in the register up to 3 months after first visit. This was done in order to allow chronic diseases identified during osteoporosis evaluation to be included. A history of hyperthyroidism or diabetes type II where also deemed positive if patients had filled any prescription of oral antidiabetics or oral antithyroid medication predating the date of the first visit. A Charlson Comorbidity Index score was calculated and used to adjust for differences in overall comorbidity [17]. Patients were categorized as having a disease associated with osteoporosis (including treatment with aromatase inhibitors and glucocorticoids >450 mg/previous year) based on national treatment guidelines. (See supplementary material for detailed information regarding collected data, ICD-8/ICD-10, ATC codes etc.)
Endpoints
Evaluated outcomes were risk factor associations with T-scores and overall/site-specific osteoporosis by DXA in the total hip, femoral neck, or lumbar spine at the time of referral.
Change in risk profile and prevalence of diseases associated with osteoporosis in patients seen in the period of 2000–2004, 2005–2008, and 2009–2012 was assessed.
Statistics
SAS software (version 9.3) was used for the statistical analysis. Descriptive variables are presented as mean value with standard deviation (±SD) or medians with interquartile range (IQR) for continues variables. Categorical variables are presented as number and percent of responders.
Difference in characteristics of patients who filled the questionnaire and patients failing to do so with regard to BMD and age were analyzed using the Student’s t test for continuous variables. Further comparisons were done using χ 2, or Wilcoxon two sample tests.
Correlation analysis between variables was performed using Spearman’s analysis. Uni- and multivariate regression analysis were performed using generalized linear models. Whenever unequal group variances were detected, p values was calculated using Welch test. Predictors of prevalent osteoporosis were identified by logistic regression.
Sub analyses in osteoporosis treatment naive patients were performed.
Age was tested as an interaction term. Age stratification sub-analysis (Table 5) was performed when a positive effect modification on explanatory variables was identified. When risk factors were thought to represent more or less the same only one where included in the multivariate analysis. A wide array of different comorbidities and medicinal products was not assed or included in multivariate analysis due to low prevalence.
Statistical significance was defined as a two-tailed p value <0.05.
Results
Included patients had a mean age of 61.2 (± 11.7) years. In total 1857 (29.6 %) women had a T-score of less than −2.5 at either measuring site. A T-score below −2.5 in the lumbar spine was evident in 1489 (23.7 %) of patients, whereas 611 (9.8 %) and 848 (13.8 %) had a T-score in the osteoporotic range at the total hip and femoral neck region. Patient characteristics are presented in Table 1. Patients not included in the study were slightly older (mean difference −2.34 years, CI −3.04; −1.65) and had a marginally lower T-score in the total hip (mean difference 0.19, CI 0.13–0.25) and femoral neck (mean difference 0.17, CI 0.11–0.22) as compared to patients included in the study.
When comparing patients seen in 2000–2004, 2005–2008, and 2009–2012, we found that a significantly higher (overall p = 0.0004) proportion of patients included in the later periods had prevalent osteoporosis and a medical condition associated with osteoporosis. As such, 23.8, 26.5, and 29.7 % of patients had a registration of one of the mentioned medical conditions at the time of BMD measurement. Furthermore, (Table 2) a dramatic drop in the proportion of current smokers (p = >0.001) as well as an increase in the proportion of patients having received anti-osteoporotic treatment was evident. Among others an increasing proportion of patients having CPD, diabetes, MOF, and using calcium supplements were evident. Age and BMI of patients was slightly higher in the later inclusion period.
Results of the univariate analysis are presented in Table 3.
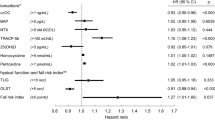
Subsequent multiple regression (Table 4) revealed age, BMI, glucocorticoid use within 1 year, a history of CPD, low-daily dietary consumption of calcium, current smoking, low exercise level, former osteoporosis treatment, former MOF, estrogen deficiency, rheumatoid arthritis (RA), prevalent alcohol-related diagnoses, and use of loop diuretics, to be independent risk factors associated with lower T-scores in the total hip. Treatment with thiazides was associated with a higher T-score.
The mentioned risk factors accounted for approximately 35 % of the variance in total hip BMD.
Of the mentioned significant associations in the total hip only glucocorticoids use, alcohol consumption and RA were not found to have the same association with low T-score at the femoral neck. Furthermore a family history of fractures was associated with low femoral neck T-scores. R 2 in the femoral neck was 0.31.
Fewer significant associations were identified at the lumbar spine. As such high age, estrogen deficiency, former MOF, former osteoporosis treatment, hyperthyroidism, low BMI, low exercise level, and family history of fractures were found to be associated with lower spinal bone mass. Loop diuretic and thiazide use were associated with a higher T-score.
At all sites an association of taking calcium supplements with low BMD was found to be present.
Effect modification/interaction with age is shown in Table 5.
At the lumbar spine, multiple interactions with age were detected.
Age stratification among others showed use of loop diuretics to be statistically associated with higher spinal T-scores in only the +75-year olds. Higher Charlson score was associated with lower lumbar spinal T-score in patients between 50 and 75 years of age. Thiazide use on the other hand was associated with higher T-scores in the lumbar spine in people above the age of 50.
When evaluating the association of potential risk factors with osteoporosis by DXA (T-score <−2.5 at any site), fewer risk factors were identified (Table 6). Age, estrogen deficiency, hyperthyroidism, prevalent MOF, former osteoporosis treatment, lower BMI, taking calcium supplementation, current smoking, no exercise, and using less thiazides were significantly associated with a higher OR of having osteoporosis. Furthermore RA and CPD was associated with osteoporosis by DXA at the total hip. Current use of loop diuretics and glucocorticoid use was associated with both total hip and femoral neck T-score below −2.5.
Discussion
In this study, we were able to demonstrate a clear independent association between many of the reviewed risk factors and low BMD in a population of predominantly postmenopausal women. Possible risk factors often not included in different risk calculators, i.e., exercise level, CPD, and use of loop diuretics were found to be associated with low BMD and potentially add information to the estimate of risk calculators. Thiazide use on the other hand seems to have a beneficial effect on BMD, and this effect might be considered when using treatment with diuretics in patients with known or suspected osteoporosis. Our data suggest that non-smoking, higher bodyweight, not having a alcohol-related diagnosis, high exercise level as well as a high intake of dietary calcium are important with regard to preservation of bone mass and may add information on both the selection of patients for osteoporosis evaluation as well as information on modifiable lifestyle factors to be used in the general prevention of osteoporosis. Efforts should be made to optimize these aspects whenever one evaluates bone health and emphasizes the need for widespread information targeted at the general population. We found that our model accounted for 35 % of the variance of BMD at the hip thus indicating that many important factors influencing bone mass are still not accounted for. The variance explained in our model are similar to or better than other studies [18–21].
Our data indicates that the risk profile of patients being referred for osteoporosis evaluation changes over time and that the proportion of patients having a medical diagnosis associated with secondary osteoporosis (as described in the supplemental material) at the time of evaluation seems to be increasing. Our findings might reflect a general tendency toward an increased focus on diseases known to be associated with fractures and secondary osteoporosis, like COPD and type-2 diabetes [22]. Adding all reported causes of secondary osteoporosis (diseases, use of glucocorticoids >450 mg and use of aromatase inhibitors within the previous year), an increase of 24 % in number of referred patients with suspected secondary osteoporosis was seen. This increased focus on secondary osteoporosis is important, since these patients often present with severe bone loss and/or elevated fracture risk. Correspondingly, we found osteoporosis prevalence to increase from 27.0 % in the start to 30.8 % in the later period.
A dramatic reduction in the proportion of current smokers was also observed. This could well be due to changes in Danish legislation which came into effect in May 2007 prohibiting smoking at public institutions, workplaces, bars, and restaurants.
The study has several strengths that make this study unique compared to others. Systematic prospective collection of self-reported and measured data from consecutively referred patients makes evaluation of risk factors of low bone mass in a real-life setting possible. Combining these with the Danish registry system, adds information not obtainable from the cohort itself. To our knowledge no other studies, describing overall risk factors of low BMD, have included information from the above-mentioned data sources.
The large number of women included over more than a decade as well as the ability to demonstrate a large number of independent associations when taking predictors attributable to both hereditary, life style, and comorbidity-related causes into account also makes this study interesting. A comprehensive picture of the overall risk profile of low BMD and osteoporosis in women can thus be presented. In traditional register-based research, information on many important aspects (i.e., smoking status, family fracture history, nutritional factors, exercise status, and menopausal status) regarding other known risk factors are missing whereby conclusions might be misleading. In this study, we were able to address many of these risk factors.
This cohort represents a spectrum of patients thought to be at risk of having osteoporosis in a real-life setting. This quality can be lacking in randomized controlled trials where strict inclusion- and exclusion criteria’s might limit the usefulness of the generated results in everyday life. Dowd et al. [23] evaluated participation eligibility of 120 patients with osteoporosis in 4 different ongoing RCT’s and found that only 3–21 % could participate. Exclusion reasons included age, co-medication, and comorbidity.
Findings from previous studies [18, 19, 24–27] and recognized risk factors [28] for osteoporosis and fractures included in different fracture risk calculators such as FRAX are in agreement with our findings, especially when looking at the total hip or femoral neck. Furthermore risk factors recognized to have a negative effect on bone health, such as low exercise level, CPD and use of loop diuretics, were confirmed [29–31].
We found increasing doses of redeemed thiazide to be associated with higher BMD in the femur and in the lumbar spine in the +50-year old. The fact that we did not find an association in the younger age group could be due to the duration of treatment and that the younger might not have been treated for a prolonged period. Furthermore the reason why thiazide is used might also be different between age groups.
A negative association with a familial fracture history at both the femoral neck and lumbar spine was found but could not be affirmed when looking at osteoporosis status. It is possible that this association would be stronger if only a hip fracture history was considered. Fractures in first-degree relatives have been shown to be associated with a small increased risk of any fracture, osteoporotic, or hip fracture even after BMD adjustment [32] emphasizing the need to address this aspect when evaluating patients.
Regarding glucocorticoid use only the negative association with total hip T-scores and site-specific osteoporosis at the total hip and femoral neck remained statistically significant.
Analyzing glucocorticoid use based on use of more than 450 mg during the last year did not change our findings. In the full multivariate analysis, both RA and CPD were significant risk factors in predicting either overall or site-specific osteoporosis by DXA, whereas IBD was not. This is in accordance with previous studies showing chronic obstructive pulmonary disease to be independently associated with osteoporosis regardless of prednisolone use [31] and that bone loss can be present even in glucocorticoid treatment naive women with RA [33]. Predictors of overall osteoporosis did not differ significantly according to osteoporosis treatment status (Table 6) although hyperthyroidism was not found to be a predictor of overall osteoporosis in treatment naïve women.
Perhaps surprisingly the use of calcium and vitamin D supplements was found to be associated with having a lower BMD. The reason for this could be that patients recognized as being at risk of osteoporosis are more likely to start taking these supplements, as soon as this is brought to their attention. This confounding by indication may mask an actual positive effect of calcium on BMD, as has been demonstrated in several studies [34]. This is emphasized by the fact that high dietary calcium intake in our study is associated with higher T-scores in the total hip and femoral neck. We did unfortunately not have any information about the dose or duration of the calcium supplementation being used, since it is available without prescription. It is possible that examining the association with total daily intake of calcium (dietary + supplementation) would have led to another result. In Denmark, Vitamin D (calcium supplements) is an over the counter drug and a large proportion of the population is using vitamin D supplements. This might be especially common among women focused on the risk of osteoporosis as its use is recommended by the national board of health in all patients believed to be at risk of osteoporosis. For these reasons, we do not find the prevalence of vitamin D supplement use is surprising.
The associations of risk factors seem to vary with age and BMD measurement site. When relating risk factors to spinal T-score, the associations was weaker. In especially older persons, the accuracy of spinal DXA measurements is weakened by changes in the region of interest, such as vertebral deformity, scoliosis, osteophytes and extraskeletal calcification, all tending to lead to a falsely elevated BMD value [1].
This could likewise be the reason for the surprising finding of loop diuretics being associated with higher spinal T-scores in the +75-year olds in contrary to the femoral findings.
Only few interactions with age were detected in the total hip and femoral neck. This is more or less in line with recent findings [35]. In contrast, the many identified effect modifications with age make use of risk factors to identify patients with low BMD in the lumbar spine more difficult from a clinical point of view, since the patients age has to be taken into account.
This study has limitations regarding lack of information about certain possible relevant risk factors of low BMD such as self-reported alcohol use. The prevalence of many risk factors of secondary osteoporosis was too low to be assessed. Register-based information from The National Hospital Discharge Register covers only registrations at hospital level. Underestimation of the prevalence of especially less severe cases of comorbidity such as alcoholism not treated at the hospital was thus evident. We have previously demonstrated that hyponatremia could be considered a novel risk factor of low bone mass, but did not include this as a risk factor in this paper [6]. Relating to dietary calcium intake categorization was done using approximations of minimum intake from dairy products and adding it to an approximate average contribution from non-dairy products. The use of a complex food frequency questionnaire was found to be too difficult to handle in routine clinical setting. Nevertheless conclusions made relating to dietary calcium intake must be interpreted with care as the calculated minimum intake from dietary calcium is a rough approximation. We therefore only conclude that higher intake seems to be beneficial but from these data a recommendation as to how high is not possible.
A significant amount of women did not have their D-vitamin measured before 2008. A very low percentage had very severe deficiency. In the univariate analysis, associations with T-scores were insignificant. After correcting for the month of which blood samples were taken, we saw a significant reduced femoral neck T-score in patients with severe deficiency. We defined adequate levels of vitamin D to be above 50 nmol/L for adequate skeletal health but recognize that for patients considered at risk of osteoporosis, a higher level (75 nmol/L) might be better [36].
A clear underestimation of the prevalence of spinal fractures is present, since routine x-rays of the spine was not a part of the individual evaluation and that vertebral fractures in general often remain undiagnosed, despite the presence of clinical signs [37]. We did not have any information about the trauma mechanism of fractures (high or low trauma). In order to include fractures more frequently associated with osteoporosis, only fractures at a major osteoporotic site were included. As referral is based on specific recognized risk factors some degree of selection bias cannot be excluded and this could influence generalizability of our results. It is likewise possible that patients being healthier in general are the ones being referred.
A significant limitation of this study is that we evaluated risk of low BMD and osteoporosis and not risk of experiencing a fracture. Some of the evaluated risk factors have in other studies been shown to be associated with fractures at least partly independent of BMD. The fact that we do not find these risk factors to be a predictor of low bone mass does not imply that these risk factors are unimportant in terms of fracture risk. In conclusion, a systematic collection of clinical information, questionnaire data, and individual coupling with information from the unique Danish national registries enables a platform for further studies to be established. Modifiable risk factors identified in this study could be potential candidates in a prevention strategy among the background population. Our study advocate that avoiding excessive alcohol intake and smoking, doing exercise more than once a week as well as having a relevant dietary calcium intake is likely to be beneficial. The findings of a negative association of loop diuretic use and a positive effect of thiazide diuretics with relation to T-scores should be considered when diuretic treatment is needed in patients with osteoporosis. Our findings furthermore emphasize the need to be aware of the negative effect of diseases such as CPD and RA, regardless of glucocorticoid use. Finally our data indicate that the risk profile of patients is changing over time and that the proportion of referred patients having a medical disorder potentially associated with increased risk of osteoporosis seems to be growing.
References
E. Hernlund, A. Svedbom, M. Ivergård, J. Compston, C. Cooper, J. Stenmark, E.V. McCloskey, B. Jönsson, J.A. Kanis, Osteoporosis in the European Union: medical management, epidemiology and economic burden: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 8, 136 (2013). doi:10.1007/s11657-013-0136-1
D. Marshall, O. Johnell, H. Wedel, Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312, 1254–1259 (1996)
E.S. Siris, R. Adler, J. Bilezikian, M. Bolognese, B. Dawson-Hughes, M.J. Favus, S.T. Harris, S.M. Jan de Beur, S. Khosla, N.E. Lane, R. Lindsay, A.D. Nana, E.S. Orwoll, K. Saag, S. Silverman, N.B. Watts, The clinical diagnosis of osteoporosis: A position statement from the National Bone Health Alliance Working Group. Osteoporos. Int. 25(5), 1439–1443 (2014). doi:10.1007/s00198-014-2655-z
E.R. Bogoch, V. Elliot-Gibson, D.E. Beaton, S.A. Jamal, R.G. Josse, T.M. Murray, Effective initiation of osteoporosis diagnosis and treatment for patients with a fragility fracture in an orthopaedic environment. J. Bone Joint Surg. Am. 88, 25–34 (2006)
A.R. McLellan, S.J. Gallacher, M. Fraser, C. McQuillian, The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos. Int. 14, 1028–1034 (2003)
J.P. Holm, A.O. Amar, L. Hyldstrup, J.E. Jensen, Hyponatremia, a risk factor for osteoporosis and fractures in women. Osteoporos. Int. 27, 989–1001 (2016)
E. Saxholt, S. Fagt, J. Matthiessen, T. Christensen, Den lille Levnedsmiddeltabel, 4th edn. (Danmarks Tekniske Universitet, Fødevareinstituttet, 2010)
T. Kelly, Bone mineral reference databases for American men and women. J. Bone Miner. Res. 5(Suppl1), S249 (1990)
A.C. Looker, H.W. Wahner, W.L. Dunn, M.S. Calvo, T.B. Harris, S.P. Heyse, C.C. Johnston, R. Lindsay, Updated data on proximal femur bone mineral levels of US adults. Osteoporos. Int. 8, 468–489 (1998)
J.T. Schousboe, J.A. Shepherd, J.P. Bilezikian, S. Baim, Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on bone densitometry. J Clin Densitom 16, 455–466 (2013)
C.A. Nowson, J.J. McGrath, P.R. Ebeling, A. Haikerwal, R.M. Daly, K.M. Sanders, M.J. Seibel, R.S. Mason, Vitamin D and health in adults in Australia and New Zealand: a position statement. Med. J. Aust. 196, 686–687 (2012)
L.C. Thygesen, C. Daasnes, I. Thaulow, H. Brønnum-Hansen, Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health. 39, 12–16 (2011)
H.W. Kildemoes, H.T. Sørensen, J. Hallas, The Danish National Prescription Registry. Scand. J. Public Health 39, 38–41 (2011)
P. Vestergaard, L. Rejnmark, L. Mosekilde, Fracture risk associated with systemic and topical corticosteroids. J. Intern. Med. 257, 374–384 (2005)
E. Lynge, J.L. Sandegaard, M. Rebolj, The Danish National Patient Register. Scand. J Public Health. 39, 30–33 (2011)
P. Vestergaard, L. Mosekilde, Fracture risk in patients with celiac disease, Crohn’s disease, and ulcerative colitis: a nationwide follow-up study of 16,416 patients in Denmark. Am. J. Epidemiol. 156, 1–10 (2002)
S.K. Thygesen, C.F. Christiansen, S. Christensen, T.L. Lash, H.T. Sørensen, The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med. Res. Methodol. (2011). doi:10.1186/1471-2288-11-83
W.S. Browner, J.A. Cauley, E.S. Orwoll, J.C. Scott, D.M. Black, J.L. Tao, S.R. Cummings, Factors associated with appendicular bone mass in older women. The Study of Osteoporotic Fractures Research Group. Ann. Intern. Med. 118, 657–665 (1993)
E.S. Orwoll, D.C. Bauer, T.M. Vogt, K.M. Fox, Axial bone mass in older women. Study of Osteoporotic Fractures Research Group. Ann. Intern. Med. 124, 187–196 (1996)
J.A. Cauley, R.L. Fullman, K.L. Stone, J.M. Zmuda, D.C. Bauer, E. Barrett-Connor, K. Ensrud, E.M.C. Lau, E.S. Orwoll, Factors associated with the lumbar spine and proximal femur bone mineral density in older men. Osteoporos. Int. 16, 1525–1537 (2005)
G. Bączyk, T. Opala, P. Kleka, M. Chuchracki, Multifactorial analysis of risk factors for reduced bone mineral density among postmenopausal women. Arch. Med. Sci. 2, 332–341 (2012)
M. Janghorbani, R.M. Van Dam, W.C. Willett, F.B. Hu, Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am. J. Epidemiol. 166, 495–505 (2007)
R. Dowd, R.R. Recker, R.P. Heaney, Study subjects and ordinary patients. Osteoporos. Int. 11, 533–536 (2000)
B. Heidari, R. Hosseini, Y. Javadian, A. Bijani, M.H. Sateri, H.G. Nouroddini, Factors affecting bone mineral density in postmenopausal women. Arch. Osteoporos. (2015). doi:10.1007/s11657-015-0217-4
J.A. Kanis, H. Johansson, O. Johnell, A. Oden, C. De Laet, J.A. Eisman, H. Pols, A. Tenenhouse, Alcohol intake as a risk factor for fracture. Osteoporos. Int. 16, 737–742 (2005)
C. De Laet, J.A. Kanis, A. Odén, H. Johansson, O. Johnell, P. Delmas, J.A. Eisman, H. Kroger, S. Fujiwara, P. Garnero, E.V. McCloskey, D. Mellstrom, L.J. Melton, P.J. Meunier, H.A.P. Pols, J. Reeve, A. Silman, A. Tenenhouse, Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos. Int. 16, 1330–1338 (2005)
J.A. Kanis, O. Johnell, A. Oden, H. Johansson, C. De Laet, J.A. Eisman, H. Kroger, E.V. McCloskey, D. Mellstrom, L.J. Melton, H. Pols, J. Reeve, A. Silman, A. Tenenhouse, Smoking and fracture risk: a meta-analysis. Osteoporos. Int. 16, 155–162 (2005)
D. Preiss, P. Welsh, S.A. Murphy, J.E. Ho, D. Waters, D.A. DeMicco, C.P. Cannon, M.S. Sabatine, S.R.K. Seshasai, P. Barter, E. Braunwald, J.J.P. Kastelein, J.A. De Lemos, M.A. Blazing, T.R. Pedersen, M.J. Tikkanen, N. Sattar, K.K. Ray, Osteoporosis prevention, diagnosis, and therapy. JAMA 285, 785–795 (2001)
B. Abrahamsen, D. Brask-lindemann, K.H. Rubin, P. Schwarz, A review of lifestyle, smoking and other modifiable risk factors for osteoporotic fractures. Bonekey Rep. 3, 1–7 (2014)
L. Rejnmark, P. Vestergaard, L. Mosekilde, Fracture risk in patients treated with loop diuretics. J. Intern. Med. 259, 117–124 (2006)
S.-J. Chen, W.-C. Liao, K.-H. Huang, C.-L. Lin, W.-C. Tsai, P.-T. Kung, K.-H. Chang, C.-H. Kao, Chronic obstructive pulmonary disease and allied conditions is a strong independent risk factor for osteoporosis and pathologic fractures: a population-based cohort study. QJM (2015). doi:10.1093/qjmed/hcv012
J.A. Kanis, H. Johansson, A. Oden, O. Johnell, C. De Laet, J.A. Eisman, E.V. McCloskey, D. Mellstrom, L.J. Melton, H.A.P. Pols, J. Reeve, A.J. Silman, A. Tenenhouse, A family history of fracture and fracture risk: a meta-analysis. Bone 35, 1029–1037 (2004)
C. Roux, Osteoporosis in inflammatory joint diseases. Osteoporos. Int. 22, 421–433 (2011)
I.R. Reid, B. Mason, A. Horne, R. Ames, H.E. Reid, U. Bava, M.J. Bolland, G.D. Gamble, Randomized controlled trial of calcium in healthy older women. Am. J. Med. 119, 777–785 (2006)
S. Andersen, P. Laurberg, Age discrimination in osteoporosis screening—data from the Aalborg University Hospital Record for Osteoporosis Risk Assessment (AURORA). Maturitas 77, 330–335 (2014)
E.-H. Fuleihan, R. Bouillon, B. Clarke, M. Chakhtoura, C. Cooper, M. McClung, R.J. Singh, Serum 25-hydroxyvitamin D levels: variability, knowledge gaps, and the concept of a desirable range. J Bone Miner. Res. 30, 1119–1133 (2015)
R. Nuti, C. Caffarelli, G. Guglielmi, L. Gennari, S. Gonnelli, Undiagnosed vertebral fractures influence quality of life in postmenopausal women with reduced ultrasound parameters. Clin. Orthop. Relat. Res. 472, 2254–2261 (2014)
Acknowledgments
No financial or other support in any way has been granted as a consequence of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JPH has participated as a subinvestigator in studies by Amgen and MSD. JEBJ: Board membership in Amgen, Eli Lilly, MSD, Novartis, Nycomed. Payment for lectures by Amgen, Eli Lilly and MSD. LH has been giving lectures sponsored by Novartis, Lilly, Takeda/Nycomed, Novo-Nordisk, Amgen, GlaxoSmithKline, Servier, MSD, Ferrosan, Pfizer, PharmaVinci and Renapharma.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by Statens Serum Institute, the Danish Data Protection Agency and Statistics Denmark.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Holm, J.P., Hyldstrup, L. & Jensen, JE.B. Time trends in osteoporosis risk factor profiles: a comparative analysis of risk factors, comorbidities, and medications over twelve years. Endocrine 54, 241–255 (2016). https://doi.org/10.1007/s12020-016-0987-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-0987-5