Abstract
Cataract, characterized by the opacification of the lens, is the leading cause of reversible blindness and visual impairment globally. The study aims to investigate the role of trace elements such as Cd, Co, Cr, Cu, Fe, Hg, Mn, Ni, Pb, Se, and Zn in the development and severity of cataract. Elements were quantified by inductively coupled plasma mass spectrometry in blood and aqueous humor of 32 cataract cases and 27 controls living in the Latium region, Italy. The association between element concentration in blood and aqueous humor and cataract severity, gender, and age of subjects were also assessed. Results showed Cr levels significantly elevated in both blood and aqueous humor of cataract cases, with concentrations that increased with cataract severity. In addition, blood Pb levels were significantly higher in older cases and positively correlated with the age of cataract cases, while blood Co and Cu levels negatively correlated with cataract severity, suggesting changes in the levels of these elements. In conclusion, this study provides evidence of the involvement of specific elements in cataract development and severity, and the findings highlighted important avenues for future research. Understanding the biological mechanism underlying element-induced cataract may contribute to preventing cataractogenesis and providing targeted interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cataract is an opacification of the lens that obscures the passage of light to the retina of the eye leading to a visual impairment. It is the main cause of reversible blindness with an estimated 95 million people affected worldwide. In addition, it is reported that more than 10 million people worldwide are blind due to cataract [1]. In Italy, the cataract affects ca. 8.5% of adults aged 70–74 years, 12.4% aged 75–80 years, and 17.1% aged over 80 years [2]. Moreover, approximately 650,000 people undergo cataract surgery every year in Italy [3].
The most common risk factors are related not only to aging and UV exposure but also systemic disorders (e.g., autoimmune and chronic kidney diseases, hypertension, and diabetes mellitus), lifestyles (e.g., smoking or heavy alcohol intake), obesity, family history, trauma, and use of steroids which may accelerate the development of cataract [4].
In general, age-related changes in lens transparency can be the response to toxic environmental factors causing excessive generation of reactive oxygen species (ROS). In this context, the ROS can induce protein and lipid aggregation in the lens and aqueous humor [5, 6].
In addition, the exposure to toxic trace elements and the disruption of the homeostasis of essential trace elements can influence the pathophysiological changes in the human body by formation of ROS, including in the ocular compartment creating the conditions for the development of eye diseases. Concerning toxic elements, Cd may contribute to mitochondria damage playing a crucial role in the formation of ROS making the lens less resistant to photooxidation improving the risk of cataract formation [5, 7]. In addition, it has been reported that Cd accumulates in the nervous retina, choroid, and retinal pigment epithelium (RPE), and the deleterious effects of Cd on RPE cells included altered cell morphology, decreased cell survival, elevated ROS levels, and concentration-dependent disruption of membrane integrity [6, 8].
Chromium occurs ubiquitously in nature and exists mainly in two stable forms as trivalent Cr(III) and hexavalent Cr(VI). Both forms have recognized toxicity at various levels in the human body inducing oxidative stress [9,10,11]. Regarding Cr, the authors reported that heat shock proteins HSP90aa1 and S100, both involved in many cellular processes [12, 13], functionally interact during the regulation of retinal cells under the influence of Cr ions. The metal has led to retinal edema playing an important role in the development of retinopathy [14, 15].
Once in the body, Hg exerts its toxicity in different way, including mitochondrial dysfunctions and the formation of ROS since it may act as catalyst for Fenton-type reactions [16]. It has been reported that Hg(II) ions induce the non-amyloid aggregation of human γC- and γS-crystallins, two of the most abundant γ-crystallins in lens, uncovering the Hg potential role in the bioinorganic chemistry of cataract. The mechanism of Hg-induced aggregation involves direct metal-lens protein interactions and poses the basis for cataractogenesis [17].
Nickel exposure leads to the formation of free radicals in tissues, leading to a cascade of damaging events [18]. Fish eye exposed to Ni reported cellular anomalies in the primary function of retina leading to visual loss or poor vision [19]. Yet again, Ni levels in human cadaver donor eyeballs were significantly increased in late age-related macular disease (AMD) compared to controls [20].
Concerning Pb, it can create oxidative stress inhibiting the antioxidant defense and depleting glutathione [21, 22]. The authors reported the association between Pb bone levels and cataract [23], suggesting that reduction of Pb exposure may decrease the global burden of cataract. In addition, physiologically relevant dosages of Pb can induce lenticular opacity in vitro and degradation of crystallins and cytoskeletal proteins [24]. Moreover, Pb exposures are suggested to be risk factors for increased blood retinal barrier (BRB) permeability in AMD [25].
Among the essential elements, Co is a component of vitamin B12 and is required for cell activity [26]. Cobalt is also capable of being toxic at high levels for various organs and systems, including the nervous one leading to the altered visual function [27,28,29]. The eye toxicity can be exerted by the capacity of Co (i) to bind to albumin and transferrin proteins and their distribution throughout the body, (ii) to block the Ca-dependent synaptic transmission including those of the photoreceptors, (iii) to interfere with the mitochondria cellular respiration leading to oxygen deprivation, and (iv) to act in chemically induced hypoxia-mimicking conditions by stimulating hypoxia-inducible factors that can lead to retinal photoreceptor cell degeneration [29]. On the other hand, deficiency of Co, although rare in adults, might cause several symptoms (i.e., weakness, loss of appetite and weight, paleness, fatigue, and eye watery discharge) [30]. In the eyes, intravitreal injection of cobalt chloride in mouse was able to induce retinal photoreceptor degeneration because of the vulnerability of photoreceptor cells to oxygen environment in the degenerative process [31].
Copper is a redox-active metal that plays a key role as a catalytic cofactor for Cu-dependent enzymes [32]. Copper is found in different retinal regions, and the retinal physiology and functions are related to the concentrations of this element as well as Cu is able to modify the activity of rhodopsin in retina [33]. On the other hand, the interaction of Cu(II) ions with γD-, γC-, and γS-crystallins induced their non-amyloid aggregation causing lens opacity [34].
The role of Fe in various and vital cellular metabolism and its involvement in oxidative damage through Fe catalyzed formation of ROS is well known. The Fe-induced ROS participates in tissue damage leading to corneal disease, light-induced retinopathy, cataractogenesis, AMD, retinal degeneration, photoreceptor damage in uveitis, glaucoma, and diabetic retinopathy [35, 36].
Manganese is an element that maintains proper cell function as well as it is a co-factor for many enzymes [37]. In eyes, cone function abnormalities on an electroretinogram, which correspond with impaired renewal of photoreceptor outer segment discs, have been associated with dietary Mn deficiency [38, 39]. Moreover, Mn was found to be lower in cataractous lenses with respect to controls [40].
Selenium as selenoproteins or selenocysteine can reduce the increased level of hydrogen peroxide present in the aqueous humor of cataract subjects protecting the lens against ROS-induced damage [1]. On the other hand, studies suggested that low Se levels may negatively affect lens metabolism, increasing the opacity [41, 42]. Deficiency of serum Se levels may pose a potential risk factor for both nuclear and cortical age-related cataracts [43].
Zinc plays a vital role in the normal functioning of antioxidant enzymes and protects eye structures from the deleterious effects of light and oxidative stress. A decrease in the intracellular Zn level may increase the vulnerability of RPE cells to UV irradiation inducing RPE cell apoptosis [44] and may hinder dark adaption [45]. Increased Zn levels may lead to increased metallothionein concentrations or to the oxidation of sulfhydryl groups; these results may reduce the permeability of the lens membrane. In addition, elevated levels of Zn in lens linked to the presence of high molecular weight proteins could be considered as precursors of insoluble protein aggregates causing lens opacification [1].
Thus, variations of levels of toxic and essential trace elements in the body might be associated with the development of eye diseases, cataract included. To this end, the present study determined Cd, Co, Cr, Cu, Fe, Hg, Mn, Ni, Pb, Se, and Zn in blood and aqueous humor of cases affected by cataract with respect to their levels in controls, also considering risk factors as patient gender and aging. The final objective was to provide data relative to cataract and human health and possibly make a contribution in preventing cataractogenesis.
Materials and Methods
Subjects
Thirty-two cases (mean age, 75.0 ± 9.0 years; 19 females and 13 males) with cataract were recruited from the Unit Departmental Emergency Ophthalmologic of the Umberto I Hospital of Rome, Italy. Except for the presence of cataract, no other injuries were observed in eye structures in cases. Samples of blood and aqueous humor were collected from each of them.
As controls, blood was collected from 27 blood donors (mean age, 75.8 ± 7.1 years; 18 females and 9 males) who have attended routine ophthalmological examinations. Controls did not have neither cataract nor any other eye diseases.
The presence and degree of cataracts were diagnosed by standard procedures, including slit lamp fundus examination, intraocular pressure measurement, visual field examination, and optical coherence tomography (OCT) scans. Cataracts were classified following the Lens Opacities Classification System III [46] and indicated as low, medium, and high in this study. Table 1 reports the characteristics of subjects. All subjects filled out a detailed questionnaire reporting personal characteristics, lifestyles, diet, residence, occupation, outdoor activity, supplementation, metallic prosthesis, etc.
Participants facing the following inclusion criteria were included in the study: intraocular pressure < 21 mmHg; no conditions affecting the retina and optic nerve such as glaucoma, macular degeneration, diabetic retinopathy, or HIV-related retinopathy; no history of ocular trauma or visual field alterations; absence of posterior pole diseases such as macular degeneration and absence of ocular media opacities such as cataracts; no previous ophthalmic surgery; and absence of neurodegenerative diseases. In addition, the following criteria were used to exclude participants: heavy drinkers, current smokers; presence of body prosthesis; intake of nutritional supplements; intake of drugs; and special diets (as vegan or vegetarian). The enrolled participants presented a normal BMI in the range of 19.71–24.74 kg/m2; they were moderate drinkers (up to 2 drinks on average per day); they were non-smokers or had quit smoking for at least 10 years; most of them had a very limited outdoor activity and were retired from work, did not present metallic prosthesis in the body, and declared to consume a mixed diet.
All subjects gave the written informed consent before procedures. The study protocol was approved by the Institutional Ethical Committee of the University of Rome (protocol number 1005/2021, approval date November 10, 2021) and conducted according to the Declaration of Helsinki.
Sample Preparation
One milliliter of blood from each subject was collected into a 15-ml polistyrene tube and added with 2 ml of ultrapure HNO3 (VWR, Leuven, Belgium) and digested on a heat block (ModBlock, CPI International, Santa Rosa, CA, USA) at 80 °C until complete dissolution. The digests were further diluted with ultrapure deionized water (Micro Pure UV, Thermo Scientific Barnstead, Langenselbold, Germany). Procedural blanks were used to assess the possible metal contamination from plastics and reagents. The certified reference material (CRM) ClinChek® Whole Blood Control, Level I (Recipe, Munich, Germany) was analyzed to determine method recovery and intra-day precision. Accuracy was in the range of 93–105% and precision between 4.3 and 8.1% for all elements.
Approximately 100 μl of aqueous humor samples were collected from cases undergoing cataract surgery using phacoemulsification. Intraoperatively, aqueous humor samples were obtained through an insulin syringe and further stored at − 20 °C. For element analysis, aqueous humor samples were simply diluted 1:20 v/v with high purity deionized water (Micro Pure UV). Quality was controlled with CRMs, namely, the Seronorm lyophilized human urine level 1 and level 2 (Sero AS, Billingstadt, Norway). Accuracy ranged between 90 and 111% at level 1 and between 92 and 98% at level 2. Precision on replicated measurements of CRMs was better than 10% and 5.3% at level 1 and level 2.
Determination of Trace Elements
The Thermo Scientific iCAP Q inductively coupled plasma mass spectrometry (iCAP Q ICP-MS, Bremen, Germany) was used to quantify the following elements: 114Cd, 59Co, 52Cr, 63Cu, 56Fe, 202Hg, 55Mn, 60Ni, 82Se, 208Pb, and 64Zn. In order to efficiently reduce polyatomic interferences on the analytical masses, the He pressurized QCell in Kinetic Energy Discrimination (KED) mode was employed. The addition calibration method was used to quantify the elements, and 103Rh at 1 ng/ml in the analytical solutions was used as internal standard to account for possible instrumental drifts.
Statistics
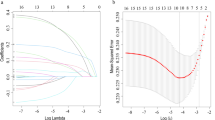
Since data were not normally distributed, results were expressed as median (P50), 5th and 95th percentiles (P5–P95). Differences between elements in cases and controls and association element-variables (gender, age, and stage of disease) were tested by non-parametric tests (U Mann–Whitney, Kruskal–Wallis, Spearman’s ρ), and p values < 0.05 were considered statistically significant. Moreover, the receiver-operating characteristic (ROC) curves were used to establish an element concentration threshold value in blood able to distinguish cases and controls. The quality of ROC results was expressed in terms of the area under the ROC curve (AUC), specificity (proportion of correctly identified controls, also referred to as false positive rate), and sensitivity (proportion of correctly identified cataractous cases, also called true positive rate). The IBM SPSS Statistics 28 was used as a statistical package.
Results
Table 2 reports the concentration of trace elements in the blood of cataract cases and controls. Results showed significantly higher blood Cr levels (P50; 1.26 ng/ml vs. 0.46 ng/ml; p = 0.004) in cases when compared to controls.
Considering the gender, only blood Cr content resulted significantly increased in diseased males with respect to control males (P50; 1.27 ng/ml vs. 0.37 ng/ml; p = 0.030), and a similar trend was also observed in females although not significant (P50; 1.25 ng/ml vs. 0.58 ng/ml; p > 0.05).
In addition, dividing the cases into two age-groups (15 cases ≤ 70 years and 17 cases > 70 years), blood Pb concentration was significantly higher in the oldest group (P50; 30.1 ng/ml vs. 16.0 ng/ml; p = 0.009; Fig. 1), while the other elements were not associated with age.
Also, by the correlation analysis, blood Pb levels (p = 0.008; ρ = 0.464) positively correlated with the age of cases.
Considering the cataract severity, blood Cr content resulted significantly elevated in cases of the high severity group with respect to the medium severity group (P50; 1.35 ng/ml vs 0.60 ng/ml; p = 0.022; Fig. 2).
On the contrary, both blood Co (P50; 0.30 ng/ml vs. 0.21 ng/ml; p = 0.049; Fig. 3) and Cu (P50; 1024 ng/ml vs. 895 ng/ml; p = 0.016; Fig. 4) levels significantly decreased in cases of the high severity group with respect to the medium severity group.
Using the correlation analysis, blood Cr (p = 0.02; ρ = 0.434) positively correlated with cataract severity; while blood Co (p = 0.048; ρ = − 0.352) and Cu (p = 0.013; ρ = − 0.410) levels were negatively correlated with severity.
Furthermore, the ROC analysis was used as a diagnostic test to determine the blood Cr concentration threshold level able to discriminate cataract cases from controls and concentrations of 0.38 ng/ml of Cu (AUC, 0.721; sensitivity, 91%; specificity, 70%) accurately divided cases from the control group.
Table 3 sets forth trace element values in the aqueous humor of cataract cases, with the highest concentration observed for Zn followed by Fe > Se > Cu. Among toxic elements, the highest humor aqueous concentration was detected for Ni, followed by Hg > Mn and Pb. Very low levels of Cd, Co, and Cr were found in humor aqueous samples of cataract cases.
As in blood, Cr was raised in subjects of the high severity group with respect to the medium severity group (P50; 1.24 ng/ml vs. 0.78 ng/ml; p = 0.045; Fig. 5).
In addition, the correlation test confirmed the positive correlation between Cr in the aqueous humor and disease severity (p = 0.043; ρ = 0.392).
Discussion
Cataract is a progressive loss of transparency of the eye lens, and the mechanism of cataractogenesis has not been fully elucidated. However, several factors increase the risk of cataract formation such as cigarette smoking, genetics, UV light, systemic diseases, intake of drugs, other eye diseases, exposure to toxic elements, and disrupted homeostasis of essential elements [47]. Regarding elements, they are ubiquitous considering that, nowadays, humans are exposed to elements from different sources (food, cosmetics, jewelry, drinking water, air, metal prosthesis, etc.) and via several exposure routes (environment, diet, lifestyles, residential areas, occupational settings, etc.). The aim of this case–control study was to detect the variations in trace element content that can be ascribed to the cataract disease reducing as much as possible some confounding factors such as a residential area, occupation, smoking, alcohol, supplementations, drug intake, and type of diet.
Moreover, to have more complete information, this study collected and further analyzed for trace elements in both the aqueous humor and blood of cataract cases. Aqueous humor is the clear liquid in the posterior and anterior chambers of the eye produced by the ciliary processes, and it represents the surrogate vascular system for the cornea and lens, delivering nutrients and removing metabolic waste for these avascular tissues [48, 49]. The aqueous humor analysis allows us to obtain information on the accumulation or decrease of elements in situ likely due to the presence of cataract. On the other hand, the blood analysis instead provides information on the systemic exposure to elements. Blood element composition may reflect changes due to a diseased condition or it may reflect contributions of factors ranging from genetics to lifestyles. The integrated information obtained from aqueous humor and blood allowed a more comprehensive insight into the role of elements in cataract.
In addition, the obtained trace elements data can help in the early diagnosis of cataracts by understanding the biology of this disease and may suggest opportunities for cataract treatment. For example, supplementation of Cu, Co, Zn, ascorbic acid, etc. could ameliorate symptoms and problems as well as it may slow the progression of the disease. This might help the patients’ quality of life and the National Health System in terms of reduction of hospitalization and economic saving.
Results showed that Cr levels were significantly increased in blood of subjects with cataract with respect to controls, and the metal significantly raised with the higher severity of the disease. This accumulation was also observed in the aqueous humor of cataractic subjects and also in this matrix the Cr content positively correlated with the severity of cataract. These findings supported the hypothesis that accumulations of toxic metals such as Cr in cataractic subjects could contribute to the pathogenesis of the disease. Interestingly, ROC analysis showed that a concentration of blood Cr concentration equal to 0.38 ng/ml was able to discriminate cataract cases from controls. The authors observed visual defects and undifferentiated cornea, lens, and retina of the chicken eye when treated with Cr(VI) [50]. Once more, structural damage of the cornea of albino rats and visual impairment due to Cr(VI) was observed [51]. Moreover, several hazards to the cornea and lens of rats and severe morphological and histological changes were induced by the administration of Cr-picolinate, but the authors reported that these damaging effects can be restored by supplementation of the amount of vitamin C [52]. Wu et al. exposed human corneal epithelial (HCE) cells to Cr(VI) and observed ROS formation causing DNA strand breaks in HCE cells. They also reported that simultaneous administration of hyaluronic acid increased HCE cell survival rates [53]. Thus, some beneficial effects of supplementation could be considered, in the future, against the eye toxicity caused by Cr [52, 53].
Regarding the few studies on Cr reported in the literature, results were contradictory and not decisive on the role of Cr in the eye. Among them, an exploratory study based on the analysis of aqueous humor and lens samples collected from cataract patients revealed that Cr was the most common metal found in both matrices [54]. A similar study reported the presence of Cr in the aqueous humor in 77 patients with cataract. In addition, Cr was quantified in the aqueous humor and serum in cataract patients with and without diabetes mellitus [55]. The authors found that the aqueous humor Cr level in eyes with diabetes cataract was significantly lower than that in eyes with senile cataract [56]. Another study reported a decreased level of Cr in aqueous humor of subjects with glaucoma with respect to controls [57], while Haddad evidenced an accumulation of Cr in the eye lenses of females with respect to males [58]. On the other hand, authors did not find significant differences in the serum concentrations of Cr among patients with pseudoexfoliation syndrome (PEX), pseudoexfoliation glaucoma (PEG), and the control subjects [59].
Lead is an ubiquitory metal, and its exposure can cause numerous acute and chronic diseases in humans [60, 61]. In this study, Pb blood concentrations of the diseased cases and controls were similar, but differences in blood Pb levels were found in the diseased group as a function of age. The gradual rise in adult blood Pb levels with increasing age may reflect an increase in bone remodelling with age. In fact, it has been reported that Pb is stored in bone for 10–30 years, and during the lifetime, it is released back into the blood (as an endogenous source) by bone remodelling [62].
Considering the eyes, Pb accumulates over time in the RPE and choroid of the eye increasing oxidative stress which can induce chronic diseases of aging [63]. Thus, the bioaccumulation of Pb with age as a possible risk factor for senile cataract and its effect on the eye cannot be excluded. On the other hand, no relevant issues were observed in aqueous humor. There is no conclusive scientific evidence for the Pb involvement in the formation of cataract. A study examined the associations between blood Pb and cataract risk, and no relationship between cataract surgery and blood Pb was observed [6]. Other authors quantified Pb levels in cataractous human lenses, but not in normal ones [64]. Shukla et al. [65] reported higher concentrations of Pb in lenses from cataract subjects than in control subjects. The same authors suggested that molecular arrangement in the eye lens lattice has been altered due to the presence of high concentrations of Pb leading to cataract development [65]. An epidemiological study reported a higher risk for cataracts when the highest versus lowest quintiles of bone Pb levels in a longitudinal cohort study were compared, while blood Pb levels were not associated with higher risk of cataract [23]. Moreover, Pb levels detected in aqueous humor of subjects with glaucoma and cataract were not different [66]. In other postmortem studies, higher levels of Pb were found in the retina of donor eyes with age-related macular degeneration (AMD) compared to the control eyes, while this increment was not observed in choroid-RPE complex of postmortem eyes [20, 67, 68].
With reference to Co, both excess and deficiency of this metal can be harmful for the human health [29, 30]. In addition, vitamin B12 deficiency was associated with optic neuropathy characterized by slow-progressing optic atrophy [30, 69, 70]. Some studies demonstrated that serum vitamin B12 levels are decreased in glaucoma patients [71, 72]. An epidemiological study found that subjects with vitamin B12 deficiencies reported a higher incidence of early and late AMD diagnosis [73]. The supplementation of vitamin B12 was reported to improve the neuropathic pain in the eye dry disease [74, 75] and a strong protective influence on cortical cataract was observed [76]. The present results did not find the difference between Co in cases and Co in controls neither in blood nor in aqueous humor, but data showed that blood Co concentrations decreased (of ca. 2-times) with the higher severity of the disease. Also, for Co, the literature data are poor, and results from different studies are quite inconsistent. Considering the serum matrix, the authors did not find difference between the Co levels in controls and glaucomatous subjects [77]. In aqueous humor collected from patients with and without AMD undergoing cataract surgery, Co level was found ca. 3-times higher in AMD patients with respect to controls [78]. Hou et al. quantified Co in normal and senile cataractous lenses, and the metal was significantly lower in senile cataractous lenses than those in normal lenses [40]. In another study, Co was found comparable in the aqueous humor of patients with primary open-angle glaucoma (POAG), pseudoexfoliation glaucoma (PEXG), and controls [79].
Although Cu has proper function in eye due to its high affinity to the retina, reduction or increasing of its level could create impairment in the visual function. In the case of reduction, patients reported reduced color vision and visual acuity, retinal nerve fiber thinning, optic atrophy, and constricted visual fields [33]. Damaged vacuole-containing myelin and optic nerve demyelination were observed in Cu deficiency in rats fed diets with insufficient Cu. The authors related these effects to the reduced activity of cupro-enzymes or free Cu ions involved in the synthesis of phospholipids [80]. In the serum of subjects with AMD, the increased levels of homocysteine, homocysteine-thiolactone, and oxidative stress with concomitant decreased contents of Cu may play a role in the pathogenesis of this disease [81].
On the contrary, an excess of Cu may accelerate the formation of ROS causing inflammation and direct damage to cell membranes and mitochondria. Moreover, Cu can induce retinal neuron death by activation of nitric oxide synthetase and interaction with glutamatergic NMDA and AMPA receptors. [33].
As observed in the case of Co, the blood Cu levels negatively correlated with the severity of the cataract. It can be supposed that cataract severity may contribute to disturbing metal homeostasis boosting several detrimental effects on the eye including the oxidative stress increment, antioxidant barrier reduction, impairment of DNA repair mechanisms, apoptosis of lens epithelial cells, and disruption of the balance of proteins and lipids in lens [6]. On the contrary, the homeostasis of metals as Co and Cu is essential for maintaining a healthy balance of antioxidants and proper redox regulation preserving lens clarity and preventing cataracts.
It has been reported that middle-aged people improved their survival with a Cu/Zn supplementation in a long-term study of eye disorder [82], and another study reported that the risk of AMD progression was reduced by supplementing the patients with Cu and Zn [83].
As for the other elements, previous published data on Cu were inconclusive. In particular, Rai et al. [84] reported increased level of serum Cu in patients with cataract. Monoj and Jayaram [85] showed no significant alterations in the levels of Cu in serum of senile mature cataract patients. Another study indicated increased Cu blood level in subjects with optic neuritis [86]. Yildirim et al. [87] quantified Cu in lens of subjects with and without pseudoexfoliation syndrome (PSX), and the results were not statistically different as well as those found by Panteli et al. [88] in aqueous humor. In pseudoexfoliative cataract group, Cumurcu et al. [89] reported high levels of Cu in aqueous humor, lens, and serum compared to controls evidencing a role in the cataract process. Other authors did not find the difference in Cu in serum and aqueous humor when glaucomatous subjects and controls were compared [66, 77]. Association between AMD and aqueous humor Cu levels was assessed by Junemann et al. [78] reporting lower Cu concentrations in AMD than non-AMD subjects.
The other metals did not result to be significantly different between cases and controls and did not significantly change with other factors as gender, cataract severity, and age, thus leading to the interpretation that they were not significantly linked to the development or the progression of cataracts.
Conclusions
Environmental pollutants may have a role in the molecular mechanisms underlying common diseases, such as cataract. Both the exposure to toxic elements and the disrupted homeostasis of essential elements may start cellular processes able to pose risks for cataractogenesis.
Regarding toxic elements, blood Cr levels were higher in cases than in controls, and Cr contents positively correlated with the severity of the disease in both blood and aqueous humor. In addition, higher blood Pb concentrations in older cases, suggest that Pb bioaccumulation with age is a possible risk factor for senile cataract development. Essential elements such as Co and Cu decreased in blood as the severity of the disease increased.
All these elements may have a role in cataract-associated metabolic pathways, as for example, the increase in ROS production and the decrease of antioxidant defenses, the interference with the mitochondria leading to oxygen deprivation, and the retinal photoreceptor cell degeneration. Thus, the maintenance of the homeostasis of essential elements such as Co and Cu and the lower possible level of toxic ones such as Cr and Pb may have great importance in eye disease prevention and in general in public health prevention.
The obtained results were in line or different with respect to previous published studies. The variations among studies can be linked to several factors such as sampling area, patients’ characteristics, environmental exposures, personal susceptibility to metals, and experimental protocols. In any case, irrespective of whether obtained results were consistent or inconsistent with those of previous literature, the present data not only supported the role of metals in cataracts but also contributed with new evidences in the field. Although studies with a high number of cases are required to support the present findings, this study contributed with valuable insights into understanding the biological mechanisms and causes of cataract by investigating both the systemic and ocular compartments.
At last, addressing the impact of trace elements, exposure on ocular health requires collaborative efforts among scientists, health professionals, and policymakers to formulate targeted interventions and promote public health initiatives.
Data Availability
Data are unavailable due to privacy or ethical restrictions.
References
Micun Z, Falkowska M, Młynarczyk M, Kochanowicz J, Socha K, Konopińska J (2022) Levels of trace elements in the lens, aqueous humour, and plasma of cataractous patients—a narrative review. Int J Environ Res Public Health 19:10376
IAPB – Italian section of the International Agency for the Prevention of Blindness. https://iapb.it/cataratta/. Accessed 21 December 2023
ANSA - Agenzia Nazionale Stampa Associata. https://www.ansa.it/canale_saluteebenessere/notizie/medicina/2019/11/20/ogni-anno-650.000-persone-operate-di-cataratta-in-italia_dffd0d6a-4e2a-4665-aa5f-fdffd5b0e367.html. Accessed 19 December 2023
Gupta VB, Rajagopala M, Ravishankar B (2014) Etiopathogenesis of cataract: an appraisal. Indian J Ophthalmol 62:103–110
Nita M, Grzybowski A (2016) The role of the reactive oxygen species and oxidative stress in the pathomechanism of the age-related ocular diseases and other pathologies of the anterior and posterior eye segments in adults. Oxid Med Cell Longev 2016:3164734
Wang W, Schaumberg DA, Park SK (2016) Cadmium and lead exposure and risk of cataract surgery in U.S. adults. Int J Hyg Environ Health 219:850–856
De Sio S, Goglia C, Cristaudo A, Pacella E, Romanelli F, Santilli V, Vitarelli A, Mandolesi D, Balladore F, Nieto H (2016) Italy and Argentina compared: an epidemiological study of occupational diseases. Ann Ig 28(1):50–57
Wills NK, Sadagopa Ramanujam VM, Chang J, Kalariya N, Lewis JR, Weng T-X, van Kuijk FJGM (2008) Cadmium accumulation in the human retina: effects of age, gender, and cellular toxicity. Exp Eye Res 86:41–51
Sharma N, Kaur Sodhi K, Kumar M, Kumar Singh D (2021) Heavy metal pollution: insights into chromium eco-toxicity and recent advancement in its remediation. Environ Nanotechnol Monit Manag 15:100388
Costa M, Murphy A (2019) Overview of chromium(III) toxicology. In: Vincent JB (ed) The nutritional biochemistry of chromium (III), 2nd edn. Elsevier, Amsterdam, The Netherlands, pp 341–359
IARC, International Agency for Research on Cancer (1990) Chromium, nickel and welding. Lyon, France, Volume 49
Jackson SE (2013) Hsp90: structure and function. Top Curr Chem 328:155–240
Donato R, Cannon BR, Sorci G, Riuzzi F, Hsu K, Weber DJ, Geczy CL (2013) Functions of S100 Proteins. Curr Mol Med 13:24–57
Kuzenko YV, Kuzenko OV, Dyomin YA (2018) Eye retinal changes under the influence of chromium ions. J Ophthal (Ukraine) 1(480):67–73
La Torre G, Pacella E, Saulle R, Giraldi G, Pacella F, Lenzi T, Mastrangelo O, Mirra F, Aloe G, Turchetti P, Brillante C, De Paolis G, Boccia A, Giustolisi R (2013) The synergistic effect of exposure to alcohol, tobacco smoke and other risk factors for age-related macular degeneration. Eur J Epidemiol 28(5):445–446
Rice KM, Walker EM Jr, Wu M, Gillette C, Blough ER (2014) Environmental mercury and its toxic effects. J Prev Med Public Health 47:74–83
Domínguez-Calva JA, Pérez-Vázquez ML, Serebryany E, King JA, Quintanar L (2018) Mercury-induced aggregation of human lens γ-crystallins reveals a potential role in cataract disease. J Biol Inorg Chem 23(7):1105–1118
ATSDR - Agency for Toxic Substances and Disease Registry (2005) Toxicological profile for nickel. Department of Health and Human Services, Public Health Service, Atlanta, USA, U.S
Nagarjuna A, Mohan D (2017) Biochemical and histopathological changes induced by nickel in the striped mullet, Mugil cephalus (Linnaeus 1758). Bull Environ Contam Toxicol 98:33–40
Aberami S, Nikhalashree S, Bharathselvi M, Biswas J, Sulochana KN, Coral K (2019) Elemental concentrations in Choroid-RPE and retina of human eyes with age-related macular degeneration. Exp Eye Res 186:107718
Jomova K, Valko M (2011) Advances in metal-induced oxidative stress and human disease. Toxicology 283:65–87
Valko M, Jomova K, Rhodes CJ, Kuča K, Musílek K (2016) Redox- and non-redox-metal-induced formation of free radicals and their role in human disease. Arch Toxicol 90:1–37
Schaumberg DA, Mendes F, Balaram M, Dana MR, Sparrow D, Hu H (2004) Accumulated lead exposure and risk of age-related cataract in men. JAMA 292:2750–2754
Neal RE, Lin C, Zigler JS Jr (2003) Pb exposure induces cataract formation in cultured rat lens and alters cytoskeletal protein profiles. IOVS Invest Ophthalmol Vis Sci 44:3491
Shen X-F, Huang P, Fox DA, Lin Y, Zhao Z-H, Wang W, Wang J-Y, Liu X-Q, Chen J-Y, Luo W-J (2016) Adult lead exposure increases blood-retinal permeability: a risk factor for retinal vascular disease. Neurotoxicology 57:145–152
Genchi G, Lauria G, Catalano A, Carocci A, Sinicropi MS (2023) Prevalence of cobalt in the environment and its role in biological processes. Biology 12:1335
Leyssens L, Vinck B, Van Der Straeten C, Wuyts F, Maes L (2017) Cobalt toxicity in humans: a review of the potential sources and systemic health effects. Toxicology 387:43–56
Paustenbach DJ, Tvermoes BE, Unice KM, Finley BL, Kerger BD (2013) A review of the health hazards posed by cobalt. Crit Rev Toxicol 43(4):316–362
Apel W, Stark D, Stark A, O’Hagan S, Ling J (2013) Cobalt–chromium toxic retinopathy case study. Doc Ophthalmol 126:69–78
Meo SA (2009) Cobalt deficiency. In: Lang F (ed) Encyclopedia of molecular mechanisms of disease. Springer, Berlin, Heidelberg, Germany, pp 380–381
Hara A, Niwa M, Aoki M, Kumada M, Kunisada T, Oyama T, Yamamoto T, Kozawa O, Mori H (2006) A new model of retinal photoreceptor cell degeneration induced by a chemical hypoxia-mimicking agent, cobalt chloride. Brain Res 1109:192–200
Bocca B, Forte G, Oggiano R, Clemente S, Asara Y, Peruzzu P, Farace C, Pala S, Fois AG, Pirina P, Madeddu R (2015) Level of neurotoxic metals in amyotrophic lateral sclerosis: a population-based case–control study. J Neurol Sci 359:11–17
Ugarte M, Osborne NN, Brown LA, Bishop PN (2013) Iron, zinc, and copper in retinal physiology and disease. Surv Ophthalmol 58:585–609
Palomino-Vizcaino G, Schuth N, Domínguez-Calva JA, Rodríguez-Meza O, Martínez-Jurado E, Serebryany E, King JA, Kroll T, Costas M, Quintanar L (2023) Copper reductase activity and free radical chemistry by cataract associated human lens γ-crystallins. J Am Chem Soc 145:6781–6797
Goralska M, Ferrell J, Harned J, Lall M, Nagar S, Fleisher LN, McGahan MC (2009) Iron metabolism in the eye, a review. Exp Eye Res 88(2):204–215
Trovato Battagliola E, Pacella F, Malvasi M, Scalinci SZ, Turchetti P, Pacella E, La Torre G, Arrico L (2022) Risk factors in central retinal vein occlusion: a multi-center case-control study conducted on the Italian population: demographic, environmental, systemic, and ocular factors that increase the risk for major thrombotic events in the retinal venous system. Eur J Ophthalmol 32(5):2801–2809
Smith MR, Fernandes J, Go Y-M, Jones DP (2017) Redox dynamics of manganese as a mitochondrial life-death switch. Biochem Biophys Res Commun 482:388–398
Endo K, Itoh N, Maehara S, Shinozaki A, Imagawa T, Uehara M (2008) Functional disorder of the retina in manganese-deficient Japanese quail revealed by electroretinography using a contact lens electrode with built-in light source. J Vet Med Sci 70:139–144
Gong H, Amemiya T (1996) Ultrastructure of retina of manganese-deficient rats. Invest Ophthalmol Vis Sci 37:1967–1974
Hou X, Hou Y (1996) Determination of 19 elements in human eye lenses. Biol Trace Elem Res 55(1–2):89–98
Karaküçük S, Mirza GE, Ekinciler F, Saraymen R, Karaküçük I, Üstdal M (2009) Selenium concentrations in serum, lens and aqueous humour of patients with senile cataract. Acta Ophthalmol Scand 73:329–332
Flohé L (2005) Selenium, selenoproteins and vision. Dev Ophthalmol 38:89–102
Post M, Lubiński W, Lubiński J, Krzystolik K, Baszuk P, Muszyńska M, Marciniak W (2018) Serum selenium levels are associated with age-related cataract. Ann Agric Environ Med 25:443–448
Hyun HJ, Sohn JH, Ha DW, Ahn YH, Koh J-Y, Yoon YH (2001) Depletion of intracellular zinc and copper with TPEN results in apoptosis of cultured human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci 42:460–465
Srivastava VK, Varshney N, Pandey DC (2009) Role of trace elements in senile cataract. Acta Ophthalmol 70:839–841
Chylack LT Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, Friend J, McCarthy D, Wu S-Y (1993) The lens opacities classification system III. Arch Ophthalmol 111(6):831–836
Flieger J, Dolar-Szczasny J, Rejdak R, Majerek D, Tatarczak Michalewska M, Proch J, Blicharska E, Flieger W, Baj J, Niedzielski P (2021) The multi-elemental composition of the aqueous humor of patients undergoing cataract surgery, suffering from coexisting diabetes, hypertension, or diabetic retinopathy. Int J Mol Sci 22:9413
Kiel JW, Hollingsworth M, Rao R, Chen M, Reitsamer HA (2011) Ciliary blood flow and aqueous humor production. Prog Retin Eye Res 30(1):1–17
Stamper RL, Lieberman MF, Drake MV (2009) Aqueous humor formation. In: Stamper RL, Lieberman MF, Drake MV (eds) Becker-Shaffer’s diagnosis and therapy of the glaucomas, 8th edn. Mosby, St. Louis, Missouri (USA), pp 8–24
Asmatullah SN, Shakoori AR (1998) Embryotoxic and teratogenic effects of hexavalent chromium in developing chicks of Gallus domesticus. Bull Environ Contam Toxicol 61:281–288
Hassan NA, Shehab AA (2004) Hexavalent chromium (VI) induced toxicity on rat corneal structure: a light scanning electron microscopy study. Mansoura J Forensic Med Clin Toxicol 12:1–22
Amany M, Sawsan K, Abdel-Wahhab M (2006) Chromium-picolinate induced ocular changes: protective role of ascorbic acid. Toxicology 226:143–151
Wu W, Jiang H, Guo X, Wang Y, Ying S, Feng L, Li T, Xia H, Zhang Y, Chen R, Chen T, Lou J (2017) The protective role of hyaluronic acid in Cr(VI)-induced oxidative damage in corneal epithelial cells. J Ophthalmol 2017:3678586
Schmeling M, Gaynes BI, Tidow-Kebritchi S (2014) Heavy metal analysis in lens and aqueous humor of cataract patients by total reflection X-ray fluorescence spectrometry. Powder Diffr 29:155–158
Dolar-Szczasny J, Święch A, Flieger J, Tatarczak-Michalewska M, Niedzielski P, Proch J, Majerek D, Kawka J, Mackiewicz J (2019) Levels of trace elements in the aqueous humor of cataract patients measured by the inductively coupled plasma optical emission spectrometry. Molecules 24:4127
Cumurcu T, Mendil D, Erkorkmaz U (2008) Aqueous humor and serum levels of chromium in cataract patients with and without diabetes mellitus. Ophthalmologica 222(5):324–328
Iomdina E, Arutyunyan L, Khorosheva E (2019) Analyzing trace elements in the structures of glaucomatous eyes. Int J Biomed 9(1):23–25
Haddad HH (2012) The effect of heavy metals cadmium, chromium and iron accumulation in human eyes. Am J Anal Chem 3:710–713
Ceylan OM, Demirdöğen BC, Mumcuoğlu T, Aykut O (2013) Evaluation of essential and toxic trace elements in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Biol Trace Elem Res 153:28–34
IARC, International Agency for Research on Cancer (2006) Inorganic and organic lead compounds. IARC, Lyon, France, volume 87
Sani AH, Amanabo M (2021) Lead: a concise review of its toxicity, mechanism and health effect. GSC Biol Pharm Sci 15:055–062
Barbosa F Jr, Tanus-Santos JE, Gerlach RF, Parsone PJ (2005) A critical review of biomarkers used for monitoring human exposure to lead: advantages, limitations, and future needs. Environ Health Perspect 113:1669–1674
Erie JC, Butz JA, Good JA, Erie EA, Burritt MF, Cameron JD (2005) Heavy metal concentrations in human eyes. Am J Ophthalmol 139:888–893
Cekic O (1998) Copper, lead, cadmium and calcium in cataractous lenses. Ophthalmic Res 30(1):49–53
Shukla N, Moitra JK, Trivedi RC (1996) Determination of lead, zinc, potassium, calcium, copper and sodium in human cataract lenses. Sci Total Environ 181(2):161–165
Bocca B, Forte G, Pisano P, Farace C, Giancipoli E, Pinna A, Dore S, Madeddu R (2020) A pilot study to evaluate the levels of aqueous humor trace elements in open-angle glaucoma. J Trace Elem Med Biol 61:1265
Erie JC, Good JA, Butz JA (2009) Excess lead in the neural retina in age-related macular degeneration. Am J Ophthalmol 148(6):890–894
Biesemeier A, Yoeruek E, Eibl O, Schraermeyer U (2015) Iron accumulation in Bruch’s membrane and melanosomes of donor eyes with age-related macular degeneration. Exp Eye Res 137:39–49
Czarnek K, Terpiłowska S, Siwicki AK (2015) Selected aspects of the action of cobalt ions in the human body. Cent Eur J Immunol 40(2):236–242
Chan W, Almasieh M, Catrinescu MM, Levin LA (2018) Cobalamin-associated superoxide scavenging in neuronal cells is a potential mechanism for vitamin B(12)-deprivation optic neuropathy. Am J Pathol 188:160–172
Stein JD, Khawaja AP, Weizer JS (2021) Glaucoma in adults-screening, diagnosis, and management: a review. JAMA 325:164–174
Kim KE, Kim MJ, Park KH, Jeoung JW, Kim SH, Kim CY, Kang SW (2016) Prevalence, awareness, and risk factors of primary open-angle glaucoma: Korea National Health and nutrition examination survey 2008–2011. Ophthalmology 123:532–541
Rochtchina E, Wang JJ, Flood VM, Mitchell P (2007) Elevated serum homocysteine, low serum vitamin B12, folate, and age-related macular degeneration: the blue mountains eye study. Am J Ophthalmol 143(2):344–346
Ren X, Chou Y, Jiang X, Hao R, Wang Y, Chen Y, Li X (2020) Effects of oral vitamin B1 and mecobalamin on dry eye disease. J Ophthalmol 2020:9539674
Ozen S, Ozer MA, Akdemir MO (2017) Vitamin B12 deficiency evaluation and treatment in severe dry eye disease with neuropathic ocular pain. Graefes Arch Clin Exp Ophthalmol 255(6):1173–1177
Kuzniarz M, Mitchell P, Cumming RG, Flood VM (2001) Use of vitamin supplements and cataract: the blue mountains eye study. Am J Ophthalmol 132(1):19–26
Fick A, Jünemann A, Michalke B, Lucio M, Hohberger B (2019) Levels of serum trace elements in patients with primary open-angle glaucoma. J Trace Elem Med Biol 53:129–134
Jünemann AGM, Stopa P, Michalke B, Chaudhri A, Reulbach U, Huchzermeyer C, Schlötzer-Schrehardt U, Kruse FE, Zrenner E, Rejdak R (2013) Levels of aqueous humor trace elements in patients with non-exsudative age-related macular degeneration: a case-control study. PLoS ONE 8(2):e56734
Hohberger B, Chaudhri MA, Michalke B, Lucio M, Nowomiejska K, Schlötzer Schrehardt U, Grieb P, Rejdak R, Jünemann AGM (2018) Levels of aqueous humor trace elements in patients with open-angle glaucoma. J Trace Elem Med Biol 45:150–155
Dake OY, Amemiya T (1991) Electron microscopic study of the optic nerve in copper deficient rats. Exp Eye Res 52:277–281
Bharathselvi M, Biswas S, Raman R, Selvi R, Coral K, Narayanansamy A, Ramakrishnan S, Sulochana KN (2016) Homocysteine & its metabolite homocysteine-thiolactone & deficiency of copper in patients with age related macular degeneration - a pilot study. Ind J Med Res 143:756–762
Clemons TE, Kurinij N, Sperduto RD (2004) Associations of mortality with ocular disorders and an intervention of high-dose antioxidants and zinc in the age-related eye disease study: AREDS Report No. 13. Arch Ophthalmol 122:716–726
Erie JC, Good JA, Butz JA, Pulido JS (2009) Reduced zinc and copper in the retinal pigment epithelium and choroid in age-related macular degeneration. Am J Ophthalmol 147:276–282
Rai PSK, Deokar S, Yadav RR, Shelke S, Sundharan S (2017) Serum zinc and copper levels: a marker of disease activity in senile cataract patients. Int J Res Med Sci 5(8):3697–3700
Manoj B, Jayaram S (2014) Serum levels of antioxidant trace elements zinc and copper in senile mature cataract. Int J Cur Res Rev 06:131–137
Kaźmierczak K, Malukiewicz G, Lesiewska-Junk H, Laudencka A, Szady-Grad M, Klawe J, Nowick K (2014) Blood plasma levels of microelements in patients with history of optic neuritis. Curr Eye Res 39(1):93–98
Yildirim Z, Uçgun NI, Kiliç N, Gürsel E, Sepici-Dinçel A (2007) Pseudoexfoliation syndrome and trace elements. Ann NY Acad Sci 1100:207–212
Panteli VS, Kanellopoulou DG, Gartaganis SP, Koutsoukos PG (2009) Application of anodic stripping voltammetry for zinc, copper, and cadmium quantification in the aqueous humor: implications of pseudoexfoliation syndrome. Biol Trace Elem Res 132:9–18
Cumurcu T, Mendil D, Etikan I (2006) Levels of zinc, iron, and copper in patients with pseudoexfoliative cataract. Eur J Ophthalmol 16:548–553
Author information
Authors and Affiliations
Contributions
G.F. and B.B.: formal analysis, data curation, and writing of the original version.
E.P. and E.T.B.: conceptualization, sampling, and methodology.
M.M.: methodology and data curation.
N.R. and P.D.: sampling and data curation.
A.M.: review editing.
All authors have approved the manuscript and agreed with the order of authors.
Corresponding author
Ethics declarations
Ethics Approval
The study was conducted according to the declaration of Helsinki. The study protocol was approved by the Institutional Ethical Committee of the University of Rome (protocol number 1005/2021, approval date November 10, 2021).
Consent to Participate
The written informed consent was obtained from all individual participants included in the study.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Forte, G., Battagliola, E.T., Malvasi, M. et al. Trace Element Concentration in the Blood and Aqueous Humor of Subjects with Eye Cataract. Biol Trace Elem Res (2024). https://doi.org/10.1007/s12011-024-04207-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12011-024-04207-3