Abstract
Chronic obstructive pulmonary disease (COPD) is associated with numerous comorbidities, among which osteoporosis is of high significance. Low bone mass and the occurrence of fragility fractures is a common finding in patients with COPD. Typical risk factors related directly or indirectly to these skeletal complications include systemic inflammation, tobacco smoking, vitamin D deficiency, and treatment with oral or inhaled corticosteroids. In particular, treatment with glucocorticoids appears to be a strong contributor to bone changes in COPD, but does not fully account for all skeletal complications. Additional to the effects of COPD on bone mass, there is evidence for COPD-related changes in bone microstructure and material properties. This review summarizes the clinical outcomes of low bone mass and increased fracture risk, and reports on recent observations in bone tissue and material in COPD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Clinical Findings in Patients with COPD
COPD is characterized by chronic airflow limitation and pathologic changes in the lung and is predominantly caused by smoking. In accordance with the Global Initiative for Chronic Obstructive Lung Disease (GOLD), the disease is stratified from mild to very severe forms according to the degree of airflow limitation assessed by spirometry [1]. Low bone mass and the occurrence of fragility fractures is a common finding in patients with COPD [2–5]. The prevalence of osteopenia and osteoporosis is high, and typically with increasing severity of COPD, the percentage of osteoporotic patients is increasing. In her review article, Biskobing described that 35 to 72 % of patients with COPD had been reported to be osteopenic, and 36 to 60 % osteoporotic [6]. A recent study showed that low volumetric BMD was present in 58 % of all subjects with COPD, was even more frequent in those with worse COPD, and had a prevalence of 84 % among subjects with very severe COPD [7•]. Risk of fragility fractures is high in COPD. Nuti et al. [8] reported that about 40 % of men and women with COPD had sustained at least one vertebral fracture. They reported also that a greater COPD severity was associated with a higher prevalence of fracture. Similar, in a more recent report, vertebral fractures occurred in 37 % of all subjects and were associated with lower volumetric BMD at each GOLD stage of severity [7•]. In addition, sarcopenia has been associated with severity of COPD which might be a cause of increased number of falls and fractures [9].
Bone mechanical properties based on micro finite element analysis have been assessed in patients with COPD. Romme et al. [10••] reported on bone stiffness and failure load in male patients with COPD compared to male individuals without COPD. For this purpose, they assessed bone structure of the distal radius and tibia by high-resolution peripheral quantitative computed tomography. After stratification for areal BMD at the femoral neck, they did not observe any significant differences between subjects with and without COPD. Osteoporotic COPD patients were similar in all study parameters compared to osteoporotic patients without COPD and non-osteoporotic COPD patients did not differ from non-osteoporotic patients without COPD. However, the authors found that gas transfer capacity of the lung significantly positively correlated with estimated failure load of the distal tibia in their cohort. As this relationship was observed after normalization with respect to femoral neck areal BMD, it suggests that gas transfer capacity of the lung might impact the structural and mechanical parameters of the bone [10••].
Patients with COPD often are treated with glucocorticoids (GC) in an attempt to improve respiratory function by reducing inflammation and airway hyper-responsiveness. However, the use of GC may in turn heighten bone fragility in patients with COPD. The favored effects and side effects of systemic treatment with GC in COPD have been reviewed recently [11]. It is well-known that systemic treatment with GC has deleterious effects on the bone including direct effects on the bone cells (enhancing osteoclastic resorption and impairing maturation of osteoblasts), as well as effects on calcium absorption and excretion [12–16]. The quantification of the increased fracture risk during oral GC therapy showed that the relative rates of vertebral and hip fractures were particularly increased [17]. Fracture risk was reported to be dependent on GC dose [17, 18].
Treatment with inhaled GC is well-established in asthma, but controversially discussed in COPD treatment [19]. Price et al. have reported that data on an effect of inhaled GC on mortality or lung function are sparce and indiscriminate use of inhaled GC in COPD may expose patients to an unnecessary increase in the risk of side effects in particular when high doses of inhaled GC are used [19]. In contrast to oral GC therapy, inhaled GC are claimed to predominantly act locally in the airways thus minimizing side effects, including increased bone fracture risk. However, there are reports on side effects in particular in patients who received high doses (recently reviewed by Chee and colleagues [20]). Inhaled GC are often prescribed in combination with bronchodilators (such as long-acting beta2-agonists). The combination therapy has proven beneficial compared to placebo for forced expiratory volume in one second, exacerbation rate, symptoms, and health status in COPD patients [21]; however, the isolated and combined effects of inhaled GC and brochodilators on bone is controversial. In a Danish COPD population, inhaled long-acting beta2-agonists, inhaled agonists plus inhaled GC, and inhaled GC were not associated with fracture risk [22]. In contrast, a meta-analysis (including studies with at least 24 weeks duration of treatment and participants of any COPD severity) revealed that inhaled GC use is associated with a modest, but statistically significant increase in the risk of fractures in patients with COPD (Odds ratio = 1.27; 95 % confidence interval, 1.01 to 1.58 in the 16 randomized controlled trials) [23••].
While a contribution of GC to low bone mass and/or bone fragility appears to be well-established, GC therapy does not appear to fully account for bone fragility in COPD. This indicates that the underlying disease per se has a significant impact on bone properties. Direct effects of COPD on the bone are suggested to be caused by mediators, cytokines, or activated inflammatory cells which enter the systemic circulation from the inflammation in the lung [24]. Other causes might include reduced physical activity of patients and their limited exposure to sunlight. The latter and/or a genetic link of COPD to vitamin D levels might be causes of vitamin D deficiency in patients with COPD [25, 26]. There is a high prevalence of hypovitaminosis D in COPD patients [27, 28••]. Noteworthy, plasma 25(OH)D concentration was positively associated with bone density and exercise capacity in moderate to very severe COPD [29]. As aforementioned, COPD is predominantly caused by smoking and the majority of patients have a long history of tobacco smoking. In a large cohort of more than one thousand males from a Dutch and Belgium Lung Cancer Screening Trial, vertebral fracture prevalence was higher in current than in former smokers; however, fracture prevalence was similar in patients with COPD compared to those without [30]. Nicotine at high doses was reported to exert negative effects on bone cells and fracture repair in vitro and in vivo (reviewed in [31]), thus this might also be an important contributor to the observed skeletal alterations in patients with COPD. Further, a genetic link to COPD was identified by a significant association between polymorphism in the transient receptor potential cation channel TRPV4 gene and the prevalence of COPD [32, 33].
As many influencing factors and comorbidities exist in COPD, a general estimation of the contribution of the disease to skeletal complications is challenging. Attempts were made to find relationships between parameters describing the functional status of the lung with BMD. For instance, it was shown that the percentage of low attenuation area of the lung (indicative of the extent of pulmonary emphysema) was correlated with low BMD [34].
Independent of the multifactorial origin of the skeletal problems in COPD, the data suggest a need of adequate anti-osteoporotic therapy in COPD. As up to now no fracture prevention guidelines are available specifically for patients with COPD, a clinical approach for improving identification and treatment of patients at high risk of fracture has been published recently [35].
Bone Biopsy Findings in COPD
Beyond bone mineral density (BMD), information on “bone quality” is important to get more insights into the underlying mechanisms of increased bone fragility and to identify patients at high fracture risk [36, 37]. At the tissue level, bone quality includes parameters such as bone volume and architectural indices. At the material level, bone quality includes characteristics such as the local degree of bone matrix mineralization, bone composition, and mechanical properties. These bone quality parameters are strongly influenced by bone formation and resorption. Thus, various parameters of bone at different hierarchical length scale might contribute to the reduced ability to resist fracture in a specific disease [38]. For COPD, the information on such tissue and material characteristics is relatively sparce so far.
Commonly, material properties are measured in transiliac bone biopsy samples. Kulak and colleagues [28••] studied samples from twenty patients for bone histomorphometry. The study cohort comprised postmenopausal women having mild to severe COPD (according to the GOLD classification), with the majority of patients having a long history of smoking (i.e., more than 20 pack-years). The patients were either untreated or treated with inhaled GC. Histomorphometric alterations in both compartments, cancellous and cortical bone were observed. The most significant findings were structural alterations, including lower trabecular bone volume, decreased thickness, and higher separation of trabeculae with a decreased connectivity compared to sex- and age-matched controls. Moreover, cortical width was reduced and the porosity was nearly twofold in the patients with COPD. Bone formation rate was not different from normal in average; however, it was lower in those with more severe COPD.
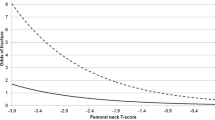
Recently, we were able to characterize the identical biopsy samples used for the aforementioned histomorphometric analyses by quantitative backscatter electron imaging for bone mineralization density distribution (BMDD) [39]. BMDD is a measure of the degree and heterogeneity of bone matrix mineralization and is generally closely related to the bone turnover rate (which determines the average tissue age) and mineralization kinetics (the time course of mineral accumulation in the newly formed bone matrix) of the individual. Considering the entire study cohort, we found no significant differences in BMDD when compared to reference BMDD data. However, the subset of most severely affected patients with COPD (GOLD III and GOLD IV) revealed a more homogenously mineralized bone matrix than in patients with moderate COPD in accordance with their lower bone turnover rates (Fig. 1). We also observed that the patients with the lowest bone volume had also the lowest degree of bone matrix mineralization. This suggests that in some patients with COPD, additional to reduced bone volume, lower bone material density contributes to the decreased BMD (by DXA).
Quantitative backscatter electron imaging analysis of transiliac bone biopsy samples from patients with COPD. On the left side, details of backscatter electron images of typically thin trabeculae from biopsies from a patient with moderate COPD (top) and a patient with severe COPD (bottom) are shown. On the right side, the corresponding cancellous BMDD for both patients is presented (dashed line indicates moderate COPD, solid line severe COPD). Please note the narrower peak in severe COPD indicative for less heterogeneity of mineralization densities. The white dashed line and the grey area in the background indicate mean ± 1 standard deviation of cancellous reference BMDD for adult individuals (reference data from [39])
A clinically important finding from both the histomorphometry and backscatter electron imaging analyses [28••, 40••] was that there were no significant alterations in any studied parameter between patients with inhaled GC treatment versus those without treatment. In particular, there was no difference in the degree of bone matrix mineralization between treated and untreated. Noteworthy in this context, systemic treatment with GC was shown to decrease the degree of bone mineralization in a rat model [41]. Although general conclusions are limited in view of the small sample size of our biopsy cohort, this finding nevertheless suggests that if inhaled GC treatment exerts effects on bone tissue and material properties, these appear to be small.
Moreover, both COPD biopsy studies [28••, 40••] together indicated that the ability of the osteoblast to form a matrix might be decreased resulting in a lower amount of formed bone, but that the mineral accumulation in the newly formed matrix follows a normal pace. Thus, impairments of the mechanical competence of COPD bone are unlikely directly related to the degree and heterogeneity of the bone matrix mineralization. Preliminary data on organic matrix properties point towards differences in COPD patients compared to healthy age- and sex-matched controls [42].
Conclusion
Osteoporosis and the occurrence of fragility fracture is a major concern in patients with COPD independent of treatment with GC. In accordance with low BMD, reduced bone volume has been observed in transiliac biopsy samples from patients with COPD. Although bone matrix mineralization was normal on average, the bone mineralization findings suggest that in some patients with lower bone volume, additionally, lower bone matrix mineralization might contribute to the decrease in BMD. The effects of COPD on other bone material characteristics are still unknown. Given the increasing number of COPD patients, there is a need for further studies at the bone material level, such as mechanical properties and organic matrix characteristics. Such studies might help to identify patients at high fracture risk and might provide further information on the pathophysiologic mechanisms in bone in COPD.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global initiative for chronic obstructive lung disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532–55.
Graat-Verboom L, Smeenk FW, van den Borne BE, Spruit MA, Donkers-van Rossum AB, Aarts RP, et al. Risk factors for osteoporosis in Caucasian patients with moderate chronic obstructive pulmonary disease: a case control study. Bone. 2012;50(6):1234–9.
Cielen N, Maes K, Gayan-Ramirez G 2014 Musculoskeletal disorders in chronic obstructive pulmonary disease. BioMed Research International Volume 2014, Article ID 965764, 17 pages http://dx.doi.org/10.1155/2014/965764
Jørgensen NR, Schwarz P. Osteoporosis in chronic obstructive pulmonary disease patients. Curr Opin Pulm Med. 2008;14(2):122–7.
Romme EA, Smeenk FW, Rutten EP, Wouters EF. Osteoporosis in chronic obstructive pulmonary disease. Expert Rev Respir Med. 2013;7(4):397–410. doi:10.1586/17476348.2013.814402.
Biskobing DM. COPD and osteoporosis. Chest. 2002;121(2):609–20.
Jaramillo JD, Wilson C, Stinson DS, Lynch DA, Bowler RP, Lutz S, et al. COPDGene Investigators. Reduced Bone Density and Vertebral Fractures in Smokers. Men and COPD Patients at Increased Risk. Ann Am Thorac Soc. 2015;12(5):648–56. In this large study comprising more than 3300 male smokers, the impact of smoking on low bone mass and vertebral fracture risk was demonstrated. COPD and especially emphysema were found associated with risk of osteoporosis after adjustment for steroid use and other variables.
Nuti R, Siviero P, Maggi S, Guglielmi G, Caffarelli C, Crepaldi G, et al. Vertebral fractures in patients with chronic obstructive pulmonary disease: the EOLO Study. Osteoporos Int. 2009;20(6):989–98.
Costa TM, Costa FM, Moreira CA, Rabelo LM, Boguszewski CL, Borba VZ. Sarcopenia in COPD: relationship with COPD severity and prognosis. J Bras Pneumol. 2015;41(5):415–21.
Romme EA, Rutten EP, Geusens P, de Jong JJ, van Rietbergen B, Smeenk FW, et al. Bone stiffness and failure load are related with clinical parameters in men with chronic obstructive pulmonary disease. J Bone Miner Res. 2013;28(10):2186–93. doi:10.1002/jbmr.1947. In this work, information on estimates of mechanical data from COPD bone have been assessed for the first time by finite element analysis.
Pandya D, Puttanna A, Balagopal V. Systemic effects of inhaled corticosteroids: an overview. Open Respir Med J. 2014;8(Suppl 1: M2):59–65.
Hofbauer LC, Gori F, Riggs BL, Lacey DL, Dunstan CR, Spelsberg TC, et al. Stimulation of osteoprotegerin ligand and inhibition of osteoprotegerin production by glucocorticoids in human osteoblastic lineage cells: potential paracrine mechanisms of glucocorticoid-induced osteoporosis. Endocrinology. 1999;140(10):4382–9.
Cooper MS. Sensitivity of bone to glucocorticoids. Clin Sci. 2004;107:111–23.
Kim HJ, Zhao H, Kitaura H, Bhattacharyya S, Brewer JA, Muglia LJ, et al. Glucocorticoids suppress bone formation via the osteoclast. J Clin Invest. 2006;8:2152–60.
Weng MY, Lane NE. Medication-induced osteoporosis. Curr Osteoporos Rep. 2007;4:139–45.
Unnanuntana A, Rebolledo BJ, Khair MM, DiCarlo EF, Lane JM. Diseases affecting bone quality: beyond osteoporosis. Clin Orthop Relat Res. 2011;469(8):2194–206.
van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C. Use of oral corticosteroids and risk of fractures. J Bone Miner Res. 2000;15(6):993–1000.
van Staa TP, Leufkens HG, Cooper C. The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int. 2002;13(10):777–87.
Price D, Yawn B, Brusselle G, Rossi A. Risk-to-benefit ratio of inhaled corticosteroids in patients with COPD. Prim Care Respir J. 2013;22(1):92–100.
Chee C, Sellahewa L, Pappachan JM. Inhaled corticosteroids and bone health. Open Respir Med J. 2014;8:85–92.
Bonay M, Bancal C, Crestani B. The risk/benefit of inhaled corticosteroids in chronic obstructive pulmonary disease. Expert Opin Drug Saf. 2005;4(2):251–71.
Vestergaard P, Rejnmark L, Mosekilde L. Fracture risk in patients with chronic lung diseases treated with bronchodilator drugs and inhaled and oral corticosteroids. CHEST. 2007;132:1599–607.
Loke YK, Cavallazzi R, Singh S. Risk of fractures with inhaled corticosteroids in COPD: systematic review and meta-analysis of randomised controlled trials and observational studies. Thorax. 2011;66(8):699–708. This meta-analysis of randomized clinical trials and observational studies suggested a dose-dependent increased risk of fractures associated with the long-term use of inhaled glucocorticoids in patients with COPD.
Lacativa PG. Farias ML osteoporosis and inflammation. Arq Bras Endocrinol Metabol. 2010;54(2):123–32. Review.
Gilbert CR, Arum SM, Smith CM. Vitamin D deficiency and chronic lung disease. Can Respir J. 2009;16(3):75–80.
Persson LJ, Aanerud M, Hiemstra PS, Hardie JA, Bakke PS, Eagan TM. Chronic obstructive pulmonary disease is associated with low levels of vitamin D. PLoS ONE. 2012;7(6), e38934. doi:10.1371/journal.pone.0038934.
Franco CB, Paz-Filho G, Gomes PE, Nascimento VB, Kulak CA, Boguszewski CL, et al. Chronic obstructive pulmonary disease is associated with osteoporosis and low levels of vitamin D. Osteoporos Int. 2009;20(11):1881–7.
Kulak CA, Borba VC, Jorgetti V, Dos Reis LM, Liu XS, Kimmel DB, et al. Skeletal microstructural abnormalities in postmenopausal women with chronic obstructive pulmonary disease. J Bone Miner Res. 2010;25(9):1931–40. doi:10.1002/jbmr.88. This was the only study on bone biopsy samples from COPD patients so far. Microstructural abnormalities and altered bone formation indices were described.
Romme EAPM, Rutten EPA, Smeenk FWJM, Spruit MA, Menheere PPCA, Wouters EFM. Vitamin D status is associated with bone mineral density and functional exercise capacity in patients with chronic obstructive pulmonary disease. Ann Med. 2013;45(1):91–6.
de Jong WU, de Jong PA, Vliegenthart R, Isgum I, Lammers JW, Oudkerk M, et al. Association of chronic obstructive pulmonary disease and smoking status with bone density and vertebral fractures in male lung cancer screening participants. J Bone Miner Res. 2014;29(10):2224–9.
Kallala R, Barrow J, Graham SM, Kanakaris N, Giannoudis PV. The in vitro and in vivo effects of nicotine on bone, bone cells and fracture repair. Expert Opin Drug Saf. 2013;12(2):209–33.
Zhu G, ICGN Investigators, Gulsvik A, Bakke P, Ghatta S, Anderson W, et al. Association of TRPV4 gene polymorphisms with chronic obstructive pulmonary disease. Hum Mol Genet. 2009;18(11):2053–62.
McAlexander MA, Luttmann MA, Hunsberger GE, Undem BJ. Transient receptor potential vanilloid 4 activation constricts the human bronchus via the release of cysteinyl leukotrienes. J Pharmacol Exp Ther. 2014;349(1):118–25.
Ohara T, Hirai T, Muro S, et al. Relationship between pulmonary emphysema and osteoporosis assessed by CT in patients with COPD. Chest. 2008;134(6):1244–9.
Romme EA, Geusens P, Lems WF, Rutten EP, Smeenk FW, van den Bergh JP, et al. Fracture prevention in COPD patients; a clinical 5-step approach. Respir Res. 2015;16:32. doi:10.1186/s12931-015-0192-8.
Fratzl P, Gupta HS, Paschalis EP, Roschger P. Structure and mechanical quality of the collagen-mineral nano-composite in bone. J Mater Chem. 2004;14:2115–23.
Seeman E. Bone quality: the material and structural basis of bone strength. J Bone Miner Metab. 2008;26(1):1–8.
Wagermaier W, Klaushofer K, Fratzl P. Fragility of bone material controlled by internal interfaces. Calcif Tissue Int. 2015;97(3):201–12.
Roschger P, Paschalis EP, Fratzl P, Klaushofer K. Bone mineralization density distribution in health and disease. Bone. 2008;42:456–66.
Misof BM, Roschger P, Jorgetti V, Klaushofer K, Borba VZ, Boguszewski CL, et al. Subtle changes in bone mineralization density distribution in most severely affected patients with chronic obstructive pulmonary disease. Bone. 2015;79:1–7. doi:10.1016/j.bone.2015.05.018. This study provided the only information on bone matrix mineralization in patients with COPD so far. Altered heterogeneity of mineralization was reported for the most severely affected patients.
Yao W, Cheng Z, Pham A, Busse C, Zimmermann EA, Ritchie RO. Glucocorticoid-induced bone loss can be reversed by the actions of PTH and Risedronate on different pathways for bone formation and mineralization. Arthritis Rheu. 2008;58(11):3485–97.
Paschalis E, Gamsjaeger S, Dempster D, Jorgetti V, Borba V, Klaushofer K, Moreira C. Bone Material Compositional Properties at Actively Bone Forming Trabecular Surfaces are Able to Discriminate Between Chronic Obstructive Pulmonary Disease (COPD) Patients that Sustain Fragility Fractures vs. Those Who Do Not, Irrespective of Glucocorticoid Therapy. Abstract ASBMR-meeting 2015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Barbara M. Misof, Carolina A. Moreira, Klaus Klaushofer, and Paul Roschger declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Secondary Causes of Osteoporosis
Rights and permissions
About this article
Cite this article
Misof, B.M., Moreira, C.A., Klaushofer, K. et al. Skeletal Implications of Chronic Obstructive Pulmonary Disease. Curr Osteoporos Rep 14, 49–53 (2016). https://doi.org/10.1007/s11914-016-0301-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-016-0301-8