Abstract
Purpose of Review
Review epidemiology, pathophysiology, and management of hypertension in the pediatric dialysis population.
Recent Findings
Interdialytic blood pressure measurement, especially with ambulatory blood pressure monitoring, is the gold standard to assess for hypertension. Tools to assess dry weight aid in achievement of euvolemia, the primary therapy for management of hypertension. Persistent hypertension should be treated with antihypertensive medications and potentially with native nephrectomies.
Summary
Cardiovascular disease continues to be the primary cause of morbidity and mortality in the dialysis population with hypertension as an important modifiable factor. Achievement on dry weight and limiting both aggressiveness of interdialytic weight gain and ultrafiltration rate underlie the best approach. Tools to assess volume status beyond clinical assessment have shown promise in achieving euvolemia. When hypertension persists despite achievement of euvolemia, antihypertensive medications may be required and in some cases native nephrectomies. Future studies in children are needed to determine the best antihypertensive class and ideal rate of ultrafiltration on hemodialysis towards achievement of normotension and reduction of cardiovascular risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the USA, there were 9672 children ≤ 21 years of age who received treatment for end-stage renal disease (ESRD), with an additional 10,251 adult survivors of childhood onset ESRD at the end of 2015 [1]. Internationally, the prevalence of ESRD in children 19 and younger ranges between 18 and 100 per million of age-related healthy population [2]. Cardiovascular disease is the major cause of morbidity and primary cause of mortality in the ESRD population for both adults and children [1, 3]. The United States Renal Data System [1] registry data demonstrated a mortality rate of 27 per 1000 patient years between 2010 and 2014. The primary cause of death was cardiac arrest with mortality due to cardiovascular disease accounting for close to 30% of the deaths [1]. Internationally, mortality is ~ 30 times higher among adults with childhood onset of dialysis as compared to the general population, with cardiovascular disease accounting for 20–40% of the mortality [4•, 5, 6]. Cardiovascular death rate is 1000 times higher among children and 100 times higher in young adults with ESRD as compared to the general population [6]. The cause of cardiovascular disease in ESRD is not completely understood and is likely multifactorial, including chronic inflammation, atherosclerosis, malnutrition, hyperphosphatemia, and hypertension.
Hypertension is an important modifiable risk factor for cardiovascular disease among ESRD patients. Among adults, the prevalence of hypertension, as defined as systolic blood pressure (BP) > 150 mmHg and diastolic BP > 85 mmHg, remains as high as 86% [7]. The North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS) registry data of 2264 peritoneal dialysis (PD) and 1183 hemodialysis (HD) patients aged ≤ 21 years demonstrated hypertension (defined as blood pressure > 90% for age, gender, and height) in 41% of PD and 51% HD patients [8•]. Hypertension was more common among patients with glomerular cause of ESRD, < 6 years of age, and Black race [8•]. Internationally, among 851 PD and 464 HD pediatric patients from 15 countries, uncontrolled hypertension (defined as > 95% for age, gender, and height) was seen in 56.4% in PD and 63.8% in HD patients. Younger age, shorter dialysis vintage, and glomerular cause of ESRD were contributing factors to hypertension [9•]. Pediatric studies have also demonstrated associations of hypertension with intermediate markers of cardiac morbidity such as left ventricular hypertrophy [10,11,12], increased carotid artery intimal-medial thickness [13], and coronary artery calcifications [14].
Volume excess from sodium and water retention is considered the primary etiology of hypertension in the dialysis population. Other factors include inappropriate activation of the renin-aldosterone-angiotensin system (RAAS), overactivity of the sympathetic nervous system (SNS), endothelial cell dysfunction, arterial stiffness, and iatrogenic from medications. Here we review the pathophysiology and management of hypertension in the dialysis population.
Blood Pressure Measurement
Ambulatory blood pressure monitoring (ABPM) is the gold standard towards assessment of hypertension, nocturnal hypertension, masked hypertension, and white coat hypertension, as it is for the healthy population. Particularly in HD, pre- and post-HD blood pressures provide an inaccurate estimate of interdialytic blood pressure burden as assessed by 44-h ABPM [15•]. Blood pressures surrounding the HD procedure do not correlate with end organ damage such as elevated left ventricular mass index [16,17,18]. Forty-four-hour ABPM has demonstrated increased accuracy in detecting hypertension as compared to a 24-h assessment. Blood pressure loads > 25% on 44-h ABPM was associated with higher left ventricular mass index in children on chronic hemodialysis as compared to assessment with 24-h ABPM [19]. Home blood pressures correlate more closely with ABPM, end organ damage, and cardiovascular mortality when compared to peri-dialytic measurements [16, 20, 21•]. Among 47 children on peritoneal dialysis, systolic blood pressure loads on 24-h ABPM were associated with increased risk of elevated left ventricular mass index [22]. In another study, ABPM was more sensitive in diagnosing hypertension as compared to casual blood pressures among 25 pediatric peritoneal dialysis patients (56 vs. 32%, p < 0.05) [23].
Sodium and Water Retention
Inability to excrete sodium and water is the leading cause of hypertension in the dialysis population. Retention of sodium and water leads to increased extracellular volume and therefore increased cardiac output. Normotensive children on dialysis tend to have increased residual urine output as compared to hypertensive children [24]. Increased interdialytic weight gain has also correlated with increased blood pressure loads on ABPM [24]. The relationship between volume excess and hypertension is not exact, as a normotensive person can be hypervolemic and a hypertensive person can be normovolemic. This was demonstrated in a retrospective study that assessed 463 pre-HD BP assessment in 23 children over a year, relative to their hydration status as assessed by bioimpedance [25]. In the study, hypervolemia was defined as > 7% volume excess. Of the assessments that demonstrated hypertension, only 31% demonstrated hypervolemia, and 33% of the assessments that demonstrated normotension, hypervolemia was seen in 33% [25]. When hypertension is due to hypervolemia, achievement of normotension is often delayed by weeks after the achievement of normovolemia [26]. This observation is described as the “lag phenomenon.”
Dry Weight
Dry weight is defined as the body weight at the end of dialysis at which the patient can remain normotensive without antihypertensive medication, despite fluid accumulation, until the next dialysis treatment [27]. Stated differently, dry weight is the lowest weight a patient can tolerate without having symptoms of hypotension [27]. Thus, dry weight is often achieved by trial and error, and dry weight is thought to be achieved when the patient develops signs of hypotension, such as drop in blood pressure, cramping, yawning, headache, or abdominal pain. Complicating this further is that a patient may display signs of intravascular volume depletion despite being in salt and volume excess due to the aggressiveness of the ultrafiltration, or impaired ability for physiologic vasoconstriction during ultrafiltration due to vasodilatory antihypertensive medications.
Clinical assessment of dry weight includes monitoring weight, presence of edema, jugular venous distension, and crackles on lung auscultation in patients with volume excess and symptoms of orthostasis, sunken eyes, and hypotension in those with intravascular volume depletion. The clinical assessment is inaccurate in states of more subtle volume excess of depletion. Markers such as weight are further confounded in a growing child. Due to the limitations of relying on clinical assessment of dry weight, different techniques have been studied to aid in assessment and achievement of dry weight (Table 1). Biochemical markers include atrial natriuretic peptide, cyclic guanidine monophosphate, brain natriuretic peptide, and troponin T [28, 29]. Most of the biomarkers can be affected by various factors other than volume status, thus limiting their clinical utility. Ultrasound measurement of inferior vena cava diameter and its collapsibility is a simple and non-invasive way to assess intravascular volume status. Challenges that prevent broad use include inter-operator error and patient variability in diameter measurements [27, 29].
Bioelectrical impedance analysis, or bioimpedance, is a method that determines the electrical opposition (impedance) to the flow of an electric current through the body. The analysis using alternating current to determine total body water can be determined as a single frequency or multi-frequency. The addition of multi-frequency allows the ability to distinguish between intracellular and extracellular compartments [27, 29]. In adults, bioimpedance analysis has shown that extracellular volume change correlated with the ultrafiltration volume [30]. Using multi-frequency bioimpedance, HD patients demonstrated expanded extracellular space pre-dialysis as compared to healthy controls, and HD patients that demonstrated underhydration as compared to controls experienced more intradialytic hypotension [31]. Other studies in adults using bioimpedance have demonstrated underestimation of ultrafiltration volumes by 30% based on ECF volumes pre- and post-HD [27]. Pediatric studies have demonstrated the utility of this technique, showing good correlation of measured blood volume change to percentage body weight change [32], and serial clinical use to assess dry weight at a single center led to improvement in the medial left ventricular mass index and reduction in the left ventricular hypertrophy [33]. The technology does have limitations. Temperature and ion changes that occur during dialysis may affect electrical impedance, as may patient factors such as electrolyte imbalance, hematocrit values, and protein levels [27].
Lung ultrasound has been used to assess volume status. In the setting of extracellular fluid excess, hydrostatic forces will create a transudative effusion that leads to a decrease in the acoustic mismatch between lung and surrounding tissues. This creates a partial reflection and discrete hyper-echogenic reverberation of the ultrasound beam arising from the pleural line known as “B-lines” [34]. In adults, lung ultrasound findings including B-lines correlated with other markers of fluid overload including clinical parameters [35, 36], B-type natriuretic peptide, inferior vena cava diameter, and bioimpedance [37, 38]. B-lines are not present in euvolemic patients and appear before clinical signs of volume excess [35, 39, 40]. In a single-center study of 96 patients on HD in which lung ultrasound, bioimpedance, and echocardiography were prospectively studied for their ability to predict mortality, pre-dialysis B-line score and left ventricular mass index were significantly associated with survival times [41]. A recent pediatric study that included patients with end-stage renal disease on both modalities of dialysis and patients with acute kidney injury demonstrated a significant correlation between B-lines and volume excess as determined by target weight [34]. Among 13 children on dialysis in which objective parameters of volume excess were studied including lung ultrasound, bioimpedance, clinical parameters, and inferior vena cava parameter, only lung ultrasound correlated significantly with volume overload [34, 42].
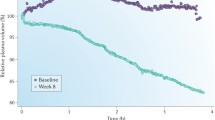
Relative plasma volume monitoring during HD provides insight into the relative rate of ultrafiltration compared to the rate of refilling of plasma volume from the extravascular space. Photo-optical technology measures hematocrit or protein values. Increase in hematocrit or protein concentration is inversely proportional to the change in plasma volume [27]. The graph is displayed as 1/hematocrit, where a downward slope reflects a decrease in plasma volume and therefore intravascular volume. A flat slope will reflect similar rates of ultrafiltration and refilling. A steep downward slope reflects an ultrafiltration rate that is faster than the refilling rate. This technology can also be used to prevent aggressive ultrafiltration and prevent intradialytic hypotension. The use of this technology in adults has led to mixed results with some reporting improvement in dry weight [43, 44] and some reporting improvement in casual blood pressures [45] and lower systolic blood pressure as measured by 44-h ABPM [46]. A randomized trial utilizing plasma volume monitoring was associated with higher access-related hospitalization and mortality [47]. Although the authors of the study and others have cautioned generalizations of the study due to atypically low hospitalization rates and mortality of the control group, and an observation that the control group may have received a more aggressive reduction in post-dialysis weight [47, 48], several pediatric studies have studied the use of plasma volume monitoring [49, 50, 51•, 52]. In a multicenter prospective study of 20 pediatric patients, plasma volume monitoring was used to target 100% ultrafiltration goal with 50% to be removed in the first hour (max plasma volume change of 8–12% per hour) and the remaining 50% over the subsequent time (max plasma volume change of 5% per hour) [51•]. They demonstrated a decrease in dialysis associated morbidity, reduction in antihypertensive medication, and improved ABPM profiles. There was no change in weight or left ventricular mass index at the end of the 6-month study [51•]. In 9 pediatric HD patients, the use of plasma volume monitoring to challenge dry weight and reduce antihypertensive use systematically over four phases (each phase more aggressively challenging dry weight) resulted in mean dry weight reduction, decreased blood pressure measured both casually and by ABPM, and a reduction in antihypertensive burden. There was a notation of increased intradialytic symptoms when weight was actively challenged in the later phases, but this did not reach statistical significance [52].
A recent study that compared various methods of assessment of volume status in chronic HD patients demonstrated that B-line scores with lung ultrasonography were more accurate in predicting overhydration as compared to bioelectrical impedance analysis and continuous volume monitoring when measured by inferior vena cava diameter [53]. A pragmatic and more accurate approach for assessment of volume status may be to utilize many if not all of the tools at the clinicians’ disposal as described by Ronco et al. [54].
Dietary Sodium Intake
The link between sodium intake and hypertension has been known since at least 1700 BC [26] and has been confirmed by modern studies dating to the 1950s when cultures with low salt intake were noted to have low normal blood pressures, even in elderly age [26, 55, 56]. The observation that dietary sodium restriction and ultrafiltration led to improved blood pressure management was noted by Belding Scribner when treating the first patient to receive chronic dialysis, who suffered from malignant hypertension [57]. Controlling dietary sodium intake facilitates achievement of dry weight [58] and is associated with decreased thirst, lower interdialytic weight gain, improved blood pressure control, lower LVMI, and decreased mortality in adults [59,60,61]. Despite guidelines recommending limiting sodium intake in children with kidney disease and hypertension between 1500 and 2300 mg depending on the age [62], data from a registry of children with chronic kidney disease demonstrated that sodium intake in children with chronic kidney disease stages 2–4 was greater than 3000 mg daily with 25% of adolescents consuming more than 5000 mg of sodium per day [63]. A study looking at sodium intake among school-aged children found that the top ten food categories that contributed to 48% of the salt intake are from processed foods, with the exception of milk, which naturally has sodium [64]. Similar results of US adults demonstrated that 70.9% of the salt consumed was sodium added to food outside the home [65]. Here, renal dieticians become key members of the treatment team by educating the patient and their family on low-sodium food with high nutritional content. The social worker can also play a role by providing better access to these often more expensive foods.
Optimization of Dialysis
Duration of therapy and concentration of dialysate sodium for hemodialysis have changed in the USA since chronic dialysis became possible in the 1960s. Clyde Shields’, the first chronic dialysis patient, initial prescription consisted of hemodialysis therapy lasting up to 76 h every week with dialysate sodium of 130 mEq/L [66]. Over time, dialysis prescriptions evolved to 20-h sessions twice a week with the goal of controlling blood pressure and reducing the progression of peripheral neuropathy [67]. After the seminal National Cooperative Dialysis Study (NCDS) [68•] determined that efficiency of urea clearance and not time was important for patient survival, short dialysis consisting of 3–4-h sessions three times a week was practiced in the 1980s [67]. The dialysate sodium concentration gradually increased from 134 to 136 in the 1980s to 136–149 from 2010 to 2015 [67]. Supra-physiologic sodium concentrations were used to reduce intradialytic hypotension that occurred as ultrafiltration rates needed to be increased to achieve the appropriate volume reduction in a shortened period. The practice of modifying sodium concentration in the dialysate over the course of the dialysis session, termed sodium modeling, did lead to better patient tolerability of hemodialysis due to reduced intradialytic hypotensive episodes [69], although the decreased clearance of sodium and at times increased sodium delivery to the patient resulted in increased interdialytic thirst, higher interdialytic weight gain, increased hypertension, and intradialytic hypotension [70, 71].
Currently, there is increasing evidence that reduction in dialysate sodium at or slightly below the patient’s pre-dialysis serum concentration leads to reduction in thirst, interdialytic weight gain, and hypertension [66, 72, 73]. A small pediatric study consisting of 5 patients demonstrated a reduction in interdialytic weight gain and pre-dialysis blood pressure when dialysate sodium was reduced from 140 to 138 mEq/L [73]. A systematic review of 23 studies comparing high vs. low dialysate sodium concentration in chronic adult hemodialysis patients demonstrated that blood pressure was unaffected by the concentration of dialysate sodium. There was an increase in interdialytic weight gain in the higher dialysate sodium group and increased intradialytic hypotension in the low dialysate sodium group [74]. Mortality was assessed in three observational studies and overall demonstrated reduced mortality with higher dialysate sodium concentrations, but was confounded by patients’ serum sodium concentrations, which demonstrated an inverse relationship between serum sodium concentration and death [74,75,76]. Specifically, an international study by Hecking et al. demonstrated lower serum sodium (< 137 mEq/L) was associated with the highest risk of death, and in that group dialyzing against a bath > 140 mEq/L was protective [75].
Increasing dialysis treatment time is another factor associated with improved outcomes. The recommendations from the European Best Practice Guidelines include a minimum duration of dialysis of 4 h three times a week [77]. As per the Clinical Performance Project Measures Project analysis of 32,065 patients from 2004 to 2007, only 25% received dialysis greater than 4 h per session while 25% received < 3 h and 15 min of dialysis [78]. Adult and pediatric studies have demonstrated improved control of blood pressure, faster achievement of dry weight, and reduction in medication burden including antihypertensive medications with increased dialysis time [79, 80, 81•, 82,83,84,85,86,87,88]. Increasing time also allows to reduce ultrafiltration rate which reduces the risk of myocardial stunning [89]. Current recommendation in adults is to reduce ultrafiltration rate to < 13 ml/kg/h, but even rates > 10 ml/kg/h are associated with increased morbidity and mortality [90, 91, 92•]. Myocardial stunning is not limited to adults as a pediatric study consisting of 12 patients of whom 11 demonstrated myocardial stunning which was associated with intradialytic blood pressure reduction. In this study, there was no association with ultrafiltration rate and stunning [93•].
Optimization of sodium and water removal in peritoneal dialysis can be achieved by managing osmotic potential (adjusting dextrose concentration and dwell time) and surface area recruitment and hydrostatic pressure (adjusting fill volume). The three-pore model theory of peritoneal transport describes three various-sized pores of the peritoneal endothelium through which transports of water and solutes are transported. The smallest are aquaporin channels via which only water can be transported that are activated by hyperosmolar state created by dextrose-based solutions, small pores that allow small solutes and water, and large pores that transport macromolecules [94]. Water removal is optimized by short dwell times to maintain the higher osmotic potential by a higher dextrose concentration, and lower fill volumes to reduce hydrostatic pressure that would counteract the osmotic potential [95]. In contrast, solute removal, including sodium, is optimized by increased fill volumes to optimize recruitment of the surface area and longer dwell time [95]. Using a higher dextrose concentration also leads to more glucose degradation products that are toxic to the peritoneum [96]. Another polymer of maltodextrin that is produced by the metabolism of cornstarch offers an alternative to dextrose, named icodextrin. Icodextrin is absorbed from the peritoneal space much more slowly via the lymphatics and thus maintains the osmotic potential longer. It further exerts its effect via colloid osmosis and therefore has its effects via the small pores and not the aquaporin channels, thus leading to less sodium sieving [97]. A recent retrospective study of 50 pediatric patients who had icodextrin as their fluid for the long day dwell demonstrated improved ultrafiltration and reduced absorption of icodextrin at fill volumes above 550 ml/m2, and improved ultrafiltration with increasing age, with the youngest patients absorbing more icodextrin [98]. Icodextrin is only meant to be used for the long dwell, as metabolism over time increases its colloid potential. Studies in adults have demonstrated equivalent ultrafiltration of icodextrin over 10 h and superior beyond that time as compared to 4.25% dextrose solutions [99, 100]. Adapted automated peritoneal dialysis is where the peritoneal dialysis machine will alternate between short dwells with low fill volumes to enhance ultrafiltration and long dwells with large fill volumes to enhance solute clearance [101, 102]. In a prospective, crossover study in adults, adaptive peritoneal dialysis resulted in increased sodium and water removal and improved blood pressures as compared to conventional peritoneal dialysis [102].
Diuretics
Diuretics have no benefit in anuric patients, even at high doses given intravenously [103]. In patients with preserved residual renal function, loop diuretics may enhance urine output and limit interdialytic weight gain [104]. There are no data for cardiovascular benefit or safety of diuretics in dialysis patients, and specific studies in pediatric patients are lacking.
Volume-Independent Causes of Hypertension
The renin-angiotensin-aldosterone system (RAAS) is a well-established cause of hypertension in chronic kidney disease and in ESRD [105]. Among 51 HD patients, plasma renin activity (PRA) was higher among patients who had uncontrolled hypertension as compared to those whose blood pressure was controlled by ultrafiltration and sodium restriction [105]. Among the 18 who had uncontrolled hypertension, 17 had significant improvement in blood pressure after native nephrectomies [105]. Angiotensin II and aldosterone both contribute to left ventricular hypertrophy and endothelial cell dysfunction that is independent of blood pressures [106]. A pediatric study compared RAAS between 32 healthy normotensive controls, 23 normotensive children with chronic kidney disease, 34 hypertensive children with chronic kidney disease, and 21 children with ESRD. PRA and angiotensin I, II, and (1–7) were higher in hypertensive patients with chronic kidney disease as compared to normotensive children with chronic kidney disease and healthy controls [107]. Treating patients with chronic kidney disease with angiotensin-converting enzyme inhibitors (ACEi) resulted in increased angiotensin 1–7 and decreased angiotensin II, whereas ESRD patients with ACEi therapy did not have a decrease in angiotensin II levels [107]. This may explain why refractory hypertensive ESRD patients may benefit form native nephrectomies.
ESRD patients are also known to have increased sympathetic nervous system activity [108]. The etiology of the increased sympathetic nervous system activity may be from the diseased native kidney. This was determined in an elegant study in transplant recipients who had continued elevation of the sympathetic nervous system until they had native nephrectomies [109]. In pediatrics, there has been a documentation of increase in catecholamines on HD during episodes of intradialytic hypotension [110]. Elevated sympathetic nervous system activation has been implicated in blunted nocturnal dipping [111] and increasing frequency of dialysis from three times a week for 4 h to six times a week for 2 h seems to result in lowering sympathetic nervous system activity [106, 112].
Arterial stiffness which occurs as a consequence of arteriosclerosis is seen naturally with aging but is accelerated in chronic disease states such as diabetes and chronic kidney disease/ESRD. Increased arterial stiffness is associated with increased risk of cardiovascular disease and mortality in adults [113]. Evidence exists of premature arterial stiffness in pediatric ESRD patients with correlations to a diagnosis of hypertension [106, 114].
Other factors implicated as an underlying cause of non-volume-dependent hypertension in ESRD patients include medications such as erythropoietin stimulating agents [115], endothelial cell dysfunction that results from an imbalance of endothelial cell-derived nitric oxide and endothelin-1 resulting in vasoconstriction [106, 116], inability to degrade catecholamines due to a lack of renalase which is usually secreted by the kidney [117], and other factors also leading to atherosclerosis such as oxidative stress and inflammation [106].
Antihypertensive Medications
With the exception of diuretics, all classes of antihypertensive medications are useful in blood pressure control in the dialysis population. Antihypertensive medications are ineffective when volume excess is the etiology of hypertension and studies have demonstrated hypertension to be associated with increased antihypertensive use [118]. Among uncontrolled hypertensive patients on antihypertensive medication in the Chronic Kidney Disease in children (CKiD) Study, uncontrolled hypertension was associated with absence of ACEi or angiotensin receptor blockers (ARB) [119]. A prospective study in the same cohort also demonstrated that antihypertensive use other than ACEi or ARB predicted increased left ventricular mass index [120]. A recent adult randomized control trial, among hypertensive chronic hemodialysis patients with left ventricular hypertrophy, compared the effectiveness of Lisinopril vs. Atenolol given three times a week post-dialysis towards regression of the left ventricular hypertrophy [121]. Both medications produced similar results in blood pressure improvement based on 44-h ABPM and in regression of left ventricular hypertrophy. When monthly home blood pressures were assessed, the Lisinopril group had higher blood pressures despite a greater number of antihypertensive agents and reduction in dry weight. The study was also stopped early due to increased risk of cardiovascular morbidity and mortality in the Lisinopril group as compared to the Atenolol group [121].
Pharmacokinetics and volume of distribution of the choice of antihypertensive should be considered. Water-soluble medication will be cleared during dialysis. This may be beneficial if patients suffer from intradialytic hypotension, but may be a contributing factor in those suffering from intradialytic hypertension. When medication noncompliance is a barrier, post-dialysis medication administration as described in the study above may be beneficial.
Conclusion
Hypertension is an important modifiable factor among patients on dialysis, whose primary cause of morbidity and mortality is cardiovascular disease. Achievement on dry weight and limiting both aggressiveness of interdialytic weight gain and ultrafiltration rate underlie the best approach. Utilization of tools to assess volume status beyond clinical assessment has shown promise in achieving normotension. When hypertension persists despite achievement of euvolemia, antihypertensive medications may be required and in some cases native nephrectomies (Fig. 1).
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
2017 USRDS annual data report: epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. In: Systems USRD, ed. Bethesda, MD2017.
Harambat J, van Stralen KJ, Kim JJ, Tizard EJ. Epidemiology of chronic kidney disease in children. Pediatr Nephrol. 2012;27(3):363–73.
Mitsnefes MM. Cardiovascular disease in children with chronic kidney disease. J Am Soc Nephrol. 2012;23(4):578–85.
• McDonald SP, Craig JC, Association AaNZPN. Long-term survival of children with end-stage renal disease. N Engl J Med. 2004;350(26):2654–62. Demonstrated the impact of cardiovascular disease among adults who had ESRD since childhood.
Groothoff JW, Gruppen MP, Offringa M, Hutten J, Lilien MR, van de Kar NJ, et al. Mortality and causes of death of end-stage renal disease in children: a Dutch cohort study. Kidney Int. 2002;61(2):621–9.
Parekh RS, Carroll CE, Wolfe RA, Port FK. Cardiovascular mortality in children and young adults with end-stage kidney disease. J Pediatr. 2002;141(2):191–7.
Agarwal R, Nissenson AR, Batlle D, Coyne DW, Trout JR, Warnock DG. Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med. 2003;115(4):291–7.
• Halbach SM, Martz K, Mattoo T, Flynn J. Predictors of blood pressure and its control in pediatric patients receiving dialysis. J Pediatr. 2012;160(4):621–625.e621. This study, along with the study below, clarified the prevalence of hypertension in pediatric population.
• Kramer AM, van Stralen KJ, Jager KJ, et al. Demographics of blood pressure and hypertension in children on renal replacement therapy in Europe. Kidney Int. 2011;80(10):1092–8. This study, along with the study above, clarified the prevalence of hypertension in pediatric population.
Mitsnefes M, Flynn J, Cohn S, Samuels J, Blydt-Hansen T, Saland J, et al. Masked hypertension associates with left ventricular hypertrophy in children with CKD. J Am Soc Nephrol. 2010;21(1):137–44.
Bullington N, Kartel J, Khoury P, Mitsnefes M. Left ventricular hypertrophy in pediatric kidney transplant recipients: long-term follow-up study. Pediatr Transplant. 2006;10(7):811–5.
Sorof JM, Alexandrov AV, Cardwell G, Portman RJ. Carotid artery intimal-medial thickness and left ventricular hypertrophy in children with elevated blood pressure. Pediatrics. 2003;111(1):61–6.
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, et al. Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation. 2002;106(1):100–5.
Ahuja TS, Grady J, Khan S. Changing trends in the survival of dialysis patients with human immunodeficiency virus in the United States. J Am Soc Nephrol. 2002;13(7):1889–93.
• Agarwal R, Peixoto AJ, Santos SF, Zoccali C. Pre- and postdialysis blood pressures are imprecise estimates of interdialytic ambulatory blood pressure. Clin J Am Soc Nephrol. 2006;1(3):389–98. Demonstrated peri-dialysis blood pressure measurements did not correlate with ambulatory blood pressure.
Agarwal R, Brim NJ, Mahenthiran J, Andersen MJ, Saha C. Out-of-hemodialysis-unit blood pressure is a superior determinant of left ventricular hypertrophy. Hypertension. 2006;47(1):62–8.
Moriya H, Ohtake T, Kobayashi S. Aortic stiffness, left ventricular hypertrophy and weekly averaged blood pressure (WAB) in patients on haemodialysis. Nephrol Dial Transplant. 2007;22(4):1198–204.
Moriya H, Oka M, Maesato K, Mano T, Ikee R, Ohtake T, et al. Weekly averaged blood pressure is more important than a single-point blood pressure measurement in the risk stratification of dialysis patients. Clin J Am Soc Nephrol. 2008;3(2):416–22.
Haskin O, Wong CJ, McCabe L, Begin B, Sutherland SM, Chaudhuri A. 44-h ambulatory blood pressure monitoring: revealing the true burden of hypertension in pediatric hemodialysis patients. Pediatr Nephrol. 2015;30(4):653–60.
Agarwal R. Blood pressure and mortality among hemodialysis patients. Hypertension. 2010;55(3):762–8.
• Alborzi P, Patel N, Agarwal R. Home blood pressures are of greater prognostic value than hemodialysis unit recordings. Clin J Am Soc Nephrol. 2007;2(6):1228–34. Demonstrated ambulatory blood pressure was more associated with mortality than peri-dialysis blood pressures.
Bircan Z, Duzova A, Cakar N, Bayazit AK, Elhan A, Tutar E, et al. Predictors of left ventricular hypertrophy in children on chronic peritoneal dialysis. Pediatr Nephrol. 2010;25(7):1311–8.
Ozçakar ZB, Yalçinkaya F, Tutar E, et al. Hypertension and left ventricular hypertrophy in pediatric peritoneal dialysis patients: ambulatory blood pressure monitoring and echocardiographic evaluation. Nephron Clin Pract. 2006;104(2):c101–6.
Tkaczyk M, Nowicki M, Bałasz-Chmielewska I, Boguszewska-Bączkowska H, Drożdż D, Kołłątaj B, et al. Hypertension in dialysed children: the prevalence and therapeutic approach in Poland—a nationwide survey. Nephrol Dial Transplant. 2006;21(3):736–42.
Zaloszyc A, Schaefer B, Schaefer F, Krid S, Salomon R, Niaudet P, et al. Hydration measurement by bioimpedance spectroscopy and blood pressure management in children on hemodialysis. Pediatr Nephrol. 2013;28(11):2169–77.
Twardowski ZJ. Sodium, hypertension, and an explanation of the “lag phenomenon” in hemodialysis patients. Hemodial Int. 2008;12(4):412–25.
Jaeger JQ, Mehta RL. Assessment of dry weight in hemodialysis: an overview. J Am Soc Nephrol. 1999;10(2):392–403.
Zhu F, Rosales L, Kotanko P. Techniques for assessing fluids status in patients with kidney disease. Curr Opin Nephrol Hypertens. 2016;25(6):473–9.
Dou Y, Zhu F, Kotanko P. Assessment of extracellular fluid volume and fluid status in hemodialysis patients: current status and technical advances. Semin Dial. 2012;25(4):377–87.
Lukaski HC, Bolonchuk WW. Estimation of body fluid volumes using tetrapolar bioelectrical impedance measurements. Aviat Space Environ Med. 1988;59(12):1163–9.
Kouw PM, Olthof CG, ter Wee PM, Oe LP, Donker AJM, Schneider H, et al. Assessment of post-dialysis dry weight: an application of the conductivity measurement method. Kidney Int. 1992;41(2):440–4.
Oh G, Wong C, Begin B, Salsbery K, Sutherland S, Chaudhuri A. Whole-body single-frequency bioimpedance analysis in pediatric hemodialysis patients. Pediatr Nephrol. 2014;29(8):1417–23.
Paglialonga F, Ardissino G, Galli MA, Scarfia RV, Testa S, Edefonti A. Bioimpedance analysis and cardiovascular status in pediatric patients on chronic hemodialysis. Hemodial Int. 2012;16(Suppl 1):S20–5.
Allinovi M, Saleem M, Romagnani P, Nazerian P, Hayes W. Lung ultrasound: a novel technique for detecting fluid overload in children on dialysis. Nephrol Dial Transplant. 2017;32(3):541–7.
Trezzi M, Torzillo D, Ceriani E, Costantino G, Caruso S, Damavandi PT, et al. Lung ultrasonography for the assessment of rapid extravascular water variation: evidence from hemodialysis patients. Intern Emerg Med. 2013;8(5):409–15.
Noble VE, Murray AF, Capp R, Sylvia-Reardon MH, Steele DJR, Liteplo A. Ultrasound assessment for extravascular lung water in patients undergoing hemodialysis. Time course for resolution. Chest. 2009;135(6):1433–9.
Vitturi N, Dugo M, Soattin M, Simoni F, Maresca L, Zagatti R, et al. Lung ultrasound during hemodialysis: the role in the assessment of volume status. Int Urol Nephrol. 2014;46(1):169–74.
Basso F, Milan Manani S, Cruz DN, Teixeira C, Brendolan A, Nalesso F, et al. Comparison and reproducibility of techniques for fluid status assessment in chronic hemodialysis patients. Cardiorenal Med. 2013;3(2):104–12.
Zoccali C, Tripepi R, Torino C, Bellantoni M, Tripepi G, Mallamaci F. Lung congestion as a risk factor in end-stage renal disease. Blood Purif. 2013;36(3–4):184–91.
Torino C, Gargani L, Sicari R, Letachowicz K, Ekart R, Fliser D, et al. The agreement between auscultation and lung ultrasound in hemodialysis patients: the LUST study. Clin J Am Soc Nephrol. 2016;11(11):2005–11.
Siriopol D, Hogas S, Voroneanu L, Onofriescu M, Apetrii M, Oleniuc M, et al. Predicting mortality in haemodialysis patients: a comparison between lung ultrasonography, bioimpedance data and echocardiography parameters. Nephrol Dial Transplant. 2013;28(11):2851–9.
Allinovi M, Saleem MA, Burgess O, Armstrong C, Hayes W. Finding covert fluid: methods for detecting volume overload in children on dialysis. Pediatr Nephrol. 2016;31(12):2327–35.
Rodriguez HJ, Domenici R, Diroll A, Goykhman I. Assessment of dry weight by monitoring changes in blood volume during hemodialysis using Crit-Line. Kidney Int. 2005;68(2):854–61.
Steuer RR, Germain MJ, Leypoldt JK, Cheung AK. Enhanced fluid removal guided by blood volume monitoring during chronic hemodialysis. Artif Organs. 1998;22(8):627–32.
Dasselaar JJ, Huisman RM, de Jong PE, Burgerhof JG, Franssen CF. Effects of relative blood volume-controlled hemodialysis on blood pressure and volume status in hypertensive patients. ASAIO J. 2007;53(3):357–64.
Sinha AD, Light RP, Agarwal R. Relative plasma volume monitoring during hemodialysis AIDS the assessment of dry weight. Hypertension. 2010;55(2):305–11.
Reddan DN, Szczech LA, Hasselblad V, Lowrie EG, Lindsay RM, Himmelfarb J, et al. Intradialytic blood volume monitoring in ambulatory hemodialysis patients: a randomized trial. J Am Soc Nephrol. 2005;16(7):2162–9.
Georgianos PI, Agarwal R. Epidemiology, diagnosis and management of hypertension among patients on chronic dialysis. Nat Rev Nephrol. 2016;12(10):636–47.
Jain SR, Smith L, Brewer ED, Goldstein SL. Non-invasive intravascular monitoring in the pediatric hemodialysis population. Pediatr Nephrol. 2001;16(1):15–8.
Michael M, Brewer ED, Goldstein SL. Blood volume monitoring to achieve target weight in pediatric hemodialysis patients. Pediatr Nephrol. 2004;19(4):432–7.
• Patel HP, Goldstein SL, Mahan JD, et al. A standard, noninvasive monitoring of hematocrit algorithm improves blood pressure control in pediatric hemodialysis patients. Clin J Am Soc Nephrol. 2007;2(2):252–7. Demonstrated that the use of non-invasive blood volume monitoring in children resulted in improved blood pressure control, decreased antihypertensives, and reduced intra-dialytic symptoms.
Candan C, Sever L, Civilibal M, Caliskan S, Arisoy N. Blood volume monitoring to adjust dry weight in hypertensive pediatric hemodialysis patients. Pediatr Nephrol. 2009;24(3):581–7.
Alexiadis G, Panagoutsos S, Roumeliotis S, Stibiris I, Markos A, Kantartzi K, et al. Comparison of multiple fluid status assessment methods in patients on chronic hemodialysis. Int Urol Nephrol. 2017;49(3):525–32.
Ronco C, Kaushik M, Valle R, Aspromonte N, Peacock WF. Diagnosis and management of fluid overload in heart failure and cardio-renal syndrome: the “5B” approach. Semin Nephrol. 2012;32(1):129–41.
Dahl LK. Salt and hypertension. Am J Clin Nutr. 1972;25(2):231–44.
Oliver WJ, Cohen EL, Neel JV. Blood pressure, sodium intake, and sodium related hormones in the Yanomamo Indians, a “no-salt” culture. Circulation. 1975;52(1):146–51.
SCRIBNER BH, BURI R, CANER JE, HEGSTROM R, BURNELL JM. The treatment of chronic uremia by means of intermittent hemodialysis: a preliminary report. Trans Am Soc Artif Intern Organs. 1960;6:114–22.
Kooman JP, van der Sande F, Leunissen K, Locatelli F. Sodium balance in hemodialysis therapy. Semin Dial. 2003;16(5):351–5.
Kayikcioglu M, Tumuklu M, Ozkahya M, et al. The benefit of salt restriction in the treatment of end-stage renal disease by haemodialysis. Nephrol Dial Transplant. 2009;24(3):956–62.
Mc Causland FR, Waikar SS, Brunelli SM. Increased dietary sodium is independently associated with greater mortality among prevalent hemodialysis patients. Kidney Int. 2012;82(2):204–11.
Maduell F, Navarro V. Dietary salt intake and blood pressure control in haemodialysis patients. Nephrol Dial Transplant. 2000;15(12):2063.
(K/DOQI) KDOQI. K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43(5 Suppl 1):S1–290.
Hui WF, Betoko A, Savant JD, Abraham AG, Greenbaum LA, Warady B, et al. Assessment of dietary intake of children with chronic kidney disease. Pediatr Nephrol. 2017;32(3):485–94.
Quader ZS, Gillespie C, Sliwa SA, et al. Sodium intake among US school-aged children: National Health and Nutrition Examination Survey, 2011–2012. J Acad Nutr Diet. 2017;117(1):39–47.e35.
Harnack LJ, Cogswell ME, Shikany JM, Gardner CD, Gillespie C, Loria CM, et al. Sources of sodium in US adults from 3 geographic regions. Circulation. 2017;135(19):1775–83.
Munoz Mendoza J, Arramreddy R, Schiller B. Dialysate sodium: choosing the optimal hemodialysis bath. Am J Kidney Dis. 2015;66(4):710–20.
Kramer H, Yee J, Weiner DE, Bansal V, Choi MJ, Brereton L, et al. Ultrafiltration rate thresholds in maintenance hemodialysis: an NKF-KDOQI controversies report. Am J Kidney Dis. 2016;68(4):522–32.
• Lowrie EG, Laird NM, Parker TF, Sargent JA. Effect of the hemodialysis prescription of patient morbidity: report from the National Cooperative Dialysis Study. N Engl J Med. 1981;305(20):1176–81. First randomized control trial in dialysis that studied if time or time-averaged urea concentration was more important to reduce morbidity and mortality. Led to the creation of Kt/V to measure clearance, and a shift toward shorter time on dialysis.
Sadowski RH, Allred EN, Jabs K. Sodium modeling ameliorates intradialytic and interdialytic symptoms in young hemodialysis patients. J Am Soc Nephrol. 1993;4(5):1192–8.
Song JH, Lee SW, Suh CK, Kim MJ. Time-averaged concentration of dialysate sodium relates with sodium load and interdialytic weight gain during sodium-profiling hemodialysis. Am J Kidney Dis. 2002;40(2):291–301.
Song JH, Park GH, Lee SY, Lee SW, Kim MJ. Effect of sodium balance and the combination of ultrafiltration profile during sodium profiling hemodialysis on the maintenance of the quality of dialysis and sodium and fluid balances. J Am Soc Nephrol. 2005;16(1):237–46.
Thein H, Haloob I, Marshall MR. Associations of a facility level decrease in dialysate sodium concentration with blood pressure and interdialytic weight gain. Nephrol Dial Transplant. 2007;22(9):2630–9.
Marsenic O, Anderson M, Couloures KG, Hong WS, Kevin Hall E, Dahl N. Effect of the decrease in dialysate sodium in pediatric patients on chronic hemodialysis. Hemodial Int. 2016;20(2):277–85.
Basile C, Pisano A, Lisi P, Rossi L, Lomonte C, Bolignano D. High versus low dialysate sodium concentration in chronic haemodialysis patients: a systematic review of 23 studies. Nephrol Dial Transplant. 2016;31(4):548–63.
Hecking M, Karaboyas A, Saran R, Sen A, Hörl WH, Pisoni RL, et al. Predialysis serum sodium level, dialysate sodium, and mortality in maintenance hemodialysis patients: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2012;59(2):238–48.
Hecking M, Karaboyas A, Saran R, Sen A, Inaba M, Rayner H, et al. Dialysate sodium concentration and the association with interdialytic weight gain, hospitalization, and mortality. Clin J Am Soc Nephrol. 2012;7(1):92–100.
Tattersall J, Martin-Malo A, Pedrini L, et al. EBPG guideline on dialysis strategies. Nephrol Dial Transplant. 2007;22(Suppl 2):ii5–21.
Foley RN, Gilbertson DT, Murray T, Collins AJ. Long interdialytic interval and mortality among patients receiving hemodialysis. N Engl J Med. 2011;365(12):1099–107.
Tandon T, Sinha AD, Agarwal R. Shorter delivered dialysis times associate with a higher and more difficult to treat blood pressure. Nephrol Dial Transplant. 2013;28(6):1562–8.
Brunet P, Saingra Y, Leonetti F, Vacher-Coponat H, Ramananarivo P, Berland Y. Tolerance of haemodialysis: a randomized cross-over trial of 5-h versus 4-h treatment time. Nephrol Dial Transplant. 1996;11(Suppl 8):46–51.
• Chertow GM, Levin NW, Beck GJ, et al. In-center hemodialysis six times per week versus three times per week. N Engl J Med. 2010;363(24):2287–300. Demonstrated decreased morbidity in patients that received more frequent dialysis.
Georgianos PI, Sarafidis PA, Sinha AD, Agarwal R. Adverse effects of conventional thrice-weekly hemodialysis: is it time to avoid 3-day interdialytic intervals? Am J Nephrol. 2015;41(4–5):400–8.
Ok E, Duman S, Asci G, Tumuklu M, Onen Sertoz O, Kayikcioglu M, et al. Comparison of 4- and 8-h dialysis sessions in thrice-weekly in-centre haemodialysis: a prospective, case-controlled study. Nephrol Dial Transplant. 2011;26(4):1287–96.
Fischbach M, Terzic J, Laugel V, Escande B, Dangelser C, Helmstetter A. Measurement of hydrostatic intraperitoneal pressure: a useful tool for the improvement of dialysis dose prescription. Pediatr Nephrol. 2003;18(10):976–80.
Goldstein SL, Silverstein DM, Leung JC, Feig DI, Soletsky B, Knight C, et al. Frequent hemodialysis with NxStage system in pediatric patients receiving maintenance hemodialysis. Pediatr Nephrol. 2008;23(1):129–35.
Hoppe A, von Puttkamer C, Linke U, et al. A hospital-based intermittent nocturnal hemodialysis program for children and adolescents. J Pediatr. 2011;158(1):95–9. 99.e91
Thumfart J, Puttkamer CV, Wagner S, Querfeld U, Müller D. Hemodiafiltration in a pediatric nocturnal dialysis program. Pediatr Nephrol. 2014;29(8):1411–6.
Thumfart J, Hilliger T, Stiny C, Wagner S, Querfeld U, Müller D. Is peritoneal dialysis still an equal option? Results of the Berlin pediatric nocturnal dialysis program. Pediatr Nephrol. 2015;30(7):1181–7.
McIntyre CW. Effects of hemodialysis on cardiac function. Kidney Int. 2009;76(4):371–5.
Movilli E, Gaggia P, Zubani R, Camerini C, Vizzardi V, Parrinello G, et al. Association between high ultrafiltration rates and mortality in uraemic patients on regular haemodialysis. A 5-year prospective observational multicentre study. Nephrol Dial Transplant. 2007;22(12):3547–52.
Movilli E, Camerini C, Gaggia P, Zubani R, Feller P, Poiatti P, et al. Magnitude of end-dialysis overweight is associated with all-cause and cardiovascular mortality: a 3-year prospective study. Am J Nephrol. 2013;37(4):370–7.
• Saran R, Bragg-Gresham JL, Levin NW, Twardowski ZJ, Wizemann V, Saito A, et al. Longer treatment time and slower ultrafiltration in hemodialysis: associations with reduced mortality in the DOPPS. Kidney Int. 2006;69(7):1222–8. International study demonstrated the risk of aggressive ultrafiltration.
• Hothi DK, Rees L, Marek J, Burton J, McIntyre CW. Pediatric myocardial stunning underscores the cardiac toxicity of conventional hemodialysis treatments. Clin J Am Soc Nephrol. 2009;4(4):790–7. Described that myocardial stunning occurs in the pediatric population as well.
Rippe B. A three-pore model of peritoneal transport. Perit Dial Int. 1993;13(Suppl 2):S35–8.
Fischbach M, Schmitt CP, Shroff R, Zaloszyc A, Warady BA. Increasing sodium removal on peritoneal dialysis: applying dialysis mechanics to the peritoneal dialysis prescription. Kidney Int. 2016;89(4):761–6.
Erixon M, Wieslander A, Lindén T, Carlsson O, Forsbäck G, Svensson E, et al. How to avoid glucose degradation products in peritoneal dialysis fluids. Perit Dial Int. 2006;26(4):490–7.
Frampton JE, Plosker GL. Icodextrin: a review of its use in peritoneal dialysis. Drugs. 2003;63(19):2079–105.
Rousso S, Banh TM, Ackerman S, Piva E, Licht C, Harvey EA. Impact of fill volume on ultrafiltration with icodextrin in children on chronic peritoneal dialysis. Pediatr Nephrol. 2016;31(10):1673–9.
Collins A, Mujais S. Advancing fluid management in peritoneal dialysis. Kidney Int Suppl. 2002;81:S1–2.
Mujais S, Vonesh E. Profiling of peritoneal ultrafiltration. Kidney Int Suppl. 2002;62(81):S17–22.
Fischbach M, Desprez P, Donnars F, Hamel G, Geisert J. Optimization of CCPD prescription in children using peritoneal equilibration test. Adv Perit Dial. 1994;10:307–9.
Fischbach M, Issad B, Dubois V, Taamma R. The beneficial influence on the effectiveness of automated peritoneal dialysis of varying the dwell time (short/long) and fill volume (small/large): a randomized controlled trial. Perit Dial Int. 2011;31(4):450–8.
Hayashi SY, Seeberger A, Lind B, et al. Acute effects of low and high intravenous doses of furosemide on myocardial function in anuric haemodialysis patients: a tissue Doppler study. Nephrol Dial Transplant. 2008;23(4):1355–61.
Lemes HP, Araujo S, Nascimento D, Cunha D, Garcia C, Queiroz V, et al. Use of small doses of furosemide in chronic kidney disease patients with residual renal function undergoing hemodialysis. Clin Exp Nephrol. 2011;15(4):554–9.
Weidmann P, Maxwell MH, Lupu AN, Lewin AJ, Massry SG. Plasma renin activity and blood pressure in terminal renal failure. N Engl J Med. 1971;285(14):757–62.
Van Buren PN, Inrig JK. Hypertension and hemodialysis: pathophysiology and outcomes in adult and pediatric populations. Pediatr Nephrol. 2012;27(3):339–50.
Simões e Silva AC, Diniz JS, Pereira RM, Pinheiro SV, Santos RA. Circulating renin angiotensin system in childhood chronic renal failure: marked increase of angiotensin-(1-7) in end-stage renal disease. Pediatr Res. 2006;60(6):734–9.
Converse RL, Jacobsen TN, Toto RD, et al. Sympathetic overactivity in patients with chronic renal failure. N Engl J Med. 1992;327(27):1912–8.
Hausberg M, Kosch M, Harmelink P, Barenbrock M, Hohage H, Kisters K, et al. Sympathetic nerve activity in end-stage renal disease. Circulation. 2002;106(15):1974–9.
Rauh W, Hund E, Sohl G, Rascher W, Mehls O, Schärer K. Vasoactive hormones in children with chronic renal failure. Kidney Int Suppl. 1983;15:S27–33.
Liu M, Takahashi H, Morita Y, et al. Non-dipping is a potent predictor of cardiovascular mortality and is associated with autonomic dysfunction in haemodialysis patients. Nephrol Dial Transplant. 2003;18(3):563–9.
Zilch O, Vos PF, Oey PL, Cramer MJM, Ligtenberg G, Koomans HA, et al. Sympathetic hyperactivity in haemodialysis patients is reduced by short daily haemodialysis. J Hypertens. 2007;25(6):1285–9.
Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness on survival in end-stage renal disease. Circulation. 1999;99(18):2434–9.
Gbadegesin R, Kudelka T, Gadegbeku CA, Brophy P, Smoyer WE, Lin JJ. Arterial compliance in adolescents and young adults receiving chronic hemodialysis. Ren Fail. 2008;30(6):591–6.
Brandt JR, Avner ED, Hickman RO, Watkins SL. Safety and efficacy of erythropoietin in children with chronic renal failure. Pediatr Nephrol. 1999;13(2):143–7.
Shichiri M, Hirata Y, Ando K, Emori T, Ohta K, Kimoto S, et al. Plasma endothelin levels in hypertension and chronic renal failure. Hypertension. 1990;15(5):493–6.
Xu J, Li G, Wang P, Velazquez H, Yao X, Li Y, et al. Renalase is a novel, soluble monoamine oxidase that regulates cardiac function and blood pressure. J Clin Invest. 2005;115(5):1275–80.
Agarwal R, Weir MR. Dry-weight: a concept revisited in an effort to avoid medication-directed approaches for blood pressure control in hemodialysis patients. Clin J Am Soc Nephrol. 2010;5(7):1255–60.
Flynn JT, Mitsnefes M, Pierce C, Cole SR, Parekh RS, Furth SL, et al. Blood pressure in children with chronic kidney disease: a report from the Chronic Kidney Disease in Children study. Hypertension. 2008;52(4):631–7.
Kupferman JC, Aronson Friedman L, Cox C, Flynn J, Furth S, Warady B, et al. BP control and left ventricular hypertrophy regression in children with CKD. J Am Soc Nephrol. 2014;25(1):167–74.
Agarwal R, Sinha AD, Pappas MK, Abraham TN, Tegegne GG. Hypertension in hemodialysis patients treated with atenolol or lisinopril: a randomized controlled trial. Nephrol Dial Transplant. 2014;29(3):672–81.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatric Hypertension
Rights and permissions
About this article
Cite this article
Munshi, R., Flynn, J.T. Hypertension in Pediatric Dialysis Patients: Etiology, Evaluation, and Management. Curr Hypertens Rep 20, 61 (2018). https://doi.org/10.1007/s11906-018-0857-z
Published:
DOI: https://doi.org/10.1007/s11906-018-0857-z