Abstract
Conflicting results have been reported in small non-homogenous groups of children with chronic renal failure in terms of casual blood pressure and ambulatory blood pressure monitoring (ABPM) parameters and left ventricular hypertrophy (LVH). The aim of our study was to assess the value of ABPM and hematological and biochemical parameters in predicting LVH in children on chronic peritoneal dialysis (CPD). Echocardiography and 24-h ABPM were performed in addition to routine biochemical and hematological evaluations in 47 children on CPD (26 male, 21 female; mean age 14.74 ± 3.52 years). Mean daytime systolic blood pressure (SBP) and mean daytime diastolic blood pressure (DBP) values were found to be higher than the mean casual SBP and DBP (p = 0.001) values. Thirty-three (70.2%) children had LVH. The correlations between the left ventricular mass index and ABPM variables were good. Stepwise multiple regression analysis revealed daytime SBP load (β = 0.652; p < 0.01) and hematocrit (β = −0.282; p < 0.01) to be independent predictors of LVH. The sensitivity, specificity, positive predictive value, and negative predictive values for the combination of the SBP load >15% and hematocrit value <31% for predicting LVH were 95 [95% confidence interval (CI) 76–99], 78 (95%CI 45–94), 91 (95%CI 73–98), and 88% (95%CI 69–96%), respectively. We conclude that: (1) LVH is prevalent in children on CPD, and (2) a target hematocrit level >31% and daytime SBP load <15% may be preventive for the progression of LVH in the follow-up of children on CPD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ambulatory blood pressure monitoring (ABPM) can be used to precisely characterize the variations in blood pressure (BP) that occur during daily activities [1]. It is also superior to casual blood pressure (CBP) in predicting cardiovascular morbidity and mortality in adults [2]. To date, there have been no outcome studies on ABPM levels in children [3]. In children with primary hypertension, the left ventricular mass (LVM) index has been found to be weakly correlated with 24-h systolic BP (SBP) (r = 0.34; p < 0.05), 24-h systolic SBP load (r = 0.38; p < 0.05), daytime SBP load (r = 0.37; p < 0.05), nighttime SBP (r = 0.33; p < 0.05), and nighttime SBP load (r = 0.38; p < 0.05) [4]. However, conflicting results have been reported in small non-homogenous groups of children with chronic renal failure (CRF), including chronic peritoneal dialysis (CPD), hemodialysis (HD), and predialysis patients in terms of CBP and ABPM parameters and LVH [5–10].
A few studies have reported a positive correlation between the LVMI and indexed SBP [6], interval change in indexed SBP [9], normalization of SBP [10], and interval change in nighttime SBP load [8], while others have reported the absence of any relationship between BP, the BP index, or blood pressure load in patients with CRF [5, 7].
The aim of our study was to identify predictors of left ventricular hypertrophy (LVH) in a homogenous group of children with CRF on CPD. To this end, ABPM and hematological and biochemical parameters were evaluated together with echocardiography. To the best of our knowledge, our study cohort is the largest population sample of children on CPD reported to date for whom left ventricular geometry was assessed together with ABPM and routine hematological and biochemical variables.
Materials and methods
Subjects
This was a cross-sectional, multicenter study (five different pediatric nephrology centers in Turkey) involving 47 children on CPD. The patient cohort consisted of all CPD patients who presented to the participating pediatric nephrology centers for routine follow-up visits between October 2007 and February 2008. Inclusion criteria were (1) duration of CPD ≥3 months, (2) age between 6–20 years, (3) height ≥ 120 cm (due to the absence of ABPM reference tables for children <120 cm), (4) and absence of any primary and congenital myocardial disease. The study was conducted according to the Declaration of Helsinki, and the Human Research Ethical Committee of Kocaeli University Hospital approved the study. Informed consent was obtained from the patient and/or from the parents of each patient.
A review of the medical records and personal interviews were used to determine the age, sex, cause of chronic renal disease, duration of renal failure, duration of CPD, and type of antihypertensive medications. Clinical and laboratory data were collected on the day of the echocardiographic evaluation. Results of routine biochemical and hematological tests [urea, creatinine, calcium, phosphate, alkaline phosphatase, sodium, potassium, chloride, total protein, albumin, cholesterol, triglycerides, high-density lipoprotein (HDL), very low density lipoprotein (VLDL), low-density lipoprotein (LDL), homocysteine, ferritin, transferrin saturation, intact parathyroid hormone (PTH), blood gases, complete blood count, highly sensitive C-reactive protein (CRP), serum N-terminal-pro-brain natriuretic peptide (NT-pro-BNP), 24-h urine creatinine, and urea] were obtained. The estimated glomerular filtration rate (eGFR) was calculated as a measure of residual renal function from the formula:
where U is urine and P is plasma. The values of Kt/V urea for each patient were also calculated during the study period.
Serum NT-pro-BNP measurement
Serum NT-pro-BNP was quantified by an electrochemiluminescence immunoassay on an Elecsys 2010 analyzer (Roche Diagnostics, Indianapolis, IN) with an inter-assay coefficient of variation (CV) of 2.6% at 1068 pg/ml and a measuring range from 5 to 35,000 pg/ml. For samples with NT-pro-BNP concentrations above the measuring range, the final concentrations were taken as 35,000 pg/ml.
BP measurements
Casual BP was measured three times, with 10-min intervals between measurements, by the auscultation method using an appropriately sized cuff while the patient was at rest in a sitting down position. The diagnosis of hypertension for casual BP was based on the fourth report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents [11]. Systolic and diastolic BP (DBP) were indexed to the age-, sex-, and height-specific percentiles for each subject (measured SBP or DBP divided by the age-, sex-, and height-specific 95th percentile SBP or DBP). Standard deviation scores (SDS) for SBP and DBP were also calculated [11].
The ABPM was performed by the oscillometric method using Spacelabs Monitor model 90207 (SpaceLabs Medical, Redmond, WA). The monitor was set up to measure BP every 20 min from 08:00 am to 08:00 pm and every 30 min from 08:00 pm to 8:00 am using appropriate cuff size. A diary of the patient was evaluated with a personal interview. Records with fewer than 70% readings were considered to be unsuccessful and repeated [12]. SBP and DBP were determined for daytime (08:00 am to 08:00 pm), nighttime (midnight to 06:00 am), and 24-h periods [12]. Dipping was defined as a ≥10% drop in mean SBP or DBP between the daytime and nighttime measurements. The BP load was defined as the percentage of BP readings for a given period that exceeds the ABPM 95th percentile for that patient. SDS for ABPM were calculated using the LMS reference tables (LMS reference values of mean 24-h, daytime and nighttime systolic, diastolic and mean arterial BP relative to gender, age and height) developed by Wühl et al. [12], who used the modified LMS method of Cole and Green [13].
Echocardiography
An echocardiography was performed with the peritoneal cavity empty of dialysis solution for each patient as a part of the routine evaluation. Two-dimensional and M-mode echocardiographies were performed using the Toshiba Xario device (Toshiba Medical Devices, Hamamatsucho, Tokyo) operated by an experienced pediatric cardiologist in each center who was unaware of the results of the BP measurements. Standard techniques were used. The LVM was measured according to the American Society of Echocardiography criteria [14] and calculated using the Devereux formula [15]. The left ventricular mass index (LVMI) was calculated by dividing LVM by height2.7 to minimize the effects of age, gender, and overweight status. The LVH was defined as an LVMI >95th percentile (38 g/m2.7) for normal children and adolescents. Relative wall thickness (RWT) was measured to assess the left ventricular geometric pattern. Patients with LVH and elevated RWT (≥0.35) had concentric LVH, and those with LVH and normal RWT (<0.35) had eccentric LVH. Concentric remodeling was defined as an elevated RWT, but with normal LVMI [16, 17]. The echocardiograms were performed by four cardiologists.
Statistical analysis
The results were analyzed using SPSS for Windows ver. 13.0 (SPSS, Chicago, IL), and the descriptive statistics are presented as mean ± standard deviation (SD) if equally distributed or as median and interquartile range (IQR) if unequally distributed. Univariate analysis for group comparisons were performed using the Student t test for equally distributed variables, the Mann–Whitney test for unequally distributed variables, and the chi-square test for categorical variables. The degree of association between LVMI and clinical and laboratory variables were determined using the Pearson or Spearman correlation coefficient, where appropriate. Stepwise multiple regression analysis was performed to assess whether there were significantly independent predictors of LVMI. Receiver operating curve (ROC) analysis was performed to predict the cut-off value of the best independent variable for LVMI.
Results
The study population comprised 47 (female/male, 21/26) patients on CPD [automated peritoneal dialysis (APD), n = 10; continuous ambulatory peritoneal dialysis (CAPD), n = 31; APD and CAPD, n = 6]. The disorders causing end-stage renal disease (ESRD) in the study population included glomerular diseases (n = 24; 51%), congenital urologic disorders (n = 19; 40%), and unknown etiologies (n = 4; 9%). CPD was the first treatment modality as renal replacement therapy in 46 patients; hemodialysis was performed before CPD in one patient for 54 months. Dwell volume ranged from 800 to 1200 ml/m2; Patients on CAPD used four to five bags and those on APD ± CAPD used six to ten bags. Median duration of CPD was 29 months (range 3–123 months; IQR 47 months). Twenty-seven patients had a urine output of >400 ml/day (median 1200 ml; range 500–2900 ml/day), and 20 patients were anuric for 17 months (range 1–120 months). Twenty-eight patients (60%) were taking antihypertensive medications, of whom 11 were on one drug, nine were on two drugs, and eight were on more than two drugs; 22 of these were on angiotensin converting enzyme inhibitor. Thirty-six patients (77%) were on erythropoietin treatment. BP control was achieved in 57.4% of patients based on casual BP measurement: 17 patients (36.2%) had systolic and diastolic hypertension, and three (6.4%) had diastolic hypertension alone. The mean Kt/V urea was 2.26 ± 0.60 (range 1.22–3.95), with the Kt/V urea >2.0 in 66.6% of the patients. The patient characteristics are presented in Table 1.
Casual BP and ABPM data of the patients are shown in Table 2. Daytime mean SBP and mean DBP values were found to be higher than mean casual SBP and DBP (p = 0.001).
The mean LVMI was 49.53 ± 16.37 g/m2.7 (IQR 25.02–93.97), and 33 (70.2%) children had LVH. Only one of the patients had normal RWT and LVMI, whereas 13 (27.7%) had concentric remodeling and 33 (70.2%) had concentric hypertrophy. No eccentric hypertrophy was recorded.
When the patients were classified according to the criteria used by Sorof (SBP load >50% and 24-h SBP index >1.0), 18 patients had SBP load > 50% and a 24-h SBP index >1.0. Seventeen patients (17/18; 94.4%) in this group, and 16 of the remaining patients (16/29, 52.2%) had LVH (p <0.005). The sensitivity, specificity, positive predictive value, and negative predictive values for the criteria used by Sorof were 52 (95%CI 35–68), 93 (95%CI 69–99), 94 (95%CI 83–99), and 45% (95%CI 31%–60%), respectively.
The prevalence of LVH was higher among hypertensive patients based on casual BP (85 vs. 60%, p = 0.056). The sensitivity, specificity, positive predictive value, and negative predictive values for HT based on casual BP were 52 (95%CI 35–68%), 79 (95%CI 52–92%), 85 (95%CI 71–93%), and 41% (95%CI 27–56%), respectively.
The correlation between LVMI and casual and ABP variables (day- and nighttime BP, SDS, and BP load values for SBP, DBP, and MAP) ranged from −0.428 to 0.759 (p < 0.001; Table 3); the highest correlations were with daytime SBP load (r = 0.703; p < 0.001), nighttime SBP-SDS (r = 0.736; p < 0.001), nighttime SBP load (r = 0.759; p < 0.001), nighttime DBP (r = 0.744; p < 0.001), nighttime DBP-SDS (r = 0.708; p < 0.001), and nighttime DBP load (r = 0.733; p < 0.001).
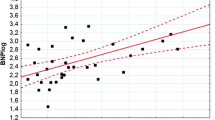
The correlations between LVMI and duration of CPD, duration of anuria, urine volume, residual GFR, hemoglobin, hematocrit, creatinine, albumin, LDL and NT-pro-BNP were poorer, with the highest correlation occurring between LVMI and pro-BNP (r = 0.583; p < 0.001; Table 3). The correlation between left ventricle end-diastolic diameter (LVEDD/body surface area) and pro-BNP was the same (r = 0.487; p = 0.001).
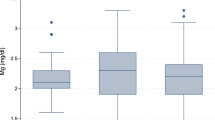
A comparison of certain variables and casual and ABPM variables according to the LVMI is shown in Table 4. All ABPM parameters, hematocrit, casual SBP-SDS, and NT-pro-BNP were significantly different in the group with LVMI ≥ 38 g/m2.7(≥95th percentile), whereas casual SBP, DBP and DBP-SDS values did not show any significant difference.
Stepwise multiple regression analysis was performed to assess whether there were significantly independent predictors of LVMI. Variables with p < 0.10 from the univariate analysis were entered into the regression model. Daytime SBP load (β = 0.652; p < 0.01) and hematocrit (β = −0.282; p < 0.01) was found to independently predict LVH. The ROC analysis for daytime SBP load and hematocrit is shown in Fig. 1. Sensitivity, specificity, positive predictive value, and negative predictive value for a daytime SBP load >15% in determining LVH was recorded as 79, 71, 87, and 59%, respectively; for a hematocrit value <31% in determining LVH, these were recorded as 76, 71, 86, and 56%, respectively. The prevalence of LVH was 95% in patients (19/20) with both SBP load >15% and hematocrit <31% compared with 22% in patients (2/9) with both SBP load <15% and hematocrit >31% (p < 0.001). The sensitivity, specificity, positive predictive value, and negative predictive values for this combination for predicting LVH were 95 (95%CI 76–99%), 78 (95%CI 45–94%), 91 (95%CI 73–98%), and 88% (95%CI 69–96%), respectively.
Discussion
The reported causes of LVH in children are similar to those in adults, with low hemoglobin, high PTH, and hypertension being the leading causes for LVH in CRF [18]. LVH is prevalent and severe even in patients on maintenance dialysis [9, 10, 18, 19]. Longitudinal studies in small pediatric series have found a correlation between LVH and BP control in chronic kidney disease (stage 2 through 4) [8] and PD or HD patients [9, 10]. Various diagnostic modalities are currently utilized for the diagnosis of target-organ damage in children with renal failure. The data reported by Sorof et al. [4] in hypertensive children suggest that ABPM may be useful in identifying children at higher risk for end organ damage at an earlier stage, i.e. LVH. However, a threshold for BP load for predicting early cardiac changes in children on dialysis has not yet been defined.
The well-known high prevalence of LVH in pediatric CPD patients was also recorded (70%) in our study. Children with normal LVM showed dominantly concentric remodeling (93%; 13/14). Thirty-three (70.2%) of our patients had concentric hypertrophy, whereas eccentric hypertrophy was absent; this suggests that chronic pressure overload was dominant among our patients and that BP control based on casual BP may be inadequate.
High BP is known to be the causal factor of concentric hypertrophy in CRF, whereas anemia and volume overload cause eccentric hypertrophy. Hypertension in PD patients can be treated by the stringent attainment of dry weight, suggesting that high BP in PD patients is secondary to volume overload. In our patients, the absence of eccentric hypertrophy and high prevalence of concentric hypertrophy suggest that chronic pressure overload may be a cause. Plasma BNP levels have also been used to predict over-hydration status in HD patients [20, 21], and BNP has also been found to be related to LVMI and the left ventricular ejection fraction in CPD patients [22]. In our series, pro-BNP levels were significantly high in the group with LVH as compared to the group without LVH. However, since concentric hypertrophy and concentric remodeling was dominant in our series (reflecting chronic pressure overload), the correlation between NT pro-BNP and LVMI was weaker and, indeed, pro-BNP was not found as an independent predictor of LVH in the multiple regression analysis.
A casual BP value ≥95th percentile is considered to be diagnostic for hypertension. Our data show that casual BP ≥95th percentile had a very low sensitivity (52%) and a negative predictive value (41%) for predicting LVH. At the present time, there is no consensus on the definition of hypertension according to BP load. Some authors have defined HT as BP load ≥25–50% [12, 23]. Sorof et al. [4] reported that the prevalence of LVH was 47% in patients with both the SBP load >50% and the 24-h SBP index >1.0; in comparison, LVH prevalence was 10% in patients without both criteria in children with hypertension (p = 0.015). The sensitivity and specificity of this combination for predicting LVH were 80 and 67%, respectively. In our series, however, the sensitivity (52%) and negative predictive value (45%) for the criteria used by Sorof were remarkably low.
Our cross-sectional study reveals a strong correlation between daytime- (r = 0.703; p = 0.001) and nighttime (r = 0.759, p = 0.001) SBP load and LVMI. The correlation coefficients were much higher than those reported by Sorof et al. [4] (r ranged between 0.33 and 0.38). We also show that daytime SBP load was an independent predictor of LVH. A systolic BP load ≥15% had a high sensitivity, specificity, and predictive value for LVH in children on CPD.
The results of a number of studies support the association between low hemoglobin and increased LVMI in both children and adults [8, 18, 19]. Two randomized studies in adults, one by Foley et al. [24] and the other by Levin et al. [25], have shown that normalization of the hemoglobin level above 10.0 g/dl does not lead to the regression of LHV [24, 25]. Another randomized study by Roger et al. [26] revealed that in chronic kidney disease (stage 3 and 4), the maintenance of hemoglobin to a level >12.0 g/dl, had similar effects on LVMI as hemoglobin at 9.0–10.0 g/dl. In our study, the hematocrit was found to be negatively correlated with LVMI. In addition, the hematocrit level was significantly lower in the group with LVH than in the group without. Stepwise multiple regression analysis revealed the hematocrit to be an independent predictor of LVH in children on CPD, with a level ≤31% having a high sensitivity, specificity, and predictive value for LVH in children on CPD. In agreement with earlier studies, we were unable to show a higher target level for hematocrit.
We are aware of the possibility of inter-observer variability in evaluating the echocardiograms. In order to minimize this effect, the echocardiography was performed by a single cardiologist from each participating center (four cardiologists from five centers). Whereas this study is limited by its cross-sectional design, our data suggest that a target level of hematocrit >31% and a daytime BP load <15% may be preventive for the progression of LVH during the follow-up of children on CPD. A prospective interventional study is warranted to test this hypothesis.
References
Berenson GS, Dalferes E Jr, Savage D, Webber LS, Bao W (1993) Ambulatory blood pressure measurements in children and young adults selected by high and low casual blood pressure levels and parental history of hypertension: the Bogalusa Heart Study. Am J Med Sci 305:374–382
Metoki H, Ohkubo T, Kikuya M, Asayama K, Obara T, Hara A, Hirose T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y (2006) Prognostic significance of night-time, early morning, and daytime blood pressures on the risk of cerebrovascular and cardiovascular mortality: the Ohasama Study. J Hypertens 24:1841–1848
Urbina E, Alpert B, Flynn J, Hayman L, Harshfield GA, Jacobson M, Mahoney L, McCrindle B, Mietus-Snyder M, Steinberger J, Daniels S, American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee (2008) Ambulatory blood pressure monitoring in children and adolescents: recommendations for standard assessment: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the council on cardiovascular disease in the young and the council for high blood pressure research. Hypertension 52:433–451
Sorof JM, Cardwell G, Franco K, Portman RJ (2002) Ambulatory blood pressure and left ventricular mass index in hypertensive children. Hypertension 39:903–908
Johnstone LM, Jones CL, Grigg LE, Wilkinson JL, Walker RG, Powell HR (1996) Left ventricular abnormalities in children, adolescents and young adults with renal disease. Kidney Int 50:998–1006
Mitsnefes MM, Kimball TR, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2003) Left ventricular mass and systolic performance in pediatric patients with chronic renal failure. Circulation 107:864–868
Matteucci MC, Wühl E, Picca S, Mastrostefano A, Rinelli G, Romano C, Rizzoni G, Mehls O, de Simone G, Schaefer F, ESCAPE Trial Group (2006) Left ventricular geometry in children with mild to moderate chronic renal insufficiency. J Am Soc Nephrol 17:218–226
Mitsnefes MM, Kimball TR, Kartal J, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2006) Progression of left ventricular hypertrophy in children with early chronic kidney disease: 2-year follow-up study. J Pediatr 149:671–675
Mitsnefes MM, Daniels SR, Schwartz SM, Khoury P, Strife CF (2001) Changes in left ventricular mass in children and adolescents during chronic dialysis. Pediatr Nephrol 16:318–323
Ulinski T, Genty J, Viau C, Tillous-Borde I, Deschênes G (2006) Reduction of left ventricular hypertrophy in children undergoing hemodialysis. Pediatr Nephrol 21:1171–1178
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114(Suppl 2):555–576
Wühl E, Witte K, Soergel M, Mehls O, Schaefer F, German Working Group on Pediatric Hypertension (2002) Distribution of 24-h ambulatory blood pressure in children: normalized reference values and role of body dimensions. J Hypertens 20:1995–2007
Cole TJ, Green PJ (1992) Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med 11:1305–1309
Devereux RB, Reichek N (1977) Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation 55:613–618
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57:450–458
de Simone G, Devereux RB, Daniels SR, Koren MJ, Meyer RA, Laragh JH (1995) Effect of growth on variability of left ventricular mass: assessment of allometric signals in adults and children and their capacity to predict cardiovascular risk. J Am Coll Cardiol 25:1056–1062
de Simone G, Daniels SR, Kimball TR, Roman MJ, Romano C, Chinali M, Galderisi M, Devereux RB (2005) Evaluation of concentric left ventricular geometry in humans: evidence for age-related systematic underestimation. Hypertension 45:64–68
Mitsnefes MM, Stablein D (2005) Hypertension in pediatric patients on long-term dialysis: a report of North American Pediatric Renal Transplant Cooperative Study (NAPRTCS). Am J Kidney Dis 45:309–315
Mitsnefes MM, Daniels SR, Schwartz SA, Khoury P, Meyer RA, Strife CF (2000) Severe left ventricular hypertrophy in pediatric dialysis: prevalence and predictors. Pediatr Nephrol 14:892–898
Soergel M, Kirschstein M, Busch C, Danne T, Gellermann J, Holl R, Krull F, Reichert H, Reusz GS, Rascher W (1997) Oscillometric twenty-four-hour ambulatory blood pressure values in healthy children and adolescents: a multicenter trial including 1141 subjects. J Pediatr 130:178–184
Nishikimi T, Futoo Y, Tamano K, Takahashi M, Suzuki T, Minami J, Honda T, Uetake S, Asakawa H, Kobayashi N, Horinaka S, Ishimitsu T, Matsuoka H (2001) Plasma brain natriuretic peptide levels in chronic hemodialysis patients: influence of coronary artery disease. Am J Kidney Dis 37:1201–1208
Osajima A, Okazaki M, Kato H, Anai H, Tsuda Y, Segawa K, Tanaka H, Tamura M, Takasugi M, Nakashima Y (2001) Clinical significance of natriuretic peptides and cyclic GMP in hemodialysis patients with coronary artery disease. Am J Nephrol 21:112–119
Lee JA, Kim DH, Yoo SJ, Oh DJ, Yu SH, Kang ET (2006) Association between serum N-terminal pro-brain natriuretic peptide concentration and left ventricular dysfunction and extracellular water in continuous ambulatory peritoneal dialysis patients. Perit Dial Int 26:360–365
Foley RN, Parfrey PS, Morgan J, Barre PE, Campbell P, Cartier P, Coyle D, Fine A, Handa P, Kingma I, Lau CY, Levin A, Mendelssohn D, Muirhead N, Murphy B, Plante RK, Posen G, Wells GA (2000) Effect of hemoglobin levels in hemodialysis patients with asymptomatic cardiomyopathy. Kidney Int 58:1325–1335
Levin A, Djurdjev O, Thompson C, Barrett B, Ethier J, Carlisle E, Barre P, Magner P, Muirhead N, Tobe S, Tam P, Wadgymar JA, Kappel J, Holland D, Pichette V, Shoker A, Soltys G, Verrelli M, Singer J (2005) Canadian randomized trial of hemoglobin maintenance to prevent or delay left ventricular mass growth in patients with CKD. Am J Kidney Dis 46:799–811
Roger SD, McMahon LP, Clarkson A, Disney A, Harris D, Hawley C, Healy H, Kerr P, Lynn K, Parnham A, Pascoe R, Voss D, Walker R, Levin A (2004) Effects of early and late intervention with epoetin alpha on left ventricular mass among patients with chronic kidney disease (stage 3 or 4): results of a randomized clinical trial. J Am Soc Nephrol 15:148–156
Acknowledgments
Dr. Duzova is supported by The Turkish Academy of Sciences (Programme to Reward Successful Young Scientists, A.D/TUBA – GEBIP/2006-6).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bircan, Z., Duzova, A., Cakar, N. et al. Predictors of left ventricular hypertrophy in children on chronic peritoneal dialysis. Pediatr Nephrol 25, 1311–1318 (2010). https://doi.org/10.1007/s00467-010-1481-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-010-1481-6