Abstract
Background
The objective of the present study was to verify whether chronic renal patients on hemodialysis (HD) with residual diuresis who were using small doses of furosemide present different levels of urinary volume and sodium excretion compared to patients with residual diuresis who do not use this drug.
Methods
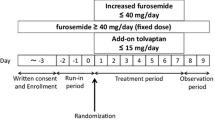
We studied 19 chronic renal patients on HD who presented any level of residual diuresis. Urine was collected during the 24-h interdialytic period, and physical examinations and blood sampling took place immediately before the start of HD. Patients were divided into two groups: the diuretic group (DG, n = 10), in which patients had been using 40 mg of furosemide for at least 3 months, and the non-diuretic group (NDG, n = 9), in which patients used no diuretics.
Results
Although both groups presented the same average glomerular filtration rate (p > 0.05) and time in dialysis (p > 0.05) the DG presented an average of twice the urinary volume in 24 h (1142 ± 184 vs. 453 ± 135 ml/24 h, respectively; p = 0.008) and double the total excreted sodium mass compared to patients in the NDG (112 ± 22.4 vs. 45.2 ± 16.0 mEq/24 h, respectively; p = 0.02).
Conclusion
The results of this study have shown that chronic use of small doses of furosemide in chronic renal patients with residual diuresis could increase urinary volume and sodium excretion compared to patients who did not use this drug.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Residual renal function (RRF) positively influences the survival time on hemodialysis (HD) of chronic renal patients, reducing the mortality risk, even when present in small quantities. RRF and, consequently, residual diuresis in HD patients can progressively decrease with dialytic treatment [1–3], and it is known that the reduction is faster in HD patients than in peritoneal dialysis (PD) patients [3–5]. Therefore, treatment aiming to maintain and minimize the loss of RRF in this group of patients is necessary [1–6].
Although the role of diuretics in managing HD patients has not yet been clearly defined [8], they can be used as a strategy to minimize RRF loss, maintaining urinary volume (UV) in HD patients [7]. Initially, this type of medication was used with the hope of preserving or even increasing RRF [7]. Recent studies show that even though UV increases after drug administration, the use of these drugs is not actually related to alterations in clearance of solutes [9].
Loop diuretics can be considered relatively safe, because they are not generally nephrotoxic and allow for better control of fluid balance, possible maximization of urine production and reduction in the need for aggressive ultrafiltration [7]. In addition, their use may be associated with lower risks of cardiac mortality [8]. Currently, it is a known fact that large doses of loop diuretics applied endovenously increase natriuresis in patients with chronic kidney disease (CKD) [6, 10, 11]; however, there are no literature studies which investigate the chronic use of small doses of furosemide in patients undergoing HD. This fact is important because it shows that in clinical practice many patients begin hemodialytic treatment using small doses of loop diuretics and once on dialysis these doses are suspended.
The object of this study was to investigate whether chronic renal patients on HD with residual diuresis who chronically use small doses of furosemide present different levels of UV and sodium excretion compared to patients with residual diuresis who do not use this drug.
Methodology
Patient selection
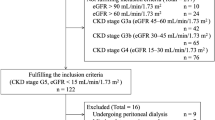
This is a transversal study, performed in patients with chronic renal insufficiency who submitted to hemodialytic treatment in a private ambulatorial HD center in 2007. The study protocol was approved by the Ethics Committee of the Federal University of Uberlandia, and a signed consent form was obtained from each patient. The selected subjects were those who, at the time of initial evaluation, had been in hemodialytic therapy for over 3 months and presented any volume of daily residual diuresis.
Having excluded anuric and diabetic patients, 63 patients were selected. Of these, 12 were excluded because they were less than 3 months on HD, 16 because they had a previous history of cardiovascular disease, 4 because of technical problems during the collection of urine samples, and 2 because they had urinary infection. Seven patients were also excluded due to renal lesion etiology, 4 due to hydronephrosis, and 3 due to polycystic renal disease. Three others were excluded because they used a dose of furosemide >40 mg per day. The remaining 19 patients were divided into 2 groups. The diuretic group (DG, n = 10) was composed of patients already taking oral furosemide for a minimum of 5 months (from 5 to 65 months). The dosage of diuretic medicine used by the patients (40 mg per day) had been previously prescribed by their own nephrologists, and suffered no interference from the researchers. The other group, the non-diuretic group (NDG, n = 9) was composed of patients who had not used diuretic medicine since the beginning of their hemodialysis treatment.
Diabetic patients were also excluded from the study due to the increased risk of urinary tract infection and non-clinically-detectable cardiovascular events. Furthermore, patients using diuretics sporadically were excluded from the study.
Treatment regimen
HD sessions were held 3 times per week, and each session lasted 4 h; all patients were treated exclusively with high-flow membranes (polysulfone).
Study protocol
After answering an identification and personal medical history questionnaire, patients went through a 24-h urine collection regimen (UV24 h). They were given containers and verbal and written orientation guidelines for the collection of all urine produced within the interdialytic period. They were told to initiate UV24 h immediately after the first morning miction and collect urine for 24 h, including from the final miction. All patients were oriented to start and finish urine collection at the same time of day [12, 13]. On the following day, a single urine sample was collected for uroculture. Immediately before the HD session, patients went through a physical examination, registration of clinical history (causes of CKD, time in dialytic treatment, medication used) as well as blood sampling. Data on interdialytic weight gain (IDWG) was also collected at this time.
Food inquest
To quantify sodium ingestion during the urine collection period, patients answered a 72-h food inquest administered by a nutritionist. The inquest was performed on three different days: HD session day, non-HD session day and weekend (no HD). Patients were advised not to change their habitual diets and to report in writing all types and quantities of food ingested. These food diaries were always received by the same nutritionist, who took notes during the patient interviews, which happened after journaling. The results presented by the nutritionist represented the average daily amount of ingested sodium. Sodium ingestion rates were calculated by the Diet PRO 5i software (Viçosa, Minas Gerais, Brazil).
Physical examination
A blood pressure (BP) assessment was performed by the researcher before starting the HD session. The BP values used in this study were expressed as the arithmetic mean of values obtained in the last three HD sessions. The IDWG was obtained just before the beginning of the session after urine collection. The interval between sessions of HD was 48 h.
Studied parameters
From the 24-h urine samples, an analysis was made of UV (UV24 h), total excreted sodium mass (UVNa), urinary sodium concentration and fractional sodium excretion (FENa) [14]. From the blood samples, an analysis was performed of sodium, urea, and creatinine. For the calculation of residual glomerular filtration rate (GFR), the average amount of residual creatinine and urea clearances [15, 16] was used, and the results were adjusted with respect to body surface. Uroculture was performed by streaking an isolated urine sample in a blood agar and eosin methylene blue plate.
Statistical analysis
Continuous variable results were expressed as mean ± standard error of mean (SEM), while the categorical variables were expressed as a proportion or percentage. The data normality analysis was performed by the D’Agostino test. For the variables presenting normal distribution, the Pearson correlation coefficient was used, and for those that did not present a normal distribution, the Spearman’s rank correlation test was used. The differences between the DG and NDG were analyzed by a Student’s t test for the variables with normal distribution and the Mann–Whitney (Wilcoxon Rank–Sum Test) for the other variables; p values of <0.05 were considered statistically significant. The statistical analysis was performed using the software Prism 5 for Windows—Version 5.02.
Results
Baseline characteristics
The patients’ general features are listed in Table 1. It can be observed that the groups did not differ with regard to gender, age, time in dialytic treatment, subjacent renal disease, use of antihypertensive drugs and BP levels. Sodium ingestion, analyzed through the food inquest, BP and IDWG presented no differences between the DG and NDG (Table 2).
Renal function and plasma parameters
Renal function parameters and urinary biochemical parameters are shown in Table 2. It was found that the DG presented higher UV24 h (p = 0.018) and higher UVNa (p = 0.045) than the NDG (Table 3). A positive correlation between UV24 h and UVNa (p < 0.0001, r = 0.95, Fig. 1) was also established. No difference was found between the DG and NDG in relation to GFR (p = 0.07) and FENa (p = 0.91). A positive and significant linear correlation was found between UV24 h and GFR (p < 0.0001, r = 0.77), as well as between UVNa and GFR (p = 0.0003, r = 0.73; Figs. 2, 3). Plasma parameters are described in Table 3. The plasma sodium level was higher in the DG (p = 0.03).
Discussion
The use of loop diuretics is one of the options during the conservative treatment of CKD patients; however, after 2 years of treatment, the use of diuretic medicine is drastically reduced [8]. There are various studies which prove that furosemide increases the excretion of sodium and water in patients with CKD on HD; however, large doses in short periods of time could lead to side-effects in some patients. In clinical practice, it was evidenced that many patients begin dialytic treatment chronically using small doses, but since there is little evidence that these are beneficial, their use is suspended when the volume of residual diuresis is reduced to minimum values. In contrast to acute use, chronic diuretic use presents an adaptive phenomenon called the diuretic braking phenomenon. According to this theory, in healthy subjects, after the first dose of furosemide, there is a considerable increase in UV followed by a higher rate of sodium excretion and lowered body weight. However, after repeated administration, there is a reduction in water and sodium loss, as well as stabilization in weight gain [17, 18]. In spite of the great importance of the adaptive phenomena related to the chronic use of furosemide, most studies investigating this drug have been performed in PD patients. Diuretics are drugs that are frequently used in clinical practice for treating edema and managing CKD patients [19]. The DOPPS study [8] verified that loop diuretics are those that are most often prescribed to HD patients, followed by thiazide diuretics and potassium-saving drugs. In our study, the use of diuretics can be characterized as chronic use, because they had been previously used for at least 5 months. Patients in the DG used small doses of furosemide (40 mg per day) and presented, on average, UV24 h more than double that of patients not on diuretic medicine (p = 0.008, Table 3). The increase in UV24 h observed in our study has also been observed in HD patients by van Olden et al. [11]; however, those patients were using high doses of furosemide acutely. Therefore, it was shown that the remaining nephrons in CKD patients clearly respond to high doses of furosemide. The dosage used in the study by van Olden [11] was excessively higher than the dose used in our study; however, the positive effects of furosemide on UV have also been found by other studies that used smaller doses of this diuretic. For example, Schimdt et al. [20], upon comparing the diuretic effects of a single dose of 240 mg of furosemide to 240 mg of muzolimine found that both drugs clearly increased UV relative to the pre-treatment period. In another study, van Olden et al. [21] found that UV increased an average of 560 ml after administration of 1000 mg/day of furosemide. The diuretic response can be quantified in many ways, including UV, total UVNa and FENa. In our study, we found that the DG presented, on average, twice as much UVNa than the NDG (p = 0.02) (Table 3). Our results are in agreement with studies that used loop diuretics acutely, such as that of Boesken et al. [10], who used the loop diuretic bumetanide and showed that after administration of this drug in HD patients, the sodium excretion rate increased 70% relative to the basal period. Van Olden et al. [11], utilizing high doses of furosemide (1000 mg/day), found that during the treatment period, UVNa increased 210% relative to the control period. Within this same study, upon comparing doses of 1000 mg and 2000 mg furosemide, it was found that higher doses presented better results. Vasavada [22], using chronic renal patients in stages 2 and 3, found that both furosemide and the loop diuretic torsemide significantly increased sodium excretion. On the other hand, the differences encountered in UV and sodium excretion rate between the DG and NDG cannot be attributed to the difference in dialytic treatment time. It is well known that RRF decreases in proportion to the dialytic treatment time; this decrease is even faster in HD patients than in PD patients [7, 23], which can be related to the inflammatory reaction of the blood contact with the surface of the dialyzer [24–26]. Nevertheless, our data has shown that the DG and NDG presented the same time in hemodialytic treatment (p = 0.86, Table 1); thus, other factors must be responsible for the greater diuresis and sodium excretion in the DG. When the 19 sample patients were analyzed, a significantly positive correlation between UV in 24 h, UVNa and GFR (p = 0.0001, r = 0.73, Fig. 2 and p = 0.0004, r = 0.73, Fig. 3, respectively) were found. Thus, greater UV and greater sodium excretion were associated with greater GFR. These correlations could explain the differences in diuresis and UVNa between both groups. Our study showed that GFR was similar in the DG and NDG (p = 0.07, Table 3); however, the mean values for GFR could have been similar due to the reduced number of patients in each group. As per van Olden et al. [21], our data has shown this correlation that patients with higher UVNa present higher GFR (p = 0.0004, r = 0.73, Fig. 3). We found that, although the groups presented the same time in dialysis, the DG presented higher UV24 h and UVNa, showing that in CKD patients with residual diuresis, small doses and long-term use of furosemide could have increased water and sodium excretion by tubular action or by the preservation of GFR. Other actions of furosemide, such as anti-inflammatory effects, have already been reported. In our study, water and sodium ingestion was not restricted, in contrast to other study protocols [20, 27]. However, through the food inquest, it was revealed that there was no difference in sodium ingestion between the DG and NDG (p = 0.443, Table 2). Our study did not verify the differences between the groups regarding IDWG (p = 0.23, Table 2). However, the lack of statistical difference could be attributed to the innate characteristics of our study (cross-sectional) in which a 24 h ingestion of water was not controlled. Nevertheless, since there was a positive significant correlation between UV and sodium excretion in a 24 h period (Table 3; Fig. 1), there is a possibility that the DG might have had less IDWG. Thus, prospective studies with a controlled liquid intake should be performed.
In contrast to what had been observed in other studies [11, 21], which acutely encountered an increase in FENa after furosemide use, our study has not encountered a statistically significant difference between FENa in the DG and NDG (p = 0.91, Table 3). In contrast to studies acutely using high doses of diuretics for short periods of time, the patients in our study had been using diuretics chronically, with small doses of furosemide for at least 5 months, and had normal sodium ingestion. The chronic use of diuretics can lead to an adaptive phenomenon (diuretic braking phenomenon), which can lead to a long-term reduction in UVNa and FENa [17].
We have also shown that there was no statistically significant difference between medium arterial pressure (MAP) (98 ± 2.8 vs. 101 ± 5.6 mmHg, respectively; p = 0.61), systolic BP (SBP) (135 ± 8.6 vs. 135 ± 8.8 mmHg, respectively; p = 0.74) and diastolic BP (DBP) (82 ± 1.8 vs. 84 ± 4.4 mmHg, respectively; p = 0.68) values in patients from the DG and NDG. These results can be explained by the fact that the patients were allowed to use antihypertensive medication during the study. In contrast to our results, Vasavada et al. [22] found that in chronic renal patients in stages 2 and 3, the use of furosemide and torsemide reduced SBP in 14 of the patients studied. With regard to plasma parameters, contrary to the studies by van Olden [11] and Schmidt [20], we found that patients who used diuretics presented higher plasma sodium concentrations compared to patients who did not use this drug (p = 0.03, Table 3). This difference in sodium concentration may be related to the volemic state of the patients. As the NDG presented lower UV24 h and UVNa, there is the possibility that this group may be hypervolemic compared to the DG.
Our study has some limitations such as the small number of patients that resulted from the selection of the patients. The in–out balance of water was not controlled in either group, due to the cross-sectional nature of the study. Despite the fact that the recommendations for the restriction of liquid ingestion were the same for both of the analyzed groups, there is the possibility that the patients ingested different volumes of water during interdialytic period.
To summarize, our data suggest that chronic renal patients on HD who make long-term use of furosemide in small doses present higher UV and UVNa than patients who do not use this drug. We suggest that prospective studies be carried out with a larger number of patients in order to identify possible mechanisms of action of long-term furosemide and its role in maintaining the RRF.
References
Shemin D, Bostom AG, Laliberty P, Dworkin LD. Residual renal function and mortality risk in hemodialysis patients. Am J Kidney Dis. 2001;38(1):85–90.
National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39 2 Suppl 1:S1–266.
Rottembourg J, Issad B, Gallego JL, Degoulet P, Aime F, Gueffaf B, Legrain M. Evolution of residual renal function in patients undergoing maintenance haemodialysis or continuous ambulatory peritoneal dialysis. Proc Eur Dial Transplant Assoc. 1983;19:397–403.
Lysaght MJ, Vonesh EF, Gotch F, Ibels L, Keen M, Lindholm B, et al. The influence of dialysis treatment modality on the decline of remaining renal function. ASAIO Trans. 1991;37(4):598–604.
Moist LM, Port FK, Orzol SM, Young EW, Ostbye T, Wolfe RA, et al. Predictors of loss of residual renal function among new dialysis patients. J Am Soc Nephrol. 2000;11(3):556–64.
Medcalf JF, Harris KP, Walls J. Role of diuretics in the preservation of residual renal function in patients on continuous ambulatory peritoneal dialysis. Kidney Int. 2001;59(3):1128–33.
Chandna SM, Farrington K. Residual renal function: considerations on its importance and preservation in dialysis patients. Semin Dial. 2004;17(3):196–201.
Bragg-Gresham JL, Fissell RB, Mason NA, Bailie GR, Gillespie BW, Wizemann V, et al. Diuretic use, residual renal function, and mortality among hemodialysis patients in the Dialysis Outcomes and Practice Pattern Study (DOPPS). Am J Kidney Dis. 2007;49(3):426–31.
Krediet RT, Douma CE, van Olden RW, Ho-dac-Pannekeet MM, Struijk DG. Augmenting solute clearance in peritoneal dialysis. Kidney Int. 1998;54(6):2218–25.
Boesken WH, Kult J. High-dose torasemide, given once daily intravenously for one week, in patients with advanced chronic renal failure. Clin Nephrol. 1997;48(1):22–8.
van Olden RW, van Meyel JJ, Gerlag PG. Acute and long-term effects of therapy with high-dose furosemide in chronic hemodialysis patients. Am J Nephrol. 1992;12(5):351–6.
Ginsberg JM, Chang BS, Matarese RA, Garella S. Use of single voided urine samples to estimate quantitative proteinuria. N Engl J Med. 1983;309(25):1543–6.
Katopodis KP, Chasiotis G, Nikolopoulos P, Seferiadis K, Siamopoulos KC. The influence of 24 h urine sampling on the evaluation of renal dysfunction. Nephrol Dial Transplant. 2007;22(11):3360–2.
Rose B. Pathophysiology of renal disease. New York: McGraw-Hill; 1987.
Caravaca F, Arrobas M, Pizarro JL, Sanchez-Casado E. Uraemic symptoms, nutritional status and renal function in pre-dialysis end-stage renal failure patients. Nephrol Dial Transplant. 2001;16(4):776–82.
van Olden RW, Krediet RT, Struijk DG, Arisz L. Measurement of residual renal function in patients treated with continuous ambulatory peritoneal dialysis. J Am Soc Nephrol. 1996;7(5):745–50.
Loon NR, Wilcox CS, Unwin RJ. Mechanism of impaired natriuretic response to furosemide during prolonged therapy. Kidney Int. 1989;36(4):682–9.
Russo D, Memoli B, Andreucci VE. The place of loop diuretics in the treatment of acute and chronic renal failure. Clin Nephrol. 1992;38(Suppl 1):S69–73.
Sanjay S, Annigeri RA, Seshadri R, Rao BS, Prakash KC, Mani MK. The comparison of the diuretic and natriuretic efficacy of continuous and bolus intravenous furosemide in patients with chronic kidney disease. Nephrology (Carlton). 2008;13(3):247–50.
Schmidt P, Loew D, Dycka J, Kopsa H, Balcke P, Zazgornik J, Deutsch E. Comparison of the effects of muzolimine and furosemide in patients with end stage renal failure on chronic dialysis. Eur J Clin Pharmacol. 1981;20(1):23–6.
van Olden RW, van Meyel JJ, Gerlag PG. Sensitivity of residual nephrons to high dose furosemide described by diuretic efficiency. Eur J Clin Pharmacol. 1995;47(6):483–8.
Vasavada N, Saha C, Agarwal R. A double-blind randomized crossover trial of two loop diuretics in chronic kidney disease. Kidney Int. 2003;64(2):632–40.
Van Stone J. The effect of dialyzer membrane and etiology of kidney disease on the preservation of residual renal function in chronic hemodialysis patients. ASAIO J. 1995;41(3):M713–6.
Hakim RM. Clinical implications of biocompatibility in blood purification membranes. Nephrol Dial Transplant. 2000;15(Suppl 2):16–20.
Pertosa G, Grandaliano G, Gesualdo L, Schena FP. Clinical relevance of cytokine production in hemodialysis. Kidney Int Suppl. 2000;76:S104–11.
Smeby LC, Wideroe TE, Balstad T, Jorstad S. Biocompatibility aspects of cellophane, cellulose acetate, polyacrylonitrile, polysulfone and polycarbonate hemodialyzers. Blood Purif. 1986;4(1–3):93–101.
Brater DC, Anderson SA, Brown-Cartwright D. Response to furosemide in chronic renal insufficiency: rationale for limited doses. Clin Pharmacol Ther. 1986;40(2):134–9.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Lemes, H.P., Araujo, S., Nascimento, D. et al. Use of small doses of furosemide in chronic kidney disease patients with residual renal function undergoing hemodialysis. Clin Exp Nephrol 15, 554–559 (2011). https://doi.org/10.1007/s10157-011-0427-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-011-0427-z