Abstract
Objective
To evaluate the safety and efficacy of revisional Roux-en-Y gastric bypass (RYGB) after adjustable gastric banding (AGB) or sleeve gastrectomy (SG) compared with primary RYGB, in regard to early and late morbidity, weight, and resolution of obesity-related comorbidities.
Methods
The group of patients undergoing revisional RYGB was matched in a 1:1 ratio with control patient who underwent a primary RYGB, based on age, gender, American Society of Anesthesiologist (ASA) score, preoperative body mass index (BMI), and diabetes mellitus. Demographics, anthropometrics, preoperative work-up, and perioperative data were retrieved.
Results
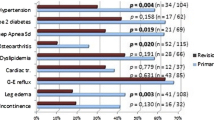
One hundred fifteen patients (16 males and 99 females) with a mean age of 45.5 ± 1.5 years underwent revisional RYGB following either LAGB in 82 patients (71.3%) or laparoscopic sleeve gastrectomy (LSG) in 33 patients (28.7%). There was no conversion and no mortality in either group. Revisional RYGB was associated with similar early (16.5 vs 15.6%, ns) and late (42.6% vs 32.2%, ns) morbidity rates with a mean follow-up of 25.3 ± 16.6 months compared to primary laparoscopic Roux-en-Y gastric bypass. The revisional RYGB group had significantly less weight loss (mean %EWL 67.4 ± 20.7 vs 72.7 ± 22.9, p = 0.023 and mean %EBMI 68.1 ± 22 vs 78.3 ± 25.7, p = 0.01) at the time of 1 year. Improvement of comorbidities including hypertension (62.5 vs 70.5%; p > 0.05), diabetes (73.7 vs 79%; p > 0.05), and obstructive sleep apnea syndrome (100 vs 97%; p > 0.05) was similar.
Conclusion
This large case-matched study suggests that conversion of SG or AGB to RYGB is feasible with early and late comparable morbidity in an accredited center; even weight results might be inferior.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery has now been established to be safe and effective for weight loss maintenance and control of obesity-related diseases as demonstrated by randomized controlled trials [1, 2]. Although laparoscopic sleeve gastrectomy (LSG) and Roux-en-Y gastric bypass (LRYGB) remain the two most commonly performed operations, a subset of patients develop either complications or recurrence of their metabolic disease over time [3] and another subset of patients may experience inadequate weight loss. According to recent published data, from 10 to 20% of patients will require revisional bariatric surgery (RBS) within 10 years, after primary treatment [4, 5]. To our knowledge, there are currently no standardized and agreed guidelines, on the optimal revisional procedure [6]. Whatever the indications, RBS remains more technically challenging than the primary surgery, due to tissue fibrosis and altered anatomy [7, 8]. According to a recent review including more than 5000 patients, revisional RYGB was associated with both increased postoperative mortality (1.3% vs 0.2%) and morbidity (29.5% vs 13.9%) rates as compared with primary RYGB [9]. Furthermore, the first recent systematic review and meta-analysis revealed that revisional RYGB has greater morbidity rate with worse weight loss when compared to primary RYGB [5].
However, there is a lack of data on common practice concerning RBS [10]. Furthermore, published retrospective case-control studies did not include clearly defined criteria for RBS, despite a recent report dividing RBS into different categories [6]. As most authors, RYGB was the commonest option used for RBS at our institute [10,11,12]. Therefore, we decide to evaluate the safety and efficacy of revisional RYGB compared with primary RYGB, in regard to early and late morbidity, weight, and resolution of obesity-related comorbidities.
Patients and Methods
Data were collected from a prospectively maintained database of morbidly obese patients undergoing laparoscopic RYGB from October 2006 to October 2017 at our French tertiary referral bariatric center. This study has been approved by the local medical ethics committee; no individual informed consent was necessary as it was a retrospective analysis. All indications for primary and revisional bariatric surgeries were endorsed in an interdisciplinary consensus meeting. Bariatric surgery was offered to patients in accordance with French guidelines for bariatric surgery. Only patients with a follow-up longer than 12 months after revisional LRYGB were considered for the analysis.
Matching Process
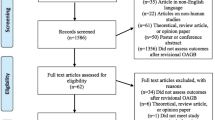
The full matching process is depicted in Fig. 1. For this study, all patients undergoing revisional LRYGB after a failed primary bariatric surgery were included for analysis. The group of patients undergoing revisional LRYGB was matched in a 1:1 ratio with control patients who underwent a primary LRYGB. Patients were matched based on age, gender, ASA score, preoperative body mass index (BMI), and diabetes mellitus. The investigators (AV and JJP) were blinded to the primary end points in both groups during manual matching to reduce bias.
Data Collection
The relevant information for each patient were prospectively collected and included demographics characteristics (i.e., comorbidities (diabetes, hypertension, obstructive sleep apnea syndrome)), type of prior bariatric procedure, time from prior bariatric procedures to revisional LRYGB, and indication for conversion. For both groups, operative time, early and late postoperative complications, and length of hospital stay were recorded. Early complications were defined as those (i.e., readmission rate or unexpected events) that occurred until postoperative day 90 or at any time during the primary hospital stay. Surgical postoperative complications included reoperation, anastomotic leakage (on computed tomography or during reoperation), bleeding (requiring blood transfusion or reoperation), and intra-abdominal abscess (requiring antibiotics or surgical drainage). Infectious complications included pneumonia, urinary tract infection, and wound infection which were scored. All the complications were stratified according to the Dindo-Clavien scale [13]. Long-term complications were defined as those occurring during the follow-up (which was at least 12 months), such as reoperation or readmission due to internal hernia or incisional hernia as well as cholecystectomy. Outcomes in weight control were evaluated with BMI, percentage of excess body weight loss (%EWL), percentage of excess BMI loss (EBMIL) after conversion. EBMIL was calculated from the initial BMI (global EBMIL) and from BMI before conversion (additional EBMIL). EWL after conversion was calculated from the initial weight (global EWL) and from weight loss before conversion (additional EWL).
Surgical Procedures
The revision from laparoscopic adjustable gastric band to RYGB was done in two steps: band removal followed by RYGB after an interval of at least 6 months, in order to allow resolution of fibrosis and scarring. The revision from LSG to RYGB was a single-stage procedure of which a surgical technique was previously reported [11].
Outcomes
Primary outcomes of this study were early and late postoperative complications. The secondary outcomes included additional weight loss and resolution of any known obesity-related comorbidities. Postoperative comorbidities were assessed as persisting (the same medications as before surgery), improved (reduction in medications), or resolved (no medications needed).
Follow-up
All patients were assessed as part of a routine follow-up program in the outpatient clinic and were seen on a regular schedule 3, 6, 9, 12, 18, and 24 months postoperatively. Thereafter, patients were seen annually. Patients lost to follow-up were contacted several times by e-mail or phone.
Statistical Analysis
Qualitative variables were described by number (percentages) and quantitative variables were described by means (standard deviation), as appropriate. The demographic data of the two groups were compared to demonstrate adequate matching. Comparison of variables referring to baseline characteristics not used for the matching process between the two groups was undertaken using chi-square or Fisher’s exact test as indicated, for categorical data. Continuous variables referring to outcomes were compared between the two groups by Student’s paired t test, to account for the sampling design. Statistical analysis was performed with SAS software V9.4 (SAS Institute, NC, Cary).
Results
Data Collection
One thousand fifty-one consecutive patients underwent LRYGB in our center during the study period (Fig. 1). Among these patients, 144 (13.7%) have a RBS. Our matching process failed to match 29 case patients. The study’s cohort included 115 patients in each group. The revisional LRYGB group consists of 115 patients (16 males and 99 females) with a mean age of 45.5± 1.5 years. The primary bariatric procedure was LAGB in 82 patients (71.3%) and LSG in 33 patients (28.7%). There were no differences in demographic characteristics between the groups of primary and revisional LRYGB groups regarding age, gender, preoperative BMI, and obesity-associated comorbidities (Table 1). The indications for RBS included inadequate weight loss or weight regain in 88 patient (76.5%), GERD in 16 patients (13.9%), dysphagia in one patient (0.9%), band complication in one patient (0.9%), and miscellaneous in 9 patients (7.8%). The time between primary bariatric procedure and revisional surgery ranged from 12 to 120 months with a median of 33 months.
Surgical Outcomes
There was no mortality in either group. Revisional LRYGB increased the mean operative time (155.2 ± 42.9 vs 145.2 ± 45.4 min) as compared with the primary LRYGB mean, but the difference was not significant (p = 0.0899) (Table 2). All procedures were performed laparoscopically without conversion. The number and type of complications are shown in Table 2. Thirty-seven patients had at least one complication within 90 days after surgery, 19 patients (16.5%) in the revisional LRYGB group and 18 patients (15.6%) in the primary LRYGB group (p = 1). There was no statistical difference in 90-day major or minor complication rates according to the Dindo-Clavien classification between the two groups (Table 2). Thirteen patients required reoperation, 6 patients (5.2%) in the revisional LRYGB group and 7 patients (6%) in the primary LRYGB group (p = 1). Indications for reoperation included hemorrhage (n = 4), leakage from the gastrojejunal anastomosis (n = 2) or from the vertical staple line of the gastric pouch (n = 1), small bowel injury (n = 1), gastrojejunal stenosis (n = 1), small bowel obstruction (n = 3), and miscellaneous (n = 1). All those patients had postoperative outcome uneventful. The duration of hospitalization was significantly greater for the revisional group (7.3 ± 5.4 vs 5.7 ± 2.2 days; p = 0.004).
With a mean follow-up of 25.3 ± 16.6 months, 86 patients experienced late postoperative complications, 49 patients (42.6%) in the revisional LRYGB group and 37 patients (32.2%) in the primary LRYGB group (p = 0.25). Thirty-nine patients required additional surgery for correction of symptomatic internal hernia (n = 9), incisional hernia (n = 17), gall stones (n = 16), and small bowel obstruction (n = 5).
Weight Loss and Comorbidities (Table 3)
The follow-up rate was 100% at 1 year. In both groups, effective body weight reduction was observed but the efficacy decreased over time. No statistical difference in %EWL (57 ± 20 vs 54 ± 20%, ns) and in %EBMI (61 ± 22 vs 57 ± 19%, ns) was observed between the two groups at 6-month follow-up. The weight loss was more pronounced at 1 year, in favor of the primary LRYGB, reaching a statistically significant difference (mean %EWL in the revisional group was 64.7 ± 20.7 and in the primary group 72.7 ± 22.9, p = 0.023). The 1-year %EBMI was significantly higher in the primary LRYGB group than that in the revisional LRYGB group (78.3 ± 25.7 vs 68.1 ± 22; p = 0.01). Comorbidities including hypertension (62.5 vs 70.5%; p > 0.05), diabetes (73.7 vs 79%; p > 0.05), and OSAS (100 vs 97%; p > 0.05) did not reveal significant improvements after the revisional procedure.
Discussion
The main finding of this case-matched study is that revision from LAGB or LSG to LRYGB in a tertiary center with long experience in redo surgery is safe and effective. However, both %EWL and %EBMI are significantly lower after revisional LRYGB when compared to those of primary LRYGB at 1 year.
With the exponential increase in the number of bariatric procedures performed yearly worldwide [14], bariatric surgeons will be confronted with a growing number of patients experiencing either weight loss failure or weight regain as well as complications or side effects linked to primary bariatric procedures. Moreover, one of the causes of it is the SG which is the most performed procedure in the world currently, at a great distance from RYGB and many other models of malabsorptive techniques with greater metabolic power and long-term efficacy. This finding leads to a significant increase in number of patients undergoing RBS. In the USA, the rate has nearly doubled in the last years [4]. This increased incidence of RBS raises concern about safety and outcome of these technically challenging procedures. Although there is a paucity of standardized practices concerning RBS, a recent survey of bariatric surgeons showed that RYGB was the commonest option used for RBS after either gastric banding or sleeve gastrectomy [10]. However, revisional RYGB is considered technically more difficult and known to carry a higher risk in comparison with primary procedure [10]. In our department, we should not perform RBS in the same time of removing gastric band, even if some teams do it with good results on safety and effectiveness [15]. In our study, including more than 100 consecutive patients with a revisional RYGB, no mortality was observed. Furthermore, operative time in RBS was similar to that of primary RYGB without conversion in laparotomy. These findings may be explained, because in our department RBS was exclusively performed by advanced bariatric surgeons (YLR, TG, NC). It is well known that surgeon experience and institutional volume play a significant role in bariatric outcomes [16, 17]. In our study, the overall early postoperative complication rate was comparable after revisional and primary RYGB (16.5% vs 15.6%, ns). This finding differs from the results published by a data registry which included 39,567 patients with a primary RYGB and 3718 patients with a revisional RYGB [18]. In this study, RBS was significantly associated in this study with an increased incidence of at least one complication requiring either reoperation (3.9 vs 2.4%, p < 0.05) or intervention within 30 days (4 vs 2.7%, p < 0.05), as compared with PBS. RBS was also significantly associated with an increased 30-day readmission rate (8.3 vs 6.3%, p < 0.05). In our study, we did not find any difference between revisional and primary groups whatever the severity of complications, according to the Dindo-Clavien classification [13]. On the contrary, a recent systematic review and meta-analysis [5] revealed that morbidity including anastomotic leakage was significantly higher in patients undergoing revisional RYGB. A significant greater risk of anastomotic leakage still remains in the case-matched subgroup, while the significant risk disappears in the case of the overall morbidity rate [5].
Most of the studies reporting postoperative outcomes of revisional RYGB consist of small comparative case series [7, 19,20,21,22,23,24,25,26,27,28] of which only eight were case-matched studies. The largest case-matched survey comparing 1224 revisional RYGB with 3612 primary RYGB did not report any outcomes in terms of postoperative complications [12]. Furthermore, more than 100 patients were only included in two studies and laparoscopic procedures were only included in five studies (Table 4). In our study, we have evaluated long-term postoperative complications and found a greater rate after revisional procedures (42.6 vs 32.2%, ns). This analysis is underpowered to detect significant difference in the presence of complications and this is a limit of this study. This finding is comparable to the study published by Zhang et al. [18]. Although RBS increased long-term postoperative morbidity (23 vs 13.1%, ns) without significant difference, these results were distorted because they included laparoscopic and open procedures [19].
We finally found that RBS was associated with significant worse weight loss effect (%EWL and %EBMIL) at 1 year when compared to the primary procedure. Difference disappears at 2 and 3 years of follow-up and might be explained by lost to follow-up (about 45% at 2 years and 60% at 3 years). This result is in accordance with the overwhelming majority of studies published. This finding is also comparable with the result observed in the largest survey in Sweden [12]. Furthermore, there were no differences in the postoperative effect on the resolution of obesity-related complications, such as diabetes mellitus, hypertension, or OSAS. These results must be interpreted with caution because a minority of case-matched studies included data from > 100 patients. Furthermore, the RYGB is a mixed technique that is not very restrictive and very scarcely malabsorptive. Any restrictive primary procedure has a high chance of failing to lose weight in the medium or long term, but in turn it generates very deep metabolic resistances in the human body, which the RYGB has not proven to be able to overcome even in the short term. The concept of revision surgery requires a great mental exercise to understand that only with techniques that produce intense metabolic effects can we succeed in the medium- and long-term surgical results. Therefore, RYGB should not be the only technique of revision surgery, but OAGB or DS procedures will have a place soon with excellent mid-term and long-term results [29,30,31].
While primary RYGB was associated with a higher improvement of comorbidity in two studies [20, 32], Thereaux et al. have recently found similar rates of remission at 5 years [33].
The present study has several limitations: The study design was retrospective but relevant information for each patient was prospectively collected in our tertiary center of obesity management. We have also used a case-matched cohort study in order to control and reduce the effect of confounding factors. Our matching process failed to match 29 patients that reflect the various characteristics of the whole cohort. Moreover, the case group was heterogeneous concerning the initial procedures, indications for revisional surgery, and time interval between the previous and the revisional procedures. However, half of case-matched studies published have included various primary bariatric procedures and we have also compared postoperative outcomes after each surgical procedure (data not shown). Finally, the average duration of follow-up is limited to 24 months.
Although, RBS is a multifactorious challenge, this large case-matched study suggests that conversion of SG or AGB to RYGB is feasible with early and late comparable morbidity in an accredited center. This information is useful for patients undergoing RBS. Furthermore, revisional RYGB results in a lower excess weight loss rate at 12 months, while rates of improvement or resolution of obesity-related comorbidities seem comparable. In an era of RBS, further prospective trials are needed to determine not only the preferred surgical strategy (i.e., mini gastric bypass, duodenal switch, and single-anastomosis duodeno-ileal (SADI) bypass) according to the indications, but also their real impact on the expectancy quality of life of the patients.
References
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric–metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386:964–73.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes — 3-year outcomes. N Engl J Med. 2014;370:2002–13.
Radtka JF, Puleo FJ, Wang L, et al. Revisional bariatric surgery: who, what, where, and when? Surg Obes Relat Dis. 2010;6:635–42.
Ponce J, DeMaria EJ, Nguyen NT, et al. American Society for Metabolic and Bariatric Surgery estimation of bariatric surgery procedures in 2015 and surgeon workforce in the United States. Surg Obes Relat Dis. 2016;12:1637–9.
Pędziwiatr M, Małczak P, Wierdak M, et al. Revisional gastric bypass is inferior to primary gastric bypass in terms of short- and long-term outcomes—systematic review and meta-analysis. Obes Surg. 2018;28:2083–91.
Brethauer SA, Kothari S, Sudan R, et al. Systematic review on reoperative bariatric surgery. Surg Obes Relat Dis. 2014;10:952–72.
Samakar K, McKenzie TJ, Kaberna J, et al. Safety and efficacy of single-stage conversion of failed adjustable gastric band to laparoscopic Roux-en-Y gastric bypass: a case–control study. Surg Endosc. 2016;30:5453–8.
van Wezenbeek MR, van Oudheusden TR, de Zoete JPJGM, et al. Conversion to gastric bypass after either failed gastric band or failed sleeve gastrectomy. Obes Surg. 2017;27:83–9.
Mahawar KK, Graham Y, Carr WRJ, et al. Revisional Roux-en-Y gastric bypass and sleeve gastrectomy: a systematic review of comparative outcomes with respective primary procedures. Obes Surg. 2015;25:1271–80.
Mahawar KK, Nimeri A, Adamo M, Borg C-M, Singhal R, Khan O, et al. Practices concerning revisional bariatric surgery: a survey of 460 surgeons. Obes Surg. 2018 [cited 2018 Aug 21]; Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s11695-018-3226-8
Gautier T, Sarcher T, Contival N, et al. Indications and mid-term results of conversion from sleeve gastrectomy to Roux-en-Y gastric bypass. Obes Surg. 2013;23:212–5.
Axer S, Szabo E, Näslund I. Weight loss and alterations in co-morbidities after revisional gastric bypass: a case-matched study from the Scandinavian Obesity Surgery Registry. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2017;13:796–800.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25:1822–32.
Obesity Surgery Working Group, Competence Network Obesity, Stroh C, Weiner R, et al. One versus two-step Roux-en-Y gastric bypass after gastric banding—data analysis of the German Bariatric Surgery Registry. Obes Surg. 2015;25:755–62.
Torrente JE, Cooney RN, Rogers AM, et al. Importance of hospital versus surgeon volume in predicting outcomes for gastric bypass procedures. Surg Obes Relat Dis. 2013;9:247–52.
Fournier P, Gero D, Dayer-Jankechova A, et al. Laparoscopic Roux-en-Y gastric bypass for failed gastric banding: outcomes in 642 patients. Surg Obes Relat Dis. 2016;12:231–9.
El Chaar M, Stoltzfus J, Melitics M, et al. 30-day outcomes of revisional bariatric stapling procedures: first report based on MBSAQIP data registry. Obes Surg. 2018;28:2233–40.
Zhang L, Tan WH, Chang R, et al. Perioperative risk and complications of revisional bariatric surgery compared to primary Roux-en-Y gastric bypass. Surg Endosc. 2015;29:1316–20.
Mohos E, Jánó Z, Richter D, et al. Quality of life, weight loss and improvement of co-morbidities after primary and revisional laparoscopic Roux Y gastric bypass procedure—comparative match pair study. Obes Surg. 2014;24:2048–54.
Martin MJ, Mullenix PS, Steele SR, et al. A case-match analysis of failed prior bariatric procedures converted to resectional gastric bypass. Am J Surg. 2004;187:666–71.
Zingg U, McQuinn A, DiValentino D, et al. Revisional vs. primary Roux-en-Y gastric bypass--a case-matched analysis: less weight loss in revisions. Obes Surg. 2010;20:1627–32.
Mor A, Keenan E, Portenier D, et al. Case-matched analysis comparing outcomes of revisional versus primary laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2013;27:548–52.
Delko T, Köstler T, Peev M, et al. Revisional versus primary Roux-en-Y gastric bypass: a case-matched analysis. Surg Endosc. 2014;28:552–8.
Malinka T, Zerkowski J, Katharina I, et al. Three-year outcomes of revisional laparoscopic gastric bypass after failed laparoscopic sleeve gastrectomy: a case-matched analysis. Obes Surg. 2017;27:2324–30.
Chowbey PK, Soni V, Kantharia NS, et al. Laparoscopic Roux-en-Y gastric bypass: outcomes of a case-matched comparison of primary versus revisional surgery. J Minim Access Surg. 2018;14:52–7.
Al-Kurd A, Grinbaum R, Abubeih A, et al. Conversion of laparoscopic adjustable gastric banding to gastric bypass: a comparison to primary gastric bypass. Obes Surg. 2018;28:1519–25.
Slegtenhorst BR, van der Harst E, Demirkiran A, et al. Effect of primary versus revisional Roux-en-Y gastric bypass: inferior weight loss of revisional surgery after gastric banding. Surg Obes Relat Dis. 2013;9:253–8.
Ruiz-Tovar J, Carbajo MA, Jimenez JM, et al. Long-term follow-up after sleeve gastrectomy versus Roux-en-Y gastric bypass versus one-anastomosis gastric bypass: a prospective randomized comparative study of weight loss and remission of comorbidities. Surg Endosc. 2018; [cited 2018 Sep 14]; Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s00464-018-6307-9
Pujol Rafols J, Al Abbas AI, Devriendt S, et al. Roux-en-Y gastric bypass, sleeve gastrectomy, or one anastomosis gastric bypass as rescue therapy after failed adjustable gastric banding: a multicenter comparative study. Surg Obes Relat Dis. 2018; [cited 2018 Sep 24]; Available from: https://linkinghub.elsevier.com/retrieve/pii/S1550728918304945
Dijkhorst PJ, Boerboom AB, Janssen IMC, et al. Failed sleeve gastrectomy: single anastomosis duodenoileal bypass or Roux-en-y gastric bypass? A multicenter cohort study. Obes Surg. 2018; [cited 2018 Sep 24]; Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s11695-018-3429-z
Navez J, Dardamanis D, Thissen J-P, et al. Laparoscopic Roux-en-Y gastric bypass for morbid obesity: comparison of primary versus revisional bypass by using the BAROS score. Obes Surg. 2015;25:812–7.
Thereaux J, Corigliano N, Poitou C, et al. Five-year weight loss in primary gastric bypass and revisional gastric bypass for failed adjustable gastric banding: results of a case-matched study. Surg Obes Relat Dis. 2015;11:19–25.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study has been approved by the local medical ethics committee; no individual informed consent was necessary as it was a retrospective analysis. All indications for primary and revisional bariatric surgeries were endorsed in an interdisciplinary consensus meeting. Bariatric surgery was offered to patients in accordance with French guidelines for bariatric surgery.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Vallois, A., Menahem, B., Le Roux, Y. et al. Revisional Roux-en-Y Gastric Bypass: a Safe Surgical Opportunity? Results of a Case-Matched Study. OBES SURG 29, 903–910 (2019). https://doi.org/10.1007/s11695-018-3606-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3606-0