Abstract
Background
Bariatric surgery outcomes have been examined in Germany since January 1, 2005. All data were registered prospectively in cooperation with the Institute of Quality Assurance in Surgery at the Otto-von-Guericke University Magdeburg.
Methods
The data were collected from an online data bank. Data collection began in 2005 for gastric banding (GB) and Roux-en-Y gastric bypass (RYGB) results. In addition to primary bariatric operations, data regarding the complications of revision procedures and redo operations were analyzed. Participation in the quality assurance study was required for all certified centers in Germany.
Results
RYGBs are a popular redo operation after failed gastric banding. In the German Bariatric Surgery Registry (GBSR), we analyzed data from 263 RYGB operations that used a one-step approach after GB and 116 operations that used a two-step approach. The leakage rates for primary RYGB decreased to 1.8 %. The incidence of leakage after a one-step RYGB after GB was lower (1.9 %) than after the two-step procedure (2.6 %).
Conclusion
RYGBs are popular procedures after failed GB in Germany. The multivariable analysis for overall intraoperative complications revealed a significant difference between the two-step and the one-step procedure. In an unadjusted and multivariate assessment, the one-step procedure had statistically lower general postoperative complications than the two-step approach. Therefore, we suggest performing band removal and RYGB as a one-step procedure. Further analysis is necessary to evaluate the risk factors for the one-step procedure. Follow-up investigations must be performed to determine whether RYGB is an effective and safe option after GB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is one of the greatest health challenges in the twenty-first century. According to the data from the International Association for the Study of Obesity (IASO), Germany ranks first for the prevalence of obesity for both genders [1]. The Federal Office of Statistics revealed that in 2011, 18.9 % of men and 22.5 % of women were overweight [2]. Life expectancy is markedly shortened by obesity, particularly in young obese persons.
In contrast with bariatric surgery, nonsurgical treatment is ineffective for sustainable weight loss and the reduction of associated comorbidities.
From the late 1990s until approximately 2005, laparoscopic adjustable gastric banding (LAGB) gained popularity due to its relatively low complexity and adjustability in combination with a low perioperative morbidity (1–5 %) and mortality rate (0–0.05 %). GB has good results, but it also has several limitations [3]. The rate of performed GB operations worldwide was 17.8 % in 2011 [4]. Band related complications, such as esophageal dilatation, gastric necrosis, band slippage, and band and pouch dilatation, occur in 8–60 % of all patients [3]. Furthermore, a growing number of patients have inadequate weight loss or weight regain after a successful initial weight loss.
There are different surgical options to treat late complications or inadequate weight loss. RYGB and SG are more frequently performed as a rescue operation after failed GB.
The aim of the present study was to compare the data available from the German Bariatric Surgery Registry (GBSR) for the primary RYGB procedure with GB conversion to RYGB as a one- or two-step procedure.
Method
The data from the GBSR were prospectively registered in an online database since January 1, 2005, at the Institute of Quality Assurance in Surgical Medicine of the Otto-von-Guericke University Magdeburg [5]. This paper evaluates the complication data of primary RYGB in comparison with the complication data of conversion to secondary RYGB after GB between 2005 and 2012. The aspects studied include basic demographics, operation parameters, perioperative complications and mortality. These parameters were used to compare primary RYGB and secondary RYGB as a one- or two-step procedure after GB. For the two-step procedure, the complications of GB removal and RYGB implantation are summarized. These data were then compared with literature results.
Statistical Analysis
A descriptive statistical analysis was performed and the absolute and relative frequencies for nominal data and the mean, standard deviation, and minimum and maximum values for continuous variables are presented. The median is presented for continuous variables that are highly variable. All calculations were performed by StatConsult GmbH using SAS® 9.2 (SAS Institute, Cary, NC, USA) with a type 1 error rate of α = 0.05. All tests were deliberately performed to the full level of significance. The baseline data were compared using a robust t test for continuous variables (weight, BMI, and age) or a χ 2 test for nominal data (presence of comorbidities and gender). For rare nominal events (complications), the Fisher’s exact test was used for statistical comparisons. To detect demographic differences between the one-step and two-step procedures for age and BMI, tests of equivalence with clinically relevant margins of 2 years and 2 kg/m2, respectively, were applied. Furthermore, a logistic regression analysis was performed for multivariable factors to estimate the corresponding odds ratios for complications, which are provided with their 95 % confidence intervals.
Results
Within the study period (from 2005 until 2012), 10,330 patients underwent RYGB surgery as a primary procedure for morbid obesity. There was an annual increase in the number of RYGB surgeries performed in Germany within the study period. The number of primary RYGB surgeries per year increased from 249 in 2005 to 2733 in 2012.
Basic Demographics
There were 402 RYGB operations performed as redo procedures after GB surgery between 2005 and 2012. In 263 cases, band removal was performed simultaneously with the RYGB. The operation was performed in two different operations in 139 cases. Of these cases, 116 were included in this analysis as a planned two-step procedure. The condition for a planned two-step procedure was that the RYGB operation was performed within 1 year after GB removal. The median time interval between both operations was 74 days (range 13 to 289 days).
In 263 patients, band removal and RYGB were performed as a one-step operation. For this population, the same proportion of women (77.6 %) underwent this surgery compared with the primary procedure. These 263 patients received operations in 42 different hospitals in Germany.
The mean age of these patients was 44.5 ± 9.8 years (20–70 years) and the mean BMI was 43.9 ± 8.1 kg/m2 (range 24.8–73.5 kg/m2).
GB removal and RYGB was performed as a two-step procedure in 116 patients in 28 hospitals. In 16 hospitals one and two-step band removal and RYGB were performed. In this population, 83.6 % of the patients were female. The mean age at the time of the redo surgery was 45.5 ± 11.3 years (16–77 years) and 45.2 years ± 11.4 (16–77 years) at GB removal. Patients undergoing the one-step procedure were younger than patients undergoing the two-step procedure (not statistically significant, p = 0.552). The BMI of patients undergoing the two-step band removal and RYGB was 43.5 ± 7.7 kg/m2 (range: 23.2–71.8 kg/m2). This was not statistically significantly lower than for the one-step procedure (p = 0.668). The demographic data from all groups are shown in Table 1.
For one-step and two-step procedures in the unadjusted analysis, gender, BMI, and age were not risk factors for leaks.
Comorbidities
Comorbidities were recorded for all patients in this study. In addition to the fact that all patients had already undergone a GB at the time of the redo surgery, 76.8 % of one-step patients and 79.3 % of two-step patients suffered from comorbidities at the time of GB removal (80.2 % at the time of RYGB). An unadjusted comorbidity influence for the leakage rate was not evaluated for one or two-step band removal and RYGB.
Operation Data
Since 2005, the data from GB procedures have been recorded in the German Bariatric Surgery Registry (GBSR). The GB primary procedure is currently performed in 95 participating hospitals. Overall, each hospital performs between 1 and 145 procedures per year. From up to 7 years of data collection, the total number of GB surgeries performed ranged from 1 to 330 per hospital. The data for RYGBs have been recorded in the GBSR since 2005.
The mean operation time for a one-step band removal and RYGB was statistically longer than the operation time for the two-step patients (163 ± 64 vs. 144 ± 60 min; p = 0.006). This is a clinically relevant difference by a margin of 10 min. The mean operation time for GB removal in the two-step procedure was 66 min (range 16–257 min).
The operations were performed using a laparoscopic approach in 99.1 % of the two-step procedures and 90.7 % of the one-step procedures. The conversion rates from a laparoscopic to open procedure were not significantly different between the one- and two-step approaches (1.9 vs. 0 %; p = 0.329).
Compared with the mean operation time for RYGB as a primary approach (116.5 ± 58 min), the operation time for a one- or two-step band removal and RYGB is significantly longer (p < 0.001), which is the same as the clinically relevant 10 min margin. The conversion rate increased from 0.7 % for primary RYGB to 1.9 % for a one-step revision of GB to RYGB (p = 0.046).
Leakage of the staple line is a complication of RYGB; we observed a significant difference in using staplers for all one-step operations (85.7 %) versus two-step operations (96.5 %) (p = 0.002). Staple line buttresses were used in 13.5 % of the one-step operations and in 16.7 % of the two-step procedures. The operative data are shown in Table 2.
Perioperative Complications
Intraoperative Complication Rates
Intraoperative complication rates were higher in the combined two-step redo operations than in the one-step operations (7.8 vs. 3.0 %; p = 0.057). The intraoperative complication rate for the second operation (RYGB) in two-step patients amounts to 4.3 %. In both approaches, the intraoperative complications were spleen and vessel injuries and gastric perforations. The multivariable analysis for overall intraoperative complications revealed a significant difference between the two-step procedure (OR = 3.0, 95 % confidence interval (CI): 1.1–8.2; p = 0.032) and the one-step procedure (Table 3). The risk of intraoperative complications is also increased by a higher number of comorbidities (OR = 1.3 [95 % CI: 1.0–1.6]).
General Postoperative Complication Rates
The overall general postoperative complication rate was 14.7 % for two-step operations (individual rate for RYGB was 13.8 %). The majority of complications for two-step procedures were pulmonary complications and urinary infections. There were no general complications described. The general complication rate for the one-step procedure was 5.7 % with a dominance of pulmonary and cardiac complications, fever, and urinary infections. In an unadjusted assessment, the one-step procedure had statistically lower general postoperative complications than the redo of GB into RYGB in two operations (p = 0.008). The multivariable analysis confirmed this finding with an OR of 3.0 (95 % CI: 1.4–6.3; p = 0.004).
Specific Postoperative Complication Rates
There was no relevant difference in the total incidence of surgery-specific postoperative complications between one- and two-step band removal and RYGB (10.3 vs. 12.1 %, p = 0.594). The individual rate of specific complications after RYGB in the two-step population was 11.2 %. In the multivariable analysis, no significant factor for specific complication rates could be detected. Patients who underwent band removal and RYGB in one operation had the same risk of leakage (leakage rate of 1.9 vs. 2.6 % in two-step operations (p = 1.000)). The data are shown in Table 4.
Mortality
For operations between January 1, 2005, and December 31, 2012, the mortality rate was 0.7 % (n = 1) for the two-step procedure. After the one-step operation, there was no mortality observed. Mortality for patients with leakage was zero for both the one- and two-step approaches.
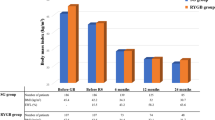
Follow-Up
The weight loss for the patients with band removal and RYGB was not lower than for the patients with primary RYGB. The partial and complete remission rates for comorbidities were higher for patients with primary RYGB than for patients with a redo operation. The follow-up data are shown in Table 5.
Discussion
Since January 1, 2005, primary and repeat bariatric procedures were recorded within the framework of a quality assurance study for the surgical treatment of obesity by the Institute for Quality Assurance in Surgical Medicine at the Otto-von-Guericke University Magdeburg with the aim of improving the quality of care [5]. Data were collected from an online database. A plausibility analysis is performed by the project organization, but there is not complete control of the origin of the patient data. These may be a bias of the GBSR, but this bias exists for all quality control studies worldwide. In a retrospective analysis, the risk of bias should always be considered. A comparison was made between patients with revisional RYGB as a one- or a two-step procedure or primary RYGB. For the revisional RYGB, the reasons for band removal and reoperation were not separately discussed and analyzed.
GB is one of the most frequently performed bariatric operations worldwide. Due to experiences with GB and its long-term effects, the operation rate in Europe and worldwide has decreased since 2008.
Meta-analysis data showed no relevant long-term differences in excess weight loss when comparing GB and RYGB [3]. The high frequency of adverse events in the perigastric area could be reduced with the introduction of the pars flaccida technique and new soft bands. These results show that GB is still a safe and effective long-term treatment for obesity.
Long-term complications, insufficient weight loss, or failed amelioration of comorbidities are indications for redo operations after GB. Because RYGB is an effective procedure in Germany, the conversion of GB to RYGB is an interesting option for redo surgeries.
GBSR data from 2005 to 2012 have shown an increasing number of reoperations after GB, particularly RYGB after a prior GB (Table 6).
The decision for one or two-step band removal and RYGB depends on the experience of the center, cost factors, and risk factors for the patients.
This redo operation can be performed either as a one-step or two-step operation. The data from the GBSR show that the one-step procedure is the most common procedure performed in Germany. The data also show a higher incidence of specific complications, particularly leakage at the gastrojejunostomy, after a two-step procedure. Bias of our investigations is that there was no evaluation of the surgeon’s experience performing one- or two-step operations as well as the missing analysis of the reasons for band removal. A higher incidence of leakage has to be discussed for more inflamed cases or band removals in the fact of band erosion.
Previous studies support these evaluations. Studies from Cadiere et al. 2011 detected a lower incidence of leakage at the GJA after primary RYGB operation (4.4 %) than after RYGB as a secondary procedure (12 %) [6]. A bias of the study is the inclusion of patients after vertical banded gastroplasty and GB. The leakage rate of patients with two-step band removal and RYGB was 8.8% in this study [6].
Because staple line insufficiency is a problem after RYGB, leading to sepsis and peritonitis, we analyzed the data from the GBSR to determine if one- or two-step operations influence leakage incidence. Our investigation revealed a slightly higher incidence of leaks for the two-step procedures (1.9 vs. 2.6 %).
A literature review on this topic is difficult because most published reports include a mix of patients after GB and vertical banded gastroplasty (VBG) or a mix of reoperations as one- or two-step procedures without any comparison of both intervention types (Table 7) [6–11].
The overall reported leakage rates after GB and RYGB ranged from 0.9 to 8.8 % without any exact differentiation between the one or two-step approaches [6, 10]. Only a few studies reported complication rates, specifically leakage, for one- and two-step band removal and RYGB. These studies do not report whether there is a difference in leakage incidence for a two-step RYGB after band removal [7, 8]. Only Apers et al. evaluated the leakage rate (6.0 % at the gastrojejunal junction) and did not observe any difference between the one or two-step procedures [9]. Data from the GBSR suggest a lower leakage rate for the one-step procedure, but there may be a bias due to the low number of patients. The leakage rate for one-step operations compared with primary RYGB is an important point for further discussions (1.9 vs. 1.8 %; p = 0.817). These data show that the one-step reoperation has the same incidence of leakage as primary RYGB.
Examinations have shown that GB leads to chronic inflammation of the gastric wall in the tissue under the band [12]. Data comparing the leakage rates of GB pars flaccida and perigastric techniques are not available in the literature. The GBSR could not be used to investigate this issue because many patients underwent GB operations before 2005 in different hospitals.
The operation time for one-step band removal and RYGB is longer than for the RYGB in the two-step procedure alone, but with the addition of band removal, the operation time is longer. The comparison of operation times between one- and two-step operations with the additional band removal includes the bias that the difference may be caused by double times for trocar placement, double suturing of the skin, and other factors.
Data from the GBSR and most publications show that overall morbidity is significantly higher in patients that undergo RYGB after primary gastric banding compared with those that undergo primary RYGB.
Slegtenhorst et al. report a higher incidence of complications for revisional RYGB (15.2 %) compared with primary RYGB (14.7 %) [13].
Worni et al. found a higher intraoperative complication rate for one-step GB removal to RYGB with a risk-adjusted OR of 2.3 and a higher postoperative complication rate with a risk-adjusted odds ratio of 8.0. The reoperation rate due to complications for these patients was 6.0 % compared with the complication related reoperation rate for primary RYGB [8]. The GBSR data revealed an OR of 1.3 (95 % confidence interval: 0.6–2.7, p = 0.471) for intraoperative and an OR of 1.1 (95 % CI: 0.6–1.9, p = 0.742) for postoperative complications for one-step reoperation compared with primary RYGB. The overall specific postoperative complications for one-step GB removal were significantly higher than for primary RYGB (OR = 2.1, 95 % CI: 1.4–3.1, p < 0.001).
GBSR data show that patients with a one-step RYGB have a lower incidence of intra- and postoperative complications. It is possible that the pouch is formed differently (smaller and longer) after GB in a one-step approach than in a two-step approach. Additionally, more scar tissue could be a reason for complications in two-step procedures. Therefore, we suggest performing band removal and RYGB as a one-step approach.
The median time interval between band removal and two-step RYGB operations was 74 days (range 13 to 289 days). The median time is influenced by patient preferences and particularly by health insurance coverage of the revisional procedure in Germany. In most cases, a new acceptance for payment of the revisional procedure by the health insurance system in Germany is necessary. This issue may be bias against the current investigation.
The multivariable data analysis from the GBSR revealed that of the factors analyzed (age, gender, comorbidities, BMI, primary gastric banding), there were no independent risk factors for leaks after a one- versus two-step RYGB after GB. Data regarding long-term weight loss and the amelioration of comorbidities after RYGB as a redo operation after GB are rare in the literature. Edholm et al. reported that the most common indications for revisional RYGB after VBG and GB were unsatisfactory weight loss. In this study, data on complications due to the procedures are not available. The weight loss data reported an excess body mass index loss of 39 % for patients with RYGB as a revisional procedure after GB, but the median BMI loss in this study was 4.4 kg/m2, which is a poor result in our opinion [14]. Slegtenhorst et al. and Zingg et al. also observed lower weight loss after revisional RYGB than after the primary procedure [13, 15].
In our opinion, data for the long-term effects of revisional RYGB, weight loss, and amelioration of comorbidities are necessary to further evaluate whether RYGB should remain the method of choice after failed GB.
Conclusions
Based on the GBSR data on the surgical treatment of RYGB after failed GB and a review of the literature, RYGB and band removal as a one-step procedure has a significantly lower incidence of overall (intraoperative and general) complications. Based on these data, band removal and RYGB performed as a one-step procedure reduces the leakage rate, but further evaluations with a higher number of procedures are necessary to confirm these findings. The problem with the evaluable data in the literature is that the primary procedures were heterogeneous and consist of GB, vertical banded gastroplasty, and sometimes sleeve gastrectomy. Therefore, a potential bias was present when comparing the GBSR data with the literature.
References
Lampert T. Übergewicht und Adipositas in Deutschland. RKI Epidemiologisches Bull. 2007;18:155–6.
Mensink GBM, Schienkewitz A, Haftenberger M, Lampert T, Ziese T, Scheidt-Nave C. Übergewicht und Adipositas in Deutschland. Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DGES1). Bundesgesundheitsbl. 2013;56:786–94.
O’Brien PE, Macdonald L, Anderson M. Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg. 2013;257:87–94.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23:427–36.
Stroh C, Weiner R, Horbach T, Ludwig K, Dressler M, Lippert H, et al. New data on quality assurance in bariatric surgery in Germany. Zentralbl Chir. 2013;138:180–8.
Cadière GB, Himpens J, Bazi M, Cadière B, Vouche M, Capelluto E, et al. Are laparoscopic gastric bypass after gastroplasty and primary laparoscopic gastric bypass similar in terms of results? Obes Surg. 2011;21(6):692–8.
Robert M, Poncet G, Boulez J, Mion F, Espalieu P. Laparoscopic gastric bypass for failure of adjustable gastric banding: a review of 85 cases. Obes Surg. 2011;21:1513–9.
Worni M, Østbye T, Shah A, et al. High risks for adverse outcomes after gastric bypass surgery following failed gastric banding: a population-based trend analysis of the United States. Ann Surg. 2013;257:279–86.
Apers JA, Wens C, van Vlodrop V, et al. Perioperative outcomes of revisional laparoscopic gastric bypass after failed adjustable gastric banding and after vertical banded gastroplasty: experience with 107 cases and subgroup analysis. Surg Endosc. 2013;27:558–64.
Hii MW, Lake AC, Kenfield C, Hopkins GH. Laparoscopic conversion of failed gastric banding to Roux-en-Y gastric bypass: short-term follow-up and technical considerations. Obes Surg. 2012;22:1022–8.
Coblijn UK, Verveld CJ, van Wagensveld BA, Lagarde SM. Laparoscopic Roux-en-Y gastric bypass or laparoscopic sleeve gastrectomy as revisional procedure after adjustable gastric band—a systematic review. Obes Surg. 2013;23:1899–914.
Morais AA, Faintuch J, Leal AA, Noe JA, Bertollo DM, Morais RC, et al. Inflammation and biochemical features of bariatric candidates: does gender matter? Obes Surg. 2011;21:71–7.
Slegtenhorst BR, van der Harst E, Demirkiran A, de Korte J, Schelfhout LJ, Klaassen RA. Effect of primary versus revisional Roux-en-Y gastric bypass: inferior weight loss of revisional surgery after gastric banding. Surg Obes Relat Dis. 2013;9:253–8.
Edholm D, Näslund I, Anders Karlsson F, Rask E, Sundbom M. Twelve-year results for revisional gastric bypass after failed restrictive surgery in 131 patients. Surg Obes Relat Dis. 2014;10:44–8.
Zingg U, McQuinn A, DiValentino D, Kinsey-Trotman S, Game P, Watson D. Revisional vs. primary Roux-en-Y gastric bypass—a case-matched analysis: less weight loss in revisions. Obes Surg. 2010;20:1627–32.
Acknowledgments
The German Nationwide Survey on Bariatric Surgery is supported by the Ministry of Research and Education Germany (BMBF) grant number 01GI1124. The responsible investigator is Christine Stroh. The following firms support the GBSR without any relation to their products: Johnson & Johnson MEDICAL GmbH, Ethicon Endo-Surgery Deutschland, Norderstedt Covidien Deutschland GmbH, and Neustadt/Donau. We thank all of the hospitals that participated in this study for their active engagement.
Conflict of Interest
The authors declare that there is no conflict of interest. Christine Stroh, Rudolf Weiner, Stefanie Wolff, Claudia Lerche, Christian Knoll, Thomas Keller, Thomas Manger and Christiane Bruns confirm that there are no links to firms whose products are mentioned in the article or to firms marketing a competing product. The topic is presented in an independent light and the information outlined is product neutral.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Stroh, C., Weiner, R., Wolff, S. et al. One Versus Two-Step Roux-en-Y Gastric Bypass After Gastric Banding—Data Analysis of the German Bariatric Surgery Registry. OBES SURG 25, 755–762 (2015). https://doi.org/10.1007/s11695-014-1527-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1527-0